Abstract
We work from a life course perspective and identify several reasons to expect age and gender differences in the link between marital quality and health. We present growth curve evidence from a national longitudinal survey to show that marital strain accelerates the typical decline in self-rated health that occurs over time and that this adverse effect is greater at older ages. These findings fit with recent theoretical work on cumulative adversity in that marital strain seems to have a cumulative effect on health over time—an effect that produces increasing vulnerability to marital strain with age. Contrary to expectations, marital quality seems to affect the health of men and women in similar ways across the life course.
Involvement in social relationships benefits physical health and reduces mortality risk; the evidence linking social relationships to health and mortality is as strong as that linking cigarette smoking, blood pressure, and obesity to health (House, Landis, and Umberson 1988). Moreover, the available evidence indicates that, of the specific relationships studied, the marital relationship holds the greatest significance for health. While the married exhibit better health than the unmarried, it is not the case that any marriage is better than no marriage at all when it comes to health benefits. The quality of relationships is also linked to health. Among the married, those in distressed marriages are in poorer health than those in nondistressed marriages (Burman and Margolin 1992), and individuals in low-quality marriages exhibit an even greater health risk than do divorced individuals (Williams 2003).
There are several reasons to think that marital quality would be even more important to health as individuals age. First, some theorists suggest that the marital relationship becomes more salient to individuals later in life (Carstensen 1992), and more salient relationships have stronger effects on individual well-being (Simon 1997). Second, immunological impairment increases with age, and the stress of poor marital quality might further accelerate aging of the immune system (Kiecolt-Glaser and Glaser 2001). Third, chronic conditions that are exacerbated by stress become increasingly common with age, perhaps creating greater biological vulnerability to stress with age (House et al. 1992). It may be that the juxtaposition of psychosocial risk factors (e.g., marital strain) along with increasing biological vulnerability sets the stage for a stronger effect of marital quality on health with advancing age. This possibility fits with recent work showing that disadvantage may accrue over the life course and have a cumulative effect on health (Dannefer 2003).
The knowledge base on marital quality and health is sound and growing, but it currently raises as many questions as it answers. At present, we have no information about how the consequences of marital quality for health might vary over the life course. Most of the available research on marital quality and health relies on age-restricted samples and nonrepresentative populations. Therefore, we have no information on possible age/marital quality interactions in predicting health outcomes in the general population. Those studies with the potential to examine age differences in the effects of marital quality on health have not examined these possible interactions. Finally, the preponderance of evidence from clinical samples suggests that marital strain may have stronger effects on the health of women than men, yet female vulnerability to marital strain may further rely on age, and this possibility has not been addressed empirically.
In the present study, we examine longitudinal data (covering an eight-year period) from a national panel survey to address the following questions: (1) How do positive and negative aspects of marital quality affect physical health? (2) Do these effects vary with age or gender? We use growth curve analysis to examine health trajectories as continuous processes. This approach allows us to investigate individual and group heterogeneity in health trajectories over time and as a function of marital quality.
BACKGROUND AND SIGNIFICANCE
We work from a life course perspective to assess marital quality and health over time. According to Elder and O’Rand (1995:454), “Life course theory is temporal and contextual in locating people in history through birth years and in the life course through the social meanings of age-graded events and activities.” Life course position may be defined by individual characteristics, particularly age, as well as marital characteristics (e.g., marital duration and prior marital history) and parental status (e.g., age and living arrangements of children). In the present study, we focus primarily on age as an indicator of life course position. Age is a particularly important facet of life course position when the focus is on physical health, since there are strong relationships between age and health and age and mortality (Kaplan 1992). Of course, there is also considerable heterogeneity in the health status of individuals of any given age, as a function of differential stress exposure, access to resources, and biological vulnerability (House et al. 1992; Kaplan 1992). We consider how marital quality may contribute to that heterogeneity.
Effect of Marital Quality on Health
Most of the evidence for a marital quality/health link comes from lab-based studies and clinical samples that focus on cardiovascular and neuroendocrine responses to marital strain or from survey research that relies on community samples.
Lab-based studies and clinical populations
Over the past 15 years, many lab-based studies have observed marital conflict and collected biomedical data on cardiovascular reactivity and hormonal responses. The results provide fairly consistent evidence that physiological changes occur during marital conflict, that marital distress impairs immune response, and that marital conflict increases cardiovascular reactivity (see a review in Burman and Margolin 1992). Most of these studies also find stronger adverse effects (in the form of greater physiological reactivity to conflict) on women than men (e.g., Kiecolt-Glaser et al. 1997, 1998).
These studies are based on stress models where marital conflict is viewed as the stressful stimulus. Stress stimulates the production of stress hormones (cortisol, epinephrine, and norepinephrine are the most commonly examined) and evokes a cardiovascular response (e.g., increased heart rate and blood pressure). The problem arises when a stressor becomes chronic—as marital stress often does—and the stress response is sustained over time. The cumulative impact of prolonged chronic stress exposure and the physiological response may then undermine overall health status in the long run: “… physiological responses to stress have cumulative, long term effects on health, including effects on tissue and organ systems, and progression and development of disease” (Robles and Kiecolt-Glaser 2003:6). The longer-term effects of marital conflict on health are seen in clinical populations. Among 189 patients with congestive heart disease, marital quality predicted four-year survival, and this effect was stronger for women (Coyne et al. 2001). In a sample of 292 women with a history of coronary heart disease, Orth-Gomer et al. (2000) found that marital stress almost tripled the risk of recurrent coronary events over a five-year period.
Community-based surveys
Most research on marital quality and health focuses on specific physical symptoms or disease outcomes, but a basic assumption of research in this area is that marital strain—through physiological or behavioral mechanisms—will eventually take a toll on global health status. A few community-based surveys provide support for this position. One longitudinal study of women found worsened physical health in relation to prior marital difficulties (Prigerson, Maciejewski, and Rosenheck 1999). Wickrama et al. (1997) analyzed data from a rural Iowa community and found a significant link between marital quality and physical illness over a three-year period. Good marital quality was inversely associated with baseline levels of physical illness as well as with the rate of decline in health over time; these findings held for both men and women. They conclude that “improving marital quality over time is associated with decreasing physical illness” (Wickrama et al. 1997:153). In a later longitudinal study, Wickrama et al. (2001) found that marital stress significantly increased the risk of hypertension onset for both men and women.
