Abstract
Background
Dyspnea is a prominent symptom in asthma. The Dyspnea-12 (D-12), an instrument that quantifies breathlessness using 12 descriptors that tap the physical and affective aspects, has shown promise for the measurement of dyspnea in cardiorespiratory disease.
Objective
We report the results of a study designed to test the validity and reliability of the D-12 in a population of patients with asthma.
Methods
This cross-sectional study included 102 patients with asthma. Subjects completed the D-12, Hospital Anxiety and Depression Scale (HAD), St George’s Respiratory Questionnaire (SGRQ), MRC scale. Confirmatory factor analysis confirmed the two-component structure of the D-12 (i.e. 7 items that tap the Physical aspects of breathlessness and 5 items that tap the Affective aspects).
Results
The D-12 subscales had excellent internal reliability (Cronbach’s alpha for the ‘Physical’ score was 0.94 and the Affective score was 0.95). The D-12 Physical component was more strongly correlated with SGRQ Symptoms (r = 0.648), SGRQ Activities (r = 0.635) and MRC grade (r = 0.636), while the Affective component was more strongly correlated with SGRQ Impacts (r = 0.765) and HAD scores (anxiety r = 0.641 and depression r = 0.602).
Conclusion
This study supports validity of the D-12 for use in the assessment of dyspnea of patients with asthma. It assesses one of the most pertinent symptoms of asthma from two viewpoints -physical and affective.
Keywords: asthma, dyspnea, symptoms, patient reported outcome measures, quality of life, adults
INTRODUCTION
Asthma, an inflammatory airways disease affecting 4-7% of the adult population in the United States and Europe,1,2 is a complex condition in which environmental, allergic and psychological elements all play a role.3,4 Dyspnea, a subjective experience of difficult or uncomfortable breathing originating from an intricate interaction between physiological and psychological factors,5 is a cardinal symptom of asthma. The measurement of dyspnea in asthma is important for several reasons: first, as one of the hallmark features of asthma, dyspnea is often the primary reason patients seek medical help; second, as a subjective symptom it represents an alarm signal to the patient, making it a vital component of self-monitoring; and finally, it is an important outcome variable in clinical care and interventional studies for which a primary goal is effective symptom management.
The qualitative experience of dyspnea involves a variety of uncomfortable physical sensations which are common across respiratory conditions.6-9 With the exception of ‘chest tightness’ and ‘wheezy’, which tend to be mostly linked to asthma, patients with respiratory disease use a range of descriptors that are common to different disease groups. Examples include ‘work’/‘effort’, ‘uncomfortable breathing’, and ‘not enough air’, and are noted to depict the physical aspects of dyspnea6-12 Thus, the Dyspnea-12 (D-12),13 an instrument designed to quantify dyspnea using descriptors that are known to be associated with different cardiopulmonary diseases, is likely to be appropriate for use in patients with asthma.
Because psychological and emotional factors influence the perception of dyspnea during bronchoconstriction, 4 the assessment of dyspnea in asthma should take account of both physical and psychological elements. It has been well established that asthma patients characterised by significant negative affectivity report more respiratory symptoms regardless of their physiological and overall clinical status.14,15,16 These symptom misperceptions are thought to be the result of blunting mechanisms highly related to a person’s psychological state. 17 Measurement of the affective component of dyspnea with an instrument validated in asthma may provide valuable insight into these mechanisms.
The D-12, an instrument that quantifies breathlessness using 12 descriptors that tap the physical and affective aspects of dyspnea, was developed in a cohort of patients with chronic obstructive pulmonary disease (COPD), interstitial lung disease (ILD), and chronic heart failure (CHF). 13 It has subsequently been shown to possess validity and reliability for the measurement of dyspnea in COPD13 and ILD. 18,19 The primary objectives of this current study were: i) to assess whether the D-12 could measure breathlessness reliably (including internal consistency and stability over time) in asthma; ii) to evaluate the validity of the D-12 in terms of its ability to demonstrate correlations with other pertinent measures of asthma activity; iii) to test its ability to distinguish between different levels of disease severity in patients with asthma; and iv) to determine whether the previously confirmed two-factor structure of the D-12 (i.e. grouping of 7 items into a ‘physical’ subscale and 5 items into an ‘affective’ subscale),18 holds in an asthma population.
