Abstract
Background
Moderate alcohol intake has been associated with better physical performance and reduced likelihood of functional limitations. Causal inference has been difficult as most studies are cross-sectional. Our study investigated the prospective relationship between alcohol consumption and the risk of incident mobility limitation.
Methods
The analysis included 3,061 participants in the Health ABC study, community-dwelling adults aged 70–79 without mobility disability at baseline. Study outcomes were the incidence of mobility limitation, defined as self-report at two consecutive semi-annual interviews of any difficulty either walking a quarter of a mile or climbing stairs, and the incidence of mobility disability, defined as severe difficulty or inability to perform these tasks at two consecutive reports. Weekly alcohol intake was assessed at baseline and categorized as follows: former, never or occasional (<1 drink/week), light (1 to 7 drinks per week for men; 1 to 3 drinks per week for women), moderate (8 to 14 drinks per week for men; 4 to 7 drinks per week for women), and heavy (> 14 drinks per week for men; > 7 drinks per week for women). Crude incidence rates were calculated per 100 person-years; Cox proportional-hazard regression analysis was used to estimate Hazard Ratios (HR) and 95% Confidence Interval (CI).
Results
During a follow-up time of 6.5 years, participants consuming moderate levels of alcohol had the lowest incidence of mobility limitation (6.4 per 100 person-years (P-Y); men: 6.4 per 100 P-Y; women 7.3 per 100 P-Y) and mobility disability (2.7 per 100 P-Y; men: 2.5 per 100 P-Y; women: 2.9 per 100 P-Y). Adjusting for demographic characteristics, moderate alcohol intake was associated with reduced risk of mobility limitation (HR:0.70;CI:0.55–0.89) and mobility disability (HR:0.66; CI:0.45–0.95), compared to never or occasional consumption. Additional adjustment for life-style related variables substantially reduced the strength of the association (HR:0.85;CI:0.66–1.08) and mobility disability (HR:0.81; CI:0.56–1.18). Conversely, adjustment for diseases and health status indicators did not importantly affect the strength of the associations, suggesting that life-style is most important in confounding the studied relationship.
Conclusions
Globally taken, these results suggest caution in attributing a direct benefit of moderate alcohol intake on functional ability.
INTRODUCTION
Increasing evidence shows that moderate alcohol consumption is associated with decreased risk of a number of adverse health events. A J or U-shaped relationship between alcohol consumption and all-cause mortality has been demonstrated, primarily owning to the reduced risk of cardiovascular events associated with moderate alcohol intake.1,2
In the last decade the relationship between alcohol intake and key geriatric outcomes, such as cognitive impairment, falls and functional decline has gained growing attention.3–7 In particular, a recent cross-sectional study4 shows that moderate alcohol intake is associated with better physical performance and reduced likelihood of functional limitations. However, because of the lack of experimental studies and important methodological weakness of the published studies, a causal relationship can not be established. Few studies investigated the relationship between alcohol and physical function with a prospective design and with an adequate follow-up time and rarely the effect of health-related factors associated with moderate alcohol intake has been closely investigated. Indeed, moderate drinkers might have many social and lifestyle characteristics that may account for the observed better physical performance. In addition, among older adults, the proportion of drinkers declines over time8 and level of alcohol intake is lower among those who had received recent medical care.9 For this reason it may be hypothesized that at least part of the reported protective effect of moderate alcohol intake may result from inclusion among non-drinkers of subjects who do not drink because of poor health status. On the other hand, the observed protective effect of moderate alcohol intake on physical function may also reflect the benefit of moderate intake on cardiovascular disease and inflammatory status,10 that in turn are well-established risk factors for functional decline and disability.
From this point of view, we hypothesized that the observed protective effect of moderate alcohol intake on physical function might be explained by three potential mechanisms: 1) the confounding effect of advantageous social and life-style factors associated with moderate drinking; 2) the better health status of moderate drinkers compared to former drinkers; 3) the beneficial effect of moderate alcohol intake on cardiovascular health and inflammatory status. The aim of the present study was, therefore, to investigate these hypotheses examining the prospective relationship between alcohol consumption and the risk of incident physical disability in a well-characterized sample of non disabled older people.
METHODS
Sample
The data were collected from 3,075 well-functioning white and black men and women, participating in the Health Aging and Body Composition (Health ABC) study, a prospective cohort study designed to investigate the impact of health conditions on age-related functional changes. Participants aged 70 to 79 years were recruited from a random sample of white Medicare beneficiaries, and all age-eligible black community residents in designated zip codes from the metropolitan areas surrounding the two field centres (Pittsburgh, PA, and Memphis, TN). Eligibility criteria included: (1) no difficulty walking 1/4 of a mile, climbing 10 steps, or performing basic activities of daily living; (2) no life-threatening illness; and (3) no plans to leave the area for three years. The present analyses are based on 3061 participants; 14 subjects were excluded because they had either no alcohol consumption data (n=12) or no follow-up information (n=2). All participants gave informed consent. The institutional review boards at each study site approved all protocols.
Measures
Alcohol Intake
Information on alcoholic beverage consumption was assessed by means of a standardized questionnaire administered at the baseline interview.10 The interviewer first explained to the participant that alcoholic beverages should include any kind of drink containing alcohol, including beer, wine, liquors, and cocktails or other mixed drinks. One drink was considered to be equal to 12 ounce of beer (one can), five ounce of wine (a full glass) or a drink containing a “shot”, a “jigger” or a “finger” of liquor (equivalent to about 1.5 ounces of liquor). After that, the participant was asked to report how many drinks he/she had in a typical week, over the past 12 months. Given the different drinking pattern of men and women, alcohol intake was categorized differently for men and women as follows: former, never or occasional (<1 drink/week), light (1 to 7 drinks per week for men; 1 to 3 drinks per week for women), moderate (8 to 14 drinks per week for men; 4 to 7 drinks per week for women), and heavy (> 14 drinks per week for men; > 7 drinks per week for women). For non drinkers the reason for not drinking was also collected, and the following primary reasons were considered: no need, dislike, medical reasons/health status, religious/moral, recovering alcoholic, family member alcoholic, cost, or other.
