Abstract
J Clin Hypertens (Greenwich). 2011;13:605–612.©2011 Wiley Periodicals, Inc.
This paper reports the results of a clinical investigation to determine the sustainability of intervention effects to lower blood pressure (BP) that were obtained through a short‐term education via home telemonitoring of BP and regular counseling by bilingual nurses during 1 year. A total of 359 middle‐aged (40–64 years) Korean immigrants completed a 15‐month intervention that consisted of 6‐week behavioral education followed by home telemonitoring of BP and bilingual nurse telephone counseling for 12 months. The final analysis revealed a sharp increase in BP control rates sustained for more than 12 months. At baseline, only 30% of the sample achieved BP control (<140/90 mm Hg). After the initial education period (approximately 3 months), 73.3% of the participants had controlled BP levels. The levels of control were maintained and continuously improved during a 12‐month follow‐up period (83.2%, P<.001). These findings suggest that home telemonitoring of BP and tailored counseling are both useful tools to sustain or improve short‐term education effects.
High blood pressure (HBP) remains a major public health concern both in the United States and worldwide. According to a recent report by the Institute of Medicine, 1 the health and economic burden of cardiovascular disease (CVD) and its risk factors, such as HBP, has a major impact not only in developed countries but also in many low‐ and middle‐income countries. There is a great need for crystallized lessons learned from developed countries such as the United States in the management of HBP that can be essential for implementing effective treatment strategies for individuals affected by such emerging epidemics such as HBP and CVD worldwide.
Unfortunately, the report card for addressing the management of HBP in population levels for developed countries including the United States is suboptimal. Despite abundant knowledge, treatment options, and well‐established clinical guidelines for HBP, only 24% to 29% of people affected by the condition actually achieve the optimal levels of BP. 2 Moreover, the disease burden of HBP is known to disproportionately affect certain groups of individuals, especially those who are socially disadvantaged. Certain ethnic minority groups such as African Americans and Korean Americans have been reported to have a higher prevalence of uncontrolled HBP when compared with individuals from dominant cultural groups. 3 , 4 , 5 , 6 , 7
Managing chronic health conditions such as HBP requires providing evidence‐based pharmacologic treatment and effective education of critical behaviors to promote healthy individual choices and appropriate self‐care. The importance of promoting self‐care in managing HBP is underscored by the overall low control rate of HBP despite the overwhelming evidence for the effectiveness of pharmacologic interventions in reducing BP both in the United States and other developed countries.
Lifestyle modification or psychobehavioral education interventions of HBP have varying degrees of success. 8 , 10 , 11 , 12 , 13 , 14 , 15 While most of these interventions have yielded successful outcomes in a relatively short amount of time (8 weeks–6 months), the sustainability of those intervention outcomes or long‐term effects are questionable as many studies are only measured by short‐term outcomes.
Given that the nature of managing BP control is considered a lifetime endeavor, it is important to find effective ways to improve both self‐care skills and motivations for individuals with HBP during the course of their lifetime. Unfortunately, there has been little discussion about systematic ways to improve and maintain self‐care skills after critical knowledge and skills are obtained through a lifestyle modification education program with the goal of achieving and maintaining optimal BP as well as preventing complications.
A significant omission from the current literature includes ways of incorporating ever‐increasing health technology as a tool for motivating and improving self‐care behaviors in long‐term settings. Recently, intervention studies examining the effects of self‐BP monitoring suggested that self‐monitoring of BP is associated with moderate BP reduction independent of other factors. 16 , 17 , 18 , 19 These findings are worth further exploration to see the effects of self‐monitoring as a potential means of sustaining positive effects through effective education or behavioral lifestyle modification interventions provided in community samples.
In light of these considerations, we designed a study that examined the sustainability of a community‐based lifestyle modification educational program using telephone‐transmitted self–BP monitoring technology and nurse‐led counseling performed in a sample of patients with HBP. In this paper, we present a pattern of sustainability of the individual’s knowledge on self‐care skills and BP control 1 year after the group achieved the positive effect on these outcomes through short‐term education.
