Abstract
Background
Social support and coping strategies are important determinants of health, especially for those in the immigrant community adjusting to a new environment.
Purpose
This study assessed the buffering effects of perceived social support and different coping styles on cardiovascular reactivity to stress among Chinese immigrants in the New York City Chinatown area.
Method
Participants (N = 50, 76% women, and 22–84 years old) completed questionnaires assessing their perceived social support and coping strategy preferences. They were then asked to recall a stress provoking event related to their immigration experience in a semi-structured interview format.
Results
Hierarchical multiple regression analyses confirmed the interaction effect between perceived social support and problem-focused, emotion-focused, or reappraisal coping on heart rate reactivity. Additionally, Chinese immigrants who upheld more Chinese values were highly correlated with stronger perceived availability of social support and were more likely to incorporate the use of problem-focused and reappraisal coping styles.
Conclusion
Findings suggest that high level of social support and the use of reappraisal coping strategies were associated with attenuated cardiovascular responses to stress.
Keywords: Social support, Coping, Cardiovascular health, Chinese immigrants
Previous research has demonstrated that stress has an adverse effect on cardiovascular health (1). Cardiovascular reactivity to stress provocation is a hypothesized mechanism linking stress to cardiovascular health (2). Specifically, individuals showing an elevation in cardiovascular responses such as heart rate (HR), systolic blood pressure (SBP), and diastolic blood pressure (DBP), to stress provocation may be at higher risk for future development of coronary heart disease (CHD), than those exhibiting relatively smaller cardiovascular responses (3). Social support and certain coping strategies have been shown to moderate and attenuate the impact of stressors on well-being (4,5). Studies focusing on reactivity indicated that the presence of a supportive companion may attenuate cardiovascular responses to stress during provocation in the lab compared to a non-supportive condition (6). In terms of coping strategies, conflicting results have been reported with some studies showing that certain types of coping styles (e.g., problem focused coping and emotion focused coping) were associated with lower cardiovascular reactivity during stressful events, while other studies did not support this association (7–10).
Chinese Immigrants, Stress, and Cardiovascular Reactivity
According to the U.S. Census Bureau (11), the total Chinese-American population residing in the United States was more than 2 million. Within New York City itself, Chinese-Americans numbered almost 400,000, with 78% of them being foreign-born (12). These statistics are a conservative estimation of the Chinese population in the U.S. as they do not account for the number of illegal immigrants.
Immigration is a process that affects individuals in many ways, and is often considered to be intensely stressful (13). Difficulties experienced by Chinese immigrants include language barriers, adjusting to an unfamiliar environment, differences between Chinese and American cultures, and problems relating to children who are often more acculturated than their parents (14). They may also struggle to find meaningful work, experience problems communicating with mainstream society, and have issues negotiating the cultural conflicts emerging within their own home (14). Changes in lifestyle that frequently accompany immigration to a new society may have a direct and an indirect effect on health via added stress experienced. These changes, such as diet, have been found to increase vulnerability to developing cardiovascular disease (15,16).
Just a handful of studies have examined cardiovascular responses to stress among Asians or Asian Americans. Studies focusing on Asians, mostly conducted in Singapore, have demonstrated that Asians are a heterogeneous group in terms of their cardiovascular health. When comparing Indians and Chinese, researches have shown that Chinese participants had lower reactivity to stress and lower rates of CHD than Asian Indians (17,18). Another study focusing on Chinese women in Singapore found that social support schemas were associated with participants having lower cardiovascular reactivity to anger recall tasks (19). Overall, these studies suggested that Chinese tended to have lower cardiovascular disease risk than other Asian groups.
In terms of studies focusing on Asian Americans, most of these studies compared cardiovascular reactivity among Asian Americans with Caucasians (20,21). Results tended to demonstrate that Asian Americans appeared to have lower cardiovascular reaction to stress compared to Caucasians (21). However, cardiovascular disease (CVD) has been seen to be higher among Asian American Indians when compared to Caucasians (22). In general, the generalizablity of these studies may be restricted as their samples were very homogeneous with most of the studies focused on young and highly acculturated undergraduate students. Hence, the results of these cardiovascular reactivity studies discussed may not be generalizable to Chinese immigrants.
Coping Resources (Perceived Social Support)
Perceived social support is an important resource for coping with stress and may be a strong and reliable determinant of health outcomes (23–26). Perception of social support during times of stress may have a positive impact on health by helping alter perceptions of threat, lower anxiety, and increase coping ability. Additionally, cognitive aspects of social support may serve as a buffer, which may attenuate physiological reactivity to stress (25,27,28). Studies have found that when participants who knew that social support was available if needed engaged in a speech task showed lower HR, SBP, and DBP compared to participants who did not have access to support (29).
Among Chinese immigrants values of interdependence and collectivism which define Chinese cultural beliefs, prevent Chinese people from seeking support to cope with stress. This inability to access support reflects a reluctance to burden others with their personal needs, the possibility of losing face, and threat of ostracism from one’s own group (30). Consequently, first generation Chinese immigrants may be less likely to seek support from their family and friends compared to non-immigrants. Research has shown that both Asians living in Asia and Asian immigrants living in other countries are significantly less likely to report drawing on social support to cope with stress compared to European Americans (31). Hence, perceived social support in the first generation Chinese immigrant communities may not serve as a buffer that attenuates cardiovascular responses to stress.
Coping Styles
Coping styles refer to both strategies used to cope with a variety of stressors and individuals’ habitual preferences in coping with problems (32). Lazarus and Folkman (33) proposed that coping strategies could be categorized into two categories: problem-focused coping and emotion-focused coping. However, studies have found that conceptualizing coping into two categories was overly simplistic and led to inconsistencies (4,34,35). Other researchers such as Cox and Ferguson (36) identified four basic dimensions of coping: problem-focused coping (e.g., active coping, planning), reappraisal coping (positive reinterpretation, acceptance), emotion-focused coping (e.g., seeking emotional support, emotional venting), and avoidance coping (e.g., denial, mental and behavioral disengagement; 35).
Penley and his colleagues (37) conducted a meta-analysis to examine the association between different types of coping strategies and health outcomes. They conceptualized avoidance as a kind of emotion focused coping and reported that emotion-focused coping strategies including distancing oneself, self-control, accepting responsibility, wishful thinking, and avoidance had a significantly negative association with health outcomes. A positive association between problem-focused coping strategies (except confrontational coping) and overall health was found. Positive reappraisal was not significantly associated with physical health outcomes in their study.