Wickrama and colleagues’ (1997 (2001) excellent studies provide important evidence of the link of marital quality and health in a community sample; however, as they note, the unique qualities of their sample (white, rural, parents of young children) preclude generalization to a more diverse population. It may be that the more conservative cultural and family values found in rural Midwestern communities are associated with a stronger marriage and family orientation, and such an orientation may make marital quality more salient to health and well-being than it is in a cross-section of Western society. Moreover, these studies do not consider the possibility of age differences in the consequences of marital quality.
Age and Gender Differences in the Effects of Marital Quality on Health
As noted earlier, there are several reasons to expect that the health effects of marital quality would be greater at older ages. House (1992) argues that the impact of psychosocial risk factors on health may depend on age, and we contend that marital stress is such a risk factor. Gender, in addition to age, shapes social experiences over the life course in ways that may influence marital quality and health outcomes. For example, women consistently report lower marital quality than men in national surveys (e.g., Umberson et al. 1996), and relationships may be more salient to the well-being of women than men (Kessler and McLeod 1984). Clinical studies consistently show that women are more physiologically reactive to marital stress than are men (Kiecolt-Glaser et al. 1996). On the other hand, a growing body of evidence indicates that, although men’s and women’s relationships may differ in quantity and quality, the same levels of relationship quality have similar effects on the psychological well-being of men and women (Umberson et al. 1996). Moreover, Wickrama et al. (1997, 2001) find no evidence of gender differences in their community studies of marital quality and physical well-being. Finally, gender differences in the effects of marital quality on well-being may depend on age, and this possibility has not been addressed empirically. Moen (2001) emphasizes that age and gender work together to shape life experiences for men and women across the life course. The importance of marital quality for health may then differ for men and women at different points in the life course.
Reciprocity and Health Trajectories
The stress model suggests that marital quality, particularly marital strain, has a causal effect on physical health, but physical illness may also affect marital quality. Booth and Johnson (1994) analyze national longitudinal data and conclude that health decline has a modest effect on one of two measures of perceived marital quality. Wickrama et al. (1997) used latent growth curve modeling in their Iowa sample to address the temporal ordering of marital quality and health; they conclude that “… the effect of marital quality on physical illness accounts for most of the association between marital quality and physical illness …” (p. 153).
Some groups and individuals experience relative stability in health over time, while others experience steady or precipitous declines in health, and still others experience improvement in health (House et al. 1992; Kaplan 1992). Latent growth curve models are ideally suited to examining trajectories of change in health over time (McDonough and Berglund 2003; Wickrama et al. 1997). They “offer a flexible way to examine relationships between life course processes at the individual level that are heterogeneous across individuals, and to identify sources of heterogeneity” (George and Lynch 2003:359).
In the present study, we use latent growth curve models to examine trajectories in health over time and link these trajectories to marital dynamics. Moreover, because we can examine the dynamic relationship between marital quality and health over time, we can begin to address issues of reciprocity between marital quality and health. We use growth curve techniques to assess the following four hypotheses:
-
Hypothesis 1
Poor marital quality is associated with lower baseline levels of self-rated health, and this association is stronger at older ages.
-
Hypothesis 2
Poor marital quality accelerates the decline in self-rated health over time, and this effect is stronger with advancing age.
-
Hypothesis 3
Marital quality will have stronger effects on health among women than men, particularly at older ages.
-
Hypothesis 4
Although there may be some reciprocity between marital quality and self-rated health, the effect of marital quality on self-rated health will predominate.
DATA AND METHODS
Data
We use three waves of data from the Americans’ Changing Lives (ACL) panel survey of individuals in the contiguous United States (House 1986). The original sample (ages 24–96 in 1986) was obtained using multistage stratified area probability sampling with an oversample of African Americans, persons over 59 years of age, and married women whose husbands were over the age of 64. Face-to-face interviews lasting approximately 90 minutes each were conducted with individuals in 1986 (N = 3,617), 1989 (N = 2,867), and 1994 (N = 2,398).
In 1986, 1,904 married individuals who were either non-Hispanic white or African American were interviewed. Seventy-one percent (N = 1,352) of these individuals were interviewed in all three waves of data collection, while 11.4 percent (N = 217) died by 1994, and the rest (17.6%, N = 335) did not respond to one or both of the follow-up surveys. Of the 1,352 individuals who were interviewed at all three time points, 78.3 percent (N = 1,059) remained married to the same spouse over the eight-year period, 8.4 percent (N = 113) divorced, 12.1 percent (N = 164) were widowed, and 1.2 percent (N = 16) were separated without divorcing during this period.
In this study, we look at the 1,049 individuals who were continuously married across the three waves of data collection and who were either non-Hispanic white or African American (too few cases were available to assess other racial/ethnic groups). All analyses include a binary control variable indicating whether the individual is in a first or subsequent marriage (N = 182). We employ the Full Information Maximum Likelihood (FIML) missing-data-handling feature of Mplus to deal with the 38 missing values on positive marital quality and 49 missing values on negative marital quality among 1,049 individuals. In the present study, change over time refers to change over the eight-year study period.
Selectivity in the Sample
Our sample includes individuals who were continuously married over a period of at least eight years. We emphasize that, in the present study, inference applies to a selected population of individuals who may be healthier and more prone to stay married. While not representative of the entire population, this is a random sample from this select population of intact marriages. Because one limitation of this study is that results may be less applicable to the subpopulation of individuals who have a higher risk of divorce and hence have shorter average marital durations, we estimated a hazard model for divorce based on the entire ACL sample over the eight-year interval as a function of a number of variables shown to be associated with divorce risk in previous studies (number of previous marriages, age at marriage, teenager when married, high financial strain, employment of wife, stepchild in the home, marital duration, recent thoughts of divorce, spouse has done things respondent can never forgive, African American race, and years of education—all measures were assessed at Time 1 and questions about marriage referred to one’s marriage at Time 1) (White 1990). Using a Heckman-type correction, we include the predicted hazard from this model as a control variable in the subsequent models on our sample of intact marriages (Heckman 1976).
Measures
Marital quality
Marriage scholars emphasize the importance of distinguishing different dimensions of marital quality (Glenn 1990). In preliminary factor analyses, we examined the six questions about marital quality that were asked at all three time points in the ACL. We determined that these measures form two latent constructs, which we call positive marital experience and negative marital experience. The measurement model relates a vector of observed indicators to a latent marital quality factor. More formally, the ith individual’s value on the jth indicator at time t is expressed as
| (1) |
where Fit is a latent factor with measurement slopes (or factor loadings) λj, measurement intercepts αj, and normally distributed measurement errors eij.
