Abstract
Physician perception of medication adherence may alter prescribing patterns. Perception of patients has been linked to readily observable factors, such as race and age. Obesity shares a similar stigma to these factors in society. We hypothesized that physicians would perceive patients with a higher BMI as nonadherent to medication. Data were collected from the baseline visit of a randomized clinical trial of patient–physician communication (240 patients and 40 physicians). Physician perception of patient medication adherence was measured on a Likert scale and dichotomized as fully adherent or not fully adherent. BMI was the predictor of interest. We performed Poisson regression analyses with robust variance estimates, adjusting for clustering of patients within physicians, to examine the association between BMI and physician perception of medication adherence. The mean (s.d.) BMI was 32.6 (7.7) kg/m2. Forty-five percent of patients were perceived as nonadherent to medications by their physicians. Higher BMI was significantly and negatively associated with being perceived as adherent to medication (prevalence ratio (PrR) 0.76, 95% confidence interval (CI): 0.64–0.90; P = 0.002; per 10 kg/m2 increase in BMI). BMI remained significantly and negatively associated with physician perception of medication adherence after adjustment for patient and physician characteristics (PrR 0.80, 95% CI: 0.66–0.96; P = 0.020). In this study, patients with higher BMI were less likely to be perceived as adherent to medications by their providers. Physician perception of medication adherence has been shown to affect prescribing patterns in other studies. More work is needed to understand how this perception may affect the care of patients with obesity.
Introduction
Provider beliefs and attitudes about patients can have great impact on the care and outcomes of patients. Provider perceptions of the patient can influence the degree to which the provider complies with accepted guidelines in acute coronary syndrome, hemophilia and HIV (1–4). The perceived adherence to medication influences physician prescribing patterns and may lead to a failure to intensify therapy in diabetes (5,6). In addition, the perception of nonadherence can lead to a sense of frustration in physicians which may lead to more paternalistic attitudes in the management of the patient (7).
Providers find it difficult to communicate about adherence issues and tend to rely on their own inferences (8). Lutfey et al. found that observable factors, such as race and age, influence the physicians’ perceptions about the patient’s medication adherence—despite the independence of patient self-report from these factors (9–11). Similar to race and age, there are negative attitudes regarding obesity in our society (12,13). Recent studies have found that obesity stigma has increased dramatically despite the increased prevalence of obesity (14–17). The literature documents a clear, negative bias of physicians toward obesity (18–21). Much of this work describes general attitudes held by physicians; few studies, if any, document negative attitudes toward individual patients with obesity.
Obesity is an easily observable factor that elicits negative responses in physicians (18), and like race and age, may influence provider perceptions of medication adherence (9). We hypothesized that patients with a higher BMI would be more likely to be perceived as nonadherent by their providers. We also hypothesized that this relationship would be independent of patient-reported medication adherence as well as other patient and physician variables. In addition, we hypothesized that blood pressure control would partially mediate the relationship between patient BMI and physician perception of patient medication adherence in this sample of patients with hypertension.
Methods and Procedures
Study design and setting
Data for this study were obtained from the baseline visit of the patient–physician partnership (PPP) study, a randomized controlled trial of physician and provider interventions to improve patient–physician communication (22). Forty physicians and 240 of their patients with available height, weight, and physician perception of adherence data were included in this analysis. Primary-care physicians were recruited from 15 urban community practices in the Baltimore, MD, area from January 2002 to January 2003. Patients of enrolled physicians, aged >18 years and English-speaking, with hypertension were identified from physician rosters and recruited for participation. Patients were enrolled from September 2003 to August 2005.
Measures
Prior to patient enrollment, physicians completed a baseline questionnaire about demographic factors (age, gender, race, specialty, and practice experience). At enrollment, patients completed a survey about their health status, demographic factors (age, gender, race/ethnicity, educational attainment, income, and employment status), health literacy, and adherence to recommended therapies for hypertension. Patients also had a physical exam which included height and weight and blood pressure. Blood pressure control was defined as an average systolic <140 mm Hg and an average diastolic <90 mm Hg over three readings and the method used has been described previously (22). Height and weight were taken from the clinical record and were measured according to each clinic’s protocol. Literacy was assessed with the rapid estimate of adult literacy in medicine (REALM) and was examined as a dichotomous variable defined a priori as ≥9th grade or <9th grade (23,24). Patient self-reported medication adherence was assessed with the Morisky scale and was examined as a dichotomous variable of adherent (answered “no” to each of the three items in the scale) or nonadherent (25). The Morisky scale has been found to have a sensitivity of 72% and specificity of 74% for ≥80% medication compliance (26). Disease burden was determined by summing the number of self-reported health conditions from the following list of 16: diabetes, arthritis, asthma or chronic obstructive pulmonary disease, cancer, neurological disease, stroke, heart failure, angina, back problems, irritable bowel, thyroid, kidney disease, eye disease, mental health, alcohol/substance abuse, and other health problem.
