Abstract
Objective
Physicians are inaccurate in predicting non-adherence in patients, a problem that interferes with physicians’: 1) appropriate prescribing decisions and 2) effective prevention/intervention of non-adherence. The purpose of the current study is to investigate potential reasons for the poor accuracy of physicians’ adherence-predictions and conditions under which their predictions may be more accurate.
Methods
After the medical encounter, predictions of patient-adherence and other ratings from primary-care physicians (n=24) regarding patient-factors that may have influenced their predictions were collected. Patients (n=288) rated their agreement regarding the prescribed treatment after the encounter and reported adherence one month later.
Results
Several factors were related to physicians’ adherence-predictions, including physicians’ perceptions of patient-agreement regarding treatment. However, some factors were not related to adherence and agreement-perceptions were inaccurate overall, potentially contributing to the poor accuracy of adherence-predictions. The degree to which physicians discussed treatment-specifics with the patient moderated agreement-perception accuracy but not adherence-prediction accuracy.
Conclusions
Training providers to discuss certain treatment-specifics with patients may improve their ability to perceive patient-agreement regarding treatment and may directly improve patient-adherence.
Practice Implications
Discussing treatment-specifics with patients may directly improve adherence, but providers should not rely on these discussions to give them accurate estimates of the patients’ likely adherence.
Keywords: patient adherence, physician predictions, patient beliefs, perceived agreement
1. Introduction
It has been well documented that physicians are inaccurate estimators of adherence and are “no better than chance” at judging which patients are adherent and which are not (1,2). When estimating the degree of adherence for any particular patient, physicians have been shown to be accurate only 10 to 40% of the time, for both medication and other treatments (3-5). Improving non-adherence detection by physicians has the potential to directly increase patients’ treatment adherence and improve patients’ health outcomes for the reasons outlined below.
Accurate detection of patient non-adherence is important for determining which patients may require intervention—a determination that physicians are uniquely positioned to make for the following reasons: treatment adherence is initiated in the medical encounter and has been defined as “the extent to which a patient’s behavior (in terms of taking medication, following a diet, modifying habits, or attending clinics) coincides with medical or health advice”(6). Initial patient attitudes regarding the treatment and its efficacy are formed in the medical visit, and treatment utility attitudes are key predictors of intentions to adhere (7). If physicians were able to accurately predict that a patient would be nonadherent to a treatment, then they could address the potential issues initially, avoiding poor outcomes, repeat office visits, and patient frustration. Furthermore, targeting interventions given only to those who are “high-risk” is the most efficient, effective, and economical method of ameliorating a problem (8).
Accurate detection of patient non-adherence is also important for making appropriate prescription decisions. Physicians may withhold a treatment if they think a patient is or is likely to be non-adherent for illnesses that may become drug-resistant in the general population if patients are non-adherent (e.g., antiretroviral medications, hemophilia medications, an antibiotics) (9-11).
Physicians have reported using biological markers, such as blood-levels of a medication to predict patients’ adherence to the medication (12-15). However, these biological markers may be unreliable estimates of adherence (16). For example, some biological indicators are affected by individualized metabolic pathways or by patients’ anxiety (“white coat syndrome”;17) and require ambulatory monitoring that is expensive in order to demonstrate and use as adherence-estimators.
Whether physicians use characteristics of the individual patient, such as directly observable information or information from medical records such as gender, race/ethnicity, age, and chronic illness diagnoses, has not been widely assessed with research, although one scenario-based experiment found that physicians were more likely to judge African-American men as less adherent to their antiretroviral medications (14). Patient gender and race have been studied as influences on providers’ prescribing behaviors (18,19). After controlling for medically relevant information regarding cardiovascular catheterization, researchers have found that physicians were less likely to prescribe treatment to women and to African-Americans, compared to men and Caucasian-Americans, respectively (18) and that physicians rated men as more likely to benefit from cardiac catheterization than women (19). Since factors such as race and gender influence prescribing behaviors in some medical situations, it is plausible that they would also affect providers’ predictions for patient adherence to the prescribed treatment. Demographics such as race or socioeconomic status have not been found to predict adherence (2,14). If physicians’ predictions are associated with the above characteristics, then this might be one reason why their adherence predictions have poor accuracy.