Methods
Design and Sample
The Self‐Help Intervention Program for HBP care (SHIP‐HBP) was a community‐based clinical trial designed to test the effects of a culturally tailored behavioral intervention in Korean Americans residing in the Baltimore‐Washington Metropolitan area. The SHIP‐HBP combined a 6‐week psychobehavioral education program with 12 months of BP self‐monitoring and telephone counseling conducted by bilingual nurses. Details about the study design were reported elsewhere. 20 In brief, the study employed a 2×2 factorial design with two key factors: a mode of education (ie, in‐class vs mail) and intensity of telephone counseling (ie, more‐intensive, biweekly counseling vs less‐intensive, monthly counseling). Participants in both counseling groups used BP self‐monitoring throughout the 12‐month counseling period (Figure 1). Study outcomes included systolic BP (SBP) and diastolic BP (DBP) levels and several psychosocial variables that were collected at baseline and at 3, 9, and 15 months (except for BP measurements made via self‐monitoring at home). The positive BP changes in study outcomes at the 3‐month follow‐up were also reported. 20 In the present paper, we report the study outcomes collected at 3 months through 15 months, during which the telephone counseling was offered.
Figure 1.
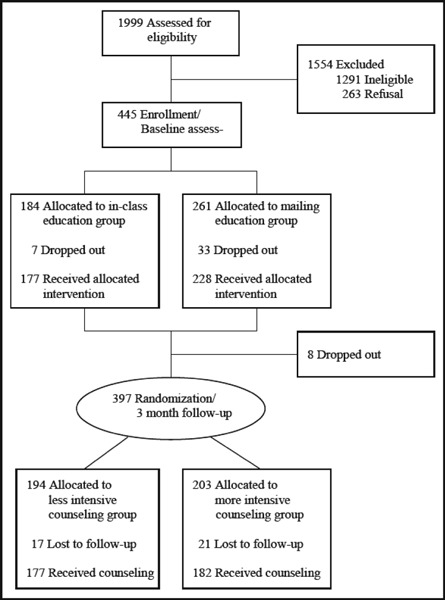
Participant tracking.
Eligibility criteria for the SHIP‐HBP trial included age 40 to 64 years, SBP ≥140 mm Hg and/or DBP ≥90 mm Hg on two separate occasions or taking antihypertensive medication, and self‐identification as a Korean American. At baseline, 445 eligible Korean Americans were recruited through ethnic churches, grocery stores, and ethnic newspaper advertisements. During the course of the clinical trial, 85 participants dropped out, resulting in 359 Korean Americans at the 15‐month follow‐up. There were no significant differences in sociodemographic characteristics between patients who remained in the study and those who dropped out.
Procedures
Study procedures were approved by the institutional review board and every participant provided written informed consent. During the baseline evaluation, trained bilingual nurses obtained 3 BP measurements at 1‐minute intervals, while demographic and psychosocial variables were measured via self‐report. Participants were then assigned to either the in‐class or the mail education groups to receive HBP‐related education for a 6‐week period. On completion of the 6‐week education, participants were given a BP monitor (A&D UA‐767; A&D Company, Ltd, Tokyo, Japan) equipped with a teletransmission system along with instructions. They were asked to measure their BP at home and transmit the BP data via phone during the following 6 weeks of the test period, during which it was made certain that all participants were able to measure and transmit their BP readings.
At 3 months (ie, at the end of the 6‐week test period), the Korean Americans were randomly assigned to either the more‐intensive counseling (MIC) or less‐intensive telephone counseling (LIC) groups. The MIC group received biweekly telephone counseling, while the LIC group received less‐frequent, monthly counseling by a trained bilingual nurse for 12 months. Trained nurse counselors made the phone calls from a private office at a local community center. As a safety measure, nurses called the participants regardless of the counseling schedule if the transmitted BP readings were ≥160/100 mm Hg and contacted a consulting physician on the study team. When the BP readings were ≥180/110 mm Hg, nurses either called the patient immediately to ask him/her to visit a nearby emergency department or called his/her physician. Nurses followed‐up with off‐schedule phone calls and then with an additional call within a week for updates.
During the counseling period, participants were instructed to measure their BP 3 times both on waking (am reading) as well as before retiring to bed at night (pm reading). The participants were asked to perform both sets of triplicate measurements ≥2 a week. The transmission device automatically saved up to 200 BP measurements. Nevertheless, in order to facilitate timely screening of abnormal BP readings and feedback, participants were asked to send their measurements via telephone once a week. Transmitted BP data was used to generate BP reports, which showed the time and frequency of both the BP measurements and BP readings. BP reports were made available to both the participant as well as the nurse counselor throughout the 12‐month counseling period.
Measurements
During the 12‐month counseling period, BP was measured at home by participants using the A&D UA‐767, which is a fully automatic device using the oscillometric method. Given varying numbers of BP measurements for each participant, it was determined that the biweekly means of SBP and DBP measurements be used to derive BP data for the current investigation (see details about compliance with home BP monitoring). In accordance with the guidelines laid out in the Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment and Control of High Blood Pressure (JNC 7), BP control was defined as home‐measured BP <135/85 mm Hg (130/85 mm Hg for patients with diabetes).