Outcomes
Participants were contacted by telephone every 6 months and visited a clinic every year during which health status was assessed and data about functional status were collected. The study outcome measure was the incidence of mobility limitation, defined as self-report at two consecutive semi-annual interviews of any difficulty either walking a quarter of a mile or climbing stairs without resting. In order to evaluate the incidence of more severe functional impairment (defined as mobility disability), a second study outcome that included only the incidence of severe difficulty or inability to perform these tasks at two consecutive reports, was also considered. Follow-up time was the time from the baseline visit until the date of the first of the two consecutive reports of the study endpoints. For those who did not experience any study outcomes, the follow-up time was censored at the end of follow-up, death or last contact date.
Covariates
The following demographic characteristics were considered as covariates: age, gender, race, study site, level of education, family income, and smoking habits. Baseline objective lower extremity performance was evaluated using 6-meters gait speed. Cognitive function was assessed using the Modified Mini-Mental State Exam (3MS),11 with cognitive impairment defined as a 3MS score <80.12 Depressed mood at baseline was evaluated by means of the standard Center for Epidemiologic Studies Depression Scale.13 Body Mass Index (BMI ) was computed as weight in kilograms divided by the square of height in meters. Physical activity performed during the last week was assessed. Time spent on climbing stairs, walking for exercise or other purposes, aerobics, weight or circuit training, high-intensity and moderate-intensity exercise activities was obtained as well as information on the intensity level. A metabolic equivalent value was assigned to each activity/intensity combination.14 The scores were summed across activities and multiplied by body weight to create an overall physical activity score in Kcal/week. Participants were categorized as physically inactive if they expended less than 200 Kcal/week.15
Health ABC includes two levels of information on health conditions at baseline. Prevalence of chronic conditions (cardiovascular disease [CVD-coronary heart disease, cerebrovascular disease, heart failure], hypertension, diabetes, knee osteoarthritis) was determined through disease algorithms using self-reported physician-diagnosed disease information, clinic data, and medication use mirroring adjudicated diagnoses in the Cardiovascular Health Study.16 In addition, the study included objective indicators of subclinical disease for many of the conditions. The ankle brachial index (ABI) was calculated as the systolic blood pressure (SBP) of the ankle divided by the SBP of the arm. ABI was used as an indicator of atherosclerosis severity.17 Renal function was assessed by means of creatinine clearance calculated according to the Cockcroft-Gault equation.18 Respiratory function was evaluated by means of the Tiffenau Index (ratio between forced expiratory volume in first second and forced vital capacity [FEV1/FVC]). Incident conditions were adjudicated at each clinical center according to algorithms established at the beginning of the study and requiring confirmatory data. Incident CVD was defined as any fatal event or overnight hospitalization in an acute care hospital for myocardial infarction, angina, heart failure, and stroke. Inflammatory status was assessed by Interleukin-6 (IL-6) levels, (ELISA kit from R&D Systems, Minneapolis, MN).
Statistical Analysis
Sample characteristics were compared across alcohol intake categories using the χ2-test for categorical variables and analysis of variance for continuous variables. Crude incidence rates were calculated per 100 person-years. A regression model including alcohol intake categories as linear and quadratic terms was used to test for non-linear trends; the likelihood ratio test was also used to compare the goodness of fit of the model including the linear and quadratic terms for alcohol intake categories with the model including the linear term only. Cox proportional-hazard regression analyses were performed to compute the Hazard Ratio (HR) for incident persistent mobility limitation and persistent mobility disability, according to baseline alcohol consumption. Hazard ratio was calculated relative to non drinkers and occasional drinkers (< 1 drink/week), as preliminary data analyses show no risk difference among these two groups. The assumption of proportionality, assessed through the analysis of Schoenfeld residuals,19 was conserved.
To address the study hypotheses, and in order to discriminate the effect between potential confounders and mediators, diverse analytic models were built. To the initial model adjusted for demographic variables (age, gender, race, study site; Model 1), we added the following variable groups: lifestyle related variables (education, income, smoking status, physical activity, BMI; Model 2); diseases and health status indicators that may act as confounders (knee osteoarthritis, FEV1/FVC, creatinine clearance, CESD score, 6-m walk time; Model 3), diseases and health status indicators that may act as mediators (hypertension, diabetes, prevalent CVD, ankle brachial index, cognitive impairment, IL-6 and finally incident CVD; Model 4). Finally a fully adjusted model was fitted (Model 5). To estimate to which extent lifestyle characteristics and health status contributed to the hypothesized protective effect of moderate alcohol intake on functional outcomes, we compared the HR for moderate alcohol intake estimated from model 1 (HR_basic), with HRs estimated from models including life-style related variables and health status indicators (HR_adjusted). The presence of a significant interaction between alcohol consumption, sex and race was tested by means of the likelihood ratio test. All analyses were performed using Stata 9.0 for Windows(Stata Corporation, College Station, TX).
RESULTS
The mean age of the study sample was 73.6 years, 51.7% were women, and 41.6% were black. Women were more likely to be never- or occasional drinkers (Table 1). Participants consuming moderate levels of alcohol were less likely to have low education level, poor income, obesity and physical inactivity. Moderate alcohol intake was associated with lower prevalence of cardiovascular risk factors and with lower prevalence and incidence of CVD. The best baseline lower extremity performance was observed among participants consuming moderate levels of alcohol.