Research relating coping strategies and cardiovascular reactivity to stress has been minimal. Studies have found that the use of both problem-focused and emotion-focused coping enhanced recovery from stress following provocation (7–9,38). Other studies have found either no associations between problem and emotion-focused coping and cardiovascular responses to stress or increased reactivity to stress or slowed recovery from stress with the use of problem and emotion-focused coping (9,10,39). Overall, there is confusion about the effect of coping mechanisms on cardiovascular responses to stress.
It is unknown which coping strategies would be more beneficial for Chinese immigrants’ cardiovascular health. Studies done on the Chinese national population samples showed the use of four types of coping styles: 1) mobilization of personal resources, 2) seeking help from social resources, 3) avoidance and doing nothing about the situation, and 4) appealing to a supernatural power (40,41). However, these coping strategies may not apply to a heterogeneous Chinese immigrant sample as Hwang’s (40) study focused on college students in Taiwan and Shek and Cheung’s (41) sample involved working parents in Hong Kong. Although data are scarce on the use of coping strategies and their impact on health among Chinese immigrants, problem-focused coping has been found to be beneficial for Korean immigrant participants (42). Additionally, according to Chinese cultures, since suffering is essential for developing one’s character (43), Chinese participants who were less acculturated would utilize more reappraisal coping strategies.
Research Aims and Hypothesis
The purpose of this study is to explore the relationships between perceived social support, coping styles, and cardiovascular reactivity to stress among Chinese immigrants. To date, the majority of studies of social support and coping strategies have been done with Caucasian Americans with only a few studies focused on other ethnicities. Although perceived social support and coping mechanisms are universal constructs, there is evidence for differences between cultures in the perception of social support and the choices of coping strategies that are available or acceptable (31,42,44). Since relatively little is known about Chinese immigrants’ perception of social support and their choice of coping styles, this study assessed the effects of perceived social support and coping strategies among New York City Chinese immigrants’ cardiovascular responses to stress provocation.
It was hypothesized that: 1) Participants who perceived themselves as having a. a greater level of social support and b. used more problem-focused, emotion-focused, and reappraisal coping were predicted to have smaller cardiovascular reactivity changes (i.e., SBP, DBP, and HR) in response to stress provocation compared to those individuals who perceived themselves as having a lower level of social support and used less of the above three coping strategies. 2) Participants who tended to uphold more Chinese values would be less likely to perceive availability of social support to cope with their stress than those who maintained less or no Chinese values. 3) Participants who were less acculturated to American culture would be more likely to use problem-focused coping and reappraisal coping to cope with stress than those who were more acculturated to American cultures.
Method
Participants
Participants included 50 (12 men, 38 women; age range = 24 – 84 years, M = 57.3 years) volunteers. They were drawn from a larger study at the New York Downtown Hospital located in Chinatown focusing on levels of acculturation, social status, eating habits, and cardiovascular health among Chinese immigrants. After the completion of the larger study, subjects were called and asked if they had an interest in participating in a study on stress and social support.
All participants were required to be Chinese and to have been born in China. Exclusion criteria were difficulty understanding the questionnaire, having a history of serious mental disorder, or having a serious, chronic disease that affected their behavior.
Table 1 presents the sample characteristics and participants’ health status.
Table 1.
Characteristic of Study Population (N=50)
| N | % | |
|---|---|---|
| Gender | ||
| Male | 12 | 24 |
| Female | 38 | 76 |
| Marital Status | ||
| Currently married | 33 | 66 |
| Never married | 5 | 10 |
| Separated | 4 | 8 |
| Widow | 8 | 16 |
| Preferences of Language Spoken | ||
| Chinese Only | 42 | 84 |
| English Only | 0 | 0 |
| Both | 8 | 16 |
| Level of Education | ||
| No school | 1 | 2 |
| Elementary school | 9 | 18 |
| High school | 18 | 36 |
| College or above | 22 | 44 |
| Employment status | ||
| Employed | 24 | 48 |
| Unemployed | 2 | 4 |
| Retired | 19 | 38 |
| Housewife | 5 | 10 |
| Annual Household Income | ||
| 0–9999 | 10 | 20 |
| 10000–19999 | 9 | 18 |
| 20000–29999 | 13 | 26 |
| 30000–49999 | 4 | 8 |
| 50000 or above | 13 | 26 |
| Not stated | 1 | 2 |
| BMI, kg/m2 | ||
| <18.5 | 1 | 2 |
| 18.5–24.9 | 34 | 68 |
| 25–29 | 13 | 26 |
| >30 | 2 | 4 |
| Waist Circumstances (inches) | ||
| Male | ||
| >40 | 2 | 4 |
| <40 | 10 | 20 |
| Female | ||
| >35 | 5 | 10 |
| <35 | 33 | 66 |
| History of Hypertension | ||
| Yes | 19 | 38 |
| No | 31 | 62 |
| Status of Smoking | ||
| Yes | 3 | 6 |
| No | 47 | 94 |
Procedures
The study personnel presented participants with a consent form and provided a detailed explanation of the study. Following consent, participants completed questionnaires assessing their level of perceived social support and coping strategies. Demographic data were also collected. After completion of the questionnaires, participants were attached to monitoring equipment that measured BP and HR and were requested to sit still and not talk during the adaptation period and the recovery period. During adaptation, the participants were monitored for 8 minutes at 2-minute intervals, thus obtaining four baseline measures of BP and HR. Following adaptation, a trained interviewer used the 8-minute Social Competence Interview to help the participants recall a stress-provoking incident related to their immigration experience that occurred within the past 6 months. Throughout the 8-minute interview, the participants were continuously monitored at 1-minute intervals, obtaining a total of eight readings. Recovery was monitored for 20 minutes following the interview at 2-minute intervals, obtaining 10 measures of BP and HR.
Participants did not receive any compensation for their involvement in this study. However, they received $40 and a physical check-up from the larger study. All data were kept in a locked filing cabinet within the research offices of the Principal Investigator.
The original questionnaire package was in English. Since a majority of the participants did not read English, the questionnaire package was translated into traditional Chinese characters. To ensure the accuracy of the translation, the questionnaire was then back-translated into English by another bilingual research assistant and compared with the original questionnaire. Discrepancies between the two translations were reconciled by discussion. The decision to read Chinese or English questions depended on the preference of the individual participant. The bilingual Chinese interviewer was trained to administer the interview in both English and Chinese.
Measures
Interpersonal Support Evaluation List (ISEL)
The ISEL (45) was used to assess the perceived availability of potential social support among the participants. The scale includes 40 items with half the items being positive statements and half the items being negative statements. Participants responded to questions on a 5-point Likert scale. The item scores were summed to obtain a total score, with higher scores indicating higher levels of social support. Chronbach’s alpha estimate for this study was .96.