Physicians may also estimate characteristics of the patient that are not directly observable or available in medical charts to assess whether the patient will adhere to their prescribed treatment. One such characteristic, the focus of the current investigation, is the degree to which the patient agrees with the physician regarding the illness and treatment specifics (e.g., what the cause of the illness/problem is, how the treatment will address the illness, how long it will take for the treatment to work, how the patient will know if the treatment is working). This characteristic is the focus of our investigation, because patients’ beliefs regarding the illness and treatment, including treatment efficacy beliefs (7) and their illness representations (the causes, control/treatment, duration/timeline, consequences, and symptom-recognition of an illness; 8,20), have been shown to be highly predictive of patient adherence (e.g.,21,22). Therefore, theoretically, if physicians can accurately perceive the patients’ agreement on the treatment and illness, they should have more accurate predictions of adherence. Poor adherence prediction may potentially be due to one of two possible cases regarding this issue: 1) physicians’ adherence-predictions are not associated with their perceptions of agreement with the patient or 2) physicians’ adherence-predictions are associated with their perceptions of agreement with the patient but their perceptions of agreement are inaccurate. This distinction would inform interventions to improve physicians’ accuracy in predicting patient-adherence.
The purpose of the current study is to investigate possible sources of information that physicians use to predict adherence and to investigate potential reasons for physicians’ poor prediction-accuracy, including the observable patient characteristics and patient-agreement regarding the illness- and treatment-specifics introduced above. Lastly, the current investigation tests a potential moderator of the accuracy of physicians’ perceptions of agreement with the patient (i.e., a moderator of the association between physicians’ perceptions of agreement and patients’ perceptions of agreement) and the accuracy of their predictions of patient-adherence (i.e., a moderator of the association between physicians’ predictions of patient adherence and patients’ actual adherence) that may also inform future interventions to improve physicians’ predictions of adherence. We propose that if the physician discusses the treatment and illness specifics with the patient, then their perceptions of agreement and also their predictions of adherence will be more accurate. Holding discussions means more information is shared and physicians should have a better sense of patient agreement regarding the illness and treatment specifics (the patients’ illness representations). Other researchers have proposed that discussions between physicians and patients regarding patient preferences and lifestyle may improve physicians’ ability to predict non-adherence (10), but no one has assessed whether discussions regarding the patients’ illness- and treatment-specific beliefs can improve this ability.
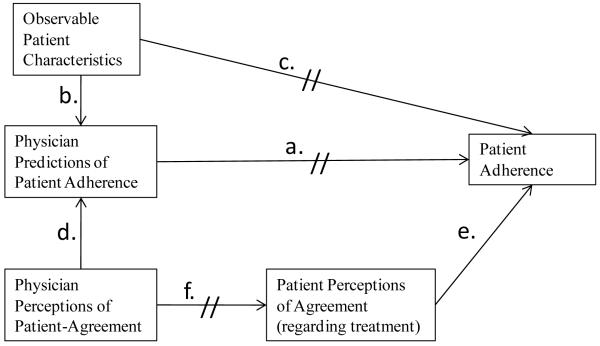
The specific hypotheses of the current investigation are illustrated in Figure 1 and are the following: 1) physicians’ predictions of patient adherence will have poor accuracy, defined for the current study as any correlation less than .30 (a small/weak correlation on Cohen’s scale, which is equivalent to approximately 10% of the variance in actual adherence being explained by physicians’ predictions of adherence—an estimate reported in a review of relevant studies (10); relationship a in Figure 1); 2a) physicians’ predictions of patient adherence will be associated with information about the patient that is directly observable and/or evident from medical records (relationship b); 2b) these observable/medical-record characteristics will not be related to actual patient adherence (relationship c); 3a) physicians’ predictions of patient adherence will be associated with physicians’ perceptions of patient-agreement regarding the illness and prescribed treatment (relationship d); 3b) patients’ perceptions of agreement with the physician regarding the illness and prescribed treatment will predict their adherence (relationship e); 3c) physicians’ perceptions of agreement will have poor accuracy (i.e. physicians’ perceptions will not match patients’ perceptions of agreement; relationship f); 4) the accuracy of physicians’ perceptions of agreement will depend on (be moderated by) the degree to which they discuss treatment specifics with the patient during the medical encounter (discussions will moderate relationship f); 5) the accuracy of physicians’ predictions of patient adherence will depend on (be moderated by) the degree to which they discuss treatment specifics with the patient during the encounter (discussions will moderate relationship a).
Figure 1.
The study hypotheses are illustrated in this figure. Double line markings through a path indicate that the relationship between the two variables connected by the path is hypothesized to be non-significant. References to “agreement” are agreement regarding the illness- and treatment-specifics, such as likely illness and treatment duration, time until treatment works, likely efficacy of treatment, etc. Note that the paths in the figure are hypothesized relationships and are not meant to depict strict causal relationships or imply that the current data are more than correlational.