Table 1.
Selected general characteristics of the study population according to alcohol intake (drinks/week)
| Never/<1 | Former | Light 1 to 7 in men 1 to 3 in women |
Moderate 8 to 18 in men 4 to 7 in women |
Heavy > 14 in men > 7 in women |
p value | |
|---|---|---|---|---|---|---|
|
Demographics and life-style related characteristics
| ||||||
| Age, years | 73.6±2.9 | 73.8±2.9 | 73.6±2.9 | 73.3±2.7 | 73.6±2.8 | 0.29 |
| Female % | 64.2 | 43.8 | 27.2 | 54.6 | 43.8 | <.001 |
| Black % | 45.4 | 55.9 | 25.2 | 17.2 | 31.3 | <.001 |
| Study site Memphis % | 45.2 | 50.0 | 57.3 | 55.1 | 62.5 | <.001 |
| Education %: | ||||||
| Less than high school | 26.1 | 37.1 | 15.5 | 7.8 | 19.5 | |
| High school | 36.3 | 33.1 | 25.9 | 24.8 | 26.6 | <.001 |
| Postsecondary | 37.3 | 29.3 | 58.4 | 67.4 | 53.9 | |
| Miss | 0.3 | 0.4 | 0.2 | 0.0 | 0.0 | |
| Family income %: | ||||||
| Less than 10K | 13.7 | 16.7 | 4.7 | 1.8 | 7.8 | |
| 10K to 25K | 36.7 | 38.3 | 25.9 | 23.4 | 35.9 | |
| >25K to 50K | 24.8 | 24.8 | 31.3 | 33.5 | 28.9 | <.001 |
| ≥50K | 9.7 | 9.7 | 26.9 | 29.4 | 13.3 | |
| Miss | 10.6 | 13.2 | 11.2 | 11.9 | 14.1 | |
| Current smoking % | 9.0 | 10.6 | 11.2 | 9.6 | 19.5 | <.001 |
| Physical activity %: | ||||||
| <200 Kcal/wk | 40.0 | 39.9 | 25.2 | 21.6 | 25.8 | |
| 200 to 1000 Kcal/wk | 33.3 | 30.3 | 34.3 | 39.9 | 44.5 | <.001 |
| ≥1000 Kcal/wk | 29.8 | 29.8 | 40.5 | 38.5 | 29.7 | |
| BMI %: | ||||||
| <20 Kg/m2 | 4.0 | 2.6 | 3.7 | 4.1 | 10.2 | |
| 20 to 25 Kg/m2 | 27.5 | 26.8 | 28.0 | 35.3 | 35.2 | |
| >25 to 29 Kg/m2 | 41.0 | 41.9 | 45.5 | 45.4 | 38.3 | <.001 |
| ≥30 Kg/m2 | 27.5 | 28.6 | 22.8 | 15.1 | 16.4 | |
|
| ||||||
|
Diseases and health status indicators
| ||||||
| Potential confounders | ||||||
| Knee OA % | 16.3 | 13.5 | 15.7 | 18.7 | 19.5 | 0.25 |
| FEV1/FVC | 76.1±8.5 | 74.4±9.1 | 74.3±9.2 | 73.6±8.5 | 74.2±9.3 | <.001 |
| Creatinine Clearance, ml/min | 63.1±17.6 | 64.4±18.2 | 66.6±16.9 | 64.8±17.0 | 65.0±16.3 | 0.002 |
| Six m walk, m/sec | 1.16±0.24 | 1.12±0.24 | 1.24±0.25 | 1.25±0.23 | 1.21±0.20 | <.001 |
| Baseline CESD score | 4.7±5.3 | 5.0±5.7 | 4.7±5.3 | 3.7±4.5 | 5.3±6.2 | 0.009* |
| Potential mediators | ||||||
| Hypertension % | 44.9 | 50.7 | 39.4 | 34.9 | 35.9 | <.001 |
| Prevalent cardiovascular disease % | 23.1 | 27.1 | 23.7 | 17.0 | 18.8 | 0.02 |
| Diabetes % | 15.0 | 25.2 | 9.9 | 6.9 | 2.3 | <.001 |
| Incident cardiovascular disease % | 23.9 | 28.7 | 22.8 | 19.3 | 31.3 | 0.007 |
| Ankle Brachial Index <0.9 % | 13.4 | 17.3 | 9.1 | 11.0 | 10.9 | <.001 |
| IL-6, pg/mL | 2.4±1.9 | 2.6±2.1 | 2.1±1.6 | 2.4±1.9 | 2.9±2.2 | <.001* |
| Cognitive impairment % | 10.6 | 13.8 | 7.1 | 1.8 | 8.6 | <.001 |
Continuous variables are reported as mean ± standard deviation
p values are from log-transformed data
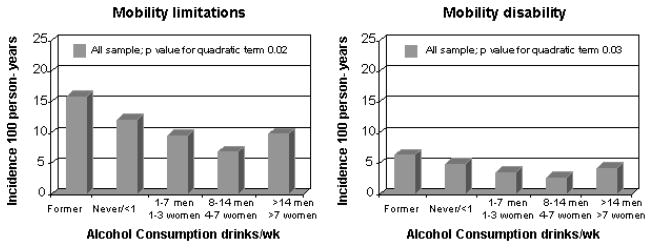
During a follow-up time of 6.5 years, persistent mobility limitation occurred in 1512 (49.4%) participants, and 720 (23.5%) participants experienced persistent mobility disability. Women compared to men had higher incidence of both mobility limitation (54.9% vs 43.5%, p <.001) and mobility disability (27.0% vs 19.8%, p <.001). Figure 1 shows incidence rates of mobility limitations and mobility disability according to alcohol consumption. Participants consuming moderate levels of alcohol had the lowest incidence of mobility limitations (6.4 per 100 person-years) and mobility disability (2.7 per 100 person-years).