Coping Orientations to Problems Experienced Scale (COPE)
The COPE inventory (35) was used to measure coping strategies. It contains 60 items and is answered on a four-point frequency scale, with higher scores indicating more use of a specific coping strategy. The measure has 14 subscales and all of them had alpha reliability coefficients ranging from .45 to .92 for each subscale. Based on Carver et al.’s (35) exploratory factor analysis of the COPE scale scores, four factors were produced. The first factor is composed of subscales Active Coping, Planning, and Suppression of Competing Activities. The second factor includes subscales Acceptance, Restraint Coping, and Positive Reinterpretation and Growth. The third factor consists of subscales Focus On and Venting of Emotion, Social Instrumental Support Seeking, and Social Emotional Support Seeking. The final factor includes subscales Denial and both Mental and Behavioral Disengagement. The four factors are similar to Cox and Ferguson’s (36) four basic dimensions of coping: problem-focused, reappraisal, emotion-focused, and avoidance. Scores for each factor can range from 12 to 48. In this sample, Chronbach’s alphas of subscales Problem-Focused Coping, Reappraisal, Emotion-Focused Coping, and Avoidance were .87, .78, .84, and .45 respectively.
Asian Value Scale (AVS)
The AVS (46) assessed the participants’ endorsement of Chinese values such as collectivism, following social norms, and humility. The scale consists of 36 statements on a scale from 1 (strongly disagree) to 7 (strongly agree) with a high score indicating upholding more Asian values. Chronbach’s alpha of .67 was found in this study.
Blood pressure and heart rate
The OMPRON HEM-780 Automatic Blood Pressure Monitor (OMRON Healthcare, Inc., Bannockburn, IL) was used to measure BP (including SBP and DBP) and HR using the participant’s non-dominant arm. This device uses the oscillometric method. The accuracy of the readings is ± 3mmHg or 2% of readings.
Social Competence Interview (SCI)
The SCI (47–49) is a semi-structured interview which is designed to measure a person’s cardiovascular responses while they are discussing personal stress or a recurring conflict with a sympathetic interviewer. Scoring of the interview was not reported here as it was not the focus of the study.
Data Reduction
Three cardiovascular measures were examined: SBP, DBP, and HR. Change scores were used as the cardiovascular dependent measure because they have long been recognized as an appropriate way of characterizing cardiovascular reactivity (50). Change scores were computed using the mean of the 8 readings taken during the interview subtracted from the mean of the 4 baseline measures. As recommended by Llabre and her colleagues (51), raw change scores were used.
Data Analysis
All analyses were performed using the SPSS 14.0 graduate student statistical package. Descriptive statistics focusing on demographic, perceived social support, coping strategies, and cardiovascular measures (BP and HR) were computed. To examine relationship between both demographic characteristics and health status (i.e., age, years in the U.S., height, weight, and BMI) and both BP and HR, correlational analyses were calculated. Independent sample t-tests were used to examine the effects of gender, history of hypertension, and smoking (if applicable) on reactivity changes. Analysis of variance was computed to examine the association between categorical variables (i.e., level of education and employment) and cardiovascular measures. Correlations were computed between level of acculturation, perceived social support, and coping styles.
Finally, moderation models were evaluated with hierarchical multiple regression. Interaction terms were measured by multiplying perceived social support and relevant coping strategies (i.e., problem-focused, emotion-focused, reappraisal, and avoidance). The models were computed to examine whether participants who had a high level of perceived social support and used more problem-focused, emotion-focused, and reappraisal coping strategies would predict smaller reactivity changes in results of SBP, DBP, and HR. This was compared to participants who had a low level of perceived social support and less use of the above coping strategies. With reactivity change scores as dependent variables, covariates (age, waist circumference, and the relevant baseline HR, SBP, and DBP) were included as the first step because they were significantly correlated with this study’s cardiovascular measures. As suggested by Aiken and West (52), the main effects (perceived social support, various coping strategies) were centered and entered in the second step, followed by the cross product term as the third step.
Results
Effects of Demographic Variables on Cardiovascular Measures
Table 2 presents the descriptive statistics (body composition and cardiovascular measures) of the sample. As can be seen in Table 3, demographic variables including waist circumference, age, and years residing in the U.S. were positively associated with baseline cardiovascular measures, but not cardiovascular reactivity change scores. Length of stay in the U.S. was positively correlated with baseline SBP, age was positively associated with baseline HR and SBP, and waist circumference was positively correlated with baseline SBP and DBP. Variables including gender, smoking status, history of hypertension, BMI, levels of education, and employment status were not significantly correlated with any cardiovascular measures.
Table 2.
Descriptive Statistics of Participants’ Body Composition and Cardiovascular Measures
| Participants Characteristics | M± SD | Range |
|---|---|---|
| Weight Circumferences (inches) | ||
| Male | 34.48±4.67 | 27–42 |
| Female | 31.41±3.07 | 26–41 |
| BMI (kg/m2) | 23.45±36 | 18.5–24.9 |
| Cardiovascular Parameters | ||
| Baseline SBP | 98.25±23.33 | 66–178.25 |
| Baseline DBP | 63.39±11.77 | 41.75–94.25 |
| Baseline HR | 68.18±20.91 | 42.75–139.25 |
| Reactivity SBP Change | 19.1±9.36 | |
| Reactivity DBP Change | 8.17±5.97 | |
| Reactivity HR Change | 19.31±18.30 | |
Table 3.
Participants’ Correlation between Demographic Variables, Coping and Social Support Variables, and Cardiovascular Measures
| Subscale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | .16 | .34** | .38** | −.03 | .04 | −.15 | .16 | −.08 | .30* | .32* | .22 | −.05 | −.14 | −.04 |
| 2. BMI | - | .83** | .04 | .02 | .09 | .05 | .15 | .17 | .26 | .14 | .21 | −.12 | −.15 | −.22 | |
| 3. Waist Circumferences | - | .19 | .10 | .08 | −.06 | .22 | .11 | .27 | .28* | .31* | −.21 | −.21 | −.00 | ||
| 4. Length in the US | - | .01 | .21 | .02 | .11 | −.05 | −.01 | .39** | .26 | −.04 | −.26 | −.04 | |||
| 5. Perceived Social Support | - | .48** | .54** | .75** | −.36* | .61** | .28 | .58** | −.74** | −.37** | .49** | ||||
| 6. Problem-Focused Coping | - | .72** | .69** | −.14 | .44** | .24 | .51** | −.51** | −.39** | .01 | |||||
| 7. Emotion-Focused Coping | - | .61** | .00 | .46** | −.11 | .20 | −.35* | −.11 | .11 | ||||||
| 8. Reappraisal Coping | - | −.07 | .54** | .39** | .59** | −.72** | −.45** | .27 | |||||||
| 9. Avoidant Coping | - | −.33* | −.03 | −.25 | .26 | .12 | −.07 | ||||||||
| 10. Baseline Heart Rate | - | −.01 | .43** | −.39** | −.25 | .10 | |||||||||
| 11. Baseline SBP | - | .80** | −.52** | −.56** | .29 | ||||||||||
| 12. Baseline DBP | - | −.63** | −.56** | .31* | |||||||||||
| 13. Heart Rate Reactivity | - | .68** | −.47** | ||||||||||||
| 14. Systolic BP Reactivity | - | −.05 | |||||||||||||
| 15. Diastolic BP Reactivity | - |
p < .05 level, two-tailed.
p < .05 level, two-tailed.
