ABSTRACT
Hypertension represents a serious problem in Romania, as there are over 3 million hypertensive people in our country. There is a high incidence of deaths caused by hypertension.
We performed an analytical prospective study that aims to determine: prevalence of arterial hypertension in a population from Cluj county, distribution on age and gender, arterial hypertension severity, association of hypertension with other cardiovascular risk factors. Our study included 2266 patients, age 14 years old up to over 90 years old, both masculine and feminine gender, known with hypertension and new-diagnosed ones. Each subject was submitted to an interview based on a questionnaire. Diagnosis of arterial hypertension was established according to ESH criteria that consider as hypertension: values over 140/90 mmHg. Out of all subjects submitted to the study 647 (29.74%) were diagnosed with arterial hypertension and, from these, 102 (15.13%) were new-diagnosed patients.
We found out a predominance of arterial hypertension at the age of 51-60 and over 60, an increased involvement of feminine sex; an association of hypertension with other major cardiovascular risk factors: obesity, diabetes, dislypidemia.
Arterial hypertension represents an important health problem in Romania due to an increased prevalence, major impact on morbidity and mortality by cardiovascular and cerebro-vascular disease. These facts accentuate the necessity of an early diagnosis, of making people aware of the severity of the disease and it’s impact on their lifestyle.
Keywords: arterial hypertension, cardiovascular risk factors
INTRODUCTION
Arterial hypertension represents an important health problem worldwide (1). There are over 3 million hypertensive people in Romania and there is a high incidence of deaths caused by hypertension (2-5). Our study aims to determine: prevalence of arterial hypertension in a population from Cluj county (supervised by a family phisician), association with other risk factors that increase the potential of cardiovascular complications in a population from the teritory of family medical units from Ambulatory Department of Cluj-Napoca City Hospital and assesment of possible complications. ❑
MATERIAL AND METHODS
We included in the study patients known with arterial hypertension, as well as new diagnosed individuals from a family physician (6). The study included a number of 2266 patients. They were selected out of all patients registered to the family phisician who came for an appointment (routine control or necessity visit). The study was performed from 2007 to 2009. Each selected subject was submitted to an interview based on a questionnaire. We measured arterial pressure, performed anthropometric measures and laboratory tests (7,8). Diagnosis of arterial hypertension was established according to ESH criteria: after three different visits at the doctor, a limit of arterial hypertension of 140/90 mmHg or, if the pacient was under antihypertensive treatment (9,10). We measured arterial hypertension according to standards, three times at each visit (in order to exclude white uniform fear). Patients with increased values of arterial hypertension at the first visit were called back at 2 weeks interval for a new estimation of arterial blood pressure. We considered an average of measured values of arterial hypertension. Laboratory tests were performed at the second visit to the physician (12). Diabetes mellitus was defined as three values of glycemia over 120 mg%.
Visceral obesity is assesed by waist circumference, that must be over 102 cm for males and over 88 cm for females (ATP NCEPIII definition) and by body mass index. Body mass index was estimated using the formula: BMI=Weight (kg)/Hight2 (m2) – normal BMI < 25, overweighted BMI =25-30, obesity BMI > 30. We considered as physical effort – to cover at least 3 kilometers of walking per day, together with other benefical activities that consume energy (playing, running, etc.).
As normal cholesterol values we considered those under 200 mg/dl, for HDL-Cholesterol over 40 mg/dl in men and over 50 mg/dl in women and for LDL-cholesterol under 130 mg/dl generaly and under 100 mg/dl for diabetes and for trygliceride under 150 mg/dl. Mixt dyslipidemia is defined by the presence in the same individual of at least 2 abnormal values of cholesterol, LDL, HDL, tryglicerides (12). Family records of cardiovascular disease were concluded after case history and adequate medical documents (13,14). As statistics method we used EpiInfo6. The study is an analytical prospective one. Criteria for inclusion in the study were: age between 14-90 years old, patients agreement to participate to study. We estimated values of arterial hypertension in general population, prevalence of arterial hypertension in the group of study, association of arterial hypertension with other risk factors. ❑
RESULTS
Out of 2266 patients considered for the study, 647 (29.74%) were diagnosed with arterial hypertension and, from these, 102 (15.13%) were new-diagnosed patients.
