Abstract
Moca is a cell phone-facilitated clinical information system to improve diagnostic, screening and therapeutic capabilities in remote resource-poor settings. The software allows transmission of any medical file, whether a photo, x-ray, audio or video file, through a cell phone to (1) a central server for archiving and incorporation into an electronic medical record (to facilitate longitudinal care, quality control, and data mining), and (2) a remote specialist for real-time decision support (to leverage expertise). The open source software is designed as an end-to-end clinical information system that seamlessly connects health care workers to medical professionals. It is integrated with OpenMRS, an existing open source medical records system commonly used in developing countries.
Keywords: developing nations, health care, information and communication technology, mobile communication
Introduction
Over the last five years, the usage of mobile phones has exploded globally so that almost 90% of humans live within range of cellphone transmitter and more than 6 billion cellphones have been sold globally. This consumer-driven demand has led to two important societal changes; 1) almost everyone can afford a hand-held computer and communication device, which is backed by an extensive global supply infrastructure, and 2) almost everyone is familiar with the capabilities and user interface of cellphones. As device-convergence accelerates, it is becoming increasing clear than clinicians and patients alike are demanding a single device for entering and retrieving data, monitoring their surroundings, authentication, identification, labeling and communicating.
The use of cell phones to facilitate both real-time and store-and-forward medical consultation is an established tool for delivering specialty care, most notably dermatology and wound care [1–3]. In a review of the teledermatology literature, Whited reported that the agreement rate between clinic-based dermatologists and store-and-forward tele-dermatologists averaged 80% but can approach almost 95% [4]. Additional reports found that cell phone cameras can provide off site surgeons with images that can effectively be used to determine surgical care [5–6].
Outside of the novelty of a growing technology, there are many cultural and infrastructural reasons to adopt the cell phone as a vehicle to improve health care. One of the largest problems with health care delivery in developing countries, apart from lack of expert decision support and expert domain knowledge concerning equipment use, is the lack of a strong supply chain for delivering both equipment [7] and information [8]. Conventional medical equipment, often donated through benevolent intentions, can rapidly end up on the shelf because simple parts that break are not rapidly available [7]. Furthermore, transmission of timely information, even when mediated through modern channels such as email, is highly dependent on human intervention to transfer the data and add key information such as patient identifiers, history and diagnosis [8].
Two key advantages of using a cellular phone infrastructure to provide medical care are: rapidity of automated information transmission, and an established hardware supply chain. Moreover, since the cell phone is increasingly the major technology to facilitate communication, a human imperative, users make extra-ordinary strides to ensure this hardware is maintained and functioning on a daily basis. Finally, the average cellphone comes equipped with an increasing number of sensors and peripherals that allow for augmented medical data collection, including accelerometers for activity, cameras for analyzing and recording changes in skin lesions, pallor, wounds etc., voice recorders for note dictation or pain analysis (through stress tones), RFID or barcode readers, and of course WiFi/GPRS connections for interfacing with databases.
The software
Moca is an open-source remote medical diagnostics platform for health workers in developing nations. It is an end-to-end system that seamlessly connects health workers to medical professionals. Moca is integrated with OpenMRS, an existing open source medical records system commonly used in developing world health care. The goal is to provide a scalable, flexible technology to NGOs and social entrepreneurs to scale models of mobile tele-health.
Using mobile technologies for tele-health in developing nations requires dealing with many standards, different networks and local challenges ranging from intermittent connectivity and cultural differences. Our system provides an instant end-to-end infrastructure for media-centric remote diagnosis by experts that can be located anywhere in the world. Packetization, a synchronization model, and multi-modal data transport allow Moca to operate even in poor cellular coverage areas. While the system is mobile-centric, it is designed to provide alternatives such as WiFi and tethered uploads for bandwidth-constrained situations.
Moca also realizes that few instantiations of remote medical diagnostics are the same. Unlike hodge-podge solutions, Moca is highly customizable, allowing organizations to create their own workflows. These workflows can be dynamically loaded onto phones running Moca, and they can be shared between other organizations. Moca is committed to the Open Source concept. Its platform is released under the GNU GPL, allowing people to extend, improve, and tweak the system as they choose. We strongly believe that the best way to innovate is through open innovation, allowing organizations, universities, and companies to contribute to Moca.
Finally, user interface is crucial, that’s why the Moca interface has been laboriously engineered for ease-of-use and clarity. By leveraging Google Android’s API, Moca offers a highly usable and inviting interface.