2. Methods
The data analyzed for this study are from a larger dataset, which was collected in order to study the overall processes of patients’ illness-representation formation and change, as well as patient adherence and outcomes in a primary care clinic. The physicians’ data are the focus of the current analyses and are correlational and measured cross-sectionally; some of the patient data used in the current analyses were measured cross-sectionally and some were measured longitudinally. The larger study’s design and patient data measures and characteristics are described below, insofar as they pertain to the current analyses (i.e., for testing the accuracy of the physicians’ perceptions of agreement with the patient and predictions of patient-adherence).
2.1 Procedure
2.1.1 Patients
After receiving institutional review-board approval for the study, patients were recruited from a primary care clinic; all patients who came to the clinic for an appointment were approached for participation, 3 days per week, from September 2007 until November 2008. Informed consent from participants was obtained in writing while they were in the waiting room. All patient data included in the current analyses were collected by phone within 48 hours of the medical visit, except for patient adherence, which was assessed one month after the visit.
2.1.2 Physicians
After each patient visit, physicians were given a 1-page questionnaire to complete. Physicians were asked to predict how adherent the patients would be in the month after the visit, and they were asked to rate factors that may have influenced their predictions. Every feasible effort was made to obtain the questionnaires from participating physicians; attempts to collect the questionnaires by research staff ceased after three requests for missing questionnaires.
2.2 Participants
Only patients under 18 years of age, who did not speak English, or who were not patients of participating physicians were excluded from participation. Patients were only recruited once for the study. Physicians completed questionnaires for only 288 of the 402 initially recruited participants (patient sample size=288). Demographic information for the patients included in the current study is presented in Table 1. Independent samples t-tests showed that patients included in the current analyses did not differ from those who were excluded on any of the variables described below.
Table 1.
Sample Characteristics. The physician ratings were made by 24 physicians for 288 patients.
| Measure/Characteristic | Mean Value (SD)/Percentage | Range |
|---|---|---|
| Physician predictions of patient adherence | 4.04 (.75) | 1-5 |
| Physician perceptions of agreement | 3.92 (.86) | 1-5 |
| Patient demographics | ||
| Female gender | 64% | |
| Age at time of visit | 56.83 (16.50) | 21-90 |
| Minority status | 30% | |
| Patient chronic status (1+ chronic conditions) | 70% | |
| Patient adherence | .0306 (.69) | Z-scores |
| Patient perceptions of agreement | 4.29 (.78) | 1-5 |
| Degree to which physicians discussed treatment and illness |
3.97 (2.27) | 0-7 |
All physicians were members of the primary care clinic faculty or were residents under the supervision of the faculty. Twenty-four physicians participated in the study, consisting of 10 full faculty members and 14 residents. Eighty-four percent of patients were seen by faculty physicians.
2.3 Physician-rated and objective measures
2.3.1 Predictions of patient adherence
Physicians were asked: “How confident are you that the patient will follow the prescribed treatment: Not at all, a little bit, somewhat, quite confident, very confident?”
2.3.2 Physician perceptions of agreement
Physicians’ perceptions of agreement with the patients about illness and treatment specifics were measured with 4 items, all on a 5-point scale from “not at all” to “very much”. The items matched those given to patients, below, differing only in their reference to the patient/physician. The items, with wording read by the physicians are the following: “Is the patient’s view of how long this condition will last similar to yours,” “The patient and I agreed on the causes of the condition,” “Overall, the patient and I share a common understanding of the condition,” and “Overall, how much would you say you and your patient share a common understanding of the treatment?” The 4 items were averaged into a composite variable and had high internal consistency (α = .95).
2.3.3 Patient demographics
Gender (1= female), age at the time of the visit, and minority status (converted to 0 = Caucasian, 1 = Minority due to lower proportion of minorities in the sample).
2.3.4 Patient chronic illness status
The patients’ chronic status (no chronic conditions = 0, has 1+ chronic conditions=1) was recorded from the patient self-reports of physician-diagnoses (“Have you ever been told by a health profession that you have: diabetes, cardiovascular disease, hypertension, asthma/COPD, or other chronic illness?”). Physicians had access to the patients’ electronic medical records (EMR), which provide information on the patients’ number and type of chronic illnesses. The patient-report variable was made dichotomous because the emphasis of the current study is on adherence to treatments for a presenting problem (newly prescribed treatment) and to minimize the chance of discrepancies between the patients’ reports and the EMR.