Physicians and patients were asked to report their gender and race. For race, physicians and patients were asked to identify what they considered their main racial or ethnic group from the following options: non-Hispanic white, non-Hispanic black, Hispanic or Latino, Asian or Pacific Islander, American Indian or Alaskan Native or other. Due to sample size, physician and patient race was examined as black or not black in multivariate analyses. Patients also self-reported their income and health insurance status.
After the enrollment of patient–provider encounter, physicians and patients completed questionnaires about their perceptions of the visit and of one another. Physicians were asked to rank their perception of the patient’s adherence to medications on a 4-point Likert scale after the completion of the patient visit. Two categories were created: fully adherent (Likert score 4) and not fully adherent (Likert score 1–3). Physicians were asked additional perceptions of the patients after the encounter. Physicians were asked to rank the patient’s literacy on a 5-point Likert scale. This variable was categorized as physician perceives patient to be “literate” (Likert score 5) or physician perceives patient to have low literacy (Likert score 1–4). Physicians were also asked to rate their effectiveness in influencing patient behavior on a 5-point Likert scale. This was categorized as effective (Likert score 4–5) or not effective (Likert score 1–3).
The primary outcome was the physician perception of the patient’s adherence to antihypertensive medications, dichotomized as fully adherent and not fully adherent. The independent variable of interest was patient BMI (calculated from measured height and weight). We also looked at clinically relevant BMI categories. We divided BMI into five clinical categories—normal (BMI <25 kg/m2), overweight (BMI 25–30 kg/m2), obesity class 1 (BMI 30–35 kg/m2), obesity class 2 (BMI 35–40 kg/m2), and obesity class 3 (BMI ≥40 kg/m2).
Statistical analyses
Analyses were performed using STATA 9.2 (Stata, College Park, TX). Descriptive analyses of all variables were performed. Pearson’s χ2 and adjusted Wald test were used to compare characteristics between strata of physician perceptions of medication adherence categories, as appropriate. These bivariate analyses were adjusted for the clustering of patients among physician. Dichotomization cutoffs of Likert scales were based on the distribution of the data and discussion among the investigators about the face validity of the dichotomization. All cutoffs were defined a priori and when possible, sensitivity analyses with ordinal variables were used to ensure that dichotomization did not affect the point estimates. Poisson regression with robust variance estimates, clustered by physician, was performed. Poisson regression with robust variance estimates was used as low perceived adherence was a common outcome (>10%) and Poisson regression with robust variance estimates provides a more reliable estimate of prevalence risk ratio compared to standard logistic regression (27). Covariates that were associated with physician perception of patient medication adherence at the P < 0.10 level were included in multivariate models, including patient’s age, race, literacy, patient-reported medication adherence, income, health insurance, physician perception of patient literacy, and physician perception of effectiveness in influencing patient behavior. As blood pressure control is a tangible measure of disease management, physicians may use blood pressure control to gauge patient adherence to medications. An additional model was performed to examine whether blood pressure control was a partial mediator in this relationship. Lastly, we looked for a dose response in the relationship of BMI and physician perception of medication adherence by performing a Poisson regression analysis with robust variance estimates, clustered by physician, comparing overweight and three classes of obesity to those patients with a normal BMI (<25 kg/m2).
Ethics
This study was approved by the Johns Hopkins institutional review board. Patients and providers provided written consent prior to inclusion in the study.