Moderation Effects of Perceived Social Support and Coping Strategies on Cardiovascular Reactivity Changes
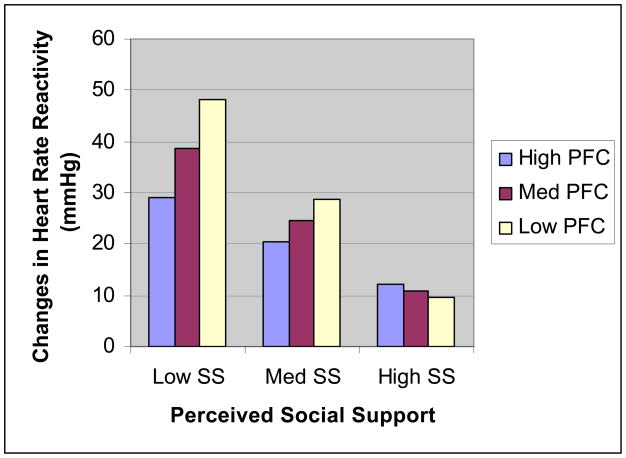
A series of hierarchical regressions were performed to understand whether the association between perceived social support and cardiovascular reactivity changes would be moderated by various coping strategies. First, significant main effects for perceived social support (β = −.94, t = −6.48, p < .001) and problem-focused coping (β = −.61, t = −2.24, p = .03) on HR reactivity changes were found. The interaction between perceived social support and problem-focused coping on HR reactivity changes was also significant (β = .04, R2 = .68, p < .01). To illustrate this interaction effect, high, medium, and low levels of social support groups were created (based on the mean and ±1 SD) and is depicted in Fig. 1. Results suggested that those who perceived low and moderate levels of social support availability and incorporated relatively more use of problem focused coping were predictive of smaller HR reactivity changes. However, those who perceived high levels of social support had larger HR reactivity changes if they tended to use more problem-focused coping. No significant main and interaction effects between perceived social support and problem-focused coping were found in analyses of SBP and DBP reactivity changes.
Figure 1.
Mean changes in heart rate reactivity as a function of perceived social support and problem-focused coping. PFC = problem-focused coping; SS = social support.
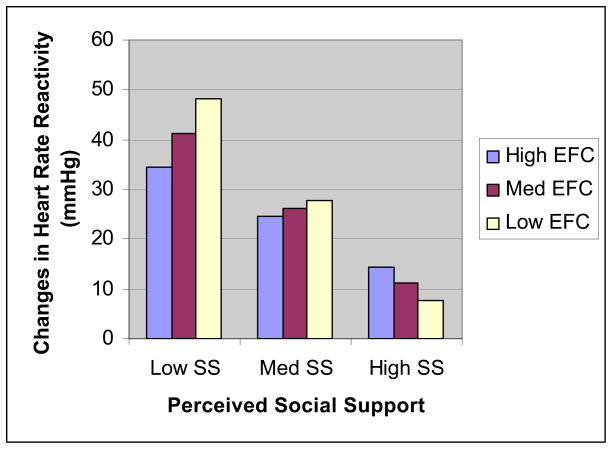
A simple effect of perceived social support was found in measures of HR reactivity changes (β = −.75, t = −6.48, p < .001). Additionally, a significant interaction between perceived social support and emotion-focused coping on HR reactivity changes (β = .03, t = 2.28, p < .03) was found. As depicted by Fig. 2, individuals who reported having low and moderate levels of perceived social support have lower HR reactivity changes if they utilize more emotion-focused coping. In contrast, those who had a high perceived availability of social support and tended to use more emotion-focused coping were predicted to have high HR reactivity changes. No significant result was found among SBP and DBP reactivity changes.
Figure 2.
Mean changes in heart rate reactivity as a function of perceived social support and emotion-focused coping. EFC = emotion-focused coping; SS = social support.
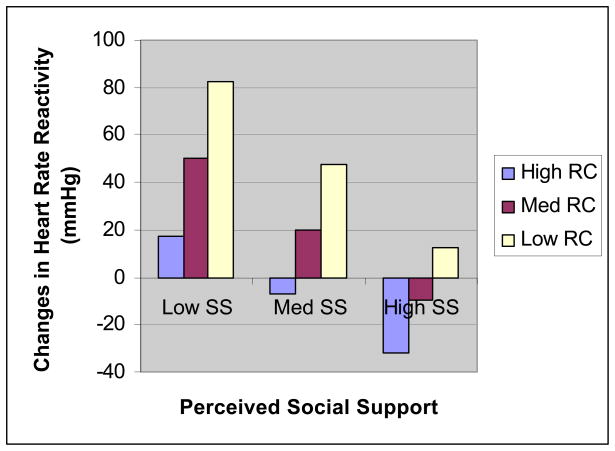
Perceived social support (β = −1.48, t = −3.58, p = .001) and reappraisal coping (β = −3.22, t = −3.21, p = .002) were negatively associated with HR reactivity changes. The interactive effect of perceived social support and reappraisal coping on HR reactivity changes was also significant (β = .03, t = 2.49, p < .02). Fig. 3 depicts this interaction term. The results revealed that individuals characterized by high perceived social support and more use of reappraisal coping had the smallest HR reactivity changes. No significant association was found for the interaction of perceived social support and reappraisal coping with SBP and DBP reactivity changes.
Figure 3.
Mean changes in heart rate reactivity as a function of perceived social support and reappraisal coping. RC = reappraisal coping; SS = social support.
Finally, no significant main and interaction effects were shown between perceived social support and avoidant coping on HR, SBP, and DBP reactivity changes.
Effects of Acculturation on Social Support, Problem-Focused and Reappraisal Coping Strategies
Participants who upheld more Chinese culture values were positively associated with stronger perceived availability of social support (r = .41, p < .005). Additionally, upholding more Chinese values was positively associated with the use of problem-focused coping (r = .40, p < .005) and reappraisal coping (r = .60, p < .001). No significant relationships between levels of acculturation and emotion-focused coping, and acculturation and avoidance coping were found.