METHODS
Study Population
All patients diagnosed with asthma according to British Thoracic Society (BTS); Scottish Intercollegiate Guidelines Network guidelines20 and attending specialists out-patient asthma clinics in the North West of England between April 2008 and October 2009 were invited to participate. One-hundred and thirty-two eligible patients were identified, and 102 participated after providing signed written consent. The study was approved by the Salford and Trafford Local Ethics Committee (07/H1004/168).
Study Protocol
We conducted a cross-sectional study with repeated measures two weeks apart. At study entry, each participant completed the D-12, which yields a Total score (range 0-36, with higher scores corresponding to greater dyspnea) and two component scores: Physical (includes items 1 – 7, and scores range from 0-21; e.g., ‘My breathing requires more work’ and ‘I have difficulty catching my breath’) and Affective (includes items 8 – 12, and scores range from 0-15; e.g., ‘My breathing makes me feel depressed’ and ‘My breathing is distressing’). A number of other health related measures were completed: the Medical Research Council (MRC) Dyspnea scale,21 used to classify participants according to the magnitude of task that stimulates dyspnea (range 1 – 5, with higher scores corresponding to worse status); the St George’s Respiratory Questionnaire (SGRQ),22 a standardized questionnaire for the assessment of health related quality of life in obstructive lung disease (higher scores connote greater impairment); and the Hospital Anxiety and Depression scale (HAD) a widely used tool for assessing psychological distress (7 items tap anxiety with a score range of 0-21, and 7 items tap depression with a score range of 0 -21; higher scores indicate greater emotional distress).23
Pulmonary function tests and the six-minute walk distance test (6MWD) were conducted at study entry according to American Thoracic Society (ATS) guidelines,24 and values for forced expired volume in one second (FEV1) and forced vital capacity (FVC) were expressed as a percentage of age, gender, and height predicted normal (i.e., FEV1% and FVC%, respectively). Values for the distance walked during the 6MWD are reported in meters. Participants were allocated to BTS stepwise management for adults with asthma according to prescribed medications (i.e., Step 1: Mild intermittent asthma – inhaled short-acting ß2 agonist as required; Step 2: Regular preventer therapy – inhaled steroid 200-800mg; Step 3: initial add-on therapy – inhaled long-acting ß2 agonist; Step 4: persistent poor control – increased inhaled steroid, addition of fourth drug e.g. leukotrine receptor antagonist; Step 5: continuous or frequent use of oral steroids).20
For test-retest, participants completed the D-12 again at home two weeks later. This time period was considered to be long enough for participants not to recall (and simply reiterate) their baseline responses whilst their clinical condition remained constant. A global health transition item was also completed - participants were asked if, compared to when they completed questionnaires at baseline, their general health was: ‘much better’, ‘somewhat better’, ‘about the same’, ‘somewhat worse’, or ‘much worse’. The transition item was used to determine whether or not perceived general health condition had changed between the two time points and to provide an anchor against which change scores from the dyspnea instruments could be compared.
Statistical Analysis
The psychometric properties of the D-12, including floor and ceiling effects, internal consistency, test-retest reliability and construct validity, were examined in this study. Parametric and distribution-independent tests were performed throughout the analyses. No major discrepancies between these two approaches were found, so results are reported from the parametric tests to allow easier interpretation. Except for the confirmatory factor analysis, statistical tests were run using SPSS software (Version 16.0). Statistical significance was accepted at p ≤ 0.05 and summary results are presented as mean ± SD.
Reliability of the D-12
The internal consistency of the D-12 and its two components were tested using Cronbach’s alpha coefficient, for which values from 0.7-0.9 indicate acceptable internal consistency for a multidimensional instrument.25 To investigate the stability of the D-12, we measured the test-retest intraclass correlation coefficient (ICC) in participants who recorded a global health transition of ‘about the same’. Values greater than 0.7 indicate good reliability.
Validity of the D-12
To assess the two-factor structure of the D-12 (i.e. construct validity) we used SAS PROC CALIS (SAS Institute, Cary, NC) to run confirmatory factor analysis (CFA). Five tests were applied to assess acceptable fit: 1) chi-square, 2) root mean square error of approximation (RMSEA), 3) Bentler’s Comparative Fit Index (CFI), 4) Bentler and Bonnett’s Non-normed Index (NNI), and 5) Bentler and Bonnett’s Normed Fit Index (NFI). Fit is indicated by a chi-square p ≥ 0.05, RMSEA < 0.06, CFI ≥ 0.9, NNI ≥ 0.9, or NFI ≥ 0.9.26 See online material for details regarding CFA.