Results
Patient and provider characteristics are presented in Table 1. The mean (s.d.) age was 61.2 (11.8) years. The majority of patients in this study were female (62%), black (62%), had health literacy ≥9th grade (63%), and reported adherence to medication (60%). Over half of the patients (54%) had a female physician and 27% had a black physician. Fifty-eight percent had controlled blood pressure and 66% of patients were respected more or much more than the average patient by their physicians. The mean patient BMI (s.d.) in the study was 32.9 (8.1) kg/m2. Over half of the physicians were female (54%) and non-black (71%). The mean (s.d.) age of physicians was 43.0 (8.6) years.
Table 1.
Patient and physician characteristics
| Characteristics | |
|---|---|
| Patient (n = 240) | |
| Age, years, mean (s.d.) | 61.2 (11.8)a |
| Female | 65 |
| Black | 62 |
| Literacy ≥9th grade | 63 |
| Patient reports nonadherence | 40a |
| Annual income <$35,000 | 72 |
| No health-care insurance | 9 |
| BP controlled | 58 |
| Disease burdenb | 2.7 (1.8) |
| Diabetes | 44a |
| Congestive heart failure | 5 |
| History of stroke | 5 |
| Kidney disease | 4a |
| BMI, kg/m2, mean (s.d.) | 32.6 (7.7) |
| Physician (n = 40) | |
| Age, years, mean (s.d.) | 43.0 (8.6) |
| Female | 54 |
| Black | 29 |
| Physician perception of patient (n = 240) | |
| Physician perceives patient to have low literacy | 53 |
| Physician perceives effective in influencing patient | 61 |
Reported as % unless otherwise noted.
Significantly associated with BMI (linear regression adjusted for physician clusters).
Disease burden is the count of the following 16 chronic diseases: diabetes, arthritis, asthma/chronic obstructive pulmonary disease, cancer, neurological, stroke, heart failure, angina, back problems, irritable bowel, thyroid, kidney disease, eye disease, mental health, alcohol/substance abuse, other health problem.
Forty-five percent of patients were viewed as nonadherent to medication by their physician. Patients who were perceived as nonadherent to medication by their providers were more likely to have higher BMI (34.4 kg/m2 vs. 31.1 kg/m2, P = 0.035), be younger (59.1 years vs. 62.9 years, P = 0.011), report nonadherence to medications (50% vs. 31%, P = 0.001), have an annual income less than $35,000 (83% vs. 62%, P = 0.0001), not have health-care insurance (15% vs. 5%, P = 0.0071) and not have controlled blood pressure (49% vs. 65% controlled, P = 0.049) when compared to patients perceived as fully adherent by their physician, after adjustment for physician clusters (see Table 2). No physician or relationship characteristics were associated with physician perception of patient medication adherence.
Table 2.
Characteristics associated with physician perception of patient medication adherence
| Characteristics | Perceived as medication nonadherent (n = 109) | Perceived as medication adherent (n = 131) | P valuea |
|---|---|---|---|
| Patient | |||
| BMI, kg/m2, mean (s.d.) | 34.4 (8.3) | 31.1 (6.8) | 0.035 |
| Age, years, mean (s.d.) | 59.1 (11.6) | 62.9 (11.6) | 0.011 |
| Female | 67 | 82 | 0.47 |
| Black | 70 | 56 | 0.063 |
| Literacy ≥9th grade | 57 | 68 | 0.075 |
| Patient reports nonadherence | 50 | 31 | 0.0010 |
| Annual income ≥$35,000 | 17 | 38 | 0.0001 |
| No health-care insurance | 15 | 5 | 0.0071 |
| Disease burden, mean (s.d.)b | 3.1 (1.9) | 2.5 (1.6) | 0.014 |
| Diabetes | 54 | 35 | 0.0056 |
| Congestive heart failure | 7 | 4 | 0.33 |
| History of stroke | 7 | 3 | 0.21 |
| Kidney disease | 5 | 4 | 0.79 |
| BP controlled | 49 | 65 | 0.049 |
| Physician | |||
| Age, years, mean (s.d.) | 43.2 (7.3) | 42.7 (8.5) | 0.69 |
| Female | 50 | 59 | 0.26 |
| Black | 26 | 30 | 0.47 |
| Physician perception of patient | |||
| Physician perceives patient to have low literacy | 62 | 35 | 0.0007 |
| Physician perceives effective in influencing patient | 48 | 32 | 0.079 |
Reported as % unless otherwise reported.