2.4 Patient-rated measures
2.4.1 Patient adherence
Adherence was assessed at the 1-month follow-up interview with the Medication Adherence Report Scale (23), a valid and reliable self-report measure of patient adherence consisting of 5 items, each on a 5-point scale from “always” to “never” (e.g., “Did you ever forget to do your treatment?”). The 5 items were averaged into a composite and had acceptable internal consistency (α = .70).
2.4.2 Patient perceptions of agreement
Patients’ perceptions of agreement with the physicians about illness and treatment specifics were measured with the same 4 items that are presented in Section 2.3.2 but with reference to the physician rather than the patient. The 4 items were averaged into a composite variable and had good internal consistency (α = .82).
2.4.3 Degree to which physician discussed treatment/illness
The degree to which physicians discussed the illness- and treatment-specifics with the patients (including the patients’ beliefs about the illness and treatment) was assessed via patient report of the physicians’ objective behaviors. Objective behaviors of the physician were assessed to avoid social desirability bias (24) that may have resulted from asking patients to evaluate subjectively their physicians’ performance. Seven items, all with yes/no responses, were summated into a composite: “The doctor discussed with me what might be the cause”; “The doctor told me how long I could expect to have this problem”; “The doctor told me what s/he was looking for during the physical exam”; “The doctor gave me clear instructions about my treatment: what to do, when, how often, and for how long”; “The doctor told me what I might expect when taking my medication/treatment”; “The doctor gave me some tips to help me work my treatment into my daily routine”; “The doctor told me how to monitor my problem to see if the treatment is working”. The scale had acceptable internal consistency (α = .79).
2.5 Statistical analysis
Correlations were used to asses Hypotheses 1-3, and hierarchical linear regression was used to assess Hypotheses 4 and 5 (alpha=.05). Fisher’s z transformation was used to calculate 95% confidence intervals for the correlations and 95% confidence intervals were calculated for the unstandardized regression coefficients reported for analyses of Hypotheses 4 and 5. SPSS version 17 was used for all analyses.
3. Results
Random-intercepts, multilevel modeling analyses were first conducted (in SPSS; SPSS Inc.) to determine the significance of a physician-level effect on the assessed relationships. None of the predictors, outcomes, or relationships between the predictors and outcomes differed significantly by physician; therefore, the data were analyzed assuming independence of patient observations.
3.1 Sample Characteristics
Sample characteristics and means (SDs) are presented for all study variables in Table 1. The breakdown of race in the current sample is the following: 63% Caucasian-American, 14% African-American, 4% Asian, less than 1% Native-American, and 5% “other” race. The types of chronic illness in the current sample included the following: 18% had type II diabetes, 15% cardiovascular disease, 48% hypertension, 15% asthma or COPD, and 25% “other” chronic condition.
3.2 Hypothesis 1
Physicians’ prospective predictions of patient adherence were weakly but significantly and positively correlated with patients’ self-reported adherence (Pearson r =.19, 95% CI (.13,.25), p<.05), supporting the hypothesis that the prediction accuracy would be poor.
3.3 Hypotheses 2a and 2b
Table 2 presents bivariate Pearson correlations and significance values of the correlations between all study variables. Patients’ minority status was significantly associated with physicians’ predictions of patient adherence (Pearson r = −.23, 95% CI (−.17,−.28), p<.001), as hypothesized, but patients’ chronic illness status, gender, and age were not (respectively, Pearson r = −.01, 95% CI (−.05,.07); .11, 95% CI (.05,.17); .05, 95% CI (−.01,.11); p>.05 for all). None of these factors were related to actual patient adherence, as hypothesized (respectively, Pearson r = .04, 95% CI (−.02,.10); −.05, 95% CI (−.11,.01); .00, 95% CI (−.06,.06); .03, 95% CI (−.03,.09); p>.05 for all).
Table 2.
Pearson or point-biserial correlations between study variables; internal consistency statistics (Cronbach’s alphas) are given on the diagonals in italics, where applicable.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Physician Prediction of Patient Adherence |
— | ||||||||
| 2 | Patient Adherence | 0.19* | 0.70 | |||||||
| 3 | Chronic Status of Patient | −0.01 | 0.04 | — | ||||||
| 4 | Patient Gender | 0.11 | 0.00 | 0.03 | — | |||||
| 5 | Patient Age | 0.05 | 0.03 | 0.26** | −0.04 | — | ||||
| 6 | Patient Minority Status | −0.23** | 0.04 | −0.01 | 0.09 | −0.19** | — | |||
| 7 | Physician Perception of Agreement |
0.62** | 0.19* | −0.17** | 0.05 | −0.13* | −0.18** | 0.95 | ||
| 8 | Patient Perception of Agreement |
0.15 | 0.19* | −0.01 | −0.02 | −0.08 | −0.17* | 0.00 | 0.82 | |
| 9 | Degree to which Physician Discussed Treatment |
0.00 | .25** | −0.13 | −0.14 | −.18* | .10 | 0.04 | .37** | 0.79 |
Note. Chronic Status of Patient is a dichotomous variable=0 if no chronic illness and =1 if 1 or more chronic illnesses; Patient gender is dichotomous with 1=female; Patient minority status is dichotomous with minority race=1 and Caucasian American race=0; all other variables are continuous with ranges presented in Table 1.