The technology
Moca is a standard-focused open-source system that supports audio, images, location-based data, text, and in the future, video. Moca’s front-end for data and media capture is accessible through a fully programmable workflow interface. The back-end provides an intuitive user interface for management of medical media. Moca was built to be integrated with OpenMRS and other commonly used medical record systems for portability. The system infrastructure and design allows for modularity and interoperation.
Some of the other key features provided include:
Built-in training and workflow solution at the mobile device level can be used to train local nurses and health workers.
Open source foundation to encourage re-use of the solutions being developed.
Expert-labeled database that contains quality auditing and cost controls, rapid search and review, and a training set for (future) automated artificial intelligence (A.I.) classification of images, audio and video.
Software is downloaded to the phone so decision support is available even when connection is poor or non-existent.
Data transfer is algorithmically controlled to ensure reliable uploads even in poor coverage areas.
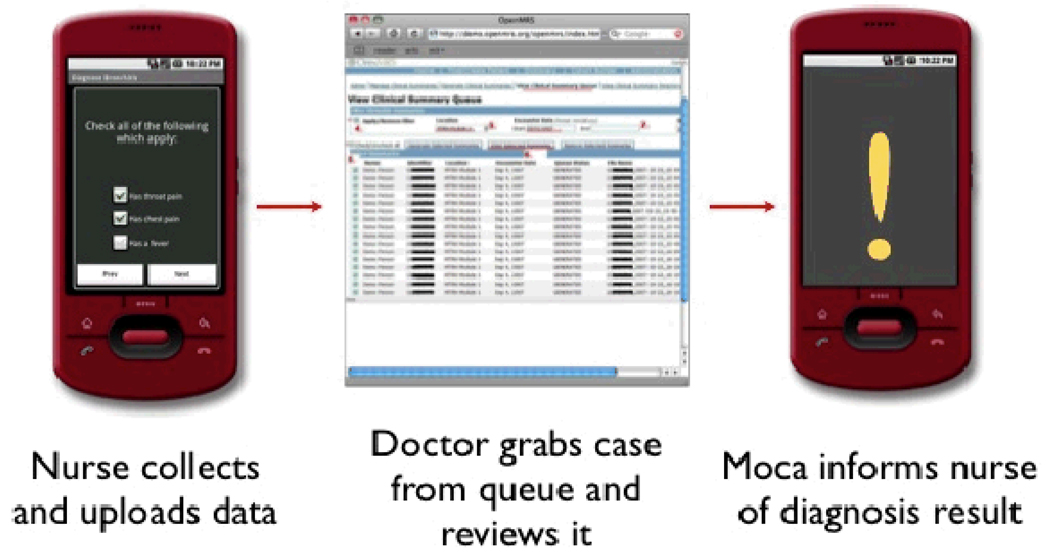
Using the Moca application, health workers can run a procedure and collect patient data. Moca then uploads the information to OpenMRS for a doctor to review. After reviewing the case, the doctors can notify the health worker of the diagnosis by sending results to the Moca application (Figure 1).
Figure 1.
Moca Workflow
Clinicians have the ability to build unique procedures for health care workers and organizations to use. Procedures are at the very core of Moca. They are step-by-step workflows. In most scenarios, a procedure is a set of pages that each have questions or prompts. Sometimes a page will prompt a user to take a picture or record audio. Other pages in a procedure may ask the user to enter text, or check boxes.
Procedures in Moca are defined in an extremely compact XML format. While it is easy to write a procedure in our procedure format, we plan on developing graphical tools to define procedures in the future. In the future, we also plan on integrating an X-Forms implementation standardized by OpenROSA. This will allow greater interoperability.
In addition to containing pages with question/response pairs, a procedure has the ability to branch. Branching is defined in the Procedure XML, and allows for any arbitrary logic to be performed on other previously answered questions. This extremely powerful feature can be used to do everything from not asking certain questions if they are not relevant given prior responses, to allowing physicians to create complete decision tree diagnosis utilities.