To examine convergent validity of the D-12 in this cohort, Pearson’s coefficient was used to test correlations between D-12 scores and other patient reported outcomes, including SGRQ, HAD, and MRC scores. We also tested for correlations with FEV1%, FVC%, and 6MWD. Student’s unpaired t-test and one-way analysis of variance (ANOVA) were used to compare D-12 scores between sub-groups stratified on 6MWD greater or less than 350 metres)27 or asthma severity (according to the five steps in the BTS guidelines).20
RESULTS
Patient Details
102 patients completed the questionnaires at entry and 87 at follow-up. The mean ± SD and range of the physiological and patient reported outcomes for the study population are summarised in Table 1. According to the BTS guidelines20 17% of participants were currently on asthma management Step 1; 14% on Step 2; 41% on Step 3, 14% on Step 4, and 16% on Step 5. There was no difference in D-12 Total and component scores between genders (all t values < 0.2, p values > 0.05), and there was no association between D-12 scores and age (all Pearson r values < 0.11, p values > 0.05).
Table 1.
Baseline characteristics
| All patients (N = 102) (mean ± SD) |
|
|---|---|
| Age, year | 50 ± 14 |
| Sex ratio, Female:Male (%) | 53:49 |
| Race (%) | |
| White | 90 |
| Asian | 6 |
| Black African | 2 |
| FVC% predicted | 91 ± 21.5 |
| FEV1% predicted | 84 ± 24.1 |
| 6MWD (m) | 434.8 ± 163 |
| D-12 Total | 16.8 ± 10.8 |
| Physical | 10.5 ± 6.1 |
| Affective | 6.3 ± 5.1 |
| MRC dyspnea grade | 2.6 ± 1.4 |
| SGRQ | |
| Symptoms | 67. 9 ±19.5 |
| Activity | 53.5 ±29.1 |
| Impacts | 43.8 ± 26.1 |
| Total | 51.1 ±23.4 |
| HADS | |
| Anxiety | 8.1 ± 5.1 |
| Depression | 6.2 ± 4.4 |
Definition of abbreviations: D-12 = Dyspnea-12; FEV1 = forced expired volume in one minute; FVC = forced vital capacity; 6MWD = six-minute walk distance; MRC = Medical Research Council; SGRQ = St George’s Respiratory Questionnaire; HAD = .Hospital anxiety and depression scale.
FEV1 and FVC expressed as percentage of predicted value
There were no missing data for either the D-12 at study entry or follow-up. The mean D-12 scores at entry were as follows: Total score, 19.9 (SD = 12); Physical score, 10.5 (SD = 6.1); Affective score, 6.5 (SD = 5.1). The percentage of subjects with the lowest D-12 Total score of zero (floor effect) was 2.3%, and the percentage of subjects with the highest possible score (ceiling effect) was 5.9%.
Internal Consistency and Repeatability of the D-12
Cronbach’s alpha coefficients for the D-12 components scales were 0.94 for the Physical component, 0.95 for the Affective component, and 0.96 for the Total score. The ICC for the repeatability of the D-12 component and Total scores measured in the group of patients who reported a health transition score of ‘about the same’ (n = 48) were between 0.93 – 0.96 (p < 0.001).
D-12 Construct Validity
Three CFA fit statistics; the CFI, NNI, and NFI were all > 0.9, indicating acceptable fit and thus confirming the D-12 underlying structure of Physical and Affective components in this patient group. See online material for details regarding CFA results.
Relationship between D-12 scores and other Measures of Health Status
The D-12 Physical and Affective components were most strongly correlated with the SGRQ Impacts component (r = 0.758 and r = 0.765, respectively) (Table 2). Compared to the D-12 Affective component, the Physical component was more strongly correlated with SGRQ Symptoms, SGRQ Activities and MRC grade, while the Affective component was more strongly correlated with HAD scores (Table 2).
Table 2.