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
3.4 Hypotheses 3a, 3b, and 3c
All three hypotheses were supported. As can be seen from Table 2, physicians’ predictions of patient adherence were significantly and positively correlated with physicians’ perceptions of agreement with the patient regarding the illness and treatment (Pearson r=.62, 95% CI (.59,.66), p<.01). Patients’ perceptions of agreement with the physician regarding the illness and treatment were significantly but weakly related to their adherence (Pearson r=.19, 95% CI (.13,.25), p<.05). However, physicians’ perceptions of agreement had poor accuracy: physicians’ perceptions of agreement did not match patients’ perceptions of agreement (Pearson r =0.00, 95% CI (−.06,.06); p=.99). Overall, physicians perceived less agreement than did patients (mean 3.92(.86) versus 4.29(.78), respectively).
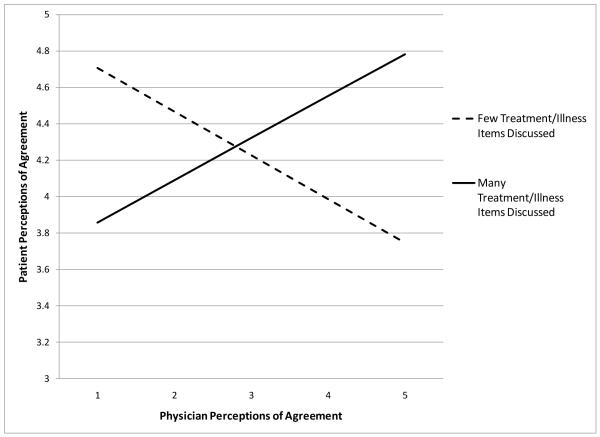
3.5 Hypothesis 4
Whether the degree to which physicians discussed illness/treatment specifics with the patient during the medical encounter moderated the accuracy of physicians’ perceptions of agreement with the patient (i.e. moderated the relationship between physicians’ and patients’ perceptions of agreement) was tested using hierarchical linear regression. The interaction term between physicians’ perceptions of agreement and the degree to which they discussed illness/treatment specifics with the patient significantly predicted patients’ perceptions of agreement, providing support for the hypothesis (t(286) = 3.87, p <.001). The moderation/interaction is depicted in Figure 2.
Figure 2.
The relationship between physicians’ and patients’ perceptions of agreement on the illness and treatment specifics was moderated by the degree to which physicians discussed these specifics with the patient during the medical encounter. The more specifics discussed, the better was the match between patients’ and physicians’ perceptions (the greater was the accuracy of the physicians’ perceptions of agreement). Values of patient perceptions of agreement in the figure were calculated at +/−1 SD of the predictor and moderator.
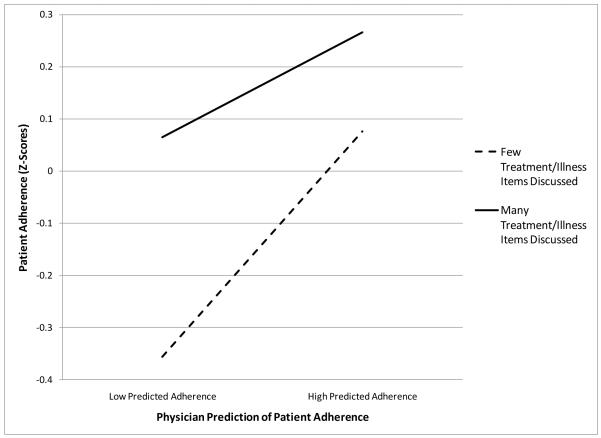
3.6 Hypothesis 5
Whether the degree to which physicians discussed illness/treatment specifics with the patient during the medical encounter moderated the accuracy of physicians’ predictions of patient-adherence (i.e. moderated the relationship between physicians’ predictions of adherence and patients’ actual adherence) was tested using hierarchical linear regression. The interaction term between physicians’ predictions of adherence and the degree to which they discussed illness/treatment specifics with the patient did not significantly predict patients’ reports of adherence, providing evidence against our hypothesis (t(286)=−.82, B=−.256, 95% CI (−.877,.365), p=.42). Therefore, the main effects are reported and interpreted in the discussion: as stated previously, physicians’ predictions were significantly, if weakly, related to patient adherence, and the degree to which physicians discussed illness/treatment specifics with patients significantly and positively predicted patient adherence (t(286)=2.18, B=.49, 95% CI (.026,.963), p<.05). The main effects are depicted in Figure 3.