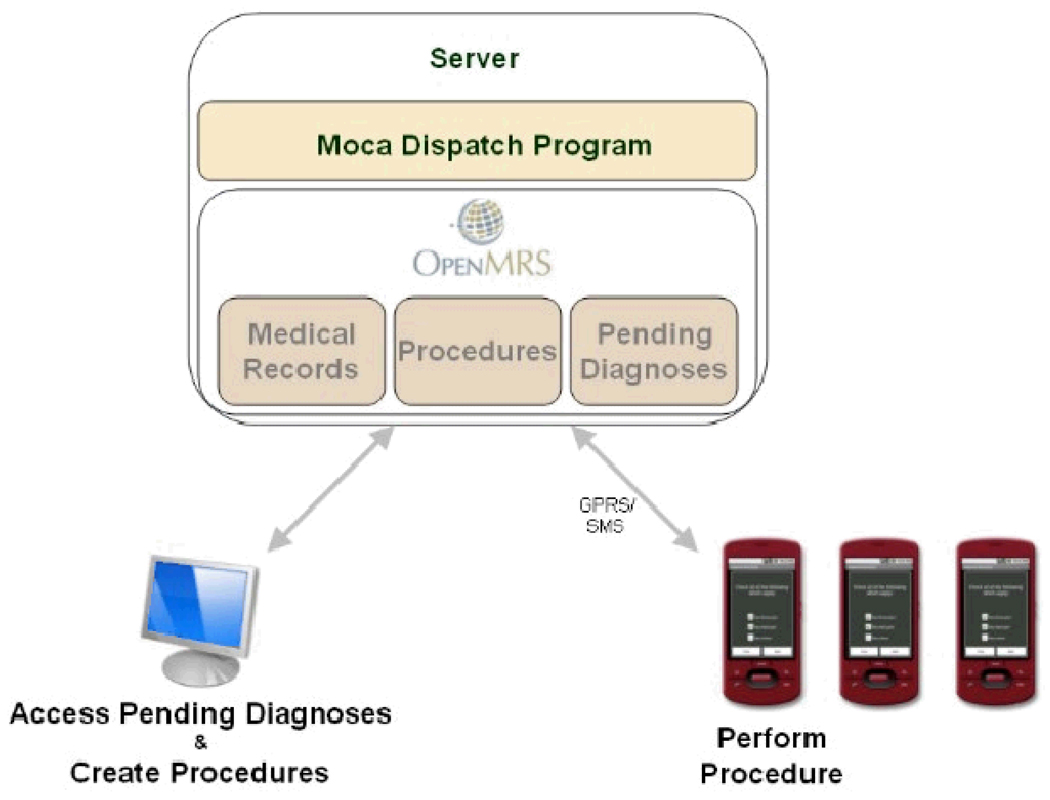
The complete Moca system consists of at least one (in most instances several) phones and a web-connected server. The server runs the medical records system of choice, such as OpenMRS, and the Moca Dispatch Server program.
The Moca Dispatch Server (Figure 2) is a program running on the server that is responsible for communication to and from phones registered in the system. It takes care of receiving data via the lower-level synchronization and packetization that the Moca-enabled phones perform. In addition to this, the Moca Dispatch Server has plug-ins that allow it to interface with medical records systems. Moca is currently fully-compatible with OpenMRS, using our OpenMRS plug-in for the Moca Dispatch Server.
Figure 2.
The Moca Dispatch Software
In addition to the Moca Dispatch Server program, the medical records system also runs on the server (although this can reside on a separate machine if the installer would like). Moca uses a custom-patched version of OpenMRS. This patch extends OpenMRS to have a queue of pending diagnoses in addition to allowing data such as images to be tagged to a patient record.
Moca is a turnkey solution that can be added to existing records systems deployments. If an organization is currently using OpenMRS, all that needs to be done is to
Install the Moca Dispatch Program onto a server
Point the Moca Dispatch Program to OpenMRS
Apply the Moca patch to OpenMRS.
A key challenge facing remote diagnostic platforms that utilize cellular networks in developing nations is the issue of connectivity. In order for a system to be useful, it must be robust. Moca uses several strategies to ensure reliable, low-cost data transfers.
Synchronization. When a Procedure tagged for upload is completed for a particular patient, the question/response pairs as well as other media (pictures, sounds, etc.) are stored in a local (on-phone) database. At this point the Procedure (or another one) can be rerun for the next patient. A background service is constantly listening for cellular service. As soon as service is available, all of the filled out forms (Procedures) are uploaded to the server.
Packetization. Some acquired data is extremely large. Video and high-resolution images, for example, take time to upload over GPRS. Oftentimes a half-completed transfer will be interrupted due to poor service. Even though a significant amount of data was transferred successfully, the mid-upload failure results in a complete drop of the data. Using packetization, Moca uploads large files in chunks so that very little bandwidth is wasted in the case of a lost connection.