Pearson’s χ2 or adjusted Wald test, as appropriate, adjusted for physician clusters.
Disease burden is the count of the following 16 chronic diseases: diabetes, arthritis, asthma/chronic obstructive pulmonary disease, cancer, neurological, stroke, heart failure, angina, back problems, irritable bowel, thyroid, kidney disease, eye disease, mental health, alcohol/substance abuse, other health problem.
In multivariate analyses, BMI remained significantly associated with physician perception of medication adherence (see Table 3). The prevalence ratio (PrR) of being perceived as adherent to medication was lower for each 10 kg/m2 higher patient BMI after adjusting for patient characteristics and physician clusters (PrR 0.80, 95% confidence interval (CI) 0.66–0.96, P = 0.020). Patient age, physician perception of patient literacy and physician perception of effectiveness in influencing patient behavior were all significantly associated with physician perception of patient medication adherence in the multivariate model.
Table 3.
Unadjusted and adjusted prevalence ratios for perceived medication adherence
| Prevalence ratio (95% CI) | P value | |
|---|---|---|
| Unadjusted model | ||
| BMIa | 0.76 (0.64–0.90) | 0.002 |
| Model 1 | ||
| BMIa | 0.80 (0.66–0.96) | 0.02 |
| Patient, ageb | 1.09 (1.01–1.19) | 0.04 |
| Patient, blackc | 0.87 (0.69–1.10) | 0.23 |
| Literacy ≥9th graded | 0.95 (0.74–1.22) | 0.70 |
| Patient-reported nonadherencee | 0.83 (0.64–1.08) | 0.16 |
| Annual income ≥$35,000f | 1.19 (0.97–1.45) | 0.09 |
| No health-care insuranceg | 0.66 (0.33–1.32) | 0.24 |
| Disease burdenh | 0.95 (0.88–1.03) | 0.20 |
| Physician perceives patient as literatei | 1.41 (1.05–1.89) | 0.02 |
| Physician perceives effective in influencing patient j | 1.40 (1.08–1.81) | 0.01 |
| Model 2 | ||
| BMIa | 0.83 (0.69–1.00) | 0.05 |
| Patient, ageb | 1.08 (0.99–1.18) | 0.08 |
| Patient, blackc | 0.87 (0.69–1.10) | 0.24 |
| Literacy ≥9th graded | 0.94 (0.73–1.21) | 0.64 |
| Patient-reported nonadherencee | 0.85 (0.65–1.10) | 0.21 |
| Annual income ≥35,000f | 1.17 (0.96–1.42) | 0.12 |
| No health-care insuranceg | 0.67 (0.34–1.34) | 0.26 |
| Disease burdenh | 0.94 (0.88–1.01) | 0.11 |
| Physician perceives patient as literatei | 1.39 (1.04–1.87) | 0.03 |
| Physician perceives effective in influencing patient j | 1.38 (1.07–1.78) | 0.01 |
| BP controlledk | 1.23 (0.87–1.73) | 0.24 |
Poisson regression, with robust variance estimates, including clustering for physician. BP, blood pressure; CI, confidence interval.
Compared to 10 kg/m2 higher BMI.
Compared to 10 year increase in age.
Compared to non-black patients.
Determined by Rapid Estimate of Adult Literacy, compared to literacy <9th grade.
Determined by Morisky scale, compared to adherent by patient report.
Compared to annual income <$35,000.
Compared to health-care insurance.
Disease burden is the count of the following 16 chronic diseases: diabetes, arthritis, asthma/chronic obstructive pulmonary disease, cancer, neurological, stroke, heart failure, angina, back problems, irritable bowel, thyroid, kidney disease, eye disease, mental health, alcohol/substance abuse, other health problem.
Compared to physician does not perceive patient as literate.
Compared to physician does not perceive themselves as effective in influencing patient.
Determined by the average of last three blood pressure readings, compared to not controlled.
We next added blood pressure control to the model. The PrR of perceived adherence with each 10 kg/m2 higher patient BMI was virtually unchanged (PrR 0.83, 95% CI: 0.69–1.00, P = 0.048). Blood pressure control was not significantly associated with physician perception of adherence to medication (PrR 1.23, 95% CI: 0.87–1.73, P = 0.24). Annual income, physician perception of patient literacy and physician perception of effectiveness in influencing patient behavior also remained statistically significantly associated with physician perception of patient medication adherence (see Table 3).