Figure 1.
Incidence per 100 person-years of mobility limitations and mobility disability according to alcohol intake
Table 2 presents results from Cox regression analyses of the relationship between alcohol intake and the study outcomes. Adjusting for demographic characteristics, and compared to never/occasional consumption, moderate alcohol intake was associated with reduced risk of mobility limitation (Model 1; HR:0.70;95%Confidence Interval[CI]:0.55–0.89) and mobility disability (HR:0.66; CI:0.45–0.95). Inclusion of life-style related variables substantially reduced the strength of the association of moderate alcohol intake with mobility limitation (Model 2;HR:0.85; CI:0.66–1.08) and mobility disability (HR:0.81; CI:0.56–1.18), that became no longer statistically significant. Conversely, adjustment for diseases and health status indicators did not substantially alter the strength of the studied associations, and full adjustment determined an attenuation of the strength similar to that obtained in the life-style adjusted model. Also striking was the increased risk of mobility limitation associated with former drinking that was substantially reduced after multiple adjustment, but remained significant even in fully adjusted models.
Table 2.
Hazard Ratios (95% CI) of mobility limitations and mobility disability according to alcohol intake in all study sample (n=3061)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||
|---|---|---|---|---|---|---|
| Events/No | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR 95% CI | HR (95% CI) | |
| Mobility limitations | ||||||
|
| ||||||
| Never/< 1 dr/wk | 746/1497 | 1 | 1 | 1 | 1 | 1 |
| Former | 403/682 | 1.33 (1.17–1.50) | 1.30 (1.15–1.47) | 1.16 (1.03–1.32) | 1.23 (1.09–1.40) | 1.15 (1.01–1.30) |
| Light (1 to 7 men; 1 to 3 women) | 234/536 | 1.01 (0.86–1.18) | 1.07 (0.92–1.25) | 0.97 (0.84–1.14) | 1.10 (0.95–1.29) | 1.08 (0.93–1.27) |
| Moderate (8 to 14 men; 4 to 7 women) | 75/218 | 0.70 (0.55–0.89) | 0.85 (0.66–1.08) | 0.75 (0.59–0.95) | 0.71 (0.56–0.91) | 0.84 (0.66–1.07) |
| Heavy (> 14 men; > 7 women ) | 54/128 | 0.93 (0.70–1.22) | 0.97 (0.73–1.29) | 0.87 (0.66–1.15) | 0.93 (0.70–1.23) | 0.94 (0.70–1.24) |
|
| ||||||
| Mobility disability | ||||||
|
| ||||||
| Never/< 1 dr/wk | 362/1497 | 1 | 1 | 1 | 1 | 1 |
| Former | 204/682 | 1.34 (1.12–1.60) | 1.30 (1.09–1.54) | 1.18 (0.99–1.41) | 1.24 (1.04–1.48) | 1.18 (0.98–1.41) |
| Light (1 to 7 men; 1 to 3 women) | 97/536 | 0.90 (0.71–1.13) | 0.97 (0.76–1.22) | 0.84 (0.67–1.06) | 1.01 (0.80–1.28) | 0.99 (0.78–1.26) |
| Moderate (8 to 14 men; 4 to 7 women) | 31/218 | 0.66 (0.45–0.95) | 0.81 (0.56–1.18) | 0.69 (0.48–1.00) | 0.69 (0.48–1.00) | 0.82 (0.56–1.20) |
| Heavy (> 14 men; > 7 women ) | 26/128 | 1.00 (0.67–1.50) | 1.07 (0.71–1.60) | 0.98 (0.66–1.47) | 1.04 (0.70–1.56) | 1.10 (0.73–1.66) |
Model 1: adjusted for age, gender, race, site
Model 2: adjusted for age, gender, race, site, and life-style characteristics (education, family income, smoking status, physical activity, BMI)
Model 3: adjusted for age, gender, race, site, and health status-potential confounders (knee osteoarthritis, FEV1/FVC, creatinine clearance, CESD score, and 6-m walk speed)
Model 4: adjusted for age, gender, race, site, and health status-potential mediators (hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, cognitive impairment, IL-6, incident cardiovascular disease)
Model 5: adjusted for age, gender, race, site, education, family income, smoking status, physical activity, BMI, hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, knee osteoarthritis, FEV1/FVC, creatinine clearance, cognitive impairment, CESD score, IL-6, incident cardiovascular disease, and 6-m walk speed
We found a different relationship between alcohol intake and the study outcomes in men and women, and a potential interaction between alcohol intake and sex for both the study outcomes was found (p value for interaction =0.06 and 0.16 for mobility limitation and mobility disability, respectively). In men (Table 3) there was no association between moderate alcohol intake and the risk of mobility limitation (HR:0.94;CI:0.65–1.36) and mobility disability (HR:0.85;CI:0.47–1.53), whereas we observed an increased risk of mobility limitation among men consuming 1 to 7 drinks/wk, compared to never/occasional drinkers (HR:1.27;CI:1.03–1.56) that was attenuated after adjustment for diseases-potential confounders (Model 4, HR:1.16;CI:0.94–1.42), but persisted after full adjustment (Model 5, HR:1.30;CI:1.05–1.61). Male former drinkers also had an increased risk of persistent mobility limitation. In women (Table 4) we observed a significant association between moderate alcohol intake and reduced risk of mobility limitation (HR:0.60;CI:0.43–0.82), that was still attenuated after adjustment for life-style related characteristics (HR:0.75;CI:0.54–1.04). Among former drinkers, the risks associated with persistent mobility limitation were also attenuated in the adjusted models. With regard to mobility disability, both light alcohol intake and moderate alcohol intake were associated in women with a significant risk reduction. Even the strength of these associations were reduced after adjustment for lifestyle-related variables and health status characteristics. No significant interaction between alcohol intake and race was observed.