Dyspnea-12 correlations with clinical variables and other patient reported measures
| D-12 Total | D-12 Physical | D-12 Affective | |
|---|---|---|---|
| FEV1 | −0.212* | −0.255* | −0.139 |
| FVC | −0.349** | −0.406** | −0.247* |
| 6MWD (metres) | −0.530** | −0.515** | −0.491** |
| MRC dyspnea | 0.597** | 0.636** | 0.493** |
| SGRQ | |||
| Symptoms | 0.647** | 0.648** | 0.591** |
| Activities | 0.601** | 0.635** | 0.571** |
| Impacts | 0.792** | 0.758** | 0.765** |
| Total | 0.781** | 0.773** | 0.721** |
| HAD - Anxiety | 0.574** | 0.493** | 0.641** |
| HAD - Depression | 0.594** | 0.540** | 0.602** |
Definition of abbreviations: D-12 = Dyspnea-12; FEV1 = forced expired volume in one minute; FVC = forced vital capacity; 6MWD = six-minute walk distance; MRC = Medical Research Council; SGRQ = St George’s Respiratory Questionnaire; HAD = Hospital anxiety and depression scale.
Correlations are expressed as Pearson’s r coefficient.
p < 0.01
p < 0.001
Relationship between D-12 scores Physiological Measures
Physiological measures of asthma severity were more strongly correlated with the Physical component of the D-12 than the Affective component (Table 2). Exercise performance measured by the 6MWD was the strongest physiological correlate of the D-12 (Table 2).
Discriminant Validity and Responsiveness of the D-12
There was a significant interaction between groups defined by BTS management step and D-12 Total score (F= 5.8, p = 0.001). There were no statistically significant differences between adjacent groups (Table 2 and Figure 1), but there was a significant difference between subgroups at the extremes (e.g., Step 1 versus Step 4 mean difference = 13.87, p = 0.003; and Step 1 versus Step 5 mean difference = 11.06, p = 0.009) (Table 3). We found that 20% of our patients had limited exercise capacity defined by a 6MWD less than350 metres; these patients had significantly higher D-12 Total score than patients whose 6MWD was equal to or greater than >350 metres (mean difference = 10.1, t = 3.6, p = 0.001).
Figure 1.
Dyspnea-12 scores (D-12) for each BTS Management Step in 102 patients with asthma at study entry. The error bars represent 95% confidence intervals for D-12 scores.
Table 3.
Mean difference in Dyspnea-12 Total scores between each BTS Management Step
| BTS Management Step |
Mean Difference in D-12 scores between each Step |
Standard Error | |
|---|---|---|---|
| Step 1: | |||
| Step 2 | 0.85 | 3.443 | |
| Step 3 | 6.22 | 2.851 | |
| Step 4 | 13.87** | 3.727 | |
| Step 5 | 11.60** | 3.443 | |
| Step 2: | |||
| Step 1 | 0.85 | 3.443 | |
| Step 3 | 5.36 | 2.914 | |
| Step 4 | 13.02** | 3.775 | |
| Step 5 | 10.75* | 3.495 | |
| Step 3: | |||
| Step 1 | 6.22 | 2.851 | |
| Step 2 | 5.36 | 2.914 | |
| Step 4 | 7.65 | 3.244 | |
| Step 5 | 5.38 | 2.914 | |
| Step 4: | |||
| Step 1 | 13.87** | 3.727 | |
| Step 2 | 13.02** | 3.775 | |
| Step 3 | 7.65 | 3.244 | |
| Step 5 | 2.27 | 3.775 | |
| Step 5: | |||
| Step 1 | 11.60** | 3.443 | |
| Step 2 | 10.75* | 3.495 | |
| Step 3 | 5.38 | 2.914 | |
| Step 4 | 2.27 | 3.775 |
p < 0.05
p < 0.01
Table 3 shows the mean difference in D-12 Total scores between each step of the BTS Management Step guidelines (BTS, 2009). The mean difference in D-12 Total score between each BTS Management Step was calculated separately.