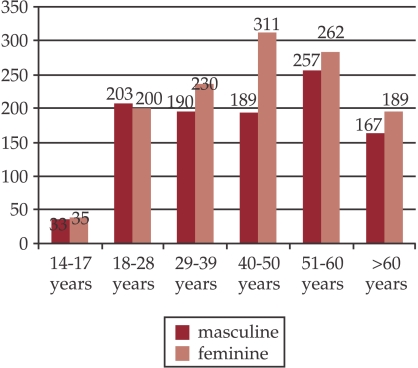
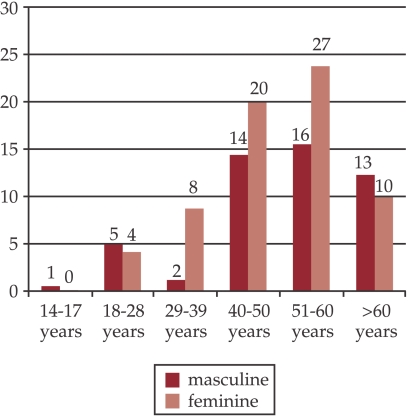
Figure 1. Total number of patients on age and sex groups.
Distribution on age groups shows a clear predominance of arterial hypertension at the age groups of: 51-60 and over 60 (15).
Distribution on gender groups shows a slightly predominance of feminine population 397 (32.35%) vs masculine 277 (26.66%).
Table 1.
Prevalence of arterial hypertension in the study group
| No | % | |
|---|---|---|
| Total no. of patients (study group) | 2266 | 100 |
| Total no. of patients with AHT | 647 | 29.74 |
| Known AHT new diagnosed cases | 545 | 84.23 |
| New diagnosed cases | 102 | 15.13 |
AHT=arterial hypertension
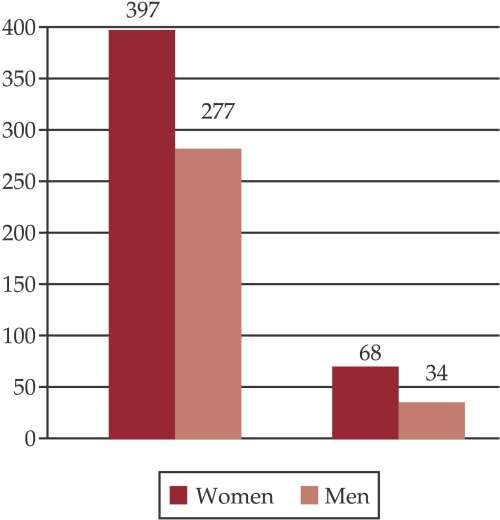
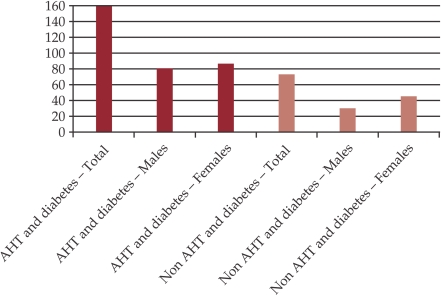
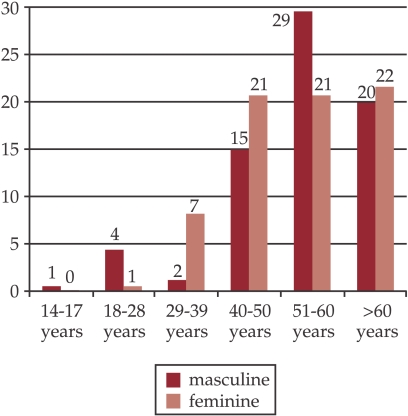
Figure 2. New diagnosed cases of hypertension distribution on gender.
New diagnosed cases of hypertension represents 102 cases (15.13%) and a predominance of female population: 68 cases (17.12%) vs male 34 cases (12.27%) (8).
We found an almost evenly distribution of patients beginning at the group of age of 18 and up to over 60 years of age. In the global group there is a predominance of feminine sex: 1227 patients (54.10%) vs 1041 masculine sex patients (45.90%) (16).
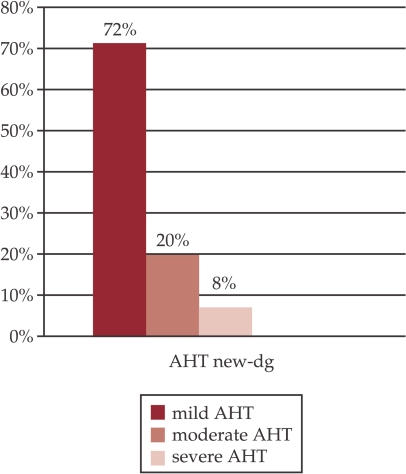
In the group of new-diagnosed patients we found out a predominance of mild form of hypertension.
Figure 3. Severity of new-diagnosed arterial hypertension.