Table 3.
Hazard Ratios (95% CI) of mobility limitations and mobility disability according to alcohol intake in men (n=1480)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||
|---|---|---|---|---|---|---|
| Events/No | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR 95% CI | HR (95% CI) | |
| Mobility limitations | ||||||
|
| ||||||
| Never/< 1 dr/wk | 208/536 | 1 | 1 | 1 | 1 | 1 |
| Former | 206/383 | 1.54 (1.27–1.87) | 1.53 (1.26–1.86) | 1.29 (1.06–1.57) | 1.26 (1.03–1.54) | 1.25 (1.02–1.53) |
| Light (1 to 7 dr/wk) | 167/390 | 1.27 (1.03–1.56) | 1.33 (1.08–1.64) | 1.16 (0.94–1.42) | 1.37 (1.12–1.69) | 1.30 (1.05–1.61) |
| Moderate (8 to 14 dr/wk) | 33/99 | 0.94 (0.65–1.36) | 1.05 (0.72–1.53) | 0.94 (0.65–1.37) | 0.87 (0.60–1.27) | 0.94 (0.64–1.38) |
| Heavy (> 14 dr/wk) | 30/72 | 1.26 (0.86–1.85) | 1.27 (0.85–1.87) | 1.06 (0.72–1.57) | 1.27 (0.86–1.87) | 1.23 (0.83–1.83) |
|
| ||||||
| Mobility disability | ||||||
|
| ||||||
| Never/< 1 dr/wk | 93/536 | 1 | 1 | 1 | 1 | 1 |
| Former | 101/383 | 1.56 (1.18–2.07) | 1.52 (1.14–2.02) | 1.30 (0.98–1.74) | 1.40 (1.05–1.86) | 1.29 (0.96–1.73) |
| Light (1 to 7 dr/wk) | 74/390 | 1.24 (0.91–1.69) | 1.28 (0.94–1.76) | 1.05 (0.77–1.43) | 1.36 (0.99–1.85) | 1.23 (0.89–1.70) |
| Moderate (8 to 14 dr/wk) | 13/99 | 0.85 (0.47–1.53) | 0.99 (0.55–1.80) | 0.80 (0.45–1.45) | 0.84 (0.46–1.51) | 0.93 (0.51–1.69) |
| Heavy (> 14 dr/wk) | 12/72 | 1.13 (0.62–2.07) | 1.11 (0.60–2.06) | 0.93 (0.50–1.71) | 1.09 (0.59–2.00) | 1.01 (0.54–1.89) |
Model 1: adjusted for age, race, site
Model 2: adjusted for age, race, site, and life-style characteristics (education, family income, smoking status, physical activity, BMI)
Model 3: adjusted for age, race, site, and health status-potential confounders (knee osteoarthritis, FEV1/FVC, creatinine clearance, CESD score, and 6-m walk speed)
Model 4: adjusted for age, race, site, and health status-potential mediators (hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, cognitive impairment, IL-6, incident cardiovascular disease)
Model 5: adjusted for age, race, site, education, family income, smoking status, physical activity, BMI, hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, knee osteoarthritis, FEV1/FVC, creatinine clearance, cognitive impairment, CESD score, IL-6, incident cardiovascular disease, and 6-m walk speed
Table 4.
Hazard Ratios (95% CI) of mobility limitations and mobility disability according to alcohol intake in women (n=1581)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||
|---|---|---|---|---|---|---|
| Events/No | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR 95% CI | HR (95% CI) | |
| Mobility limitations | ||||||
|
| ||||||
| Never/< 1 dr/wk | 538/961 | 1 | 1 | 1 | 1 | 1 |
| Former | 197/299 | 1.22 (1.03–1.43) | 1.18 (0.99–1.39) | 1.15 (0.97–1.36) | 1.15 (0.97–1.36) | 1.10 (0.93–1.31) |
| Light (1 to 3 dr/wk) | 67/146 | 0.78 (0.60–1.00) | 0.84 (0.65–1.09) | 0.80 (0.62–1.04) | 0.86 (0.66–1.12) | 0.89 (0.68–1.15) |
| Moderate (4 to 7 dr/wk) | 42/119 | 0.60 (0.43–0.82) | 0.75 (0.54–1.04) | 0.68 (0.49–0.93) | 0.62 (0.45–0.85) | 0.78 (0.56–1.08) |
| Heavy (> 7 dr/wk) | 24/56 | 0.76 (0.50–1.14) | 0.80 (0.53–1.22) | 0.78 (0.51–1.17) | 0.78 (0.52–1.18) | 0.79 (0.52–1.21) |
|
| ||||||
| Mobility disability | ||||||
|
| ||||||
| Never/< 1 dr/wk | 269/961 | 1 | 1 | 1 | 1 | 1 |
| Former | 103/299 | 1.24 (0.99–1.56) | 1.20 (0.95–1.51 | 1.17 (0.93–1.48) | 1.18 (0.94–1.50) | 1.17 (0.93–1.48) |
| Light (1 to 3 dr/wk) | 23/146 | 0.56 (0.36–0.86) | 0.62 (0.40–0.95) | 0.58 (0.38–0.89) | 0.66 (0.43–1.02) | 0.70 (0.45–1.08) |
| Moderate ( 4 to 7 dr/wk) | 18/119 | 0.58 (0.36–0.93) | 0.73 (0.45–1.20) | 0.65 (0.40–1.05) | 0.61 (0.38–1.00) | 0.79 (0.48–1.29) |
| Heavy (> 7 dr/wk) | 14/56 | 1.01 (0.58–1.73) | 1.07 (0.62–1.85) | 1.10 (0.64–1.89) | 1.07 (0.62–1.86) | 1.15 (0.66–2.01) |
Model 1: adjusted for age, race, site
Model 2: adjusted for age, race, site, and life-style characteristics (education, family income, smoking status, physical activity, BMI)
Model 3: adjusted for age, race, site, and health status-potential confounders (knee osteoarthritis, FEV1/FVC, creatinine clearance, CESD score, and 6-m walk speed)
Model 4: adjusted for age, race, site, and health status-potential mediators (hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, cognitive impairment, IL-6, incident cardiovascular disease)
Model 5: adjusted for age, race, site, education, family income, smoking status, physical activity, BMI, hypertension, prevalent cardiovascular disease, diabetes, ankle brachial index, knee osteoarthritis, FEV1/FVC, creatinine clearance, cognitive impairment, CESD score, IL-6, incident cardiovascular disease, and 6-m walk speed
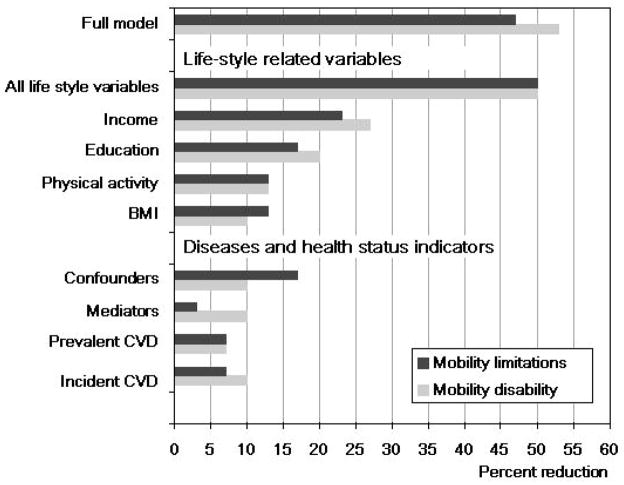