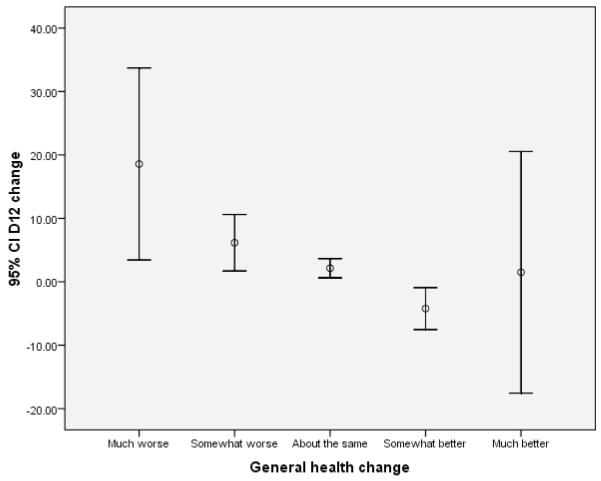
To assess sensitivity to change, changes in the patients’ scores over the 2-week period between entry and follow-up were calculated and compared with their general health transition score. Taking the population as a whole, changes over this time were small: ‘much better’ n = 7, ‘somewhat better’ n = 19, ‘about the same’ n = 48, ‘somewhat worse’ n = 9, ‘much worse’ n = 2. There was a significant association between transition scores and change in D-12 Total score between the two time points (F = 10.3, p = 0.001); the largest difference was found between the ‘much better’ and ‘somewhat better’ groups (mean difference = 12.4 SD = 3.3, p = 0.003) (Figure 2).
Figure 2.
Dyspnea-12 Total change score and change in global health reported with the transition item at follow-up. The error bars indicate 95% confidence intervals.
DISCUSSION
In this study, we observed that the D-12, a dyspnea questionnaire that taps both physical and affective perceptions, has acceptable validity and reliability for use in patients with asthma. The D-12 demonstrated excellent internal reliability. In addition, scores were correlated (in the expected direction) with physiological measures - as well as with patient reported outcomes including HRQL, activity limitation and psychological distress - known to be important in the assessment of asthma patients.
The D-12 was developed using Rasch analysis 28 – items were included in the 12-item list if they conformed to the unidimensional Rasch model. In other words, even though seven of the D-12’s items reflect physical aspects and five reflect affective aspects, all 12 items relate to the principal construct of breathlessness severity. The results of the CFA in the current study confirm this two-factor structure holds for the D-12 (‘Physical’ and ‘Affective’ components) in an asthma population.
The Affective component in particular provides a novel approach for the measurement of dyspnea in patients with asthma. In humans, the affective dimension evokes distress and may motivate behaviour. Although intricately linked, there is evidence that the affective and physical dimensions of asthma may be separately manipulated. Distraction has been shown to blunt the affective intensity of asthma, and negative emotions enhanced it.29,30 In contrast, sensory intensity was unaffected by these interventions. With its two components, the D-12 may be a useful tool for measuring the impact of these two aspects of asthma and may guide therapy. Thus, we anticipate the D-12 will be useful in clinical practice and in research, where it will have utility for assessing the effectiveness of medicinal as well as psychologically-targeted therapies.
Among its two components, the D-12 Affective component had the strongest association with disease specific distress assessed with the SGRQ Impacts component, and global psychological distress assessed with the HAD. As expected, we observed significant but weak correlations between dyspnea scores and physiological outcomes. D-12 scores correlated strongly with 6MWD, suggesting that functional capacity contributes more to patients’ perceptions of dyspnea than FEV1 and FVC. This highlights the importance of assessing patient reported outcomes in general and symptom perception in particular; these outcomes capture important information missed by physiologic measures. Although there was a progressive increase in D-12 scores from Steps 1 to 4, there was no significant difference in scores between adjacent categories. In fact, patients on Step 5 reported less dypsnea severity than those on Step 4. We found a similar pattern following post hoc analysis with the SGRQ components (results not reported). These results underscore symptom variability in the severe asthma population.
Our study has limitations. We did not capture data relating to recent asthma exacerbation or a measure of asthma control, which may have influenced patients’ responses to questionnaire items. It is likely also that there was a recruitment bias, since these were patients studied in secondary clinics. Such patients get referred because they have persistent troublesome symptoms or frequent exacerbations. The baseline data suggest that these were highly symptomatic patients, since they had only mild airflow limitation (FEV1 84% predicted), but high SGRQ scores and indicated quite significant respiratory-induced disability with a mean MRC score of 2.6. Despite this high symptom burden, there were good correlations between D12 score and measures of clinical severity. It is likely that our observations can be generalised to other secondary care patient groups, but need to be confirmed in a primary care population. Future studies should focus on examining the potential relationship between reported asthma control and dyspnea perception – the affective component in particular. The small number of patients that reported a global health change at follow-up did not allow us to calculate the minimum clinically important difference for the D-12; we believe this should be a goal for a future longitudinal study.