Factors are scaled so that higher values indicate higher levels of the intended construct. We then incorporate this measurement model into our specification of the latent growth curve model. To ensure that change over time reflects growth rather than change in the measurement scale, the scales for each indicator at each wave of measurement are standardized using the time 1 mean and standard deviation (Bryk and Raudenbush 1987). More formally, each latent marital quality factor for the ith individual at time t can be specified as a linear function of growth parameters, resulting in a linear latent growth curve model with latent intercept I representing the level of the factor at time 0 and latent slope S describing latent factor change as a function of time T. The latent linear growth model for level and change in the latent factor F can be written as
| (2) |
where rit is a normally distributed random error.
To help ensure the comparability of the latent constructs of marital quality over time, the factor loadings λj and αj in equation (1) are constrained to be equal across waves. Furthermore, to ensure that the latent construct of marital quality is the same from model to model, the same sets of estimated factor loadings from the model without covariates are used for further analyses in models with covariates. All factor loading estimates are statistically significant (we present these in parentheses below).
Positive marital experience is a latent variable composed of four items. The first item, marital satisfaction (factor loading = 1.000), is based on responses to the question, “How satisfied are you with your marriage?” (scored 1–5). The second (factor loading = 1.178) and third (factor loading = .876) items are based on responses to the questions (1) “How much does your (husband/wife) make you feel loved and cared for?” and (2) “How much is (he/she) willing to listen when you need to talk about your worries or problems?” (scored 1–5). The fourth item (factor loading = .456) considers whether one’s spouse is a person with whom the respondent can really share his or her very private feelings and concerns (0 = no, 1 = yes). Factor determinancy coefficients indicate the quality of the factor score estimates as follows: .919 for time 1, .930 for time 2, and .930 for time 3 (see Muthén and Muthén 1998).
Negative marital experience is a latent variable measured with two items. First (factor loading = 1.000), respondents were asked, “How often do you feel bothered or upset by your marriage?” (scored 1–5). Second (factor loading = 1.557), respondents were asked, “How often would you say the two of you typically have unpleasant disagreements or conflicts?” (scored 1–7). Factor determinancy coefficients are .817 at time 1, .778 at time 2, and .815 at time 3.
Life course and sociodemographic variables
Our primary proxy for life course position is age of the respondent, measured in years. A squared term for age was also included to assess potential nonlinear effects of age. The squared term was not significant in any model and was not included in final models. We also include a measure for parental status, another gauge of life course position. Parental status is measured with five dummy variables as follows: (1) minor child at home (child younger than 18 living at home = 1, otherwise 0), (2) adult child at home (child 18 years or older living at home = 1, otherwise 0), (3) minor child away (child younger than 18 living away from home = 1, otherwise 0), (4) adult child away (child 18 or older living away from home = 1, otherwise 0), and (5) no children (the reference group). All models are adjusted for the effect of additional sociodemographic characteristics that may be associated with health, including gender (0 = female, 1 = male), race (0 = other, 1 = black), education (number of years completed), and total family income in 1986 ($1,000s). Table 1 presents means and standard deviations for all variables in the analysis. In all subsequent models, all continuous independent variables such as age, education, and family income are centered at their respective means.
TABLE 1.
Means and Standard Deviations of Independent Variables (N = 1,049)
| Mean | SD | |
|---|---|---|
| Age (decades) | 4.99 | 1.48 |
| Age and living arrangements of children | ||
| Minor child at home | .41 | .49 |
| Adult child at home | .16 | .37 |
| Minor child away | .03 | .18 |
| Adult child away | .57 | .50 |
| No children | .07 | .26 |
| Gender (1 = Male) | .46 | .50 |
| Race (1 = African American) | .19 | .40 |
| Education (years) | 12.53 | 2.94 |
| Household income (in $1,000s) | 35.37 | 24.45 |
| Previous divorce | .18 | .40 |
| Marital quality | ||
| Positive marital experiences (Time 1) | .00 | .66 |
| Positive marital experiences (Time 2) | −.09 | .72 |
| Positive marital experiences (Time 3) | −.09 | .76 |
| Negative marital experiences (Time 1) | .00 | .41 |
| Negative marital experiences (Time 2) | .06 | .49 |
| Negative marital experiences (Time 3) | .14 | .49 |
| Self-rated health | ||
| Time 1 | 3.73 | .98 |
| Time 2 | 3.54 | .98 |
| Time 3 | 3.50 | 1.03 |
| Divorce/separation hazard | −.16 | .18 |
Self-rated health
Self-rated physical health status is measured with the item, “Would you say your health in general is excellent, good, fair, or poor?” (scored 1–4, with 4 indicating better health). Some evidence suggests that individuals tend to compare their health with the health of others their age when making health self-appraisals (Idler 1993), yet the validity of self-appraised health as a measure is fairly well-established; self-appraised physical health is predictive of subsequent disability (Ferraro, Farmer, and Wybraniec 1997) and mortality (Idler and Benyamini 1997).
Analytical Design
Latent growth curve analysis
Each individual has a marital quality history and a health history. Moreover, everyone begins the ACL study period with different baseline levels of marital quality and health. We are interested in predicting health trajectories from that baseline as well as the dynamic linkages between marital quality and health over time. For example, marital quality may have short-term or long-term consequences for health trajectories. It is also possible that poor health status has some effect on marital quality trajectories. Latent growth curve models are ideally suited to analyzing the dynamic relationship between marital quality and health over time.
We use latent linear growth models to assess the effects of marital quality constructs, age, and additional control variables on initial level and change in self-rated health over time. Initial level and rate of change in self-rated health are viewed as growth parameters that vary randomly among respondents. Our models account for systematic variation in growth parameters that is attributable to age and marital quality factors in addition to other control variables. The structural parameters from this part of the model provide the basis for assessing effects of key variables on level of and change in self-rated health.
The growth parameters Ii and Si depend on a set of sociodemographic characteristics X and initial levels of marital quality FMQ1 as follows:
| (3) |
and
| (4) |
where the a’s and b’s denote structural parameters of primary substantive interest, and the u’s are normally distributed error terms. The variance in the u terms measures the extent to which latent slopes and intercepts vary across subjects. The covariance between the u terms measures the degree of dependence between initial levels of self-rated health and change in self-rated health over time.
Subsequent models treat marital quality and self-rated health as two domains of a more complex parallel growth process. These models investigate possible reciprocal effects by both allowing the growth trajectory of self-rated health to depend on initial levels of marital quality and allowing change in marital quality to be affected by initial levels of self-rated health.