Other assessments included sociodemographic characteristics, insurance status, and medical history measured at baseline through the study questionnaire. In addition, psychosocial outcome variables were measured at baseline and at 3‐, 9‐, and 15‐month follow‐up. Specifically, HBP knowledge was assessed using 12 items developed by the National HBP Education Program of the National Heart Lung Blood Institute as well as by using 14 items generated by the investigative team based on the literature review. The HBP knowledge instrument has previously been used in Korean Americans. HBP beliefs were assessed using a 12‐item questionnaire. The questionnaire asked participants to indicate whether they believed certain behavioral factors could help lower their BP (ie, smoking, stress, weight, alcohol, salt, medication, coffee, diet, cholesterol, and exercise) and what the most important factors were in controlling their BP. HBP self‐efficacy was measured using a scale adapted from the HBP belief scale. The modified scale used 4‐point Likert‐type items asking how confident the person was in managing HBP in 11 different areas such as reducing salt intake, taking HBP medicines, or eating fatty foods less frequently. Higher scores indicated higher levels of self‐efficacy in the management of HBP. Depression was measured using the Kim Depression Scale for Korean Americans (KDSKA). The KDSKA contains 21 items that assesses depressive symptoms in the following 4 categories: emotional, cognitive, behavioral, and somatic. Each item is presented on a 4‐point Likert‐type scale as a declarative sentence related to one symptom of depression from the previous 1‐week period. Higher scores represented more depressive symptoms. Finally, medication adherence was measured through the medication subscale from the Hill‐Bone Compliance Scale. The scale consisted of 9 items on a 4‐point Likert‐type scale that measured the self‐reported degree of adherence to an HBP medication regimen. Higher scores indicated lower adherence.
Analysis
Only participants who self‐reported at least one BP measurement were included in the statistical analysis (N=359). Two BP outcomes (mean SBP and mean DBP measured biweekly) and 5 psychosocial outcomes (the mean scores of the HBP knowledge, HBP beliefs, HBP self‐efficacy, KDSKA, and Hill‐Bone Compliance Scale instruments measured at 3 follow‐up assessments) were modeled using mixed‐effects models to examine the rate of change over time, differences between intervention groups, and differences in the rates of change between intervention groups for each outcome. At each follow‐up, only patients who completed at least 6 of the 9 items on the Hill‐Bone Compliance Scale and taking BP medication were included in the adherence model (N=240). Each person could report up to 34 biweekly BP measurements during follow‐up. In total, 5408 biweekly BP observations were collected from 352 participants. The average number of measurements per participant was 15.4.
Nonlinear rates of change were considered for the BP models; however, the more parsimonious linear model was deemed sufficient via visual examination of the model diagnostics. Mixed‐effects models were implemented to account for the correlation induced by repeated measures. The models were adjusted for age, sex, marital status, education, work status, health insurance status, years of residence in the United States, BP medication status, family history of HBP, and years of HBP. All modeling was performed in R version 2.8.1 (R Development Core Team, 2008).
Results
Sample Characteristics
After the initial education period (approximately 3 months), there was no statistically significant difference in the variables between groups (Table I). The proportion of women was slightly more than that of men (47.1% men and 52.9% women) and the majority of participants (94.4%) were married. More than half (55.2%) of the participants had at least graduated college and 56.8% of all the participants held full‐time jobs. Less than 40% of the participants had medical insurance (39.8%) and more than 40% of the patients were not taking any BP medication (42.6%). A total of 74.7% of the participants had ≥1 family member with HBP and 14.8% had other diseases, such as diabetes and hyperlipidemia. The mean age was 51.9 years (range, 38–64 years), and mean period that the participants had HBP was 4.2 years.
Table I.