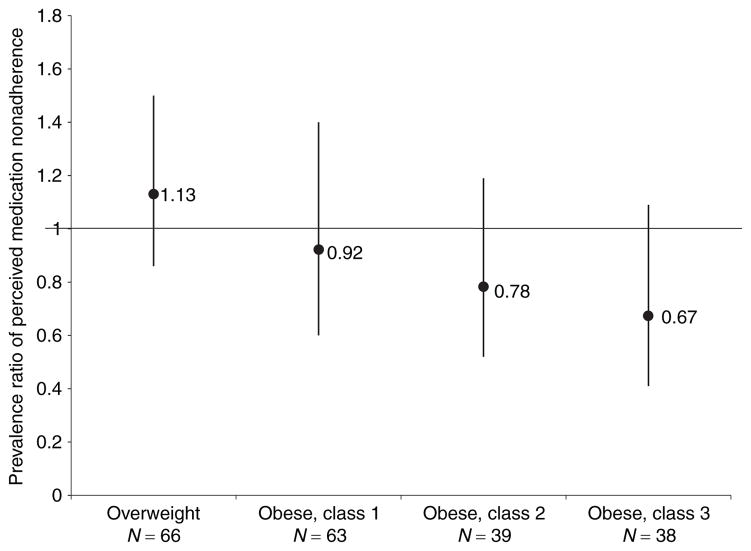
In Figure 1, we display physician perception of adherence by category of BMI. The PrR of the patient being perceived as adherent by their physician tended to be lower for each class of obesity when compared to normal weight patients but did not reach statistical significance (class 1: PrR 0.92, 95% CI: 0.60– 1.40; class 2: PrR 0.78, 95% CI: 0.52–1.19; class 3: PrR 0.67, 95% CI: 0.41–1.09).
Figure 1.
Physician perception of medication adherence by category of BMI. This figure shows the prevalence ratio of physician perceived patient medication nonadherence for categories of overweight and obesity when compared to normal weight. The analysis was adjusted for patient clustering by physician.
Discussion
Physician perception of patient adherence to medication may affect prescribing patterns and intensification of management. In this study, we found that patients with higher BMI were less likely to be perceived as adherent to medications by their physicians. This finding was robust even after adjustment for demographic factors, patient literacy, patient-reported medication adherence, blood pressure control, and other physician perceptions of the patient.
Obesity stigma is pervasive in our society and physicians also hold negative attitudes toward obesity and persons with obesity (12,13). However, few studies, if any, have explored how such stigma may influence the patient–physician relationship and the way in which a physician cares for a patient. Several studies have shown that patients who are perceived as nonadherent by their physician may not receive guideline-recommended care (1–6). In a study in HIV/AIDS, Wong et al. found that perception of nonadherence was associated with delay in prescribing recommended medications and physician perceived nonadherence in the poor, women, and Latinos (4). Lutfey et al. investigated patient factors associated with physician perception of adherence found that age and race, but not education, income or cognitive ability were associated with the patient being perceived as nonadherent by their providers (9). These studies, and others, suggest that providers may use readily observable factors to stereotype patients (10,11,28). BMI is also a readily observable factor and may also be associated with similar stereotyping; body weight has been shown to significantly affect how physicians treat their patients (29). It is unknown how the perception of nonadherence may affect other aspects of the provider–patient relationship, such as education and recommendations for lifestyle changes and screening activities.
Patient-reported medication adherence was not significantly associated with physician perception of medication adherence in the multivariate models. Many studies have shown that providers do not discuss medication adherence with their patients, do not like to discuss adherence and may not use effective communication techniques when they do discuss the topic (8,30–33). In a review of the literature in HIV/AIDS, Murri et al. found that physicians often misjudge patient adherence (34). Considering this literature, it is not surprising that physician perception of medication adherence was not more strongly associated with patient report of adherence.
Other physician perceptions of patients were strongly associated with physician perception of medication adherence. As this is a cross-sectional study, it is difficult to untangle this association further. It may be that these perceptions develop in parallel, such that negative physician perceptions of any type are grouped together. On the other hand, it is possible that one perception (such as physician perception of literacy) leads to physician perception of medication nonadherence. Future, longitudinal work is needed to better understand this phenomenon and how physician perceptions affect interventions to improve patient care. Results of interventions that aim to improve hypertension management through physician education alone are mixed (35,36). Perhaps incorporating awareness of physician perceptions of patients in addition to education about the management of hypertension would lead to greater improvements in blood pressure in quality improvement interventions than physician education alone.