Discussion
This study investigated whether perceived social support and the use of various kinds of coping strategies would predict smaller HR and BP reactivity changes among Chinese immigrants. Results indicated partial support for this hypothesis. Perceived social support and the use of problem-focused coping predicted HR reactivity changes. Problem-focused coping predicted smaller HR reactivity changes only among participants who perceived themselves as having low or moderate levels of social support. However, within the high perceived social support group, utilizing more problem-focused coping predicted larger HR reactivity changes.
Similarly, an interactive effect between social support and emotion-focused coping on HR reactivity changes was also indicated. Those who reported having low or medium levels of social support were revealed to have smaller HR reactivity changes if they also use emotion-focused coping. However, the use of emotion-focused coping among the high social support group predicted larger HR reactivity.
These results are counter-intuitive in that low and medium social support predicted the successful use of problem-focused and emotion-focused coping strategies and a lower cardiovascular response to stress. These results can be understood in the context of Chinese culture which emphasizes family interdependence, importance of maintaining a harmonious relationship, and a fear losing face and bringing shame to the family. Hence within the Chinese culture expression of stress and emotion is frequently inhibited for fear of burdening one’s loved ones (53). Hence, people who do not have the perception of having support can focus on the coping strategies that they use rather than focusing on the impact of their problems and coping strategies on their social circle. In essence, within the Chinese culture, the support and coping strategies that support providers suggest could be an added burden for individuals and interfere with their ability to cope with stress. Perceived social support when viewed within this perspective might actually contribute to enhanced anxiety and distress as evidenced in increased heart rates among participates who reported high levels of perceived social support.
Results also indicated that reappraisal coping was predictive of less marked changes in HR reactivity, regardless of the levels of social support. Chinese culture emphasizes the importance of endurance, suffering, and fatalism, which in turn leads to viewing a stressful situation in a more positive light (40,54). Hence, reappraisal coping, which comprises of cognitive adaptation rather than behavioral coping has been found to be an effective and culturally-appropriate coping mechanism for the Chinese culture. Additionally, since reappraisal coping does not require help from others, it could minimize the anxiety in individuals that they would be burdening others. Reappraisal coping may be cardio-protective within the Chinese immigrant during periods of stress.
Despite our expectations, the results of this study did not support our second hypothesis that those who upheld more Chinese values would perceive less availability of social support to cope with their stress compared to those who perceived themselves as less Chinese. We found that upholding more Chinese values was positively associated with stronger perceived availability of social support. The results of this study contradict a previous study focusing on college students in California which shown that Asian Americans from a more collectivistic culture sought social support less and found support to be less effective than European Americans from a more individualistic culture (55). This study did not yield a similar result, possibly because Kim et al.’s (55) study focused on social support seeking rather than perceived social support. Seeking support is a behavioral dimension indicating active effort. Perceived support implies the perception of already existing support. Another reason for the differences between the two studies could be that our study sample comprised of first generation Chinese immigrants and did not compare Chinese immigrants with the dominant society and subsequent generations. In our sample, a majority of the participants either lived in or were affiliated with the Chinese community (e.g., Chinatown) and did not speak fluent English. It is possible that among Chinese immigrants who are strongly entrenched within the Chinese community, there is a greater need for support in order to adapt to life in the U.S. compared to Chinese immigrants that affiliate more with the dominant culture. Immigrants entrenched within the Chinese community need support to deal with multiple aspects of their lives such as seeking training and finding jobs and overcome problems relating to language barriers and generational differences. Without support, Chinese-speaking immigrants may not be able to sustain their basic needs as the cultural and language differences contrasted greatly from their country of origin. In this case, their perceived availability of social support may be an indicator of their network size and their relationship within the local Chinese community.
Additionally, in a recent review, Kim, Sherman, and Taylor (56) proposed distinguishing social support as explicit and implicit because cultural differences impact the use of social support. Explicit support refers to the elicitation and receipt of advice, emotional comfort, and instrumental help from others (behavioral aspects of social support). This is based more on a Western model of social support (56). Implicit support means the comfort that individuals obtain either from reminding oneself that one is close to others (cognitive aspect of social support) or having the company of a close one without talking about the problems or stressors (57). Based on one of their studies, they found that implicit support is more psychologically and physiologically beneficial for Asians and Asian Americans than Caucasians (57). Similarly, perceived emotional support was found to be beneficial among Asians in Asia (e.g., Japanese and Filipinos) as well as those among collectivistic cultures (e.g., Hispanic; 58, 59). It appears that the cognitive aspect of social support could be more helpful for Asian Americans such as Chinese immigrants as they can still have support from others without worrying about burdening their close ones and experiencing the danger of losing face, which may serve as a buffer that attenuates cardiovascular responses to stress.
For our final hypothesis, as expected, a low level of acculturation to the dominant culture was found to be positively associated with a higher use of problem-focused coping and reappraisal coping styles. The use of reappraisal coping was consistent with Chinese traditional beliefs and philosophies. Chinese culture values individuals who are reserved and individuals’ abilities to endure suffering. Within Chinese culture, suffering is essential to develop self-restraint, develop character, and to understand the underlying spiritual reasons for facing problems or experiencing stress (43). Additionally, Morling and Evered found that those who were from collectivistic cultures were more likely to cope through adjusting the self and accepting the environment (also known as secondary control; 60). It may be the case that Chinese immigrants who uphold stronger Chinese values and philosophies would also be more likely to use a reappraisal coping style to cope with stress.
Limitation of the Study
It should be noted that this study had several limitations. First, the sample size of this study was small and largely made-up of women. Studies in the past have shown that there have been gender differences in both the types of coping strategies utilized and the association between social support and cardiovascular reactivity to stress (28,61,62). It is possible that if the sample had more male participants, the results would have been different. Second, the age range of our sample was large and we did not have information for when participants migrated to the United States. Therefore, the stress provocations of participants could have been highly varied. Third, our sample was also somewhat biased as this study recruited participants from a larger study, which comprised of first generation Chinese immigrants from Chinatown and participants affiliated or related with the local Chinese community. As such, the study may over-represent participants who are less acculturated to the dominant culture who tend to be more active in their community. Furthermore, the majority of our sample only spoke Chinese and was strongly affiliated with the Chinese community. Therefore, the results of this study may not be generalizable to Chinese immigrants who are fluent in English and are less affiliated with their local Chinese communities. Thus, the results of this study should be viewed with caution in terms of their generalizability.