Sample Characteristics at Baseline
| Variable | Less‐Intensive Counseling (n=177) | More‐Intensive Counseling (n=182) | Total, No. (%) (N=359) |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Women | 94 (53.1) | 96 (52.7) | 190 (52.9) |
| Married | 167 (94.4) | 172 (94.5) | 339 (94.4) |
| College or more education | 88 (49.7) | 110 (60.4) | 198 (55.2) |
| Having a job | 107 (60.5) | 97 (53.3) | 204 (56.8) |
| Having medical insurance | 66 (37.3) | 77 (42.3) | 143 (39.8) |
| Taking HBP medication | 102 (57.6) | 104 (57.1) | 206 (57.4) |
| Family history of HBP | 131 (74.0) | 137 (75.3) | 268 (74.7) |
| Having other diseases | 28 (15.8) | 25 (13.7) | 53 (14.8) |
| Variable | Mean (±SD) | Mean (±SD) | Mean (±SD) |
| Age, y (38–64) | 52.0 (±5.8) | 51.8 (±5.7) | 51.9 (±5.7) |
| Years of HBP (<1–35) | 3.7 (±4.8) | 4.8 (±7.1) | 4.2 (±6.1) |
| Systolic BP (86–209)a | 142.1 (±17.7) | 145.5 (±15.9) | 142.3 (±16.8) |
| Diastolic BP (60–131)a | 90.9 (±10.8) | 91.5 (±10.5) | 91.2 (±10.7) |
| Depression (0–2.5) | 0.5 (±0.4) | 0.5 (±0.4) | 0.5 (±0.4) |
| Self‐efficacy (2.3–4.0) | 3.3 (±0.3) | 3.2 (±0.3) | 3.2 (±0.3) |
| Health beliefb (1–5) | 4.7 (±0.4) | 4.7 (±0.5) | 4.7 (±0.4) |
| HBP knowledge (0–1) | 0.7 (±0.2) | 0.7 (±0.2) | 0.7 (±0.2) |
| Medication adherence (1–3)c | 1.4 (±0.5) | 1.3 (±0.3) | 1.3 (±0.3) |
Abbreviations: BP, blood pressure; HBP, high blood pressure; SD, standard deviation. aData available for only 358 participants. bData available for only 357 participants. cAnalyzed with 176 participants who took antihypertensive medication and answered question about medication adherence on more than 6 items.
BP Outcomes
In the analysis of BP changes using repeated measures of the mixed‐effect model (Table II), on average, we found a decrease of 0.13 mm Hg (95% confidence interval [CI], 0.06–0.20) over every 2‐week period in the mean SBP of a typical individual in the group receiving the LIC, when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities. We observed an average decrease of 0.15 mm Hg (95% CI, 0.21–0.08) over each 2‐week period in the mean SBP of a typical individual in the group receiving the MIC, when controlling for all other covariates.
Table II.
Repeated‐Measures Mixed Linear Models With Blood Pressure Measured Biweekly Starting From 3‐Month Follow‐Upa
| Mean SBP (n=352,5408 Observations) | Mean DBP (n=352,5408 Observations) | |||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | |
| Intervention less intensive | ||||||
| More intensive | −1.25 | (−3.43 to 0.93) | .260 | −0.48 | (−2.05 to 1.09) | .549 |
| Time | −0.13 | (−0.20 to −0.06) | .000 | −0.07 | (−0.11 to −0.02) | .006 |
| Time × intervention less intensive | ||||||
| More intensive | −0.02 | (−0.12 to 0.07) | .666 | −0.05 | (−0.11 to 0.02) | .154 |
Abbreviations: CI, confidence interval; DBP, diastolic blood pressure; SBP, systolic blood pressure. aThe models were adjusted for the following covariates: age, sex, marital status, education, employment status, insurance coverage, years of high blood pressure, blood pressure medication use, family history, and comorbidities.
Similarly, we found an average decrease of 0.07 mm Hg (95% CI, 0.02–0.11) over every 2‐week period in the mean DBP of a typical individual in the LIC group when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities. We observed an average decrease of 0.11 mm Hg (95% CI, 0.16–0.07) over every 2‐week period in the mean DBP of a typical individual in the MIC group, when controlling for all other covariates.
In order to illustrate these BP changes in a more simplistic manner, we have compared baseline BP with follow‐up BP using the estimated BP value based on the most typical individual in each group controlling all other covariates (eg, age, marital status, education, employment, insurance, currently taking BP medication).
The baseline BP of the MIC group was 145.5/91.5 mm Hg. After the class intervention, a typical individual in the MIC group achieved a level of well‐controlled BP at 3 months (133.03/82.37 mm Hg). This trend was also maintained at both the 9‐month (131.15/81.69 mm Hg) and at 15‐month (130.26/81.01 mm Hg) follow‐up time points. Similarly, the baseline BP of the LIC group was 142.1/90.91 mm Hg and a typical individual from the group achieved a BP measurement of 133.28/82.85 mm Hg at the 3‐month follow‐up time point. The BP of a typical individual from the LIC group at the follow‐up time points were 132.53/82.45 mm Hg and 131.77/82.05 mm Hg at 9 months and 15 months, respectively (Table III).
Table III.