Finally, we estimated to which extent lifestyle related characteristics and health status accounted for the protective effect of moderate alcohol intake on the risk of mobility limitation and mobility disability. Figure 2 shows the percent reduction of the strength of the association between moderate alcohol consumption and the study outcomes. Life-style characteristics were the variables that mostly contributed in attenuating the protective effect of moderate alcohol intake. Adjusting for these characteristics all together determined a 50% reduction of the strength of the association between moderate alcohol intake with mobility limitation and mobility disability. Income, education, BMI and physical activity were the factors that had the greatest impact. Comorbidities and health status indicators had a smaller impact on the relationship between moderate alcohol intake and the study outcomes (Figure 2), and as expected, among the several diseases considered, cardiovascular disease, both prevalent and incident, was the condition that mostly attenuated the risk reduction associated with moderate alcohol intake. Simultaneous inclusion of all the covariates led to an about 50% attenuation of the strength of the studied associations. Analysis performed after exclusion of men yielded virtually identical results.
Figure 2.
Percent reduction of the protective effect of moderate alcohol intake (8–14 dr/wk in men; 4–7 dr/wk in women) on the risk of mobility limitations and mobility disability after adjustment of the basic model (age, gender, race, study site) for all potential confounders (full model), life-style related variables, diseases and health status indicators. Among these groups of variables, single variables with an effect greater than 5% were shown. Bars show the reduction in the protective effect of moderate alcohol intake obtained using the following formula: [(HR_basic − HR_adjusted)/HR_basic − 1] × 100
DISCUSSION
The results from this study show that among a large cohort of well-functioning older men and women, light-to-moderate alcohol consumption is associated with reduced risk of functional decline over a mean follow-up time of about 4 years. However, the protective effect of moderate alcohol intake was strongly attenuated after adjustment for life-style indicators, in particular the characteristics that mostly attenuated this protective effect were education, income, BMI and physical activity.
An association between light-to-moderate alcohol intake and physical function has been previously reported in literature. In particular, some studies suggest that moderate alcohol consumption is associated with lower ADL disability, lower rate of self-reported mobility limitation, and better objective physical performance.4,20–22 However, the causal direction and the underlying mechanisms of this association are not still understood. Most of the previous studies were cross-sectional and did not allow conclusions regarding cause-effect relationships. Furthermore, the reported associations were attenuated after adjustment, suggesting that the observed relationship may be not really a causal one, but might be partly due to confounding. In fact, it has been reported that light-to-moderate drinkers, compared to non-drinkers, have some lifestyle characteristics that may protect them from functional decline, including higher physical activity level, higher education level, and lower prevalence of obesity. 23 An other possible non-causal explanation for the observed inverse association between moderate alcohol intake and physical performance involves inclusion among non-drinkers of subjects who do not drink because of higher burden of disease (reverse causality).24 This issue may assume particular importance among older people since the proportion of individuals consuming alcohol decrease with age, a trend that has been related, at least in part, to worsening health over time.9,25 Light-to-moderate alcohol intake has also important health consequences that might however account for a direct protective effect. Previous studies demonstrated that light-to-moderate alcohol intake is associated with decreased risk of a number of adverse health events, such as coronary artery disease, heart failure and diabetes,1,2,26,27 that are important causes of physical disability in older people.28,29 Furthermore, there is strong evidence that increased levels of inflammatory markers are associated with poor physical performance and muscle strength, and are strong predictors of physical decline over time.30 Light-to-moderate alcohol consumption has been associated with lower levels of IL-6 and CRP,10 suggesting that also the alcohol anti-inflammatory effect might mediate the reported association between light-to-moderate alcohol consumption and better physical performance. Nevertheless, only a few studies have investigated the prospective relationship between alcohol intake and functional decline, and the lack of adjustment for potential confounders and mediators is a limitation of most of the previous studies.