Legend AHT=arterial hypertension
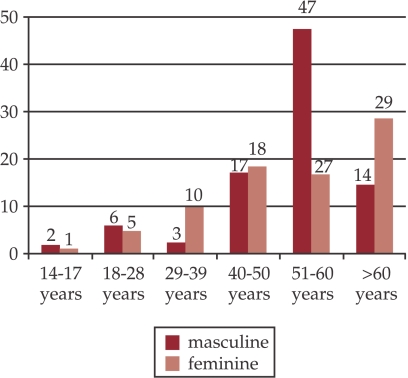
Figure 4. Family cardiovascular antecedents in first degree relatives.
Analising family cardiovascular antecedents in first degree 1 relatives we found that these were present in 179 patients, 89 males and 90 females, representing 26.55% of total number of hypertensive patients.
Studying the diabetic antecedents in grade 1 and 2 relatives in the hypertensive group we found the presence of these antecedents at 120 patients, representing 17.8% of total hypertensive patients.
Association of diabetes mellitus with hypertension in a number of 157 cases (23.29%) represents an increased risk for cardiovascular complications occurance. Distribution on sexes of diabetes is almost equal: 77 males (11.42%) and 80 females (11.87%).
Figure 5. Existence of diabetes in first and second degree relatives.
In the group of individual with normal values of arterial hypertension 67 (3.95%) individuals were diagnosed with diabetes. Out of these, 41(2.53%) were females and 36 (2.22%) were males – which indicates an equal distribution on genders (17-19).
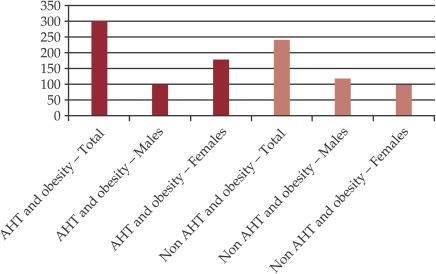
Prevalence of hypertension in subjects with visceral obesity is extremely high: 47.18%-318 overweighted people out of of 647 patients with arterial hypertension. In the obesity group there is a predominance of females:191 overweighted females, representing 60% and 127 overweighted males, representing 40%.
In the group of individuals with normal values of blood pressure, we found obesity in 255 (15.75%) cases out of 1619 subjects with normal blood pressure values – 136 (53.33%) were women and 119 (46.66%) were men, which shows a slightly higher prevalence in women vs men (20,21).
Figure 6. Association of diabetes with AHT and Non AHT individuals in the group of study.
Legend: AHT=arterial hypertension
Prevalence of arterial hypertension in subjects with obesity defined after BMI increases significantly with weight gain (22).
Figure 7. Association obesity and AHT/Non AHT in the group of study.
Legend AHT=arterial hypertension
Figure 8. Association AHT – Obesity determined by BMI.
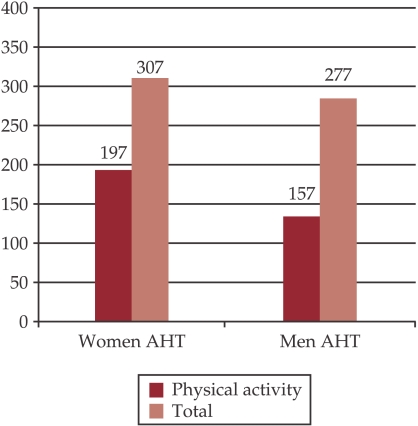
In our study we ascertained that men practise physical activities in 56.68% and women in 49.62%, indicating a slightly propensity to sedentary profile for feminine gender. Physical activity prevent cardiovascular complications occurance (23).
Figure 9. Association arterial hypertension – physical activity.
Legend: AHT=arterial hypertension
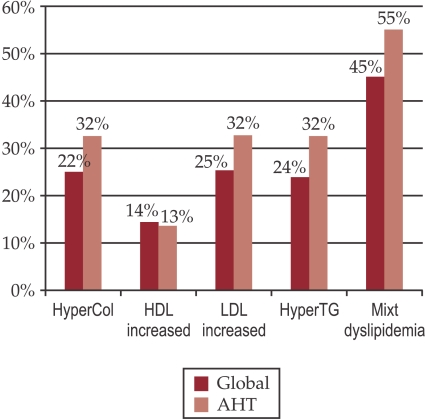
Analysing distribution on genders we found out that hypertensive women has an increased cholesterol in significantly higher percentage in comparison to hypertensive men – women 37% versus men 27%.
Figure 10. Dyslipidemia prevalence in global and hypertensive groups.