Figure 3.
Patient adherence was predicted by both physicians’ predictions of patient-adherence and to the degree to which physicians discussed the illness/treatment specifics with the patient, but not to the interaction between these two factors. Values of patient-adherence in the figure were calculated at +/−1 SD of the predictor and moderator.
4. Discussion and Conclusion
4.1 Discussion
The weak correlation between physicians’ predictions of patient adherence and patient adherence follows findings in the literature (1-5). Below, we discuss the possible reasons why the physicians’ predictions of patient adherence may have had poor accuracy.
Of the directly observable variables and variables available in the patients’ charts, only the patients’ minority status was significantly related to the physicians’ predictions of patient adherence. One possible reason for the poor accuracy of physicians’ adherence predictions is therefore that they may have used the patients’ minority status to predict adherence when minority status was not itself related to adherence. The results indicate that providers may perceive minorities to be less adherent than Caucasian-Americans. Since providers are known to make prescribing decisions based on their estimates of patient adherence (9-11), one serious implication of this finding, is that providers may therefore be less likely to prescribe HIV treatments to African-Americans and other minorities—such as has been seen with providers’ decreased likeliness to prescribe cardiac catheterization to African-Americans (18,19).
The current study did not find that race was related to adherence, but it is possible that it is in some situations. Research in cancer-treatment decisions has shown large racial discrepancies (25); whether or not these discrepancies—perhaps due to minorities’ distrust of medical treatments (26)—may exist in likeliness to adhere to treatment for particular illnesses deserves further investigation. Training physicians on these distinctions would be possible and more useful than training them to ignore entirely the patients’ race as a potential factor in their adherence.
The second possible reason why physicians’ predictions of adherence may have had poor accuracy in the current sample is that even though physicians’ perceptions of agreement with the patient regarding the illness/treatment were related to their adherence predictions and patients’ perceptions of agreement were related to their actual adherence, physicians’ perceptions of agreement had zero correlation overall with patients’ perceptions of agreement. These results indicate that if physicians were more accurate in their perceptions of patient agreement, then they may also be more accurate in their predictions of patient adherence. Moderators of these relationships are discussed next.
The interaction in Figure 2 shows that physicians’ perceptions of agreement were more accurate when the physician discussed treatment/illness specifics with the patient during the medical encounter. Moreover, when physicians did not discuss these issues with the patient, their perceptions of agreement were inversely related to patients’ perceptions of agreement. This means that discussing the illness/treatment with patients is key for accurate awareness of whether the patient agrees about the treatment or not—a factor which was shown to predict patients’ adherence to the treatment.
The finding that when physicians discuss illness/treatment specifics with the patient they are more accurate in perceiving agreement with the patient regarding the prescribed treatment and that patients’ perceptions of agreement predict actual adherence would lead one to expect that when physicians discuss illness/treatment specifics with the patient, they should be accurate in their predictions of patient adherence. However, this was not found to be the case. It is possible that the relationship between patients’ perceptions of agreement and patient adherence is not strong enough for accurate perceptions by physicians of this agreement to translate to accurate predictions of adherence.
This study had some limitations, which necessitate future research. First, the design was correlational, even though physicians’ predictions were measured one month before patient adherence was assessed. For example, patients’ race may have influenced the physicians’ adherence-predictions, but whether or not the physicians consciously used this information is not known. However, physicians may not be aware of what factors influence their judgments, so indirect assessment like the current study design is in some ways preferable to directly asking the physicians what information influences their adherence predictions. In addition to designs like the current design, which benefit from real world applicablility, experimental designs with scenarios may be utilized to manipulate the information given to physicians about their patients to assess how these manipulations affect the physicians’ predictions. Second, despite the controversy over using single-item measures (27), physicians’ predictions of patient-adherence were assessed with a single item for practical reasons and because we think a single, general estimate is more likely to mirror what physicians normally form during medical encounters with patients. Furthermore, Drolet and Morrison (28) found that multiple items in a scale contributed very little to variance explained in the outcome compared to a single-item measure, and the multiple-item measure caused the participants to be irritated with the task (a risk we felt was particularly strong for primary care physicians, who are very short on time). Lastly, patient adherence was assessed via patient self-reports rather than by some other more objective measure. However, patient-reports have been found to be accurate and are more cost and time economical than other estimates of adherence (16).
