Abstract
J Clin Hypertens (Greenwich). 2011;13:543–550. ©2011 Wiley Periodicals, Inc.
The Hypertension Initiative began in 1999 to help transition South Carolina from a leader in cardiovascular disease (CVD) to a model of heart and vascular health. Goals were to reduce heart disease and stroke by 50% by promoting healthy lifestyles and access to effective care and medications. Continuing medical education was used to train providers, encourage physicians to become American Society of Hypertension (ASH)–certified hypertension specialists and recruit practices into the community‐based practice network (CBPN). Practice data audit with provider specific feedback is a key quality improvement tool. With ASH support, the CBPN has grown to 197 practices with approximately 1.6 million patients (approximately 700,000 hypertensives). Clinical data are obtained from electronic health records and quarterly provider feedback reports are generated. Hypertension, hypercholesterolemia, and diabetes control rose and South Carolina’s ranking improved from 51st to 35th in CVD mortality from 1995 to 2006. The Hypertension Initiative expanded to the Outpatient Quality Improvement Network (O’QUIN) to encompass comparative effectiveness research and other chronic diseases. Lessons learned include: trust enables success, addressing practice priorities powers participation, infrastructure support must be multilateral, and strategic planning identifies opportunities and pitfalls. A collaborative practice network is attainable that produces positive, sustainable, and growing impacts on cardiovascular and other chronic diseases.
Unlike manufacturing and other businesses such as the airline industry that work to continuously improve the quality and safety of their products and services, the health care “industry” has struggled to implement innovations that improve health care safety, outcomes, and efficiency. 1 Practice networks were developed in the 1970s to improve health care through ongoing quality improvement and/or practice‐based research. 2 Many practices successfully implemented new guidelines and tested new treatments in primary care settings where they are most often used. 3 , 4 The National Institutes of Health (NIH) Clinical Translational Science Awards (CTSAs) embraced practice networks as a key mechanism to speed implementation of evidence‐based practice to the community and as a critical resource for comparative effectiveness research. 5
The Outpatient Quality Improvement Network (O’QUIN), located at the Medical University of South Carolina (MUSC), began as a community practice network focused on cardiovascular disease (CVD). Known as the Hypertension Initiative from 1999 to 2009, it exemplifies a practice network that has seen improvements in quality indicators. For example, this network documented an improvement in blood pressure (BP) control of <140/90 mm Hg in 208,547 hypertensive patients from 49% in 2000 to 66% in 2005. Among 82,442 patients with diabetes, dyslipidemia, and hypertension, glycosylated hemoglobin <7% improved from 49% to 54%, low‐density lipoprotein cholesterol (LDL‐C) <100 mg/dL rose from 38% to 57%, and BP <130/80 mm Hg advanced from 22% to 35%. 6 The network database has grown to approximately 1.7 million patients seen in the past 5 years (Table I). The database has supported needs assessment for and outcomes of continuing medical education (CME), enabled peer‐reviewed publications documenting various outcomes and ongoing need for improvement, and provided the foundation with comparative effectiveness research. 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 The addition of a data analyst (YZ) provides opportunities for comparison of O’QUIN findings to national databases and to conduct more in‐depth analyses. 20
Table I.
Descriptive Characteristics and Blood Pressure Distribution Among Hypertensives and Nonhypertensives Seen at a Clinical Practice in O’QUIN from 2005 to 2010a
| Hypertensives (n=692,287) | Nonhypertensives (n=954,419) | P Valueb | |
|---|---|---|---|
| Age, y | 61.0±16.2 | 39.7±20.6 | <.001 |
| Sex, male:female, % | 67.7:32.3 | 47.9:52.1 | <.001 |
| Race/ethnicity, white:black, % | 63:37 | 67:33 | <.001 |
| Weight, kg | 91.3±25.8 | 79.1±29.3 | <.001 |
| Systolic BP, mm Hg | 133.7±20.8 | 118.5±16.2 | <.001 |
| Diastolic BP, mm Hg | 78.1±13.1 | 72.1±11.0 | <.001 |
| Stage 2 HTN, ≥160/≥100 mm Hg, % | 13.1 | 0 | <.001 |
| Stage 1 HTN, 140–159/90–99, % | 24.5 | 14.3 | <.001 |
| Pre‐HTN, 120–139/80–89, % | 43.4 | 39.1 | <.001 |
| Normal, <120/<80, % | 18.9 | 46.7 | <.001 |
| Diabetes mellitus, % | 29.3 | 3.7 | <.001 |
| Hyperlipidemia, % | 66.7 | 14.6 | <.001 |
| LDL cholesterol, mg/dL | 100.1±34.7 | 111.6±34.9 | <.001 |
| Tobacco use/dependence, %c | 15.0 | 4.7 | <.001 |
| Cardiovascular disease, %d | 25.6 | 2.7 | <.001 |
Abbreviations: BP, blood pressure; HTN, hypertension; LDL, low‐density lipoprotein; O’QUIN, Outpatient Quality Improvement Network. aData captured in discrete fields of various electronic health record systems. b P values generated using appropriate 2‐sample unpaired tests. c International Classification of Diseases, Ninth Revision (ICD‐9) 305.1, V15.82. dCardiovascular disease includes: ICD‐9 410–414, 428, and 431–438 and includes peripheral vascular disease 250.7, 400.2, and 443.9.
