Abstract
The authors present the case of a sacral chordoma in which the diagnosis was delayed as the patient was diagnosed and treated as coccydynia. Persistent, severe coccydynia following minor trauma is common1 but the symptom can also be caused by significant underlying disease. The correct diagnosis was made in this patient but after significant delay. The presentation of this case involved multiple specialties and provides several learning points regarding the importance of thorough history taking and clinical examination. It highlights the importance of ‘red flag’ symptoms of low back pain2 which need to be fully investigated.
Background
We present a case involving the delayed diagnosis of a sacral chordoma. This case highlights the importance of a thorough history, examination and differential diagnosis when investigating a patient with persistent back pain. The patient in question described ‘red flag’ symptoms associated with low back pain. She did not undergo neurological nor per rectal (PR) examination and unfortunately initial imaging showing pathology was reported as normal. The diagnosis of coccydynia was not revised despite deterioration with appropriate treatment for that condition. Back pain is a common condition with a complex aetiology and can have a sinister underlying cause.
Case presentation
A 59-year-old female fell at a wedding onto her lower back. This trauma resulted in constant, severe pain in her coccyx. The pain was worse at night, radiated under her perineum to her vagina and was described as ‘sitting on golf balls’.
Initial radiographs of her spine and coccyx were reported as normal. After 1 year of pain she developed urinary symptoms and an MRI of her lumbar spine was also reported as normal. She then underwent an ultrasound scan (USS) of her pelvis that showed a possible collection. She was referred to obstetrics and gynaecology and a CT abdomen and pelvis was arranged, which showed a tumour arising from the sacrum and coccyx. Seventeen months after the onset of her symptoms and prior to her outpatient referral she presented to local hospital in acute urinary retention and was transferred to the cardiff spinal unit at the University Hospital Wales.
Investigations
Eight months after the onset of symptoms a radiograph (figure 1) of her coccyx was performed, reported as normal.
Figure 1.

Radiograph of lumbar spine and sacrum showing destruction of the sacral vertebrae.
After developing urinary symptoms at 14 months she had an MRI of her lumbar spine (figure 2) again reported as normal.
Figure 2.

MRI of the lumbar spine showing a lesion arising from the inferior border of the image.
Two months later she had an USS of her pelvis that showed a possible collection. She then underwent a CT abdomen and pelvis (figure 3), which showed a tumour arising from the sacrum and coccyx. Given the patient’s age, the likely diagnosis would be chordoma. On admission to her local hospital an MRI of her sacrum (figure 4) clearly showed the tumour. At the cardiff spinal unit a CT biopsy was performed. Histological examination showed groups of tumour cells with vacuolated cytoplasm and surrounding myxoid stroma (figure 5).
Figure 3.
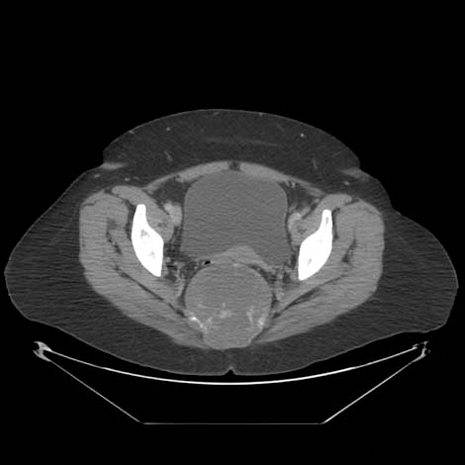
CT scan showing a tumour arising from the sacrum.
Figure 4.