Another, limitation may be the low reliability of the avoidance coping subscale Avoidance coping was not significantly associated with either support or reactivity. In the future, studies should utilize other coping scales such as the Cross-Cultural Coping Scale, which has a better internal consistency (63). Finally, level of acculturation was only based on the cognitive aspect of acculturation (an individual’s values) and was measured as a unidimensional rather than a multidimensional construct. It is not known how other aspects of acculturation (i.e., behavior) would affect Chinese immigrants’ perceived social support and their utilization of various types of coping strategies. A measure of acculturation based on Berry’s acculturation model (64) should be used in the future with multiple dimensions.
Finally, research has indicated that cardiovascular hyporesponsiveness could occur (lowered HR, BP, and heart rate variability and heightening of baseline cardiovascular measures) when participants are chronically fatigued and distressed (65). However, since our study did not measure participants’ subjective levels of stress, it is unknown whether cardiovascular hyporesponsiveness may have impacted our findings.
Implications and Future Direction
The findings of this study may have important implications for developing more studies focused on Asian immigrants’ cardiovascular health. In the past and even today, stereotypes of Asian Americans as a “model minority” may have caused researchers to overlook health and social issues in the community. The Asian American community is perceived as successful in many ways despite the many barriers immigrants generally confront when they first come to the United States (66). Additionally, a majority of the studies on Asian Americans have found that compared to all other ethnic minorities, Asian Americans tended to have low cardiovascular reactivity, morbidity, and mortality rates (21, 22). However, based on this study, which focused on Chinese immigrants with minimal or no understanding of English, the study indicated that first generation Chinese immigrants might have a higher cardiovascular disease risk as one-third of the participants had already had hypertension and several participants had high BMI and large waist circumferences. These variables were rarely present in past studies as they focused primarily on college students or those who had already acculturated to mainstream American society. Another implication of this study is that while comparative studies have shown that Asian Americans tend not to seek social support compared to other ethnicities (55), this study had shown that for those Chinese immigrants who still uphold strong Chinese values, having strong perceived availability of social support, and using more reappraisal coping are helpful for them to cope with stress. These coping methods are beneficial to their cardiovascular health.
Future studies examining social support should also focus on structural support (i.e., the quantitative aspect of social relationship). This study assessed the qualitative aspects of social support. In order to provide a more comprehensive analysis of social support, structural support should also be included, especially because prior studies have found that the size of a social network was positively correlated with lowering cardiovascular reactivity (67). Second, this study only examined one kind of coping resource (i.e., social support). Future studies should also consider other resources such as age/experience, education, and financial assets. Previous studies have found that personal attributes are also related to an individual’s adjustment to distress (23). Third, the interaction of personality traits such as hostility and agreeableness with social support and coping strategies for Chinese immigrants should also be examined. Research has already indicated that personality traits may have an interactive effect on cardiovascular reactivity. For instance, Chen and his colleagues (68) showed that there was an interactive effect of hostility and perceived social support on SBP and DBP reactivity. Lepore (69) also found that while individuals with low cynicism showed reduced reactivity to a speech stressor in the presence of a confederate, this significant result did not apply to those with high cynicism. Because no cardiovascular reactivity research has focused on the interactive effect between personality traits and coping strategies among Asians and Asian Americans, it would be worthwhile to further understand this aspect. Because of cultural differences, personality traits may have a differential effect on social support and coping strategies among Chinese immigrants. Finally, based on the results of this study, developing social support and coping intervention for Chinese immigrants may be beneficial. Future studies should examine how culturally sensitive social support and coping interventions impact Chinese immigrants’ health.
Conclusion
This study examined perceived social support, coping strategies, and cardiovascular reactivity to stress among Chinese immigrants in the New York City Chinatown area. Results of this study suggest that having moderate social support and the use of reappraisal coping strategies impacted Chinese immigrants’ cardiovascular responses to stress positively. For practical purposes, the results also suggest that culturally sensitive stress management training, which places an emphasis on cognitive reconstruction, would be very beneficial. This is especially true for Chinese immigrants who are less acculturated to U.S. culture.
Contributor Information
Christine Lee, Ferkauf Graduate School of Psychology/ Albert Einstein College of Medicine, Yeshiva University.
Sonia Suchday, Ferkauf Graduate School of Psychology/ Albert Einstein College of Medicine, Yeshiva University.
Judith Wylie-Rosett, Department of Epidemiology and Population Health, Albert Einstein College of Medicine, Yeshiva University.
References
- 1.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51(13):1237–1246. doi: 10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom Med. 2003;65(1):46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Manuck SB. Cardiovascular reactivity in cardiovascular disease: “Once more unto the breach”. Int J Beh Med. 1994;1(1):4–31. doi: 10.1207/s15327558ijbm0101_2. [DOI] [PubMed] [Google Scholar]
- 4.Ingledew DK, Hardy L, Cooper CL. Do resources bolster coping and does coping buffer stress? An organizational study with longitudinal aspect and control for negative affectivity. J Occup Health Psychol. 1997;2(2):118–133. doi: 10.1037//1076-8998.2.2.118. [DOI] [PubMed] [Google Scholar]
- 5.Tan M. Social support and coping in Turkish patients with cancer. Cancer Nurs. 2007;30(6):498–504. doi: 10.1097/01.NCC.0000300158.60273.ba. [DOI] [PubMed] [Google Scholar]