Legend: AHT=arterial hypertension
Table 2.
Association arterial hypertension – dyslipidemia
| Global | Arterial hypertension | p | Female AHT | Male AHT | p | |
|---|---|---|---|---|---|---|
| Hypercholesterolemia | 25% | 32% | 0.01 | 37% | 27% | 0.01 |
| Increased HDL | 14% | 13% | 0.01 | 16% | 9% | 0.01 |
| Increased LDL | 25% | 32% | 0.01 | 37% | 27% | 0.01 |
| Hypertrigliceridemia | 24% | 32% | 0.01 | 30% | 35% | 0.01 |
| Mixt Dyslipidemia | 45% | 55% | 0.01 | 58% | 52% | 0.01 |
| Total | 2266 | 674 | 397 | 277 |
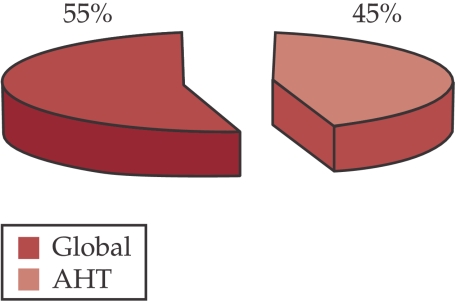
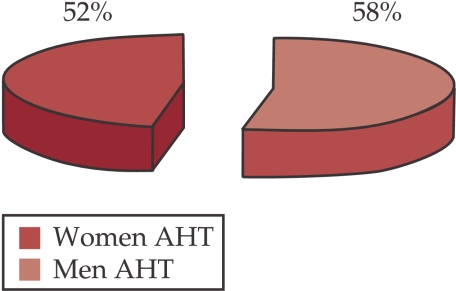
Figure 11. Mixt dyslipidemia in hypertensive group in comparison to global group.
Figure 12. Mixt dyslipidemia on gender in hypertensive group.
Legend: AHT=arterial hypertension
In normal blood pressure individuals we found 503 (31%) subjects with dyslipidemia – most cases were diagnosed with hypercholesterolemia 311 (62%); 110 (22%) with hypertrigliceridemia and 82 (16%) with increased HDL. We observed a propensity to dyslipidemia of feminine gender (24-26). ❑
DISCUSSION
Our study offers data about prevalence of arterial hypertension in a population representative for Cluj-Napoca city, as well as about cardiovascular risk factors. Considering our study methodology, data obtained is representative for Cluj county.
In our study arterial hypertension prevalence had values of 29.74%, comparable with other similar studies. Arterial hypertension has an increased prevalence in both genders, with a predominance of feminine gender (32.35% feminine versus 26.66% masculine). New-diagnosed arterial hypertension in our group of study has a significantly lower prevalence than arterial hypertension diagnosed before (15.3% versus 25.24%). This explains a better adresability of Cluj-Napoca population to health services. New-diagnosed arterial hypertension, that occurs in a significantly percentage, is a consequence of patients carelessness, stress, sedentary profile, obesity. Guides elaboration aimed to find out arterial hypertension, to educate population, to make people understand the disease and treatment in order to obtain control of the disease. We were surprised to find out that the „half rules" described by Wilber and Barrow in 1972 could be applied for our study: half of the hypertensive people are diagnosed, out of them only half are treated, and out of treated ones only half are controled. In our study 25.24% patients were known with arterial hypertension, and 15.3% were new-diagnosed. As age groups best represented was the group of 41-60 years.
Our study shows that hypertensive subjects associated other cardiovascular major risk factors: obesity, diabetes, dyslipidemia, lack of physical activity. Most of those factors had a higher prevalence in feminine sex due to alimentary habits, most women cook and they have a more sedentary profile. Association arterial hypertension – obesity, dyslipidemia, diabetes mellitus, sedentary profile increases significantly cardiovascular risk (27,28). ❑
CONCLUSION
In conclusion, arterial hypertension represents an important health problem in Romania because of an increased prevalence, by major impact on morbidity and mortality by cardiovascular and cerebral-vascular diseases; all these accentuate the necessity of an early diagnosis, of making patients aware of the treatment and of obtaining an adequate control.