Multimodal transfers. Moca has the ability to transfer data using a number of interfaces, including GPRS, WiFi, SMS, and USB tether. Different interfaces are used for different things. For example, images and sounds must be transferred on either GPRS, WiFi, or USB tether, but the text of a filled out Procedure can be sent back via SMS. The diagnosis/response from a physician that is sent back to the phone is sent via SMS. This is done for several reasons, such as the fact that if the phone is outside of the coverage area, the cellular network operator will take it upon itself to deliver the SMS notification as soon as the phone reenters service area.
Examples of envisioned Moca applications
A. Screening of Pregnant Women
Maternal and neonatal deaths result from obstetric complications such as placenta previa, breech presentation, and multiple gestations, among others. In developed countries these conditions are diagnosed through routine ultrasound, and preparations are made for either high-risk vaginal delivery (with possible conversion to a Cesarian section) or Cesarian delivery. In remote villages where there are no resources for high-risk obstetrics, these conditions significantly contribute to maternal and neonatal mortality. A mobile van is envisioned that will go from village to village for screening of pregnant women in their last trimester. Mothers diagnosed with the aforementioned conditions are advised to go to a facility with high-risk obstetric capabilities for their delivery.
B. Follow-up after Surgery
Patients are required to see their surgeon for the weeks following surgery to make sure the surgical wound is healing without infection. Patients who live in remote areas usually forego these follow-ups because of the hassle involved in traveling to the hospital. As a result, those who develop wound infections later become far more problematic to treat. With our clinical system, these patients can just follow-up in their local rural health clinic and have photos taken of their incision wound. The photos are sent to the surgeon accompanied by some clinical information. If an infection is diagnosed, the patient can either be started on antibiotics or referred back to the hospital.
C. Tele-Dermatology
The diagnosis of dermatologic conditions relies heavily on the physical appearance of the skin lesion. Real-time transmission of a good image of the lesion (rather than verbal description provided by a less trained healthcare worker) can facilitate leveraging of dermatology expertise to areas where they are not available.
D. Cervical Cancer Screening
Cervical cancer is a leading cause of death from cancer among women in resource-poor countries. Around the world, a woman dies of cervical cancer every 2 minutes. It is one of the few cancers with a long preclinical phase. Therefore, screening programs aimed at detecting and treating precancerous lesions reduce the number of cases that require treatment. Single visit screen-and-treat approach using visual inspection with 4% acetic acid (VIA) and early treatment with cryotherapy have been shown to be feasible, low-cost, and effective in reducing cervical cancer incidence and mortality in resource poor regions. However, lack of expert overview over screening in such regions leads to long lead times, and a loss of the opportunity to treat many patients. With Moca, health workers can acquire patient data and send back images of the cervix to a physician that can then remotely dispense a diagnosis. Even if the physician is hundreds of miles away, this response may arrive back to the health worker just minutes after sending the patient data to the Moca server. The health worker can then proceed with cryotherapy, if necessary, to treat the precancerous lesions.
Sustainability and future outlook
Moca has a strong list of partners on this project, including OpenMRS, MIT Media Lab Harvard School of Public Health, DiMagi, Partners in Health, OpenRosa, General Electric, NextBillion Network., and the Centers for E-Health and Tele-Medicine in Southeast Asia, a consortium consisting of six universities - Universiti Sains Malaysia (Malaysia), Institut dela Francophonie pour Medicine Tropicale (Laos), University of the Philippines Manila (Philippines), University of Gadjah Mada (Indonesia), Ciputra University (Indonesia) and Hanoi Medical University (Vietnam). In conjunction with the University of the Philippines National Tele-Medicine Center, plans are underway for a pilot deployment of the clinical information system to facilitate tele-dermatology and tele-ophthalmology in the province of Capiz in the Philippines in June. The team is set to visit the Philippines in March to meet government officials and NGO representatives in order to secure funding for project implementation.
Demonstrating value for ICT4D projects is key in order to insure sustainability. Value is defined by the outcomes achieved divided by the cost of achieving those outcomes. Interventions to address specific societal needs should undergo rigorous and robust evaluation especially when there are limited resources, whether economic or human. The use of expensive technology should be justified by value, not by its ingenious design and demonstration of its feasibility. It has to facilitate the most cost-effective way of achieving the desired outcomes and the delivery of the best return-on-investment.