BP Outcomes at Baseline and 3‐, 9‐, and 15‐Month Follow‐Up
| Predicted SBP/DBP, mm Hga | ||||
|---|---|---|---|---|
| Baseline | 3 Months | 9 Months | 15 Monthsb | |
| Less intensive | 142.1/90.9 | 133.28/82.85 | 132.53/82.45 | 131.77/82.05 |
| More intensive | 145.5/91.5 | 132.03/82.37 | 131.15/81.69 | 130.26/81.01 |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure. aThe follow‐up blood pressure (BP) is estimated for a typical man of average age (51.9 years), married, completed at least some high school, employed, no insurance, has been on blood pressure (BP) medication for an average number of years (4.2 years), is currently taking BP medication, has a family history, and has no comorbidities. bPredicted BP values at 15 months are not calculated because fewer than half of the participants had observations at 15 months.
Monthly BP Control Rate
In order to assess the sustainability of maintaining controlled BP through our intervention strategies (counseling with teletransmitted home BP monitoring), after these individuals achieved initial BP control, the proportion of individuals with controlled BP during the 1‐year period were monitored on a monthly basis (Figure 2). The proportion of controlled BP for both groups (MIC and LIC) were well‐maintained (range, 57.13%–69.87%) during the 1‐year period. In fact, the proportion of control rates of both groups continually improved, whereas the MIC group showed a greater control rate (68.87%) than the LIC group (65.22%) at 15 months. The control rate of the MIC group at 3‐month follow‐up and the control rate of the LIC group was 57.13% and 57.71%, respectively.
Figure 2.
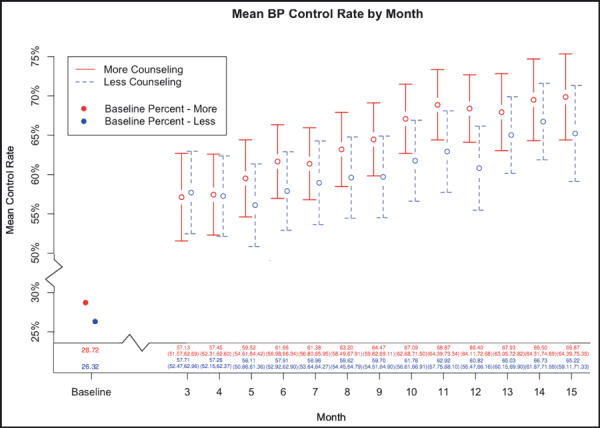
Mean blood pressure (BP) control rate by month.
Psychosocial Outcomes
We used repeated measures of mixed linear models to test the long‐term effects of the counseling intervention on relevant psychological variables and self‐help skills.
Depression. Depression scores for both counseling groups decreased over time. There were no statistically significant differences between groups, which indicates that the LIC was as effective as the MIC group. On average, we observed a decrease of 0.028 (95% CI, 0.051–0.005) in the mean depression score of participants in the LIC group and an average decrease of 0.027 (95% CI, 0.003–0.051) in the MIC group during every 6‐month period when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities (Table IV).
Table IV.
Repeated‐Measures Mixed Linear Models With Psychosocial Outcomes at 3‐, 9‐, and 15‐Month Follow‐Upa
| Depression (n=359; 1077 Observations) | Self‐Efficacy (n=359; 1076 Observations) | Health Belief (n=359; 1077 Observations) | HBP Knowledge (n=359; 1077 Observations) | Adherenceb (n=240; 634 Observations) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | |
| Intervention less intensive | |||||||||||||||
| More intensive | 0.00 | (−0.08 to 0.08) | .991 | −0.03 | (−0.09 to 0.03) | .311 | −0.05 | (−0.10 to 0.01) | .103 | −0.01 | (−0.02 to 0.01) | .633 | 0.01 | (−0.06 to 0.07) | .816 |
| Time | −0.03 | (−0.05 to −0.01) | .017 | 0.00 | (−0.02 to 0.02) | .659 | 0.02 | (0.00 to 0.04) | .090 | 0.01 | (0.01 to 0.02) | .000 | −0.05 | (−0.07 to −0.02) | .000 |
| Time × intervention less intensive | |||||||||||||||
| More intensive | 0.00 | (−0.01 to 0.01) | .730 | 0.01 | (0.00 to 0.01) | .010 | 0.00 | (0.00 to 0.01) | .615 | 0.00 | (0.00 to 0.00) | .537 | 0.02 | (−0.01 to 0.05) | .256 |
Abbreviations: CI, confidence interval; HBP, high blood pressure. aThe models were adjusted for the following covariates: age, sex, marital status, education, employment status, insurance coverage, years of high blood pressure, BP medication use, family history, and comorbidities (bMedication use not included in the adherence model because only those participants taking BP medication were included in the adherence model).