RESULTS
Consistent with other research (see Umberson et al. 2005), results from growth curve models without covariates indicate that marital quality changes over the eight-year study period, and this change is in the direction of diminishing marital quality over time. Using a model specification similar to that of equations (3) and (4), we find that positive marital experiences generally decreased over the eight-year period (b = −.011; p < .001) and negative marital experiences increased (b = .017; p < .001). We also find evidence of variation in the random intercept for both measures (var(uPI1) = .434 and var(uNI1) = .224, p ≤ .001) with modest variation in random slopes (var(uPI2) = .002 and var(uNI2) = .001, p < .05). The covariance parameters are statistically 0 and hence provide no evidence that changes in positive or negative experiences occur at a faster or slower rate for individuals who are high or low on initial marital quality.
Results from growth curve models with no covariates indicate that self-rated health also changes over the eight-year study period, and this change is in the direction of diminishing health over time (b = −.026; p < .001). This is what we would expect to find in an aging population. We also find evidence of variation in the random intercept (var(uPH1) = .602, p < .001) and variation in the random slope (var(uPH2) = .003, p < .001). The random slope and intercept are negatively correlated (cov(uPH1, uPH2) = −.008, p = .069), suggesting that those with lower initial levels of self-rated health exhibit a less steep decline over time than do those with higher initial levels of self-rated health. This may occur because those in poorer health have less room for decline over time compared to those who begin the study with the highest levels of self-rated health. Because older people have lower initial levels of self-rated health, they tend to exhibit a slower rate of change in health over the study period.
Estimated Effects of Marital Quality on Health Trajectories
Table 2 presents the results from growth curve models predicting initial levels of self-rated health (the latent intercept) and the rate of change in self-rated health over time (the latent slope). Model 1 presents results that did not include interaction terms, and model 2 presents the interaction results. The means of the growth parameters reflect level of and change in health after controlling for covariate effects. The nonsignificant term for the mean of the latent slope suggests that the rate of decline in self-rated health over the study period is explained by the addition of covariates.
TABLE 2.
Effect of Marital Quality on Self-Rated Health from Linear Growth Curve Models (N = 1,049)
| Model 1 (Basic Model)
|
Model 2 (Interaction Model)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| A. Latent Intercept
|
B. Latent Slope
|
C. Latent Intercept
|
D. Latent Slope
|
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| 1986 life course | ||||||||
| Age (in decades and centered at 4.93) | −.020 | .036 | −.005 | .005 | −.016 | .037 | −.006 | .005 |
| Age squared | — | — | — | — | — | — | — | — |
| Minor child at home | .128 | .081 | −.015 | .011 | .131 | .081 | −.016 | .011 |
| Adult child at home | −.029 | .076 | .005 | .010 | −.025 | .076 | .007 | .010 |
| Minor child away | −.073 | .161 | −.001 | .022 | −.070 | .162 | .002 | .022 |
| Adult child away | −.105 | .088 | .008 | .012 | −.101 | .088 | .008 | .012 |
| Marital quality | ||||||||
| Positive marital experiences | .164** | .052 | .000 | .007 | .168** | .052 | .000 | .007 |
| Negative marital experiences | −.043 | .080 | −.025* | .011 | −.041 | .080 | −.025* | .011 |
| Age * positive marital experiences | — | — | — | — | −.034 | .038 | −.002 | .005 |
| Age * negative marital experiences | — | — | — | — | −.050 | .054 | −.015* | .007 |
| Sociodemographic controls | ||||||||
| Gender (1 = Male) | .034 | .056 | −.008 | .008 | .029 | .056 | −.009 | .008 |
| Race (1 = African American) | −.103 | .073 | .006 | .010 | −.105 | .073 | .005 | .010 |
| Education | .065*** | .011 | −.002 | .001 | .065*** | .011 | −.002 | .001 |
| Household income (in $1,000s) | .003* | .001 | .000 | .000 | .003* | .001 | .000 | .000 |
| Previous divorce | .095 | .081 | −.018 | .011 | .095 | .082 | −.016 | .011 |
| Divorce/separation hazard | −.418 | .236 | .020 | .032 | −.440 | .245 | .028 | .033 |
|
| ||||||||
| Means of growth parameters | 2.720*** | .161 | .004 | .022 | 2.704*** | .162 | .004 | .022 |
| Variances in growth parameters | .495*** | .040 | .002 | .002 | .494*** | .039 | .002 | .002 |
| R-square | .194 | .175 | .195 | .199 | ||||
| Model fit index | CFI = .983 | RMSEA = .036 | CFI = .984 | RMSEA = .033 | ||||
p < .05;
p < .01;
p < .001 (two-tailed tests)
Notes: — indicates the parameter not in model. CFI stands for comparative fit index. RMSEA stands for root mean square error of approximation.
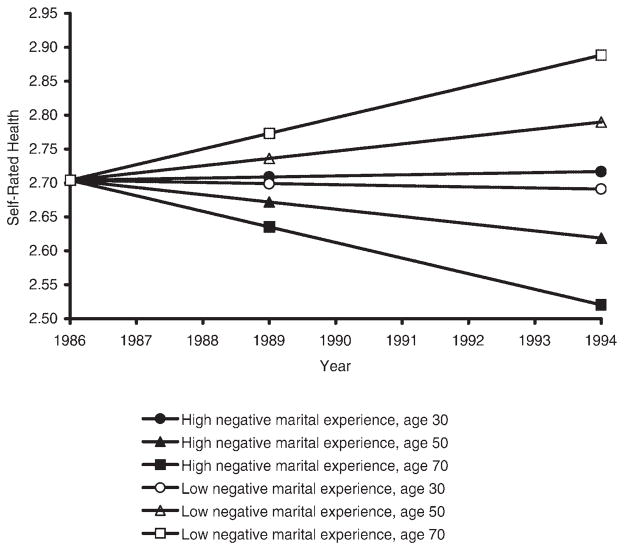
The results in Table 2 show that positive marital experiences are associated with higher initial levels of self-rated health, while negative marital experiences are not significantly associated with initial levels of self-rated health. Results from the interactive model (model 2) suggest that the effect of negative marital experiences on the rate of change in health depends on age of the respondent (as indicated by the significant interaction of age with negative marital experience in panel D). We illustrate this age effect in Figure 1, where we present the predicted trajectories of self-rated health for three age groups (age 30, age 50, and age 70 at time 1) at both high and low levels of negative marital experiences. In this example, “high” refers to those respondents who score one standard deviation or higher above the mean on negative marital experience, and “low” refers to those who score one standard deviation or lower below the mean. All groups begin at the same average initial point on self-rated health at time 1.