4.2 Conclusion
The findings of the current study together indicate that holding discussions with the patient during the medical encounter does benefit physicians by making them better aware of agreement and disagreement with patients. However, this increase in agreement-perception accuracy did not translate to significantly better adherence-prediction accuracy, indicating that although patients’ perceptions of agreement with the physician regarding the illness and treatment are important for adherence, there may be stronger predictors of patient adherence that the physician should be aware of. For instance, perhaps if physicians were more aware of the effect that discussing illness/treatment specifics with patients has on patient adherence, they would more consciously base their adherence-predictions on how well or poorly those discussions went (or if they were held at all). Future research could test whether or not this awareness increases the accuracy of the physicians’ adherence-predictions.
Since it was found that providers were poor estimators of factors known to predict patient adherence (patient agreement regarding the illness/treatment-specifics), interventions designed to train providers to discuss these factors during the medical encounter may be helpful in directly improving patient adherence.
4.3 Practice Implications
The implications for medical practice, research, and policy of the current study include the following: first, physicians should be aware that patient minority status, as well as other demographic and chronic illness-related factors, may not be related to patient adherence. Second, physicians should be aware that discussing illness/treatment-specifics with patients during the medical encounter may improve patient adherence and improve physicians’ ability to perceive patient agreement regarding the prescribed treatment. Whether the accuracy of physicians’ adherence-predictions can be improved through discussions of these illness/treatment specifics with patients requires more research.
Acknowledgments
This paper was supported through a National Institutes for Health Grant, R24AG023958, The Center for the Study of Health Beliefs and Behaviors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work was presented at the annual conference of the Gerontological Society of America in Atlanta, GA, on November 21, 2009.
References
- [1].Wagner JH, Justice AC, Chesney M, Sinclair G, Weissman S, Rodriguez-Barradas M, VACA 3 Project Team Patient- and provider reported adherence: toward a clinically useful approach to measuring antiretroviral adherence. J Clin Epidemiol. 2001;54:S91–8. doi: 10.1016/s0895-4356(01)00450-4. [DOI] [PubMed] [Google Scholar]
- [2].Zeller A, Taegtmeyer A, Martina B, Battegay E, Tschudi P. Physicians’ ability to predict patients’ adherence to antihypertensive medication in primary care. Hypertens Research. 2008;31:1765–71. doi: 10.1291/hypres.31.1765. [DOI] [PubMed] [Google Scholar]
- [3].Morton A, Riddle R, Buchanan R, Katz D, Birch J. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J Pediatr Orthopaedics. 2008;28:336–41. doi: 10.1097/BPO.0b013e318168d154. [DOI] [PubMed] [Google Scholar]
- [4].Parker CS, Chen Z, Price M, Gross R, Metlay JP, Christie JD, Brensinger CM, Newcomb CW, Samaha FF, Kimmel SE. Adherence to Warfarin assessed by electronic pill caps, clinician assessment, and patient reports: Results from the IN-RANGE Study. J Gen Intern Med. 2007;22:1254–59. doi: 10.1007/s11606-007-0233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Turner BJ, Hecht FM. Improving on a coin toss to predict patient adherence to medications. Ann Intern Med. 2001;134:1004–06. doi: 10.7326/0003-4819-134-10-200105150-00015. [DOI] [PubMed] [Google Scholar]
- [6].Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment. JAMA. 2002;288:2880–3. doi: 10.1001/jama.288.22.2880. [DOI] [PubMed] [Google Scholar]
- [7].DiMatteo MR. Future directions in research on consumer-provider communication and adherence to cancer prevention and treatment. Patient Educ Couns. 2003;50:23–6. doi: 10.1016/s0738-3991(03)00075-2. [DOI] [PubMed] [Google Scholar]
- [8].Leventhal H, Weinman J, Leventhal E, Phillips LA. Health psychology: The search for pathways between behavior and health. Annu Rev Psychol. 2008;59:477–505. doi: 10.1146/annurev.psych.59.103006.093643. [DOI] [PubMed] [Google Scholar]