Self‐Efficacy. The evaluation of self‐efficacy using a repeated measure of the mixed‐effect model found that the perceived self‐efficacy was slightly increased over time for participants in the MIC group whereas it was slightly decreased in the LIC group. We observed an average increase of 0.003 (95% CI, 0.017 decrease to 0.022 increase) in the mean self‐efficacy score for participants in the MIC group and a decrease of 0.004 (95% CI, 0.023 decrease to 0.015 increase) during every 6‐month period when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities.
HBP Knowledge and Belief. The results of a mixed linear model using HBP knowledge as an outcome variable demonstrated that as a group, the participants retained the knowledge that they obtained via the structured education program more than a year ago. In fact, both groups with different frequencies of counseling demonstrated small increases in the HBP knowledge questionnaire. We observed an increase of 0.014 (95% CI, 0.007–0.021) in the mean knowledge score of participants in the LIC group and an average increase of 0.014 (95% CI, 0.007–0.020) in the MIC group during every 6‐month period when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities (Table IV).
Similarly, the mixed‐effect model using HBP‐related health beliefs also demonstrated small increases over time in both groups: we observed a mean score increase of 0.016 (95% CI, 0.003 decrease to 0.035 increase) in the LIC group and an average increase of 0.018 (95% CI, 0.002 decrease to 0.037 increase) in the MIC group during every 6‐month period when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities.
Nonadherence Score. Participants in both groups showed improvement in their adherence levels on HBP treatment recommendations including HBP medication‐taking, low‐salt diet, and appointment keeping behavior with his/her doctor. On average, we observed a decrease of 0.046 (95% CI, 0.024–0.069) in the mean nonadherence score of participants in the LIC group and an average decrease of 0.028 (95% CI, 0.006–0.050) in the MIC group during every 6‐month period when controlling for age, sex, marital status, education, employment status, insurance coverage, years of HBP, medications, family history, and comorbidities.
Discussion
The present study indicates that individualized counseling by bilingual nurses based on teletransmitted monitoring of home BP was effective in sustaining BP control achieved through a series of group HBP education programs during 12 months in hypertensive Korean Americans. Moreover, the findings of this study suggested that counseling strategy accompanied by home BP monitoring was successful for further improving BP control. While the exact dose response association was not quantified, the participants in the more‐counseled group improved their BP and psychosocial outcomes more than participants in the less‐counseled group. This pattern of steady improvement in BP outcomes is clinically meaningful because maintaining optimal BP over time directly leads to declines in stroke and coronary artery disease incidence and mortality. 21 , 22
The favorable results in the improvement of psychosocial outcomes such as the decrease of depressive symptoms are also noteworthy. Depression is known as an important correlate of critical self‐care behavior in HBP, such as adherence to treatment recommendations and self‐efficacy. 23
Another encouraging outcome of this counseling strategy that was illustrated in this evaluation was the retainment of HBP knowledge that was obtained by participants after a 6‐week HBP cluster education program. As reported in our previous paper that described our 3‐month follow‐up results that immediately followed the cluster education, an individual’s knowledge of HBP was significantly increased after the education. 20 The present study demonstrated that the level of improved HBP knowledge was sustained after 15 months of intervention (from the point of baseline measurement). Based on this result, it is safe to conclude that regular feedback from a nurse counselor can act as a continuing booster intervention to maintain the participants’ knowledge of HBP. Nonadherence was also shown to improve at 15 months, which included HBP medical treatment, low‐sodium diet, and appointment‐keeping behavior with his/her doctor. However, we could not find a dose‐effect relationship between telephone counseling intensity and self‐care behavior despite both groups showing improvement in health behaviors. 24
Home BP monitoring has been well investigated as an intervention for improving BP control. 25 , 26 , 27 , 28 BP measurement seems to improve BP recognition, which may lead to improved BP medication adherence and better BP control. Because both groups (MIC group vs LIC group) received teletransmitted BP monitoring, we could not make any inference on the independent effect of home BP monitoring on BP outcomes.