We initially hypothesized that blood pressure control for the patient would mediate the relationship between BMI and physician perception of adherence. Physicians may use clinical measures, such as blood pressure or laboratory values, to determine whether patients are adherent to therapy. If a patient’s blood pressure is under control, then the physician may assume the patient is adherent to the medication regimen. Although there was a significant relationship between physician perception of patient medication adherence with controlled blood pressure in bivariate analysis, this was no longer significant in multivariate analysis. In addition, there was little reduction of the point estimate of the relationship between BMI and provider perception of patient medication adherence when blood pressure control was added to the model, indicating that it is not a strong mediator. Patients with obesity have been described as having hard to control blood pressure which some physicians feel to be related to nonadherence to therapy (37). However, our study does not support that physicians’ perception of patient medication adherence with obesity is mediated by blood pressure control.
Our study has several limitations. Although we had adequate power to assess our primary outcome, we had limited power to detect some of the associations between physician perception of adherence and our covariates. Similarly, we were underpowered to look at provider perception by category of BMI. However, we feel that this analysis supports our primary hypothesis and may provide useful information for providers and future research. In this initial study of provider perception of patient adherence and BMI, we are unable to explain how this relationship develops. Finally, this is a cross-sectional study, and therefore cannot assess causation.
Obesity stigma is common in health care, yet the impact of this stigma on patients is not fully understood. Several studies have documented suboptimal care that results from provider perception of nonadherence and in this study, we found that higher BMI is strongly associated with provider perception of nonadherence. Further work is needed to understand whether this finding is due to antiobesity bias in providers or to other patient–provider relationship factors, and whether provider perceptions of adherence negatively influence quality of care and outcomes for obese patients.
Acknowledgments
This work was supported, in part, by grants from the National Heart, Lung, and Blood Institute (R01HL069403 and K24HL083113). M.M.H. was supported by the Johns Hopkins Clinical Research Scholars Program (NCR 5K12RR023266). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. We acknowledge Kathryn Carson for her assistance with data management. M.M.H. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclosure
The authors declared no conflict of interest.
References
- 1.Bassetti S, Battegay M, Furrer H, et al. Why is highly active antiretroviral therapy (HAART) not prescribed or discontinued? Swiss HIV Cohort Study. J Acquir Immune Defic Syndr. 1999;21:114–119. [PubMed] [Google Scholar]
- 2.Porter A, Iakobishvili Z, Dictiar R, et al. The implementation of guidelines and prognosis among patients with acute coronary syndromes is influenced by physicians’ perception of antecedent physical and cognitive status. Cardiology. 2007;107:422–428. doi: 10.1159/000099653. [DOI] [PubMed] [Google Scholar]
- 3.Thornburg CD. Physicians’ perceptions of adherence to prophylactic clotting factor infusions. Haemophilia. 2008;14:25–29. doi: 10.1111/j.1365-2516.2007.01591.x. [DOI] [PubMed] [Google Scholar]
- 4.Wong MD, Cunningham WE, Shapiro MF, et al. HCSUS Consortium. Disparities in HIV treatment and physician attitudes about delaying protease inhibitors for nonadherent patients. J Gen Intern Med. 2004;19:366–374. doi: 10.1111/j.1525-1497.2004.30429.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.el-Kebbi IM, Ziemer DC, Gallina DL, Dunbar V, Phillips LS. Diabetes in urban African-Americans. XV. Identification of barriers to provider adherence to management protocols. Diabetes Care. 1999;22:1617–1620. doi: 10.2337/diacare.22.10.1617. [DOI] [PubMed] [Google Scholar]
- 6.Roberts KJ, Volberding P. Adherence communication: a qualitative analysis of physician-patient dialogue. AIDS. 1999;13:1771–1778. doi: 10.1097/00002030-199909100-00022. [DOI] [PubMed] [Google Scholar]