Despite the success, our network has experienced challenges described by others, including ongoing funding and coping with changes in new technology and in the practices themselves. 21 Some of our approaches to implement quality improvements across the network have proven successful in addressing challenges and may have contributed to positive outcomes.
In 1995, South Carolina ranked 51st (ranking included Puerto Rico and Washingon, DC) in the United States for deaths from heart disease and stroke. 22 South Carolina was a perennial leader in stroke mortality since 1930 and was known as the “buckle” of the “stroke belt.” 23 The Hypertension Initiative began with the mission of facilitating the transition of South Carolina from a leader in CVD to a model of heart and vascular health (Figure 1). The goals were to reduce heart disease and stroke by 50% and improve overall health. 24 , 25
Figure 1.
The Outpatient Quality Improvement Network (O’QUIN) logo was designed to capture the twin strategies: namely, healthy lifestyle, ie, physical activity and good nutrition, and access to effective health care and essential medications. These two strategies were designed to address the goals and realize the mission. CVD indicates cardiovascular disease.
Two key challenges in building a community practice‐based network are establishing trust and funding. The network began and has grown without a consistent source of funding. In 1999, the pharmaceutical industry supported the Experts in Hypertension Seminar Series with a 3‐fold purpose (Figure 2). The series was designed for the state’s roughly 2200 full‐time primary care physicians, since they were caring for most of the approximately 1 million hypertensive patients in South Carolina. From 1999 to 2002, the Hypertension Seminar Series attracted approximately 600 primary care providers, or roughly 25% of the primary care workforce. Doctors Lackland and Basile continue to play a major role in the Seminar Series through the American Society of Hypertension’s (ASH’s) Carolina‐Georgia‐Florida chapter, which assumed the main responsibility for hypertension CME in the region after 2001. 6
Figure 2.
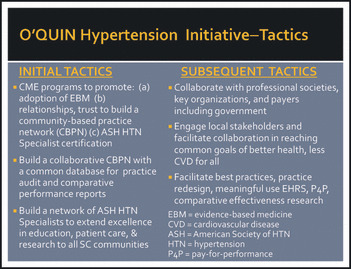
The initial set of tactics were designed to implement and grow the community‐based practice network beginning with continuing medical education (CME) program that could enhance the practice of evidence‐based medicine, prepare interested providers for the American Society of Hypertension Clinical Specialists Examination, and to develop the relationships and trust required to build a sustainable practice‐based network focused on quality improvement in CVD risk management. The subsequent tactics expanded the reach and scope of Outpatient Quality Improvement Network (O’QUIN) to effect improvements in both lifestyle and medical approaches to CVD prevention and health promotion.
The relationships developed during the Seminar Series identified physicians interested in CVD prevention through evidence‐based risk factor management. Two focus groups, conducted with these physicians in different regions of South Carolina, secured their commitment to building a common database to facilitate quality improvement through practice data audit and feedback reporting. Since none of these physicians in 1999 had electronic health record systems (EHRS), they agreed to complete data cards at each hypertensive patient visit.
Methods and Operations
Data cards from the first practice were mailed to MUSC for manual input for patients with hypertension. Data included demographics, height/weight, smoking, history of cardiovascular or chronic kidney disease, and values for BP, glycosylated hemoglobin (HbA1C), LDL‐C, and all medications used to treat hypertension, hyperlipidemia, and diabetes. The structure and function of the network began to take shape in 2000 when AstraZeneca funded the Hypertension Initiative. In 2000 to 2002, grants from the State of South Carolina and the Duke Endowment supported the growing audit and feedback report to reduce disparities in the control of hypertension and other cardiovascular risk factors. A project manager (KE) was hired to coordinate meetings, contacts with practices, and grants management. As more practices joined the network and began adopting EHRSs, two talented programmers enabled us to collect medical summary data from different EHRSs (SW, JB).