FIGURE 1.
Predicted Trajectories of Self-Rated Health by Age and Negative Marital Experience, 1986–1994
Figure 1 suggests that negative marital experience is more important to the health trajectories of older individuals than to younger ones. At high levels of negative marital experience, the oldest respondents experience a faster rate of decline in self-rated health than do the youngest respondents. The adverse effects of negative experiences may become apparent only at older ages either because they take a cumulative toll on health or because health status becomes more vulnerable to stress at older ages. The predicted trajectory for 70-year-olds with the lowest levels of marital negativity in Figure 1 suggests that there may also be greater benefits of the absence of strain at older ages.
Note that the results from models with no covariates indicated that age is associated with worsening health over the eight-year period for the sample as a whole. Once covariates are included in models, the results suggest how marital quality would affect health trajectories if all else were equal. Under these conditions (illustrated in Figure 1), we see that negative marital experiences have more impact on the health of older people in positive and negative directions. All else being equal, the absence of marital negativity may benefit health trajectories, but only at older ages. Similarly, all else being equal, the presence of marital negativity may be detrimental to health trajectories, but only at older ages.
Other Covariates
We consider age and parental status as measures of life course position. While the effect of marital strain on self-rated health depends on age, parental status is not significantly associated with self-rated health. Education and income are associated with better initial levels of health but do not slow the rate of decline in self-rated health over time. The frequent observation of the poorer self-assessed health of women compared to men is not evident in our results. Additional analyses indicate that this association does exist in the ACL data, but only when the sample is not restricted to continually married adults and when controls for the full range of sociodemographic characteristics are not included in our models. This fits with recent research indicating that the gender gap in self-assessed health disappears when gender differences in demographic characteristics and social resources are controlled (Denton, Prus, and Walters 2004).
We also assessed the possibility of gender differences in the effects of marital quality on health and the possibility that gender differences in the effects of marital quality on health might depend on age. None of the terms for gender by marital quality or gender by marital quality by age interactions were statistically significant, and they were thus omitted in final models. These results suggest that the effects of marital quality on self-rated health may be similar for men and women across the life course, even though the effect of negative marital experiences on health trajectories may depend on age.
We find marginal evidence of selectivity (suggested by the inverse association of the estimated divorce hazard term with initial levels of self-rated health, p ≤ 10). Inclusion of the estimated hazard term does not alter our results regarding the estimated effects of marital quality on self-rated health (compared to models without the hazard term), providing more confidence in our estimates from the final models.
Marital Quality and Self-Rated Health: Parallel Growth Processes
Our growth curve analysis provides evidence that marital quality affects subsequent assessments of health. However, self-rated health may also influence subsequent levels of marital quality (Booth and Johnson 1994). We are unable to fully address the question of reciprocity with the present data, but we can begin to investigate this issue with a structural equation model for individual trajectories of change in marital quality and physical illness and the reciprocal relationships between these trajectories. In these models, both marital quality and self-rated health are viewed as parallel domains of a more complex growth process. Four growth parameters are presented in Table 3: the intercept of initial marital quality (IMQ), the slope/linear change in marital quality (SMQ), the intercept of initial self-rated health (IPH), and the slope/linear change in self-rated health (SPH). Following Muthén (1997), we allow the latent intercept of each growth process to impact the latent slope of the corresponding process as described below. The latent growth models for marital quality (indexed by subscript MQ) and self-rated physical health (indexed by subscript PH) are specified as follows:
| (5) |
and
TABLE 3.
Estimated Effects of Reciprocal Relationships between Marital Quality and Self-Rated Health (ML Estimates with Robust Standard Errors) (N = 1,049)
| Latent Intercept of Marital Quality (IMQ) | Latent Slope of Marital Quality (SMQ) | Latent Intercept of Self-Rated Physical Health (IPH) | Latent Slope of Self-Rated Physical Health (SPH) | |
|---|---|---|---|---|
| Positive marital experiences | ||||
| Initial marital quality | — | — | — | .006 |
| Initial self-rated health | — | −.002 | — | — |
| Means of growth parameters | .243* | −.007 | 2.739*** | .009 |
| Variances in growth parameters | .347*** | .002*** | .510*** | .002 |
| R-square | .139 | .038 | .167 | .104 |
| cov (μMQ1, μMQ2) | .001 | |||
| cov (μPH1, μPH2) | −.006 | |||
| cov (μPH1, μMQ1) | .070*** | |||
| cov (μPH2, μMQ2) | .000 | |||
| Model fit index | CFI = .985 | RMSEA = .050 | ||
| Negative marital experiences | ||||
| Initial marital quality | — | — | — | −.025* |
| Initial self-rated health | — | .000 | — | — |
| Means of growth parameters | −.199** | .011 | 2.740*** | .005 |
| Variances in growth parameters | .155*** | .000*** | .512*** | .002 |
| R-square | .080 | .026 | .167 | .145 |
| cov (μMQ1, μMQ2) | .002*** | |||
| cov (μPH1, μPH2) | −.006 | |||
| cov (μPH1, μMQ1) | −.025* | |||
| cov (μPH2, μMQ2) | .000 | |||
| Model fit index | CFI = .964 | RMSEA = .085 | ||
p < .05;
p < .01;
p < .001 (two-tailed tests)
Notes: — indicates the parameter not in model. Age, gender, race, education, family income, previous divorce, and divorce/separation hazard are controlled in both models. CFI = comparative fit index; RMSEA = root mean square error of approximation; COV = covariance.
| (6) |
The latent intercepts for each process are
| (7) |
and
| (8) |
with latent slopes
| (9) |
and
| (10) |
We also estimate covariances between errors in growth parameters within and across processes.
The results presented in Table 3 indicate that initial levels of marital quality (positive and negative aspects) are associated with initial levels of health in the expected directions (i.e., better marital quality/better self-rated health) for the total sample, as shown by the positive estimated covariance between the latent intercepts of these growth processes (cov(uPH1, uMQ1) = .070). Table 3 also shows that initial negative marital experiences affect the rate of change in health over time (more negativity/a faster decline in health) but that initial self-rated health does not affect the rate of change in marital quality over time. Thus, we find no evidence that initial level of self-rated health or change in health over time is associated with marital quality trajectories over time (positive or negative marital experiences). Overall, then, these results are more consistent with the interpretation that initial levels of negative marital experience affect health trajectories than vice versa.