- 7.Wens J, Vermeire E, Royen PV, Sabbe B, Denekens J. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam Pract. 2005;6:20. doi: 10.1186/1471-2296-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barfod TS, Hecht FM, Rubow C, Gerstoft J. Physicians’ communication with patients about adherence to HIV medication in San Francisco and Copenhagen: a qualitative study using Grounded Theory. BMC Health Serv Res. 2006;6:154. doi: 10.1186/1472-6963-6-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lutfey KE, Ketcham JD. Patient and provider assessments of adherence and the sources of disparities: evidence from diabetes care. Health Serv Res. 2005;40:1803–1817. doi: 10.1111/j.1475-6773.2005.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40:I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 11.van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 13.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 14.Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity (Silver Spring) 2008;16:1129–1134. doi: 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- 15.Latner JD, O’Brien KS, Durso LE, Brinkman LA, MacDonald T. Weighing obesity stigma: the relative strength of different forms of bias. Int J Obes (Lond) 2008;32:1145–1152. doi: 10.1038/ijo.2008.53. [DOI] [PubMed] [Google Scholar]
- 16.Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight-based stigmatization in a weight loss surgery population: psychological and behavioral correlates. Obesity (Silver Spring) 2008;16 (Suppl 2):S69–S74. doi: 10.1038/oby.2008.457. [DOI] [PubMed] [Google Scholar]
- 17.Sarwer DB, Fabricatore AN, Eisenberg MH, Sywulak LA, Wadden TA. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring) 2008;16 (Suppl 2):S75–S79. doi: 10.1038/oby.2008.450. [DOI] [PubMed] [Google Scholar]
- 18.Klein D, Najman J, Kohrman AF, Munro C. Patient characteristics that elicit negative responses from family physicians. J Fam Pract. 1982;14:881–888. [PubMed] [Google Scholar]
- 19.Maddox GL, Liederman V. Overweight as a social disability with medical implications. J Med Educ. 1969;44:214–220. doi: 10.1097/00001888-196903000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Price JH, Desmond SM, Krol RA, Snyder FF, O’Connell JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–345. [PubMed] [Google Scholar]
- 21.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 22.Cooper LA, Roter DL, Bone LR, et al. A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci. 2009;4:7. doi: 10.1186/1748-5908-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–435. [PubMed] [Google Scholar]
- 24.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 25.Morisky DE, Levine DM, Green LW, Smith CR. Health education program effects on the management of hypertension in the elderly. Arch Intern Med. 1982;142:1835–1838. [PubMed] [Google Scholar]
- 26.George CF, Peveler RC, Heiliger S, Thompson C. Compliance with tricyclic antidepressants: the value of four different methods of assessment. Br J Clin Pharmacol. 2000;50:166–171. doi: 10.1046/j.1365-2125.2000.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 29.Hebl MR, Mannix LM. The weight of obesity in evaluating others: a mere proximity effect. Pers Soc Psychol Bull. 2003;29:28–38. doi: 10.1177/0146167202238369. [DOI] [PubMed] [Google Scholar]
- 30.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–583. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sleath B, Tulsky JA, Peck BM, Thorpe J. Provider-patient communication about antidepressants among veterans with mental health conditions. Am J Geriatr Pharmacother. 2007;5:9–17. doi: 10.1016/j.amjopharm.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Arar NH, Wen L, McGrath J, Steinbach R, Pugh JA. Communicating about medications during primary care outpatient visits: the role of electronic medical records. Inform Prim Care. 2005;13:13–22. doi: 10.14236/jhi.v13i1.576. [DOI] [PubMed] [Google Scholar]
- 33.Richard C, Lussier MT. Nature and frequency of exchanges on medications during primary care encounters. Patient Educ Couns. 2006;64:207–216. doi: 10.1016/j.pec.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Murri R, Antinori A, Ammassari A, et al. Physician estimates of adherence and the patient-physician relationship as a setting to improve adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S158–S162. doi: 10.1097/00126334-200212153-00015. [DOI] [PubMed] [Google Scholar]
- 35.Cooper LA. A 41-year-old African American man with poorly controlled hypertension: review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301:1260–1272. doi: 10.1001/jama.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006:CD005182. doi: 10.1002/14651858.CD005182.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52:1749–1757. doi: 10.1016/j.jacc.2008.08.036. [DOI] [PubMed] [Google Scholar]