In 2003, ASH funded the Hypertension Initiative to include practices in North Carolina and Georgia as a key activity of its Carolina‐Georgia chapter. In 2004, a grant from the US DHHS funded the Stroke Belt Initiative, a 4‐county strategic plan, lifestyle intervention, and practice‐based quality improvement effort to mitigate hypertension and stroke. Through an agreement with the Veterans Affairs Clinics in South Carolina, Georgia and Alabama, all VISN‐7 sites participated in the Hypertension Initiative. By 2006, 197 practices joined the network, approximately half of which were located in South Carolina, with others in Georgia, Alabama, Tennessee, North Carolina, and Virginia. Participating clinical sites included single‐ and small‐group physician practices, multi‐site privately managed and hospital‐managed clinic networks, federally qualified health centers, free clinics, academic university–based and community‐based training programs, and Veterans Affairs clinics. The clinical sites were and continue to be virtually entirely primary care practices, with the majority of providers being family physicians, general internists, general practitioners, and nurse clinicians.
In 2007, the Hypertension Initiative became a state line item in the MUSC budget, enabling us to expand our support staff. MUSC was a recipient of the CTSA in 2009, and while the network did not receive direct funding, the Community Engagement Core Director (ML) participated in focus group discussions to learn more about how practices view the network and to assist in the development of new collaborative proposals. In 2010, ASH provided financial support to expand the clinical practice network beyond the Carolinas‐Georgia‐Florida chapter. Several activities, such as practice recruitment and retention, the novel database that enables the audit and feedback report, promotion of ASH clinical hypertension specialists, the ASH CME‐accredited quarterly newsletter, and our Business Associate Agreement, are critical to a successful infrastructure.
Practice Recruitment and Retention
Practice recruitment began slowly initially as physicians attended CME programs and learned about the hypertension network. Trust became the currency that allowed the network to grow and function. Open and honest communication, initiatives based on needs of the practices, and confidential reporting were keys to maintaining trust among members. Hiring an outreach coordinator sped up the recruitment process (SM). In the 11 years of the network, fewer than 15 practices have left. Most were very small practices without EHRSs and found completing the data cards to be burdensome.
Patient Database
Once a clinic joins the network, an EHRS specialist visits the clinic to identify the EHRS product and how it is used. Various EHRS products are used by participating clinics, including SSIMed, GE Logician/Centricity, Practice Partner, eClinicalworks, MySys, Allscripts, Medinformatix, and Vista. Most EHRS store all data in a standard structured query language–based database. With access to the database, the EHRS specialist develops queries to extract all data of interest and a data import specialist cleans and normalizes data. For example, all height values are converted to meters and all prescriptions are rewritten to their generic equivalent with discrete dosage and frequency information. Values outside a valid range are omitted.
Some areas of data normalization are trivial while others require extensive oversight. For example, numeric values can be difficult when the unit or exact description is unknown. Currently, more attention is directed toward identifying and resolving issues with the completeness and accuracy of data capture. In addition, practice IT staff change, as do lead physicians and practice managers. Several practices changed EHRSs. Many hours are spent meeting with the IT department and other staff at participating practices, discussing what data are collected and how it is labeled, and, in building a relationship of trust between the clinics and the O’QUIN IT team.
Future growth is focused on increasing the number of practices, while increasing efficiency by reducing the time required to normalize data. Many new EHRSs are easily included. However, some vendors offer no assistance in understanding their proprietary data structure, which magnifies the time required to systematically decode the required information.
Practice Data Audit and Provider‐Specific Feedback Reporting
Strategies for improving provider performance include CME, academic detailing and coaching, audit and feedback, influential physicians (opinion leaders), and team change. 26 Given resource limitations, it was critical to select initial strategies that were simple, inexpensive, and highly scalable. The strategies selected were CME (Experts in Hypertension Seminar Series), audit and feedback, and influential physicians. The decision to adopt audit and feedback was based on a report from the University of Pennsylvania practice network.