We also estimated the models shown in Table 3, adding a multiple group analysis for three different age groups (24–44, 45–64, 65 and older) to continue our investigation of age differences in the link of marital quality and health (not shown). These results are consistent with our earlier results. Initial levels of positive marital experience are not associated with the rate of change in health for any age group. In addition, the multiple group analysis reveals a significant effect of initial marital negativity on trajectories of health only in the oldest age group (i.e., those ages 65 and older). The trend is in the same direction at younger ages; however, the weaker associations do not attain statistical significance.
DISCUSSION
We use growth curve techniques to estimate individual health and marital quality trajectories and the covariance between them. An investigation of individual trajectories can reveal complexities of change over time and interindividual associations among these intraindividual changes that would not otherwise be revealed by traditional autoregressive techniques. Our results suggest that marital quality has significant effects on health trajectories in the general population. While self-rated health tends to decline over time for the sample as a whole, it appears that marital strain accelerates this decline in a representative sample of adults. Moreover, marital strain appears to matter more for health as individuals age.
Why Age Matters
Several significant bodies of literature provide possible explanations for the apparent increase in physical vulnerability to marital strain with age. First, marital difficulties are a key source of stress for individuals, and lab-based and clinical studies show that marital stress can undermine immune function and activate cardiovascular reactivity (Burman and Margolin 1992). Kiecolt-Glaser and Glaser (2001) report that immune functioning declines with age and that stress has more adverse effects on immune functioning as individuals age. It then follows that, over time, marital stress would undermine immune functioning more at older ages, thus having stronger adverse effects on health at older ages.
Second, a growing literature suggests that disadvantage (or advantage) can have a cumulative effect on health (Dannefer 2003). Marital strain appears to take a toll on health, and this toll may be cumulative so that the erosion of health in response to negative experiences is more apparent at older ages. This is not unlike the cumulative effect of smoking cigarettes: The adverse effects may take many years to appear, but persistent smoking eventually takes its toll on health.
Third, chronic conditions become more common with age, and these conditions may provide points of biological vulnerability in the face of stress (House et al. 1992). For example, cardiovascular disease becomes more prevalent with advancing age. If marital stress serves to activate and sustain cardiovascular reactivity (e.g., high blood pressure, elevated heart rate), those persons with cardiovascular disease (among whom the aged are overrepresented) may be more vulnerable to this source of stress.
Fourth, as individuals age and lose key figures in their lives, they may begin to reflect more on the most important relationships and sources of meaning in their lives (Carstensen, Gottman, and Levenson 1995). The majority of married persons identify their spouse as their most important social tie and confidant (Umberson et al. 1996), and, for many persons, the marital relationship is a central source of meaning. Relationships carrying more symbolic meaning for individuals may be more important for mental health (Simon 1997), and this psychological mechanism may partly explain why marital difficulties become more important to health at older ages.
Mechanisms Linking Marital Quality and Health
An important next step is to identify the array of social, psychological, behavioral, and biological mechanisms through which marital quality affects health at different ages. Wickrama et al. (1997) show that depression and health behavior are mechanisms through which marital quality affects self-rated health. Yet the most important mechanisms linking marital quality and health may depend on age. For example, the impact of marital quality on alcohol consumption (a behavioral mechanism) may be more important to health at younger ages, while the impact of marital quality on depression (a psychological mechanism) may be more important at older ages. Future research should consider how the specific mechanisms linking marital quality and health may vary over the life course. We are currently analyzing qualitative data from in-depth interviews with couples of different age cohorts to explore some of the dynamics and processes through which marital quality may affect some of these mechanisms.
Positive Versus Negative Dimensions of Marital Quality
We examine both positive and negative marital experiences and find that only the negative experiences significantly affect self-rated health trajectories. This finding fits with previous research showing that negative aspects of relationships have stronger effects on psychological well-being than do positive aspects of relationships (Taylor 1991). Negative aspects of relationships may be more important to well-being because they are more salient in the daily lives of individuals. Individuals tend to mentally replay negative encounters more than they replay positive ones (Taylor 1991). The tendency to worry over negative relationships may contribute to the stronger effects of marital negativity that we find in our study. The classic stress and coping perspective is that stress activates a physiological response that, if sustained over time, eventually undermines physical health. The positive aspects of relationships may not have the power to enhance physiological response to measurably affect health in a nonclinical population.
Limitations of Key Measures
We were constrained by the availability of key measures of marital quality in this study. In fact, our inability to discern significant effects of positive marital experiences on health may reflect this limitation. Improvement in measurement might serve to reveal stronger linkages between marital quality and health than we find here. While other health measures (e.g., chronic conditions, disability) should be considered in future studies, we were particularly interested in extending lab-based research to test the possibility that marital strain has long-term effects on global health status. To this end, we focused on self-rated health, a measure that exhibits good reliability in survey research (Ferraro et al. 1997). However, self-reports (of health and of marital quality) are limited because they may be influenced by a number of factors, including personality and psychological well-being. Future research should assess additional measures of marital quality and health—perhaps collected through observational methods and biomedical data—and determine whether the linkages between marital quality and health are consistent across measurement types.
Reciprocity Between Marital Quality and Self-Rated Health
Our emphasis on the impact of marital quality on health trajectories is driven by theoretical work on stress and coping and research on relationships as a potential source of stress in individuals’ lives. Yet one’s health might also affect marital quality trajectories. For example, physical illness or disability may interfere with a partner’s ability to participate in housework, child care, sexual activity, and paid work activities—all factors that might undermine marital quality. Our results do not rule out the possibility of reciprocity between marital quality and health, but the present data suggest a stronger association of marital quality with subsequent health than vice versa. Our measures may underestimate the impact of health on marital quality trajectories. For example, a serious illness or health event may be required to trigger change in marital quality trajectories, and we focus on an overall measure of self-rated health rather than key health events. Moreover, we focus on the respondents’ views of marital quality and their own health rather than the health of a partner. Marital assessments may be more strongly affected by a partner’s illness than by one’s own illness (Booth and Johnson 1994). Future research should consider health events and overall health status of the respondent and partner in relation to marital quality trajectories.
Selectivity
A potential problem with marital quality research is that marriages of poorer quality and worse health may be removed from the population over time, producing a healthier sample with higher-quality marriages at older ages. We find some evidence for selectivity in our sample: There is a marginally significant association of an estimated divorce hazard term with initial levels of self-reported health (p ≤ .10). While introduction of the hazard term does not alter results (compared to models that did not include the estimated hazard term), we cannot rule out the possibility of selection bias in our results. We caution that inference in this study applies to a selected population of individuals who remain married over an eight-year period. If selection is operative and our analytic sample is healthier and happier than a random sample of the population, then we are likely to have underestimated the effects of marital quality on health.