To our knowledge, this is the first study that specifically investigated the prospective relationship between alcohol intake and risk of functional decline and assessed the role of potential confounding and mediating factors in explaining the observed relationship. In our study, relative to never/occasional drinking, light-to-moderate alcohol consumption was associated with a reduced risk of mobility limitation and mobility disability. However, controlling for lifestyle indicators, substantially weakened the association. In addition, after stratification for gender, the protective effect of moderate alcohol intake was observed only in women, and still attenuated after adjustment for life-style indicators. Globally taken, these results suggest that the reported protective effect of moderate alcohol intake on the likelihood of functional limitation mostly reflect the healthier lifestyle of subjects who consume alcohol at moderate levels.
Income, education, physical activity and BMI were the factors that mostly explained the association between moderate alcohol intake and reduced risk of functional decline, remaining also independent predictors of mobility disability. Income and education level are well-documented risk factor for disability.31 The relationship between BMI and physical activity with disability has been extensively investigated and consistent links between BMI, physical activity and functional decline have been established. Research across samples of older men and women indicates that high BMI is associated with greater functional limitations and higher rates of new disability.32,33 Several studies
demonstrated that regular physical activity may not only extend life expectancy, but also may reduce the risk of physical disability in late life.6,34–36 In our study, compared to never/occasional drinkers, subjects consuming moderate level of alcohol had lower BMI, the lowest prevalence of obesity, and the lowest prevalence of physical inactivity. From this point of view, these findings further support the hypothesis of a non-causal relationship between moderate alcohol intake and better physical performance, confirming moreover the pivotal role of BMI and physical activity in conditioning functional outcomes in older adults.
Some limitations of the present study should be considered. Alcohol intake was assessed by a standardized self-report questionnaire, which is prone to misreporting and misclassification. Moreover, our study is based on a single alcohol intake assessment at one point in time. However, among older people, drinking patterns tend to be stable over time37 and, given the relatively short follow-up period, it is unlikely that intake varied significantly. Finally, the narrow age-range of the study inclusion criteria, may limit the generalizability of the results.
In recent years, the relationship between alcohol intake and health outcomes has gained growing attention. While there is now considerable consensus that consuming alcohol at moderate level has a specific beneficial effect on the risk of cardiovascular disease, the benefit of alcohol intake on other health-related outcomes is less convincing. Globally taken, our results show that the reported protective effect of moderate alcohol intake on physical performance may be only apparent, because life-style related characteristics seem to be the real determinant of the reported association, suggesting caution in attributing a direct benefit of moderate alcohol intake on functional ability. This assume particular relevance given the risk of alcohol-dependence and the health hazards associated with excessive alcohol consumption. From this point of view, life-style recommendations for the prevention of functional decline should be based on interventions proven to be safe and effective, such as weight control and physical activity.36
Acknowledgments
This research was supported through the National Institute on Aging, contract numbers N01-AG-6-2106, N01-AG-6-2103, and N01-AG-6-2101. This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging, and by the grant R01 HL72972. Dr. Maraldi had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Hines LM, Rimm EB. Moderate alcohol consumption and coronary heart disease: a review. Postgrad Med J. 2001;77:747–752. doi: 10.1136/pmj.77.914.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maraldi C, Volpato S, Kritchevsky SB, et al. Impact of inflammation on the relationship among alcohol consumption, mortality, and cardiac events: the health, aging, and body composition study. Arch Intern Med. 2006;166:1490–1497. doi: 10.1001/archinte.166.14.1490. [DOI] [PubMed] [Google Scholar]
- 3.Cawthon PM, Harrison SL, Barrett-Connor E, et al. Alcohol intake and its relationship with bone mineral density, falls, and fracture risk in older men. J Am Geriatr Soc. 2006;54:1649–1657. doi: 10.1111/j.1532-5415.2006.00912.x. [DOI] [PubMed] [Google Scholar]
- 4.Cawthon PM, Fink HA, Barrett-Connor E, et al. Alcohol use, physical performance, and functional limitations in older men. J Am Geriatr Soc. 2007;55:212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- 5.Mukamal KJ, Mittleman MA, Longstreth WT, Jr, Newman AB, Fried LP, Siscovick DS. Self-reported alcohol consumption and falls in older adults: cross-sectional and longitudinal analyses of the cardiovascular health study. J Am Geriatr Soc. 2004;52:1174–1179. doi: 10.1111/j.1532-5415.2004.52318.x. [DOI] [PubMed] [Google Scholar]
- 6.LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S. Maintaining mobility in late life. II. Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol. 1993;137:858–869. doi: 10.1093/oxfordjournals.aje.a116747. [DOI] [PubMed] [Google Scholar]