The Penn Network began with a documented baseline hypertension control of 19%. Each physician in the network was provided with a copy of the then current hypertension guidelines. Quarterly practice data audit and feedback reporting to each physician was also provided. One year later, hypertension control improved to 53%. 27 While the literature suggests a moderate effect size for audit and feedback, 28 this was an impressive result. The challenge we faced was adapting a strategy that was successfully utilized in a largely urban setting to a less‐densely populated state with practices distributed over more than 30,000 square miles.
Our physician focus groups indicated interest in an audit and feedback program with centralized data management and reporting. The database has proved useful for needs assessment in professional education and for identifying areas for improvement, eg, frequency of care, laboratory monitoring, therapeutic inertia, and evidence‐based prescribing. For example, projections from 2003 data suggested that therapeutic inertia accounted for 19% of the variance in BP control and that control in the patient group analyzed would improve from 45% to 66% if therapeutic inertia was overcome on 30% of visits with uncontrolled BP. In order to reach this goal, we include therapeutic inertia metrics for individual providers on their audit report and emphasize the importance of this topic in our various educational venues.
Hypertension Specialists (Influential Physicians)
From the outset, hypertension specialists for ASH were to serve three critical roles, including patient care, education, and research. Through the Experts in Hypertension Seminar Series and personal relationships, physicians with a passion for hypertension control in their patients and community were encouraged to take the ASH examination to become clinical hypertension specialists. In addition to providing state‐of‐the‐art control of cardiovascular risk factors to their own patients and referral patients, the hypertension specialists were encouraged and supported to become educators and to take a leadership role to improve hypertension control in their practice setting and community through their educational activities health services research.
Efforts to increase the number of ASH‐certified hypertension specialists expanded throughout the ASH Carolinas‐Georgia‐Florida chapter. Figure 3 shows the number and distribution of ASH hypertension specialists in the 4 member states. South Carolina has achieved one of the highest ratios of hypertension specialists per capita in the United States (Table II). The growth in hypertension specialists in South Carolina was facilitated by a $5000 incentive paid from BlueCross BlueShield of South Carolina to physicians who passed the certifying examination. Hypertension specialists in South Carolina are distributed throughout the state and not only concentrated in urban settings as in many other states. The more equitable geographic distribution of hypertension specialists in South Carolina represents progress toward our original goal of having at least one hypertension specialist in every county of the state, although the goal of having a ratio of one specialist to every 20 primary care providers remains unmet. 7
Figure 3.
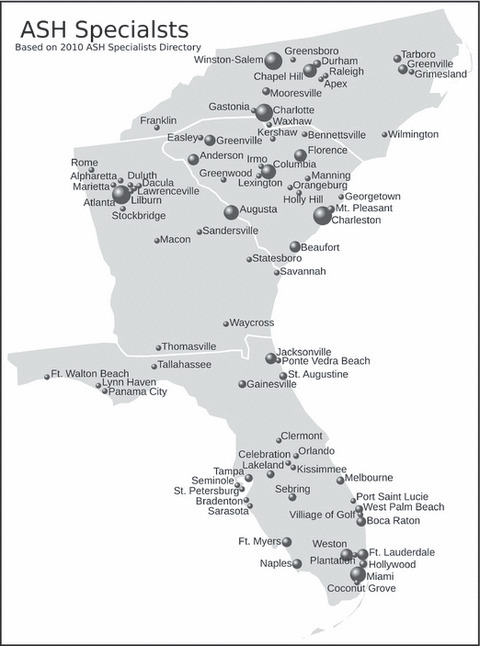
Geographic location of American Society of Hypertension (ASH)–certified clinical hypertension specialists in the Carolinas‐Georgia‐Florida chapter. The area of the black circles is proportional to the number of hypertension specialists in a city/town.
Table II.
American Society of Hypertension’s Hypertension Specialists in the Carolinas‐Florida‐Georgia Chapter
| State | Population | Hypertension Specialists , No. | Population/Specialist |
|---|---|---|---|
| Florida | 18,537,969 | 64 | 289,656 |
| Georgia | 9,829,211 | 33 | 297,855 |
| North Carolina | 9,380,884 | 41 | 228,880 |
| South Carolina | 4,561,242 | 47 | 97,048 |
Business Associate Agreement
The Health Insurance Portability and Accountability Act (HIPAA) was passed on August 21, 1996. Congress recognized that standardizing the collection and payment of medical claims could infringe on patient confidentiality. Thus, HIPAA legislation included a provision to increase and standardize health data security. Access to patient information was limited to the minimum necessary for a defined medical purpose by authorized individuals. In April 2001, the Hypertension Initiative began exploring HIPAA implications for the network and the means for insuring compliance. We recognized that a single HIPAA violation could jeopardize the entire operation and that clinics would be hesitant to join if there was a significant perceived risk of a HIPAA violation. Thus, the initiative dedicated one individual to work with the institutional review board and legal counsel for MUSC and individuals at the Commission on Medicare and Medicaid Services (CMMS) who were knowledgeable about HIPAA to develop a plan and documentation to ensure HIPAA compliance.