Gender
The life course perspective suggests that men and women experience relationships differently across the life course (Moen 2001) in ways that might affect both marital quality and health outcomes. Perhaps most significantly, lab-based studies consistently show that women are more physiologically reactive than men in response to marital stress (Kiecolt-Glazer et al. 1996). In light of these findings, we expected that marital quality would have stronger effects on the health of women than men, particularly at older ages. Yet we find no evidence of gender differences in the effects of marital quality on health at any age. The absence of a gender difference might reflect the limitations of our measures. Or it may be that women’s greater physiological reactivity in response to marital strain in the lab does not translate into actual cumulative effects on overall health status. While previous research suggests that women are more likely than men to ruminate about their relationship difficulties (Nolen-Hoeksema 2001), rumination and review may serve as a release to mitigate physiological responses to stress among women. Future research should consider that the short-term and long-term physiological responses to stress may differ for men and women and that this difference may further depend on age.
CONCLUSION
A substantial body of evidence points to the salutary effects of marital relationships for health (Waite and Gallagher 2000); however, all marriages are not equally beneficial to health. Among the married, negative marital encounters speed up declines in self-rated health over time. Unhappily married individuals have yet another reason to identify marital difficulties and seek to improve marital quality: Their very health may depend on it. Moreover, there is no reason for clinicians and policy makers to think that marital quality is less important for older couples. In fact, the negative aspects of marriage appear to become more consequential for health as individuals age.
Biographies
Debra Umberson is Professor and Chair of Sociology and Research Associate at the Population Research Center at The University of Texas at Austin. Her research focuses on gender, relationships, and health across the life course. She is currently writing a book that blends qualitative and quantitative data in the study of marital quality over the life course, and she is preparing a new study on relationships and health behavior over the life course.
Kristi Williams is Assistant Professor of Sociology at The Ohio State University and Research Associate at The Ohio State University Initiative in Population Research. Her research examines the influence of support and strain in family and other personal relationships on mental and physical health, with a particular focus on gender and life course variations in these patterns. Her recent projects include an examination of the influence of marital and cohabitation transitions on the health and well-being of single mothers and a National Institute on Aging-funded study of life course variations in the stress-buffering role of personal relationships.
Daniel A. Powers is Associate Professor of Sociology and Research Associate at the Population Research Center at The University of Texas at Austin. His recent work uses sibling data to examine family structure and family formation as joint processes. He is also involved in research on racial disparities in infant mortality by cause of death. He conducts methodological work on longitudinal data for categorical outcomes.
Hui Liu is a graduate student in the Department of Sociology and Population Research Center at The University of Texas at Austin. Her research interests include health, mortality, family, and quantitative methods.
Belinda Needham is a doctoral candidate in the Department of Sociology at The University of Texas at Austin. She specializes in the study of gender and health and is particularly interested in the link between mental and physical health over the life course.
Footnotes
This research was supported by grant RO1 AG17455 from the National Institute on Aging.
Contributor Information
DEBRA UMBERSON, University of Texas at Austin.
KRISTI WILLIAMS, The Ohio State University.
DANIEL A. POWERS, University of Texas at Austin
HUI LIU, University of Texas at Austin.
BELINDA NEEDHAM, University of Texas at Austin.
References
- Booth Alan, Johnson David R. Declining Health and Marital Quality. Journal of Marriage and Family. 1994;56:218–23. [Google Scholar]
- Bryk Anthony S, Raudenbush Stephen W. Application of Hierarchical Linear Models to Assessing Change. Psychological Bulletin. 1987;101:147–58. [Google Scholar]
- Burman Bonnie, Margolin Gayla. Analysis of the Association between Marital Relationships and Health Problems: An Interactional Perspective. Psychological Bulletin. 1992;112:39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Carstensen Laura L. Social and Emotional Patterns in Adulthood: Support for Socioemotional Selectivity Theory. Psychology and Aging. 1992;7:331–38. doi: 10.1037//0882-7974.7.3.331. [DOI] [PubMed] [Google Scholar]
- Carstensen Laura L, Gottman John M, Levenson Robert W. Emotional Behavior in Long-Term Marriage. Psychology and Aging. 1995;10:140–49. doi: 10.1037//0882-7974.10.1.140. [DOI] [PubMed] [Google Scholar]
- Coyne James C, Rohrbaugh Michael J, Shoham Varda, Sonnega John S, Nicklas John M, Cranford James A. Prognostic Importance of Marital Quality for Survival of Congestive Heart Failure. The American Journal of Cardiology. 2001;88:526–29. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- Dannefer Dale. Cumulative Advantage/Disadvantage and the Life Course: Cross-fertilizing Age and Social Science Theory. Journals of Gerontology. 2003;58B:327–37. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Denton Margaret, Prus Steven, Walters Vivienne. Gender Differences in Health: A Canadian Study of the Psychosocial, Structural and Behavioural Determinants of Health. Social Science and Medicine. 2004;58:2585–2600. doi: 10.1016/j.socscimed.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Elder Glen H, O’Rand Angela. Adult Lives in a Changing Society. In: Cook Karen S, Fine Gary A, House James S., editors. Sociological Perspectives on Social Psychology. Needham Heights, MA: Allyn and Bacon; 1995. pp. 452–75. [Google Scholar]
- Ferraro Kenneth F, Farmer Melissa M, Wybraniec John A. Health Trajectories: Long-Term Dynamics among Black and White Adults. Journal of Health and Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- George Linda K, Lynch Scott M. Race Differences in Depressive Symptoms: A Dynamic Perspective on Stress Exposure and Vulnerability. Journal of Health and Social Behavior. 2003;44:353–69. [PubMed] [Google Scholar]