- [9].Gross R, Bilker WB, Friedman HM, Coyne JC, Strom BL. Provider inaccuracy in assessing adherence and outcomes with newly initiated antiretroviral therapy. AIDS. 2002;16:1835–37. doi: 10.1097/00002030-200209060-00021. [DOI] [PubMed] [Google Scholar]
- [10].Murri R, Antinori A, Ammassari A, Nappa S, Orofino G, Abrescia N, Mussini C, D’Arminio Monforte A, Wu AW, AdlCoNA Study Group Physician estimates of adherence and the patient-physician relationship as a setting to improve adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31:S158–62. doi: 10.1097/00126334-200212153-00015. [DOI] [PubMed] [Google Scholar]
- [11].Thornburg CD. Physicians’ perceptions of adherence to prophylactic clotting factor infusions. Haemophilia. 2008;14:25–9. doi: 10.1111/j.1365-2516.2007.01591.x. [DOI] [PubMed] [Google Scholar]
- [12].Bogart LM, Kelly JA, Catz SL, Sosman JM. Impact of medical and nonmedical factors on physician decision making for HIV/AIDS antiretroviral treatment. J Acquir Immune Defic Syndr. 2000;23:396–404. doi: 10.1097/00126334-200004150-00006. [DOI] [PubMed] [Google Scholar]
- [13].Barfod TS, Hecht FM, Rubow C, Gerstoft J. Physicians’ communication with patients about adherence to HIV medication in San Francisco and Copenhagen: A qualitative study using Grounded Theory. BMC Health Serv Res. 2006;6:154–66. doi: 10.1186/1472-6963-6-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bogart LM, Catz SL, Kelly JA, Benotsch EG. Factors influencing physicians’ judgments of adherence and treatment decisions for patients with HIV disease. Med Decis Making. 2001;21:28–36. doi: 10.1177/0272989X0102100104. [DOI] [PubMed] [Google Scholar]
- [15].Wurst KE, Sleath BL, Konrad TR. Physicians’ perceptions of factors influencing adherence to antibiotic prophylaxis in children with sickle cell disease. Curr Ther Res. 2003;64:116–26. doi: 10.1016/S0011-393X(03)00016-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Haynes RB, Taylor DW, Sackett DL, Gibson ES, Bernholz CD, Mukherjee J. Can simple clinical measurements detect patient noncompliance? Hypertension. 1980;2:757–64. doi: 10.1161/01.hyp.2.6.757. [DOI] [PubMed] [Google Scholar]
- [17].Pickering T, James G, Boddie C, Harshfield G, Blank S, Laragh J. How common is white coat hypertension? JAMA. 1988;259:225–8. [PubMed] [Google Scholar]
- [18].Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ. The effect of race and sex on physicians’ recommendations for cardiac catheterization. NEJM. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- [19].Kreatsoulas C, Sloane D, Pogue J, Velianou JL, Anand SS. Referrals in acute coronary events for CARdiac catheterization: The RACE CAR trial. Can J Cardiol. 2010;26:e290–6. doi: 10.1016/s0828-282x(10)70436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The Self-Regulation of Health and Illness Behaviour. Routledge; London: 2003. pp. 42–65. [Google Scholar]
- [21].Heurtin-Roberts S, Reisin E. The relation of culturally influenced lay models of hypertension to compliance with treatment. Am J Hypertens. 1992;5:787–92. doi: 10.1093/ajh/5.11.787. [DOI] [PubMed] [Google Scholar]
- [22].Meyer D, Leventhal H, Gutmann M. Common-sense models of illness: The example of hypertension. Health Psychol. 1985;4:115–35. doi: 10.1037//0278-6133.4.2.115. [DOI] [PubMed] [Google Scholar]
- [23].Horne R. The medication adherence report scale. University of Brighton; Brighton, UK: 2004. [Google Scholar]
- [24].King MF, Bruner GC. Social desirability bias: A neglected aspect of validity testing. Psychology and Marketing. 2000;17:79–103. [Google Scholar]
- [25].Margolis ML, Christie JD, Silvestri GA, Kaiser L, Santiago S, Hansen-Flaschen J. Racial differences pertaining to a belief about lung cancer surgery. Ann Intern Med. 2003;139:558–63. doi: 10.7326/0003-4819-139-7-200310070-00007. [DOI] [PubMed] [Google Scholar]
- [26].LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Med Care Res Rev. 2000;57:146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- [27].Bergkvist L, Rossiter JR. The predictive validity of multiple-item versus single item measures of the same constructs. Journal of Marketing Research. 2007;44:175–84. [Google Scholar]
- [28].Drolet AL, Morrison DG. Do we really need multiple-item measures in service research? Journal of Service Research. 2001;3:196–204. [Google Scholar]