- 6.Kamarck TW, Manuck SB, Jennings JR. Social support reduces cardiovascular reactivity to psychological challenge: A laboratory model. Psychosom Med. 1990;52(1):42–58. doi: 10.1097/00006842-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Clark R, Adams JH, Clark VR. Effects of John Henryism and anger-coping on mean arterial pressure changes in African American women. Int J Behav Med. 2001;8(4):270–281. [Google Scholar]
- 8.Clark R, Anderson NB. Efficacy of racism-specific coping styles as predictors of cardiovascular functioning. Ethn Dis. 2001;11(3):286–295. [PubMed] [Google Scholar]
- 9.Hahn WK, Brooks JA, Hartsough DM. Self-disclosure and coping styles in men with cardiovascular reactivity. Res Nurs Health. 1993;16(4):275–282. doi: 10.1002/nur.4770160406. [DOI] [PubMed] [Google Scholar]
- 10.Vitaliano PP, Russo J, Paulsen VM, Bailey SL. Cardiovascular recovery from laboratory stress: Biopsychosocial concomitants in older adults. J Psychosom Res. 1995;39(3):361–377. doi: 10.1016/0022-3999(94)00144-t. [DOI] [PubMed] [Google Scholar]
- 11.US Census Bureau. 2000 New York City Housing and Vacancy Survey. [homepage on the Internet] Washington, DC: [updated 2009 Sept 11; cited 2010 Mar 10]. Available from: http://factfinder.census.gov/servlet/DatasetMainPageServlet?lang=en. [Google Scholar]
- 12.Barnes JS, Bennet CE. Census 2000 Brief. [homepage on the Internet] Washington, DC: The Asian Population: 2000. [cited 2010 Mar 10]. Available from : http://www.census.gov/prod/2002pubs/c2kbr01-16.pdf. [Google Scholar]
- 13.Yakhnich L. Immigration as a multiple-stressor situation: Stress and coping among immigrants from the former Soviet Union in Israel. International Journal of Stress Management. 2008;15(3):252–268. [Google Scholar]
- 14.Yee BWK, Huang LN, Lew A. Handbook of Asian American psychology. Thousand Oaks, CA, US: Sage Publications, Inc; 1998. Families: Life-span socialization in a cultural context; pp. 83–135. [Google Scholar]
- 15.Anand SS, Bennet CE. Ethnicity and cardiovascular disease. In: Yusuf S, editor. Evidence based cardiology. London: BMJ; 1998. pp. 329–352. [Google Scholar]
- 16.Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S. Cardiovacular and cancer mortality among Canadians of European, South Asian, and Chinese origin from 1979 to 1993: an analysis of 1.2 million death. CMAJ. 1999;161(2):132–138. [PMC free article] [PubMed] [Google Scholar]
- 17.Bishop GD, Robinson G. Anger, harassment, and cardiovascular reactivity among Chinese and Indian men in Singapore. Psychosom Med. 2000;62(5):684–692. doi: 10.1097/00006842-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Why YP, Bishop GD, Tong EMW, Diong SM, Enkelmann HC, Khader M, et al. Cardiovascular reactivity of Singaporean male police officers as a function of task, ethnicity and hostility. International Journal of Psychophysiology. 2003;49(2):99–110. doi: 10.1016/s0167-8760(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 19.Ratnasingam P, Bishop GD. Social support schemas, trait anger, and cardiovascular responses. International Journal of Psychophysiology. 2007;63(3):308–316. doi: 10.1016/j.ijpsycho.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Enkelmann HC, Bishop GD, Tong EMW, Diong SM, Why YP, Khader M, et al. The relationship of hostility, negative affect and ethnicity to cardiovascular responses: An ambulatory study in Singapore. International Journal of Psychophysiology. 2005;56(2):185–197. doi: 10.1016/j.ijpsycho.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Shen B, Stroud LR, Niaura R. Ethnic Differences in Cardiovascular Responses to Laboratory Stress: A Comparison Between Asian and White Americans. Int J Behav Med. 2004;11(3):181–186. doi: 10.1207/s15327558ijbm1103_7. [DOI] [PubMed] [Google Scholar]
- 22.Stoney CM, Hughes JW, Kuntz KK, West SG, Thornton LM. Cardiovascular stress responses among Asian Indian and European American women and men. Annals of Behavioral Medicine. 2002;24(2):113–121. doi: 10.1207/S15324796ABM2402_08. [DOI] [PubMed] [Google Scholar]
- 23.Gilbar O. Breast Cancer: How Do Israeli Women Cope? A Cross-Sectional Sample. Families, Systems, & Health. 2005;23(2):161–171. [Google Scholar]
- 24.Pakenham KI. Adjustment to multiple sclerosis: Application of a stress and coping model. Health Psychology. 1999;18(4):383–392. doi: 10.1037//0278-6133.18.4.383. [DOI] [PubMed] [Google Scholar]
- 25.Pierce T, Baldwin MW, Lydon JE. Sourcebook of social support and personality. New York, NY, US: Plenum Press; 1997. A relational schema approach to social support; pp. 19–47. [Google Scholar]
- 26.Helgeson VS. Two important distinctions in social support: Kind of support and perceived versus received. J Appl Soc Psychol. 1993;23(10):825–845. [Google Scholar]
- 27.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 28.Hughes BM. Research on psychometrically evaluated social support and cardiovascular reactivity to stress: Accumulated findings and implications. Studia Psychologica. 2002;44(4):311–326. [Google Scholar]
- 29.Uchino BN, Garvey TG. The availability of social support reduces cardiovascular reactivity to acute psychological stress. J Beh Med. 1997;20(1):15–27. doi: 10.1023/a:1025583012283. [DOI] [PubMed] [Google Scholar]
- 30.Sue D, Mak WS, Sue DW. Handbook of Asian American psychology. Thousand Oaks, CA, US: Sage Publications, Inc; 1998. Ethnic identity; pp. 289–323. [Google Scholar]
- 31.Taylor SE, Sherman DK, Kim HS, Jarcho J, Takagi K, Dunagan MS. Culture and Social Support: Who Seeks It and Why? J Pers Soc Psychol. 2004;87(3):354–362. doi: 10.1037/0022-3514.87.3.354. [DOI] [PubMed] [Google Scholar]
- 32.Sandler IN, Wolchik SA, MacKinnon D, Ayers TS, Roosa MW. Handbook of children’s coping: Linking theory and intervention. New York, NY, US: Plenum Press; 1997. Developing linkages between theory and intervention in stress and coping processes; pp. 3–40. [Google Scholar]
- 33.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- 34.Aldwin CM, Revenson TA. Does coping help? A reexamination of the relation between coping and mental health. J Pers Soc Psychol. 1987;53(2):337–348. doi: 10.1037//0022-3514.53.2.337. [DOI] [PubMed] [Google Scholar]
- 35.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 36.Cox T, Ferguson E. Personality and stress: Individual differences in the stress process. Oxford, England: John Wiley & Sons; 1991. Individual differences, stress and coping; pp. 7–30. [Google Scholar]
- 37.Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. J Behav Med. 2002;25(6):551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- 38.Fontana A, McLaughlin M. Coping and appraisal of daily stressors predict heart rate and blood pressure levels in young women. Behavioral Medicine. 1998;24(1):5–16. doi: 10.1080/08964289809596376. [DOI] [PubMed] [Google Scholar]