CONCLUSION
This study supports validity of the D-12 for use in the assessment of dyspnea of patients with asthma. The instrument is easy to administer, takes minutes to complete, and is simple to score. It assesses one of the most pertinent symptoms of asthma from two viewpoints - physical and affective. It is likely to be of value to those who wish to learn more about the effects of asthma on dyspnea perception, to clinicians caring for asthma patients, and to investigators studying asthma therapies (medicinal or others).
Supplementary Material
Acknowledgements
The authors are grateful to all patients at Pennine Acute Trust who took time to take part in this study. We are grateful to Dr David Weir and Dr Jon Miles for assisting with patient recruitment and thoughtful discussions during the conduct of this study.
This study was funded by Action Medical Research UK (SP4244).
Dr. Swigris is supported in part by a Career Development Award from the NIH (K23 HL092227).
Footnotes
Declaration of Interest statement: None of the authors have any real or potential conflicts of interest in relation to this research to declare.
References
- 1.Pleis JR, Lucas JW, Ward BW. Summary health statistics for U.S. adults: National Health Interview Survey, 2008. National Center for Health Statistics. Vital Health Stat. 2009;10(242) [PubMed] [Google Scholar]
- 2.Toren K, Gislason T, Omenaas E, Jogi R, Forsberg B, Nystrim L, Olin AC, Svanes C, Janson C, on behalf of the RHINE study group A prospective study of asthma incidence and its predictors: the RHINE study. Eur Resp J. 2004;24:942–946. doi: 10.1183/09031936.04.00044804. [DOI] [PubMed] [Google Scholar]
- 3.Cooper CL, Parry GD, Saul C, Morice AH, Hutchford BJ, Moore J, Esmonde L. Anxiety and panic fear in adults with asthma: prevalence in primary care. BMC Family Practice. 2007;8:62. doi: 10.1186/1471-2296-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Lieshout RJ, MacQueen G. Psychological factors in asthma. Allergy, Asthma and Clinical Immunology. 2008;4:12–28. doi: 10.1186/1710-1492-4-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Thoracic Society Dyspnea: Mechanisms, assessment, and management: a consensus statement. Am J Resp Crit Care Med. 1999;159:321–340. doi: 10.1164/ajrccm.159.1.ats898. [DOI] [PubMed] [Google Scholar]
- 6.Simon PM, Schwartzstein RM, Woodrow J, Fencl V, Teghtsoonian M, Weinberger SE. Distinguishable sensations of breathlessness in patients with shortness of breath. Am J Resp Crit Care Med. 1990;142:1009–1014. doi: 10.1164/ajrccm/142.5.1009. [DOI] [PubMed] [Google Scholar]
- 7.Mahler DA, Harver A, Lentine T, Scott JA, Beck K, Schwartzstein RM. Descriptors of breathlessness in cardiorespiratory diseases. Am J Resp Crit Care Med. 1996;154:1357–63. doi: 10.1164/ajrccm.154.5.8912748. [DOI] [PubMed] [Google Scholar]
- 8.Wilcock A, Crosby V, Hughes A, Fielding K, Corcoran R, Tattersfield A. Descriptors of breathlessness in patients with cancer and other cardiorespiratory diseases. J Pain and Symptom Management. 2002;23:182–9. doi: 10.1016/s0885-3924(01)00417-1. [DOI] [PubMed] [Google Scholar]
- 9.Smith JA, Albert P, Bertella E, Lester J, Jack S, Calverley P. Qualitative aspects of breathlessness in health and disease. Thorax. 2009;64(8):713–718. doi: 10.1136/thx.2008.104869. [DOI] [PubMed] [Google Scholar]
- 10.Moy ML, Lantin ML, Harver A, Schwartzstein RM. Language of dyspnea in assessment of patients with acute asthma treated with nebulised albuterol. Am J Resp Crit Care Med. 1998;158:749–53. doi: 10.1164/ajrccm.158.3.9707088. [DOI] [PubMed] [Google Scholar]
- 11.Binks AP, Moosavi SH, Banzett RB, Schwartzstein RM. Tightness sensation of asthma does not arise from the work of breathing. Am J Resp Crit Care Med. 2002;165:78–82. doi: 10.1164/ajrccm.165.1.2105061. [DOI] [PubMed] [Google Scholar]