Between May 2001 and April 2003, a Business Associate Agreement (BAA) was developed that met the intent and letter of HIPAA, while allowing the quality improvement and research aspects of the initiative to proceed. In brief, the BAA established the Hypertension Initiative as a business associate for quality improvement, which meets the definition of a Treatment, Payment, and Operations (TPO) relationship. The TPO relationship allows sharing of protected health information without patient consent—in this case, for health care quality. The BAA also includes a provision for using de‐identified health information, with masked identifiers for serial tracking, research, and general reporting purposes.
Newsletter
Each provider’s quarterly feedback report is accompanied by a 4‐page newsletter summarizing evidence‐based advances in managing hypertension, hyperlipidemia, and diabetes. The newsletter addresses topics such as patient adherence and lifestyle changes as well as needs identified in the database, eg, therapeutic inertia and treatment‐resistant hypertension. The newsletter was recently approved for CME credit by ASH. Physicians answer questions online to receive CME credit. The percentage of correct responses and identifying information are automatically forwarded to ASH. A statement of education credit is sent electronically to physicians who pass the post‐test. As our scope has expanded, the newsletter addresses other topics of interest, eg, health information exchange, pay‐for‐performance, and cost‐efficient approaches to patient lifestyle counseling.
Strategic Analysis
As the value of the network and its successes became better known, new opportunities emerged allowing the Hypertension Initiative to expand its focus and approach. As a result, we renamed it O’QUIN to better fit current and future activities. These activities include or will include: (1) expansion to other chronic diseases through collaboration with relevant clinical experts, (2) promotion of team change, (3) adoption of healthy lifestyles and improved adherence of patients, (4) implementation of a wide range of comparative effectiveness research trials, and (5) development of a biorepository to support genetic epidemiology and pharmacogenomics with input and participation from experts in multiple disciplines. In light of these new initiatives, we undertook a strategic planning initiative to assess the current environment of the O’QUIN team, the network itself, and the dynamic nature of the provision of primary care with a view toward the future.
Practice and Network Environment
Focus group discussions were held at 5 practices of various sizes and locations across South Carolina, and O’QUIN team members were individually interviewed to glean an ethnographic picture of the program and support an updated strategic plan. Focus group discussions were approved by MUSC’s institutional review board.
Network Perspective. O’QUIN is guided by a medical director with a passion for improving treatment and control of hypertension and related chronic disease. Several physicians commented that their chief incentive for participating was to be part of a process that helped them provide the highest quality care in order to improve patient outcomes. All pointed to the medical director with his expertise and passion for controlling hypertension and their trust in him to protect their medical data as another key to participation. The practices participate in the design of the products of the network and how data will be collected and shared. Their input is sought for the content and design of the feedback reports, newsletter, and new initiatives and to evaluate how well the network is meeting their needs. Based on comments in the focus groups and telephone calls to MUSC inquiring about changes in various rates, providers in the practices are reading their audit and feedback reports. Most lead physicians interviewed share the practice audit and feedback report with staff, while others use their personal report, compared with the network as a whole, to spur changes in care delivery, especially that related to therapeutic inertia. The current economy and ongoing changes in practice standards, new technology, and reimbursement are sources of stress for most practices. Stress is evident in early retirements of some lead physicians, cost‐cutting, and other staff changes. Despite this, practices are eager to improve their quality‐outcome indicators and want more educational opportunities.
O’QUIN Team
The dynamic nature of the network requires ongoing adjustments by the MUSC team. Weekly meetings update MUSC team members on activities, challenges, and changes in funding and facilitate collective problem‐solving in working with practices to improve quality. The team is small for a project of this size, but one key to their efficiency is that they all respect each other and share a common vision and mission.