- 39.Vitaliano PP, Russo J, Bailey SL, Young HM, et al. Psychosocial factors associated with cardiovascular reactivity in older adults. Psychosom Med. 1993;55(2):164–177. doi: 10.1097/00006842-199303000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Hwang K. Coping with residential crowding in a Chinese urban society: The interplay of high-density dwelling and interpersonal values. Acta Psychologica Taiwanica. 1979;21(2):117–133. [Google Scholar]
- 41.Shek DT, Cheung C. Locus of coping in a sample of Chinese working parents: Reliance on self or seeking help from others. Social Behavior and Personality. 1990;18(2):327–345. [Google Scholar]
- 42.Akiyama H, Antonucci TC, Campbell R. Rules of social support exchange: The U.S. and Japan. Asian American Psychological Association Journal. 1987;12(1):34–37. [Google Scholar]
- 43.Wong PTP, Ujimoto KV. Handbook of Asian American psychology. Thousand Oaks, CA, US: Sage Publications, Inc; 1998. The elderly: Their stress, coping, and mental health; pp. 165–209. [Google Scholar]
- 44.Yoshihama M. Battered women’s coping strategies and psychological distress: Differences by immigration status. Am J Community Psychol. 2002;30(3):429–452. doi: 10.1023/A:1015393204820. [DOI] [PubMed] [Google Scholar]
- 45.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social support: theory, research, and application. The Hague, Holland: Martinus Nijhoff; 1983. pp. 73–94. [Google Scholar]
- 46.Kim BSK, Atkinson DR, Yang PH. The Asian Values Scale: Development, factor analysis, validation, and reliability. Journal of Counseling Psychology. 1999;46(3):342–352. [Google Scholar]
- 47.Ewart CK, Ditmar MM, Suchday S, Sonnega JR. Instruction manual for the Social Competence Interview. Syracuse University; 2006. [Google Scholar]
- 48.Ewart CK, Jorgensen RS, Schroder KE, Suchday S, Sherwood A. Vigilance to a persisting personal threat: Unmasking cardiovascular consequences in adolescents with the Social Competence Interview. Psychophysiology. 2004;41(5):799–804. doi: 10.1111/j.1469-8986.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- 49.Ewart CK, Kolodner KB. Social Competence Interview for assessing physiological reactivity in adolescents. Psychosom Med. 1991;53(3):289–304. doi: 10.1097/00006842-199105000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Pickering TG. Challenge response predictors. General principles. Am J Hypertens. 1991;4(6):611–614. doi: 10.1093/ajh/4.11s.611s. [DOI] [PubMed] [Google Scholar]
- 51.Llabre MM, Spitzer SB, Saab PG, Ironson GH, et al. The reliability and specificity of delta versus residualized change as measures of cardiovascular reactivity to behavioral challenges. Psychophysiology. 1991;28(6):701–711. doi: 10.1111/j.1469-8986.1991.tb01017.x. [DOI] [PubMed] [Google Scholar]
- 52.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications, Inc; 1991. [Google Scholar]
- 53.Abe-Kim J, Takeuchi D, Hwang W. Predictors of help seeking for emotional distress among Chinese Americans: Family matters. J Consult Clin Psychol. 2002;70(5):1186–1190. [PubMed] [Google Scholar]
- 54.Mok E, Lai C, Zhang Z. Coping with chronic renal failure in Hong Kong. Int J Nurs Stud. 2004;41(2):205–213. doi: 10.1016/j.ijnurstu.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 55.Kim HS, Sherman DK, Ko D, Taylor SE. Pursuit of Comfort and Pursuit of Harmony: Culture, Relationships, and Social Support Seeking. Person Soc Psychol Bull. 2006;32(12):1595–1607. doi: 10.1177/0146167206291991. [DOI] [PubMed] [Google Scholar]
- 56.Kim HS, Sherman DK, Taylor SE. Culture and social support. Am Psychologist. 2008;63(6):518–526. doi: 10.1037/0003-066X. [DOI] [PubMed] [Google Scholar]
- 57.Taylor SE, Welch W, Kim HS, Sherman DK. Cultural differences in the impact of social support on psychological and biological stress responses. Psychological Science. 2007;18(9):831–837. doi: 10.1111/j.1467-9280.2007.01987.x. [DOI] [PubMed] [Google Scholar]
- 58.Campos B, Dunkel Schetter C, Abdou C, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: Positive implications for pregnant Latinas. Cultural Diversity and Ethnic Minority Psychology. 2008;14(2):155–162. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Uchida Y, Kitayama S, Mesquita B, Reyes JAS, Morling B. Is perceived emotional support beneficial? Well-being and health in independent and interdependent cultures. Personality and Social Psychology Bulletin. 2008;34(6):741–754. doi: 10.1177/0146167208315157. [DOI] [PubMed] [Google Scholar]
- 60.Morling B, Evered S. Secondary control reviewed and defined. Psychological Bulletin. 2006;132(2):269–296. doi: 10.1037/0033-2909.132.2.269. [DOI] [PubMed] [Google Scholar]
- 61.Glynn LM, Christenfeld N, Gerin W. Gender, social support, and cardiovascular responses to stress. Psychosom Med. 1999;61(2):234–242. doi: 10.1097/00006842-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 62.Hughes BM. Social support in ordinary life and laboratory measures of cardiovascular reactivity: Gender differences in habituation-sensitization. Annals of Behavioral Medicine. 2007;34(2):166–176. doi: 10.1007/BF02872671. [DOI] [PubMed] [Google Scholar]
- 63.Kuo BCH, Roysircar G, Newby-Clark IR. Development of the Cross-cultural Coping Scale: Collective, avoidance, and engagement coping. Measurement and Evaluation in Counseling and Development. 2006;39(3):161–181. [Google Scholar]
- 64.Berry JW. Acculturation: Advances in theory, measurement, and applied research. Washington, DC, US: American Psychological Association; 2003. Conceptual approaches to acculturation; pp. 17–37. [Google Scholar]
- 65.LaManca JJ, Peckerman A, Sisto SA, DeLuca J, Cook S, Natelson BH. Cardiovascular responses of women with chronic fatigue syndrome to stressful cognitive testing before and after strenuous exercise. Psychosomatic Medicine. 2001;63(5):756–764. doi: 10.1097/00006842-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 66.Young K, Takeuchi DT. Handbook of Asian American psychology. Thousand Oaks, CA, US: Sage Publications, Inc; 1998. Racism; pp. 401–432. [Google Scholar]
- 67.Roy MP, Steptoe A, Kirschbaum C. Life events and social support as moderators of individual differences in cardiovascular and cortisol reactivity. J Pers Soc Psychol. 1998;75(5):1273–1281. doi: 10.1037//0022-3514.75.5.1273. [DOI] [PubMed] [Google Scholar]
- 68.Chen YY, Gilligan S, Coups EJ, Contrada RJ. Hostility and Perceived Social Support: Interactive Effects on Cardiovascular Reactivity to Laboratory Stressors. Annals of Behavioral Medicine. 2005;29(1):37–43. doi: 10.1207/s15324796abm2901_6. [DOI] [PubMed] [Google Scholar]
- 69.Lepore SJ. Cynicism, social support, and cardiovascular reactivity. Health Psychology. 1995;14(3):210–216. doi: 10.1037//0278-6133.14.3.210. [DOI] [PubMed] [Google Scholar]