The sustaining pattern of significant improvements and of BP outcomes for both groups during a relatively long period, however, highlights the potential efficacy of the combined strategy with counseling and home BP monitoring in maintaining optimal BP levels for a long period. It seems that the self‐monitoring of BP provides a certain level of biofeedback, 29 which also helps to motivate the individual toward staying with desirable behaviors for maintaining or improving BP outcomes such as medication adherence and subscribing to a healthy lifestyle. 30
While our study is the first study of its kind to test the efficacy of a combined strategy (counseling and home BP monitoring) in producing long‐term sustainability of optimal BP outcomes, positive short‐term outcomes of tailored telephone counseling by a nurse have been reported in the literature. 31 , 32 , 33 , 34 , 35 As with other studies, our individual counseling includes problem‐solving in regards to BP measurement, medical treatment, and maintaining a healthy lifestyle (eg, diet, exercise, weight control, smoking cessation, and limited alcohol consumption). A unique characteristic of our counseling protocol was that all counseling was conducted by trained bilingual nurses. Given that the participants of this study were first‐generation immigrants facing significant language barriers when using mainstream resources, the culturally tailored education messages delivered and discussed with bilingual nurses were well received by the participants. The detailed information regarding our counseling protocol was reported elsewhere. 24
Limitations
The limitations of our study are as follows: First, because of the lack of a true control group, our inferences were strictly based on relative assessment rather than an absolute comparison between the intervention and control groups. In addition, because our intervention was multifaceted and not individually compared, we could not come to any precise conclusions on which parts of the strategy (counseling vs home BP monitoring) were the most important for yielding desirable long‐term BP outcomes.
Conclusions
The findings of this study suggest that the combined strategy of counseling and home BP monitoring is an effective strategy for improving long‐term BP outcomes for individuals. In particular, the strategies we used in this study can inform researchers and clinicians who want to find community‐based evidence materials that deliver high‐quality, equitable care for increasingly diverse patient populations.
Acknowledgement:
This research was supported by a grant from the Agency for Healthcare Research and Quality (R01 HS13160, Clinical Trials Registry NCT00473681) and the Johns Hopkins University School of Nursing Center for Excellence in Promoting Cardiovascular Health for Vulnerable Populations (funded by National Institute of Nursing Research P30 NR011409).
References
- 1. Institute of Medicine (IOM) . A population‐based policy and systems change approach to prevent and control hypertension. http://www.iom.edu/Reports/2010/A‐Population‐Based‐Policy‐and‐Systems‐Change‐Approach‐to‐Prevent‐and‐Control‐Hypertension.aspx. Accessed November 11, 2010. [PubMed]
- 2. Chobanian AV. Control of hypertension – an important national priority. N Engl J Med. 2001;345:534–535. [DOI] [PubMed] [Google Scholar]
- 3. Qureshi AI, Suri MF, Kirmani JF, et al. Prevalence and trends of prehypertension and hypertension in United States: national health and nutrition examination surveys 1976 to 2000. Med Sci Monit. 2005;11:CR403–CR409. [PubMed] [Google Scholar]
- 4. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third national health and nutrition examination survey. JAMA. 2002;287:356–359. [DOI] [PubMed] [Google Scholar]
- 5. Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill‐Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15:90–96. [DOI] [PubMed] [Google Scholar]
- 6. Klatsky AL. Alcohol, coronary disease, and hypertension. Annu Rev Med. 1996;47:149–160. [DOI] [PubMed] [Google Scholar]
- 7. He J, Klag MJ, Whelton PK, et al. Migration, blood pressure pattern, and hypertension: the Yi migrant study. Am J Epidemiol. 1991;134:1085–1101. [DOI] [PubMed] [Google Scholar]
- 8. Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. West J Nurs Res. 2006;28:190–209; discussion 210–215. [DOI] [PubMed] [Google Scholar]
- 9. Hamilton G, Toberts S, Johnson J, et al. Increasing adherence in patients with primary hypertension: an intervention. Health Values. 1993;17:3–11. [Google Scholar]
- 10. Martinez‐Amenos A, Fernandez Ferre ML, Mota Vidal C, et al. Evaluation of two educative models in a primary care hypertension programme. J Hum Hypertens. 1990;4:362–364. [PubMed] [Google Scholar]