We asked team members to list the major strengths, weaknesses, opportunities, and threats (SWOT analysis) to the ongoing success of O’QUIN. Results are seen in Table III. A strategic plan was developed that takes advantage of the strengths and opportunities, while addressing weaknesses and threats. Ongoing funding has always been a need. Expanding network activities to address all health conditions and collaborating with faculty with expertise in conditions deemed important to the practices has brought new resources into O’QUIN. For example, two new NIH grants with colleagues from nursing were recently funded. Practices are eager to participate in more research, as long as resources are shared, practices are compensated, and a focus on quality improvement is maintained. Other resource opportunities included participating in a medical insurance–supported pay‐for‐performance demonstration project and linking with our regional extension center to support the adoption and implementation of EHRSs in rural practices and designing approaches to health information exchange (HIE) and meaningful use tailored to the resources of the broad array of individual practices in O’QUIN.
Table III.
SWOT Analysis on the Future of O’QUIN
| Strengths | Weaknesses | Opportunities | Threats |
|---|---|---|---|
| Strong medical director | Diverse EHRS | Interprofessional collaboration leads to creative new ideas | Lack of funding |
| Trust in MUSC team | Practices that lack training in their EHRSs | New expansion beyond CVD | Rapidly evolving practice landscape: EHRSs, HIE, reimbursement, physician champion leaves a practice, new policies, new players in state/region who do not understand the state or practices |
| Growing number of practices | Practice IT lack time or interest in database | Add more practices | Not delivering on promises |
| Practices interested in quality improvement | Poor bandwidth in rural areas | Clinical trials conducted in network | |
| Evidence of success | Growing volume of work | New technology leading to HIE and efficiency | |
| Growing interest at MUSC in O’QUIN | Need for more funding | Comparative Effectiveness Research | |
| Strong/unique IT program | Ongoing changes in practice personnel requiring orientations | Growing interest in PBRNs in United States | |
| Business Associate Agreement | Medical director essential to success of network | ||
| Change in laboratory results in missing data | |||
| Some PCPs tired and burned‐out |
Abbreviations: CVD, cardiovascular disease; EHRS, electronic health record system; HIE, health information exchange; IT, information technology; MUSC, Medical University of South Carolina; O’QUIN, Outpatient Quality Improvement Network; PBRNs, practice‐based research networks; PCP, primary care physicians; QI, quality improvement; SWOT, Strengths, Weaknesses, Opportunities and Threats.
Rural practices are least likely to implement HIE. 29 Our practices are no exception. Many cannot afford the cost of purchasing and maintaining EHRSs and the loss of productivity that comes with implementing new systems. Stories of EHRSs that failed to provide promised services have circulated among our practice network and physicians are somewhat wary of new initiatives. Based on past work together, our network practices are asking us to position them to take advantage of new opportunities in EHRSs, HIE, and practice redesign that may ultimately lead to improved efficiency and better outcomes from evidence‐based patient care. As a result, O’QUIN was restructured under articles of collaboration that defined an executive committee composed of MUSC and practice representatives charged with managing the future direction of the network. This governing body has established criteria for conducting research within the network and planned an annual conference.
Discussion
The key lessons learned from the evolution of this practice network are: (1) trust, developed over many years, is the currency that leads to any success; (2) direction of O’QUIN is based on the active participation of all the parties and focused on the needs and priorities of the practices; (3) support for the infrastructure must come from multiple sources; and (4) ongoing strategic planning is essential to uncover new opportunities, while avoiding the many pitfalls.
Practice‐based research networks are growing across the United States as they demonstrate success in improving quality of care and patient outcomes, two key incentives for primary care providers. 2 , 21 , 30 Policies related to reimbursement based on performance and requirements for EHRS and HIE is speeding the transformation of primary care from relatively isolated, independent practices to networks of providers that implement best practice and exchange patient information to improve health outcomes at the community level. 31 , 32 As the pressure increases to change the way primary care is delivered, practices struggle to understand how they must adapt to the new world of internet technology, HIE, and reimbursement. 33
O’QUIN is fortunate to have a relatively long history as a network, with its origin anchored in quality improvement for CVD risk, which is important to practices and their patients. Our approach differed from others who used dissemination theory and practice to guide research‐based quality improvements on a variety of outcome indicators. 34 , 35 Our focus on hypertension created a natural alliance with ASH, which became a key partner in training and certifying hypertension specialists to become experts in their communities, rather than relying on academic‐based physicians. Research in the early years utilized the network database and did not impose additional burdens on practices. The O’QUIN staff was viewed as supportive of local practices in their efforts to deliver quality care, while adjusting to an increasingly complex health care environment. The audit and feedback report was designed by local physicians to meet their needs. This “bottom‐up” approach has paid off, as the network has grown and as clinics seek assistance in meeting meaningful use and quality indicator–reporting requirements. While funding is challenging, the network has grown with multiple sources of funding, developing multidisciplinary teams, and by progressive efficiency to lower cost. Strategic planning, such as conducting SWOT analyses with our team, has also guided us through uncharted areas where both opportunities and threats are apparent.