References
- 1.Kearney PM, Whelton M, Reynolds K, et al. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Wilber JA, Barrow JG. Hypertension-a community problem. Am J Med. 1992;52(5):653–663. doi: 10.1016/0002-9343(72)90055-1. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evolution and Treatment of High Blood Presure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Studiul SEPHAR – Studiul de prevalenta a HTA si evaluarea riscului cardiovascular Rev Rom Cardiol 2006. 21(13) [Google Scholar]
- 5.Sur G, Duncea C. Hipertensiunea arteriala la copil si adult. Cluj-Napoca. 2002;Ed. Casa Cartii de Stiinta [Google Scholar]
- 6.Lip GYH, Fekmeden DC, Li-Saw Hee, et al. Hypertensive heart disease. Eur Heart J. 2000;21:1653–1665. doi: 10.1053/euhj.2000.2339. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell GF, Moye LSA, Braunwald E, et al. Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after miocardial infarction in patients with impaired left ventricular function. Circulation. 1997;96:4254–4260. doi: 10.1161/01.cir.96.12.4254. [DOI] [PubMed] [Google Scholar]
- 8.Verbeck WJ, Kroon AA, Kessels AG, et al. Home versus office blood pressure measurements: Reduction of unnecessary treatment study: Rationale and study design of the HOMERUS trial. Blood Pres. 2003;12:326–333. doi: 10.1080/08037050310022405. [DOI] [PubMed] [Google Scholar]
- 9.European Society of Hypertension – European Society of Cardiology guidelines for the management of arterial hypertension J Hypertension 2003. 21 1011 1053 [DOI] [PubMed] [Google Scholar]
- 10.Guidelines for the Management of Arterial Hypertension – The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J 2007. 0:ehm236v 1 75 [DOI] [PubMed] [Google Scholar]
- 11.Kaplan N. New Issues in the Treatment of Isolated Systolic Hypertension. Circulation. 2000;102:1079–1081. doi: 10.1161/01.cir.102.10.1079. [DOI] [PubMed] [Google Scholar]
- 12.Harrison’s Principles of Internal Medicine The McGraw-Hill Companies Inc. 2008. Seventeenth Edition [Google Scholar]
- 13.Topol, Eric J. Textbook of Cardiovascular Medicine. Lippincott Williams & Wilkins. 2007;3rd Edition [Google Scholar]
- 14.Braunwald E. W.B. Saunders Co. 9th edition Philadelphia: 2001. Heart disease. [Google Scholar]
- 15.Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 16.Andersson OK, Almgren T, Persson B, et al. Survivalo in treated hypertension: follow-up study after two decades. BMJ. 1999;13:392–400. doi: 10.1136/bmj.317.7152.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37(4):1053–1059. doi: 10.1161/01.hyp.37.4.1053. [DOI] [PubMed] [Google Scholar]
- 18.El-Atat F, McFarlane SI, Sowers JR, et al. Diabetes, hypertension, and cardiovascular derangements: pathophysiology and management. Curr Hypertens Rep. 2004;6(3):215–223. doi: 10.1007/s11906-004-0072-y. [DOI] [PubMed] [Google Scholar]
- 19.Naidoo DP. The link between microalbuminuria, endothelial dysfunction and cardiovascular disease in diabetes. Cardiovasc J South Afr. 2002;13:190–199. [PubMed] [Google Scholar]
- 20.Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 1990;322:882–889. doi: 10.1056/NEJM199003293221303. [DOI] [PubMed] [Google Scholar]
- 21.Grassi G, Seravalle G, Dell’Oro R, et al. Adrenergic and reflex abnormalities in obesity-related hypertension. Hypertension. 2000;36:538–542. doi: 10.1161/01.hyp.36.4.538. [DOI] [PubMed] [Google Scholar]
- 22.Calle EE, Thun MJ, O’Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 23.Johnson ML, Pietz K, Battleman DS, et al. Prevalence of Comorbid Hypertension and Dyslipidemia and Associated Cardiovascular Disease. Am J Manag Care. 2004;10:926–932. [PubMed] [Google Scholar]
- 24.Borghi C, et al. Interactions between hypercholesterolemia and hypertension: implications for therapy. Curr Opin Nephrol Hypertens. 2002;11:489–496. doi: 10.1097/00041552-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Selby JV, Peng T, Karter AJ, et al. Surgical treatment of brain metastases. Clinical and computerized tomography evaluation of the results of treatment. Cancer. 1985;55:1382–1388. doi: 10.1002/1097-0142(19850315)55:6<1382::aid-cncr2820550637>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 26.Wong ND, Pio JR, Franklin SS, et al. Preventing coronary events by optimal control of blood pressure and lipids in patients with the metabolic syndrome. Am J Cardiol. 2003;91:1421–1426. doi: 10.1016/s0002-9149(03)00392-8. [DOI] [PubMed] [Google Scholar]
- 27.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2269. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 28.Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904. doi: 10.1001/jama.290.7.898. [DOI] [PubMed] [Google Scholar]