- 12.Coli C, Picariello M, Stendardi L, Grazzini M, Binazzi B, Duranti R, Scano G. Is there are link between qualitative descriptors and the quantitative perception of dyspnea in asthma? Chest. 2006;130:436–41. doi: 10.1378/chest.130.2.436. [DOI] [PubMed] [Google Scholar]
- 13.Yorke J, Moosavi SH, Shuldham C, Jones PW. Quantification of breathlessness using descriptors: development and initial testing of Dyspnoea-12. Thorax. 2010;65:21–26. doi: 10.1136/thx.2009.118521. (doi:10.1136/thx.2009.118521) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jansen C, Bjornsson E, Hetta J, Boman G. Anxiety and depression in relation to respiratory symptoms in asthma. Am J Resp Crit Care Med. 1994;149:930–34. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- 15.Put C, Demedts M, Van den Bergh O, Demyttenaere K, Verleden G. Asthma symptoms: influence of personality versus clinical status. Eur Resp J. 1999;13:751–56. doi: 10.1034/j.1399-3003.1999.13d09.x. [DOI] [PubMed] [Google Scholar]
- 16.Put C, Van den Bergh O, Van Ongeval E, De Peuter S, Demedts M, Verleden G. Negative affectivity and influence of suggestion on asthma symptoms. J Psychosomatic Research. 2004;57:249–55. doi: 10.1016/S0022-3999(03)00541-5. [DOI] [PubMed] [Google Scholar]
- 17.Barreiro E, Gea J, Sanjuas C, Broquetas J, Milic-Emili J. Dyspnea at rest and at the end of different exercises in patients with near-fatal asthma. Eur Resp J. 2004;24:219–25. doi: 10.1183/09031936.04.00074703. [DOI] [PubMed] [Google Scholar]
- 18.Yorke J, Swigirs J, Russell AM, Moosavi SH, Kwong G Ng Man, Longshaw M, Jones PW. Dyspnoea-12 is a valid and reliable measure of breathlessness in patients with ILD. Chest. 2011;139(1):159–64. doi: 10.1378/chest.10-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swigris J, Yorke J, Sprunger DB, Swearingen C, Pincus T, du Bois RM, Brown KK, Fischer A. Assessing dyspnea and its impact on patients with connective tissue disease-related interstitial lung disease. Resp Med. 2010;104:1350–55. doi: 10.1016/j.rmed.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.British Thoracic Society. Scottish Intercollegiate Guidelines Network British guideline on the management of asthma: a national clinical guideline. 2009.
- 21.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thora.x. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Resp Di.s. 1992;145(6):1321–7. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 24.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111e17. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 25.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 26.Suhr DD. Exploratory or confirmatory factor analysis?. Paper #200-31, 31st SAS users group international conference; San Francisco. 2006. [Google Scholar]
- 27.Cote CG, Casanova C, Marin JM, et al. Validation and comparison of reference equations for the 6-minute walk test. Eur Respir J. 2008;31:571–8. doi: 10.1183/09031936.00104507. [DOI] [PubMed] [Google Scholar]
- 28.Rasch G. Probabilistic models for some intelligence and attainment tests. Danish Institute for Educational Research; 1960. [Google Scholar]
- 29.von Leupoldt A, Ambruzsova R, Nordmeyer S, Jeske N, Dahme B. Sensory and affective aspects of dyspnoea contribute differentially to the Borg scale’s measurement of dyspnoea. Respiration. 2006;73(6):762–8. doi: 10.1159/000095910. [DOI] [PubMed] [Google Scholar]
- 30.von Leupoldt A, Mertz C, Kegat S, Burmester S, Dahme B. The impact of emotions on the sensory and affective dimension of perceived dyspnea. Psychophysiology. 2006;43:382–386. doi: 10.1111/j.1469-8986.2006.00415.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.