From 1995 to 2006, South Carolina improved its rank from 51st to 35th in CVD mortality. From 1996 to 2006, coronary heart disease deaths declined 43% and stroke deaths 42%, 36 with cardiovascular deaths declining more in South Carolina than any other “Stroke Belt” state. O’QUIN cannot take responsibility for this dramatic improvement, but we believe our role was constructive. Future progress may be facilitated through a better organized practice network with a refined strategic plan, which includes comparative effectiveness research and facilitates meaningful use of EHRSs and pay‐for‐performance incentives.
Acknowledgments and disclosures: This work was supported in part by grants from the US Army (W81XWH‐10‐2‐0057), the State of South Carolina, the American Society of Hypertension, the National Institutes of Health ([NIH] NS058728, DK067615, HL091841), and the NIH National Center for Research Resources (Clinical Translational Science Award UL1 RR029882). During the past 12 months, Dr Egan has received research support from Daiichi‐Sankyo, Novartis, and Takeda pharmaceutical companies. None of the other authors have any financial disclosures to report related to this report.
References
- 1. Nembhard I, Alexander J, Hoff T, Ramanujam R. Why does the quality of health care continue to lag? Insights from management research. Acad Manage J. 2009;23:24–42. [Google Scholar]
- 2. Green L, Hickner J. A short history of primary care practice‐based research networks: from concept to essential research laboratories. J Am Board Fam Med. 2006;19:1–10. [DOI] [PubMed] [Google Scholar]
- 3. Fagnan L, Morris C, Shipman S, et al. Characterizing a practice‐based research network: Oregon rural practice‐based research network (ORPRN) survey tools. J Am Board Fam Med. 2007;20:204–219. [DOI] [PubMed] [Google Scholar]
- 4. Solberg LI. Recruiting medical groups for research: relationships, reputation, requirements, rewards, reciprocity, resolution, and respect. Implement Sci. 2006;1:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fagnan L, Davis M, Deyo R, et al. Linking practice‐based research networks and translational science awards: new opportunities for community engagement by academic health centers. Acad Med. 2010;85:476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Egan BM, Lackland DT, Igho‐Pemu P, et al. Cardiovascular risk factor control in communities – Update from the ASH Carolinas‐Georgia Chapter, the hypertension initiative, and the Community Physicians’ Network. J Clin Hypertens. 2006;12:879–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Egan BM, Lackland DT, Basile JN. American Society of Hypertension regional chapters: leveraging the impact of the clinical hypertension specialist in the local community. Am J Hypertens. 2002;15:372–379. [DOI] [PubMed] [Google Scholar]
- 8. Giese M, Lackland D, Basile J, Egan B. 2003 Update on the hypertension initiative of South Carolina. J S C Med Assoc. 2003;99:157–161. [PubMed] [Google Scholar]
- 9. Hendrix K, Lackland DT, Egan BM. Cardiovascular risk factor control and treatment patterns in primary care. Manag Care Interface. 2003;16:21–26. [PubMed] [Google Scholar]
- 10. Basile JN, Lackland DT, Basile JM, et al. A statewide primary care approach to cardiovascular risk factor control in high‐risk diabetic and non‐diabetic patients with hypertension. J Clin Hypertens. 2004;1:18–25. [DOI] [PubMed] [Google Scholar]
- 11. Bestermann WH, Lackland DT, Riehle JE, Egan BM. A systematic approach to managing hypertension and the metabolic syndrome in primary care. South Med J. 2004;97:932–938. [DOI] [PubMed] [Google Scholar]
- 12. Lackland DT, Lin Y, Tilley BC, Egan BM. Assessment of racial differences in clinical practices for hypertension at primary care sites for medically underserved patients. J Clin Hypertens. 2004;6:26–33. [DOI] [PubMed] [Google Scholar]
- 13. Sheats N, Lin Y, Zhao W, et al. Prevalence, treatment, and control of hypertension among African Americans and Caucasians at primary care sites for medically underserved patients. Ethn Dis. 2005;15:25–32. [PubMed] [Google Scholar]