To this end, we are planning to perform cost effectiveness analysis of our technology-facilitated clinical information system. This will require meticulous collection of information including the cost of implementation and maintenance of the technology and clinical outcomes tracking. Such an analysis will allow us to calculate the cost per year of life saved, and depending on a country’s threshold for what it considers cost-effective (usually less than the per capita GDP according to the Commission on Macroeconomics and Health [9]), will determine whether the project delivers a good return-on-investment.
Finally, the ease with which resource-poor agents can program ‘intelligent’ diagnostic and training algorithms on the cell phone provides the opportunity for developing nations to enter a traditionally closed medical services and device market that usually requires high initial capital investment or high levels of specialist training. Such an opportunity in this industry may lead to a paradigm change in health care both in developing and developed countries, allowing developing nations to build a health care system for future generations. However, this change is likely to be possible only if open source practices are followed.
The Moca Team
Moca started as a class project by two MIT students – Leo Anthony Celi and Andres Monroy-Hernandez, for a course called ICT4D (designed by four MIT researchers – Gari Clifford, Rich Fletcher, Jhonathan Rotberg and Luis Sarmenta) where students learn about and work on applications of information and communication technologies for use in developing countries and underserved communities. The ICT4D course, which evolved into NextLab, is the core of the academic program of the Next Billion Network project (founded by Jhonathan Rotberg) which addresses the challenges and opportunities resulting from the next billion people acquiring cellphones over the next three years. During the fall of 2008, two new groups joined the team, one from NextLab and another from Professor Hal Abelson’s course on “Building Mobile Applications”. The Moca team currently consists of Santiago Alfaro, Zackary Anderson, Peter Bojo, Steven Camina, Leo Anthony Celi, Theodore Chan, Albert Chang, Gari Clifford, Clark Freifeld, Alexis Geaneotes, Elliot Higger, Sameer Hirji, Meghan Kane, Katherine Kuan, Richard Lu, Crystal Mao, Christopher Moses, Nicole Prowell, Russell Ryan, Luis Sarmenta, Kevin Sheu, Mark Yen, and Boyuan Zhu.
References
- 1.Whited JD, Hall RP, Simel DL, Foy ME, Stechuchak KM, Drugge RJ. Reliability and accuracy of dermatologists’ and clinic-based and digital image consultations. J Am Acad Dermatol. 1999 November;vol. 41:693–702. doi: 10.1016/s0190-9622(99)70003-4. [DOI] [PubMed] [Google Scholar]
- 2.Hofmann-Wellenhof R, Salmhofer W, Binder B, Okcu A, Kerl H, Soyer HP. Feasibility and acceptance of telemedicine for wound care in patients with chronic leg ulcers. J Telemed Telecare. 2006;vol. 12:15–17. doi: 10.1258/135763306777978407. [DOI] [PubMed] [Google Scholar]
- 3.Braun RP, Vecchietti JL, Thomas L, Prins C, French LE, Gewirtzman AJ, Saurat JH, Salomon D. Telemedical wound care using a new generation of mobile telephones. Arch Dermatol. 2005 February;vol. 141:254–258. doi: 10.1001/archderm.141.2.254. [DOI] [PubMed] [Google Scholar]
- 4.Whited JD. Teledermatology research review. Int J Dermatol. 2006 March;vol. 45:220–229. doi: 10.1111/j.1365-4632.2004.02427.x. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh CH, Tsai HH, Yin JW, Chen CY, Yang JC, Jeng SF. Teleconsultation with the mobile camera-phone in digital soft-tissue injury: a feasibility study. Plast Reconstr Surg. 2004 December;vol. 114:1776–1782. doi: 10.1097/01.prs.0000142402.07896.21. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh CH, Jeng SF, Chen CY, Yin JW, Yang JC, Tsai HH, Yeh MC. Teleconsultation with the mobile camera-phone in remote evaluation of replantation potential. J Trauma. 2005 June;vol. 58:1208–1212. doi: 10.1097/01.ta.0000175098.52974.fa. [DOI] [PubMed] [Google Scholar]
- 7.Malkin R. Design of Health Care Technologies for the Developing World. Annu Rev Biomed Eng. 2007;9:567–587. doi: 10.1146/annurev.bioeng.9.060906.151913. [DOI] [PubMed] [Google Scholar]
- 8.Clifford GD, Blaya JA, Hall-Clifford R, Fraser HSF. Medical information systems: A foundation for healthcare technologies in developing countries. 2008 June;vol. 7:18. doi: 10.1186/1475-925X-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Macro-economics and health: investing in health for economic development: report of the Commission on Macroeconomics and Health. Geneva: World Health Organization; 2001