MRI of the sacrum showing the sacral tumour.
Figure 5.
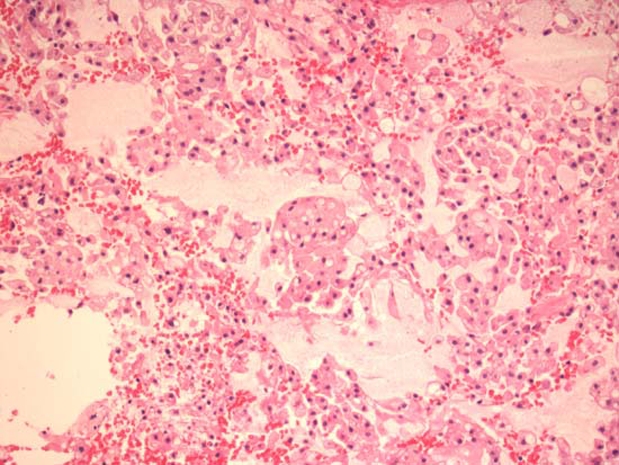
The typical physaliphorous cells of chordoma.
Differential diagnosis
The causes of coccydynia include:
-
▶
Trauma.
-
▶
Childbirth.
-
▶
Repetitive strain or sitting.
-
▶
Excess slimness/obesity.
-
▶
Cysts or tumour.
Chordomas are primary bone tumours of the spine. They account for approximately 3% of all bone tumours and 20% of primary spinal tumours, with an approximate incidence of 1 new case per million people per year.3 They can occur at any spinal level, although commonly at the sacrum and coccyx (29%) and the intracranial clivus (32%).4 Caudal tumours can present as:
-
▶
‘Low low’ back pain.
-
▶
Symptoms of bladder or bowel obstruction.
-
▶
A soft tissue mass.
Treatment
The patient underwent successful en bloc resection of her sacral chordoma. Our procedure required a multidisciplinary team approach with oncological and spinal surgery teams. The presacral dead space was reconstructed with bilateral gracilis flaps (figure 6) The rectum was preserved.
Figure 6.
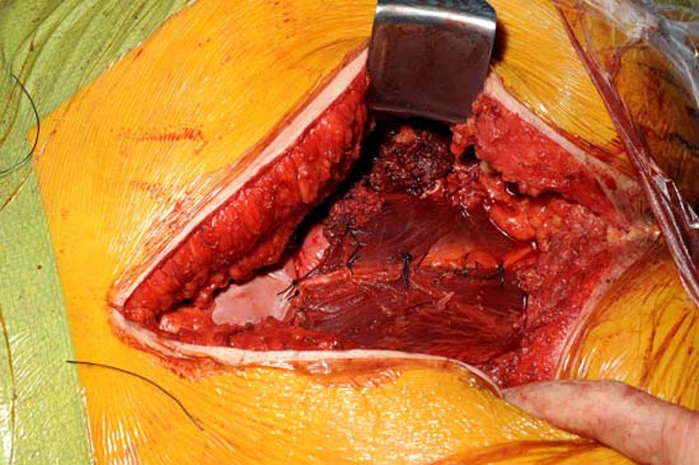
Intraoperative photograph (cranial to the left, caudal to the right). The pelvic floor reconstruction with dural repair patch over the sacral stump and bilateral gracili muscle flaps mobilised through the ischiorectal fossae, to cover the rectum. The defect was closed directly over this construction.
Outcome and follow-up
The patient made an excellent recovery. Specialist nurse input was required to manage her bladder and bowel dysfunction. Her bladder was controlled using intermittent self catheterisation and her bowels were managed using the ‘Peristeen’ colonic irrigation system. As her perineum is insensate the patient was educated regarding pressure area care. She had no neurological deficit in her lower limbs and at the 1 month follow-up was driving and had returned to work.
Discussion
There are over 100 case reports in the literature concerning sacral chordomas, with varied and interesting presentations. As chordomas are not chemo nor radiosensitive and have a tendency to recur locally, en bloc resection with wide surgical margins is the treatment of choice and may be curative.5 British Medical Journal case reports do not currently include a case of sacral chordoma. The importance of this case is the history and examination of the patient. Back pain is a common condition and may be encountered in any specialty. Clinicians should be aware of the ‘red flag’ symptoms associated with back pain.2 Night pain is not usually mechanical and may be caused by tumours. Low back pain with bladder/bowel dysfunction should be investigated fully. Severe unrelenting pain is not normally due to degenerative disease. It should be noted that many gynaecological conditions present with vague perineal pain radiating to the medial aspect of the thighs.
While primary spinal tumours are rare, they can be a cause of back pain. Full examination is mandatory; most sacral tumours are palpable on rectal examination.6
Learning points.
-
▶
‘Red flags’ in low back pain are detailed in any orthopaedic text2 or Cauda Equina Syndrome review article and clinicians should be aware of these symptoms.
-
▶
Anogenital pain, bladder and bowel symptoms are often difficult and embarrassing to investigate and diagnose. The correct diagnosis was made in this patient but after significant delays.
-
▶
In a patient with low back pain and bladder and bowel dysfunction, the omission of a PR examination is negligent.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Wray CC, Easom S, Hoskinson J. Coccydynia. Aetiology and treatment. J Bone Joint Surg Br 1991;73:335–8 [DOI] [PubMed] [Google Scholar]
- 2.Clarke A, Jones A, O’Malley M. ABC of Spinal Disorders. BMJ Books London: Wiley-Blackwell; 2010 [Google Scholar]
- 3.Kelley SP, Ashford RU, Rao AS, et al. Primary bone tumours of the spine: a 42-year survey from the Leeds regional bone tumour registry. Eur Spine J 2007;16:405–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McMaster ML, Goldstein AM, Bromley CM, et al. Chordoma: incidence and survival patterns in the United States, 1973–1995. Canc Causes Contr 2001;12:1–11 [DOI] [PubMed] [Google Scholar]
- 5.Rao G, Chang GJ, Suk I, et al. Midsacral amputation for en bloc resection of chordoma. Neurosurgery 2010;66:41–4 [DOI] [PubMed] [Google Scholar]
- 6.Mindell ER. Chordoma. J Bone Joint Surg Am 1981;63:501–5 [PubMed] [Google Scholar]