- Glenn Norval D. Quantitative Research on Marital Quality in the 1980s: A Critical Review. Journal of Marriage and the Family. 1990;52:818–31. [Google Scholar]
- Heckman James J. The Common Structure of Statistical Models of Truncation, Sample Selection and Limited Dependent Variables and a Simple Estimator for Such Models. Annals of Economic and Social Measurement. 1976;5:475–92. [Google Scholar]
- House James S. Americans’ Changing Lives: Wave 1 [MRDF] Ann Arbor, MI: Survey Research Center; 1986. [Google Scholar]
- House James S. Aging, Health Behaviors, and Health Outcomes: Some Concluding Comments. In: Warner Schaie K, Blazer Dan, House James S, editors. Aging, Health Behaviors, and Health Outcomes. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. pp. 179–84. [Google Scholar]
- House James S, Kessler Ronald C, Herzog Regula A, Mero Richard P, Kinney Ann M, Breslow Martha J. Social Stratification, Age, and Health. In: Warner Schaie K, Blazer Dan, House James S, editors. Aging, Health Behaviors, and Health Outcomes. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. pp. 1–32. [Google Scholar]
- House James S, Landis Karl R, Umberson Debra. Social Relationships and Health. Science. 1988;241:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L. Age Differences in Self-Assessments of Health: Age Changes, Cohort Differences, or Survivorship? Journal of Gerontology: Social Sciences. 1993;48:S289–S300. doi: 10.1093/geronj/48.6.s289. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L, Benyamini Yael. Self-Rated Health and Mortality: A Review of Twenty-seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Kaplan George A. Health and Aging in the Alameda County Study. In: Warner Schaie K, Blazer Dan, House James S, editors. Aging, Health Behaviors, and Health Outcomes. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. pp. 69–88. [Google Scholar]
- Kessler Ronald C, McLeod Jane D. Sex Differences in Vulnerability to Undesirable Life Events. American Sociological Review. 1984;49:620–31. [Google Scholar]
- Kiecolt-Glaser Janice K, Glaser Ronald. Stress and Immunity: Age Enhances the Risks. Current Directions in Psychological Science. 2001;10:18–21. [Google Scholar]
- Kiecolt-Glaser Janice K, Glaser Ronald, Cacioppo John T, MacCallum Robert C, Snydersmith Mary A, Kim Cheongtag, Malarkey William B. Marital Conflict in Older Adults: Endocrinological and Immunological Correlates. Psychosomatic Medicine. 1997;59:339–49. doi: 10.1097/00006842-199707000-00001. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser Janice K, Glaser Ronald, Cacioppo John T, Malarkey William B. Marital Stress: Immunologic, Neuroendocrine, and Autonomic Correlates. Annals of the New York Academy of Sciences. 1998;840:656–63. doi: 10.1111/j.1749-6632.1998.tb09604.x. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser Janice K, Newton Tamara, Cacioppo John T, MacCallum Robert C, Glaser Ronald, Malarkey William B. Marital Conflict and Endocrine Function: Are Men Really More Physiologically Affected than Women? Journal of Consulting and Clinical Psychology. 1996;64:324–32. doi: 10.1037//0022-006x.64.2.324. [DOI] [PubMed] [Google Scholar]
- McDonough Peggy, Berglund Pat. Histories of Poverty and Self-Rated Health Trajectories. Journal of Health and Social Behavior. 2003;44:198–214. [PubMed] [Google Scholar]
- Moen Phyllis. The Gendered Life Course. In: Binstock Robert H., editor. Handbook of Aging and the Social Sciences. San Diego, CA: Academic Press; 2001. pp. 179–96. [Google Scholar]
- Muthén Bengt O. Latent Variable Modeling of Longitudinal and Multilevel Data. In: Raftery Adrian E., editor. Sociological Methodology. Washington, DC: American Sociological Association; 1997. pp. 453–80. [Google Scholar]
- Muthén Linda K, Muthén Bengt O. Mplus User’s Guide. Los Angeles, CA: Muthén and Muthén; 1998. [Google Scholar]
- Nolen-Hoeksema Susan. Gender Differences in Depression. Current Directions in Psychological Science. 2001;10:173–76. [Google Scholar]
- Orth-Gomer Kristina, Wamala Sarah P, Horsten Myriam, Schenck-Gustafsson Karin, Schneiderman Neil, Mittleman Murray A. Marital Stress Worsens Prognosis in Women with Coronary Heart Disease. Journal of the American Medical Association. 2000;284:3008–14. doi: 10.1001/jama.284.23.3008. [DOI] [PubMed] [Google Scholar]
- Prigerson Holly G, Maciejewski Paul K, Rosenheck Robert A. The Effects of Marital Dissolution and Marital Quality on Health and Health Service Use among Women. Medical Care. 1999;37:858–73. doi: 10.1097/00005650-199909000-00003. [DOI] [PubMed] [Google Scholar]
- Robles Theodore F, Kiecolt-Glaser Janice K. The Physiology of Marriage: Pathways to Health. Physiology and Behavior. 2003;79:409–16. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Simon Robin W. The Meanings Individuals Attach to Role Identities and their Implications for Mental Health. Journal of Health and Social Behavior. 1997;38:256–74. [PubMed] [Google Scholar]
- Taylor Shelley E. Asymmetrical Effects of Positive and Negative Events: The Mobilization-Minimization Hypothesis. Psychological Bulletin. 1991;110:67–85. doi: 10.1037/0033-2909.110.1.67. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Chen Meichu D, House James S, Hopkins Kristine, Slaten Ellen. The Effect of Social Relationships on Psychological Well-Being: Are Men and Women Really So Different? American Sociological Review. 1996;61:837–57. [Google Scholar]
- Umberson Debra, Williams Kristi, Powers Daniel A, Chen Meichu D. As Good As It Gets? A Life Course Perspective on Marital Quality. Social Forces. 2005;84:493–511. doi: 10.1353/sof.2005.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite Linda J, Gallagher Maggie. The Case for Marriage: Why Married People are Happier, Healthier, and Better Off Financially. New York: Doubleday; 2000. [Google Scholar]
- White Lynn K. Determinants of Divorce: A Review of Research. Journal of Marriage and the Family. 1990;52:904–12. [Google Scholar]
- Wickrama KAS, Lorenz Frederick O, Conger Rand D, Elder Glen H., Jr Marital Quality and Physical Illness: A Latent Growth Curve Analysis. Journal of Marriage and Family. 1997;59:143–55. [Google Scholar]
- Wickrama KAS, Lorenz Frederick O, Wallace Lora E, Peiris Laknath, Conger Rand D, Elder Glen H., Jr Family Influence on Physical Health During the Middle Years: The Case of Onset of Hypertension. Journal of Marriage and Family. 2001;63:527–39. [Google Scholar]
- Williams Kristi. Has the Future of Marriage Arrived? A Contemporary Examination of Gender, Marriage, and Psychological Well-Being. Journal of Health and Social Behavior. 2003;44:470–87. [PMC free article] [PubMed] [Google Scholar]