- 7.Koster A, Penninx BW, Newman AB, et al. Lifestyle factors and incident mobility limitation in obese and non-obese older adults. Obesity (Silver Spring) 2007;15:3122–3132. doi: 10.1038/oby.2007.372. [DOI] [PubMed] [Google Scholar]
- 8.Adams WL, Garry PJ, Rhyne R, Hunt WC, Goodwin JS. Alcohol intake in the healthy elderly. Changes with age in a cross-sectional and longitudinal study. J Am Geriatr Soc. 1990;38:211–216. doi: 10.1111/j.1532-5415.1990.tb03493.x. [DOI] [PubMed] [Google Scholar]
- 9.Sulsky SI, Jacques PF, Otradovec CL, Hartz SC, Russell RM. Descriptors of alcohol consumption among noninstitutionalized nonalcoholic elderly. J Am Coll Nutr. 1990;9:326–331. doi: 10.1080/07315724.1990.10720388. [DOI] [PubMed] [Google Scholar]
- 10.Volpato S, Pahor M, Ferrucci L, et al. Relationship of alcohol intake with inflammatory markers and plasminogen activator inhibitor-1 in well-functioning older adults: the Health, Aging, and Body Composition study. Circulation. 2004;109:607–612. doi: 10.1161/01.CIR.0000109503.13955.00. [DOI] [PubMed] [Google Scholar]
- 11.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 12.Kurella M, Chertow GM, Fried LF, et al. Chronic kidney disease and cognitive impairment in the elderly: the health, aging, and body composition study. J Am Soc Nephrol. 2005;16:2127–2133. doi: 10.1681/ASN.2005010005. [DOI] [PubMed] [Google Scholar]
- 13.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 14.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: is “no pain, no gain” passe? JAMA. 2001;285:1447–1454. doi: 10.1001/jama.285.11.1447. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 17.Newman AB, Siscovick DS, Manolio TA, et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Heart Study (CHS) Collaborative Research Group. Circulation. 1993;88:837–845. doi: 10.1161/01.cir.88.3.837. [DOI] [PubMed] [Google Scholar]
- 18.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 19.Schoenfeld D. Chi-squared goodness-of-fit tests for the proportional hazards regression model. 1980;67:145–153. Ref Type: Generic. [Google Scholar]
- 20.Reid MC, Concato J, Towle VR, Williams CS, Tinetti ME. Alcohol use and functional disability among cognitively impaired adults. J Am Geriatr Soc. 1999;47:854–859. doi: 10.1111/j.1532-5415.1999.tb03844.x. [DOI] [PubMed] [Google Scholar]
- 21.Guralnik JM, Kaplan GA. Predictors of healthy aging: prospective evidence from the Alameda County study. Am J Public Health. 1989;79:703–708. doi: 10.2105/ajph.79.6.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nelson HD, Nevitt MC, Scott JC, Stone KL, Cummings SR. Smoking, alcohol, and neuromuscular and physical function of older women. Study of Osteoporotic Fractures Research Group. JAMA. 1994;272:1825–1831. doi: 10.1001/jama.1994.03520230035035. [DOI] [PubMed] [Google Scholar]
- 23.Naimi TS, Brown DW, Brewer RD, et al. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Shaper AG. Alcohol and mortality: a review of prospective studies. Br J Addict. 1990;85:837–847. doi: 10.1111/j.1360-0443.1990.tb03710.x. [DOI] [PubMed] [Google Scholar]
- 25.Shaper AG, Wannamethee SG. The J-shaped curve and changes in drinking habit. Novartis Found Symp. 1998;216:173–188. doi: 10.1002/9780470515549.ch11. [DOI] [PubMed] [Google Scholar]
- 26.Bryson CL, Mukamal KJ, Mittleman MA, et al. The association of alcohol consumption and incident heart failure: the Cardiovascular Health Study. J Am Coll Cardiol. 2006;48:305–311. doi: 10.1016/j.jacc.2006.02.066. [DOI] [PubMed] [Google Scholar]
- 27.Djousse L, Biggs ML, Mukamal KJ, Siscovick DS. Alcohol consumption and type 2 diabetes among older adults: the Cardiovascular Health Study. Obesity (Silver Spring) 2007;15:1758–1765. doi: 10.1038/oby.2007.209. [DOI] [PubMed] [Google Scholar]
- 28.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Volpato S, Ferrucci L, Blaum C, et al. Progression of lower-extremity disability in older women with diabetes: the Women’s Health and Aging Study. Diabetes Care. 2003;26:70–75. doi: 10.2337/diacare.26.1.70. [DOI] [PubMed] [Google Scholar]
- 30.Cesari M, Penninx BW, Pahor M, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004;59:242–248. doi: 10.1093/gerona/59.3.m242. [DOI] [PubMed] [Google Scholar]
- 31.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. New England Journal of Medicine. 2006;355:695–703. doi: 10.1056/NEJMsa044316. [DOI] [PubMed] [Google Scholar]
- 32.Coakley EH, Kawachi I, Manson JE, Speizer FE, Willet WC, Colditz GA. Lower levels of physical functioning are associated with higher body weight among middle-aged and older women. Int J Obes Relat Metab Disord. 1998;22:958–965. doi: 10.1038/sj.ijo.0800698. [DOI] [PubMed] [Google Scholar]
- 33.Launer LJ, Harris T, Rumpel C, Madans J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994;271:1093–1098. [PubMed] [Google Scholar]
- 34.Ferrucci L, Izmirlian G, Leveille S, et al. Smoking, physical activity, and active life expectancy. Am J Epidemiol. 1999;149:645–653. doi: 10.1093/oxfordjournals.aje.a009865. [DOI] [PubMed] [Google Scholar]
- 35.Leveille SG, Guralnik JM, Ferrucci L, Langlois JA. Aging successfully until death in old age: opportunities for increasing active life expectancy. Am J Epidemiol. 1999;149:654–664. doi: 10.1093/oxfordjournals.aje.a009866. [DOI] [PubMed] [Google Scholar]
- 36.Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 37.Glynn RJ, Bouchard GR, LoCastro JS, Laird NM. Aging and generational effects on drinking behaviors in men: results from the normative aging study. Am J Public Health. 1985;75:1413–1419. doi: 10.2105/ajph.75.12.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]