- 14. Hendrix KH, Riehle JE, Egan BM. Ethnic, gender, and age‐related differences in treatment and control of dyslipidemia in hypertensive patients. Ethnic Dis. 2005;15:11–16. [PubMed] [Google Scholar]
- 15. Rehman SU, Hutchison FN, Hendrix K, et al. Comparison of ethnic differences in blood pressure control at VA and non‐VA sites. Arch Intern Med. 2005;165:1041–1047. [DOI] [PubMed] [Google Scholar]
- 16. Hendrix KH, Mayhan S, Egan BM. Gender‐ and age‐related differences in treatment and control of cardiovascular risk factors among high‐risk patients with angina. J Clin Hypertens. 2005;7:386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Riehle JE, Lackland DT, Okonofua EC, et al. Ethnic differences in treatment and control of hypertension in patients with diabetes. J Clin Hypertens. 2005;7:445–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hendrix KH, Mayhan S, Lackland DT, Egan BM. Demographic differences in the prevalence and treatment of chest pain syndromes and in the control of cardiovascular risk factors: a comparison of hypertensive patients with and without chest pain. Am J Hypertens. 2005;18:1026–1032. [DOI] [PubMed] [Google Scholar]
- 19. Okonofua EC, Simpson K, Jesri A, et al. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:1–7. [DOI] [PubMed] [Google Scholar]
- 20. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 21. Bakken S, Lanigua R, Busacca L, Bigger J. Barriers, enablers and incentives for research participation: a report from the Ambulatory Care Research Network (ACRN). J Am Board Fam Med. 2009;22:43–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Centers for Disease Control; National Center for Health Statistics . Cardiovascular mortality. 1995.
- 23. Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern United States. Hypertension. 1998;6:1206–1215. [DOI] [PubMed] [Google Scholar]
- 24. Egan BM, Lackland DT. Strategies of prevention and the importance of public health and community programs. Ethnic Dis. 1998;8:143–154. [PubMed] [Google Scholar]
- 25. Gaede P, Lund‐Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–591. [DOI] [PubMed] [Google Scholar]
- 26. Walsh JME, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. [DOI] [PubMed] [Google Scholar]
- 27. Townsend RR, Shulkin DJ, Bernard D. Improved outpatient hypertension control with disease management guidelines. Am J Hypertens. 1999;12(Pt 4):88A. [Google Scholar]
- 28. Jamtvedt G, Young JM, Kristoffersen DT, et al. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2003;3:CD000259. [DOI] [PubMed] [Google Scholar]
- 29. Fontaine P, Zink T, Boyle R, Kralewski J. Health information exchange: participation by Minnesota primary care practices. Arch Intern Med. 2010;170:622–639. [DOI] [PubMed] [Google Scholar]
- 30. Gibson K, Szilagyi P, Swanger C, et al. Physician perspectives on incentives to participate in practice‐based research: a greater Rochester practice‐based research network (GR‐PBRN) study. J Am Board Fam Med. 2010;23:452–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rosenthal MB, Dudley RA. Pay‐for‐performance. Will the latest payment trend improve care? JAMA. 2007;297:740–744. [DOI] [PubMed] [Google Scholar]
- 32. EHR incentive program. Overview. Commission on Medicare and Medicaid Services. https://www.cms.gov/EHRIncentivePrograms/. Accessed December 14, 2010.
- 33. Meyers D, Clancy C. Primary care: too important to fail. Ann Intern Med. 2009;150:272–273. [DOI] [PubMed] [Google Scholar]
- 34. Feifer C, Ornstein S, Jenkins R, et al. The logic behind a multimethod intervention to improve adherence to clinical practice guidelines in a nationwide network of primary care practices. Eval Health Prof. 2006;29:65–88. [DOI] [PubMed] [Google Scholar]
- 35. Ornstein S, Nietert P, Jenkins R, et al. Improving the translation of research into primary care practice: results of a national quality improvement demonstration project. Jt Comm J Qual Patient Saf. 2008;34:379–390. [DOI] [PubMed] [Google Scholar]
- 36. Heart Disease and Stroke Statistics: 2010 update at‐a‐glance. American Heart Association. http://www.americanheart.org/downloadable/heart/1265665152970DS‐3241%20HeartStrokeUpdate_2010.pdf. Accessed December 14, 2010.