- 11. Hunt JS, Siemienczuk J, Touchette D, et al. Impact of educational mailing on the blood pressure of primary care patients with mild hypertension. J Gen Intern Med. 2004;19:925–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hennessy S, Leonard CE, Yang W, et al. Effectiveness of a two‐part educational intervention to improve hypertension control: a cluster‐randomized trial. Pharmacotherapy. 2006;26:1342–1347. [DOI] [PubMed] [Google Scholar]
- 13. Roca‐Cusachs A, Sort D, Altimira J, et al. The impact of a patient education programme in the control of hypertension. J Hum Hypertens. 1991;5:437–441. [PubMed] [Google Scholar]
- 14. Zismer DK, Gillum RF, Johnson CA, et al. Improving hypertension control in a private medical practice. Arch Intern Med. 1982;142:297–299. [PubMed] [Google Scholar]
- 15. Tanner GA, Noury DJ. The effect of instruction on control of blood pressure in individuals with essential hypertension. J Adv Nurs. 1981;6:99–106. [DOI] [PubMed] [Google Scholar]
- 16. McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. BMJ. 2005;331:493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Halme L, Vesalainen R, Kaaja M, et al., HOme MEasuRement of blood pressure study group . Self‐monitoring of blood pressure promotes achievement of blood pressure target in primary health care. Am J Hypertens. 2005;18:1415–1420. [DOI] [PubMed] [Google Scholar]
- 18. Rogers MA, Small D, Buchan DA, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension. A randomized, controlled trial. Ann Intern Med. 2001;134:1024–1032. [DOI] [PubMed] [Google Scholar]
- 19. Rudd P, Miller NH, Kaufman J, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17:921–927. [DOI] [PubMed] [Google Scholar]
- 20. Kim MT, Kim EY, Han HR, et al. Mail education is as effective as in‐class education in hypertensive Korean patients. J Clin Hypertens. 2008;10:176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brown RD, Whisnant JP, Sicks JD, et al. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke. 1996;27:373–380. [PubMed] [Google Scholar]
- 22. McGovern PG, Burke GL, Sprafka JM, et al. Trends in mortality, morbidity, and risk factor levels for stroke from 1960 through 1990. The Minnesota heart survey. JAMA. 1992;268:753–759. [PubMed] [Google Scholar]
- 23. Kim MT, Han HR, Hill MN, et al. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. [DOI] [PubMed] [Google Scholar]
- 24. Han HR, Kim J, Kim KB, et al. Implementation and success of nurse telephone counseling in linguistically isolated Korean American patients with high blood pressure. Patient Educ Couns. 2010;80:130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Artinian NT, Flack JM, Nordstrom CK, et al. Effects of nurse‐managed telemonitoring on blood pressure at 12‐month follow‐up among urban African Americans. Nurs Res. 2007;56:312–322. [DOI] [PubMed] [Google Scholar]
- 26. Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient‐tailored multifactorial intervention. Patient Educ Couns. 2005;57:5–14. [DOI] [PubMed] [Google Scholar]
- 27. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. A randomized controlled trial during 6 months. Blood Press. 2008;17:78–86. [DOI] [PubMed] [Google Scholar]
- 29. Campbell NR, Bass M, Chockalingam A, et al. Self‐measurement of blood pressure: benefits, risks and interpretation of readings. The Canadian coalition for high blood pressure prevention and control. Can J Cardiol. 1995;11(Suppl H):18H–22H. [PubMed] [Google Scholar]
- 30. Reims H, Fossum E, Kjeldsen SE, et al. Home blood pressure monitoring. Current knowledge and directions for future research. Blood Press. 2001;6:271–287. [DOI] [PubMed] [Google Scholar]
- 31. Woodward A, Wallymahmed M, Wilding J, et al. Successful cardiovascular risk reduction in type 2 diabetes by nurse‐led care using an open clinical algorithm. Diabet Med. 2006;23:780–787. [DOI] [PubMed] [Google Scholar]
- 32. Woollard J, Beilin L, Lord T, et al. A controlled trial of nurse counselling on lifestyle change for hypertensives treated in general practice: preliminary results. Clin Exp Pharmacol Physiol. 1995;7:466–468. [DOI] [PubMed] [Google Scholar]
- 33. Woollard J, Burke V, Beilin LJ. Effects of general practice‐based nurse‐counselling on ambulatory blood pressure and antihypertensive drug prescription in patients at increased risk of cardiovascular disease. J Hum Hypertens. 2003;17:689–695. [DOI] [PubMed] [Google Scholar]
- 34. McLean DL, McAlister FA, Johnson JA, et al., SCRIP‐HTN Investigators . A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists‐hypertension (SCRIP‐HTN). Arch Intern Med. 2008;168:2355–2361. [DOI] [PubMed] [Google Scholar]
- 35. Kastarinen MJ, Puska PM, Korhonen MH, et al., LIHEF Study Group . Non‐pharmacological treatment of hypertension in primary health care: a 2‐year open randomized controlled trial of lifestyle intervention against hypertension in eastern Finland. J Hypertens. 2002;20:2505–2512. [DOI] [PubMed] [Google Scholar]


