Abstract
The primary aim of this study was to test the association of early (first 6 months) adherence related to diet, self-monitoring, and attendance with changes in adiposity and cardiovascular risk factors. This study used data from the 24-month POUNDS LOST trial that tested the efficacy of four dietary macronutrient compositions for short-and long-term weight loss. A computer tracking system was used to record data on eight indicator variables related to adherence. Using canonical correlations at the 6 and 24 month measurement periods, early behavioral adherence was associated with changes in percent weight loss and waist circumference at 6 months (R = 0.52) and 24 months (R = 0.37), but was not associated with cardiovascular disease risk factor levels. Early dietary adherence was associated with changes in insulin at 6 months (R = 0.19), but not at 24 months (R = 0.08, ns). Early dietary adherence was not associated with changes in adiposity.
Keywords: Obesity, Weight management, Adherence, Computer tracking, Waist circumference, Insulin
There is consensus that adherence to weight management strategies is critical for successful initial weight loss and for long-term weight maintenance (Fappa et al. 2008). Research on the relationship between adherence and successful weight management has been hampered by two issues: (1) definition of adherence and (2) the complexity of investigating weight and health outcomes associated with a variety of behavioral prescriptions that define lifestyle behavior modification, e.g., dietary recommendations, physical activity goals, self-monitoring activities, and recommendations to attend counseling sessions (Williamson et al. 2010). In previous research, a common practice for defining adherence has been to select one (or a few) indicators of adherence, e.g., attendance to counseling sessions (Sacks et al. 2009) or an index related to following a dietary prescription (Alhassan et al. 2008; Warziski et al. 2008). This approach for defining adherence assumes that there is a single behavioral dimension that validly defines adherence and therefore, any valid indicator of adherence serves as a proxy for all indicators of adherence.
The complexity of lifestyle behavior change weight management programs has been well documented (Wadden et al. 2006; Williamson et al. 2007). Typically, the lifestyle program is described as a “package” with many procedural features, e.g., reduction of caloric intake, increased physical activity, self-monitoring, individual and/or group counseling sessions, and problem-solving (Williamson et al. 2005). The relative importance of adhering to one set of behavioral prescriptions versus another set of prescriptions for the prediction of long-term weight loss has been the focus of relatively few studies (e.g., Warziski et al. 2008). There is considerable evidence, however, that there is variability in adherence across individuals and across different behavioral aspects of adherence to medical and behavioral prescriptions (Levensky and O’Donahue 2006). The determinants of this variability have been debated, with hypotheses ranging from individual differences (e.g., Prochaska et al. 2006) to environmental determinants (e.g., Heiby and Lukens 2006) as potential causes of variability in adherence to the same weight management program. In the field of weight management, the consequences of poor adherence are well established with most experts in agreement that less than optimal adherence leads to less weight loss and poor weight loss maintenance (Fappa et al. 2008).
Recently, Williamson and colleagues (2010) provided a potential solution to the definition of adherence based upon multiple behavioral indicator variables. Williamson et al. studied co-variation among different indicators of early (first 6 months) adherence in a randomized controlled trial called the Prevention of Obesity Using Novel Dietary Strategies (POUNDS LOST) study. In this study, factor analysis was used to investigate whether indicators co-varied such that a single dimension was evident or whether the pattern of co-variation among indicators suggested the presence of more than one dimension of adherence. The study identified two dimensions (factors) that accounted for 66% of the variance of eight indicators of early adherence. The two dimensions/factors were called: (1) behavioral adherence—attendance to individual and group counseling sessions and self-monitoring of dietary intake and physical activity, and (2) dietary adherence—deviation from dietary prescriptions for total caloric intake and three macro-nutrients (fat, protein, and carbohydrates).1
This study was designed to extend to findings of the earlier study (Williamson et al. 2010) by investigating the relationship between the two dimensions of early adherence and changes in indicators of adiposity (i.e., body weight and waist circumference) and cardiovascular disease risk factors (i.e., blood lipids, blood pressure, insulin levels, and glucose levels). All outcomes measures were collected at baseline and Months 6 and 24 during the two-year trial. The primary aim of this study was to investigate the predictive relationship between early adherence to the POUNDS LOST interventions and changes in measures of adiposity and cardiovascular disease risk factors at Months 6 and 24. We hypothesized that higher levels of behavioral and dietary adherence would predict healthy changes in adiposity and improved markers of cardiovascular disease risk at both measurement points.
Method
Participants
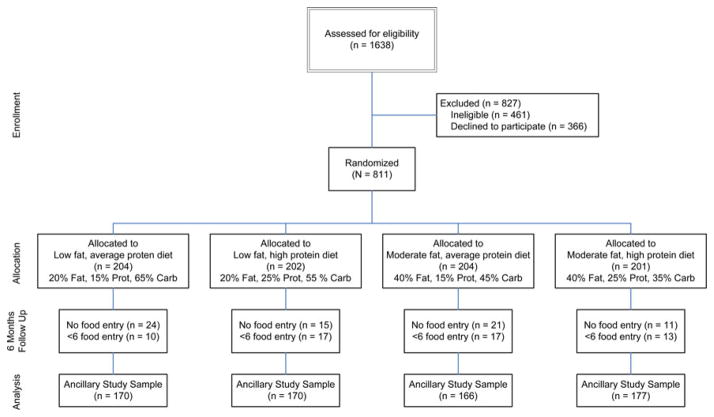
The POUNDS LOST trial (Sacks et al. 2009) was conducted at two clinical research sites: Boston, MA and Baton Rouge, LA. The study plan (determined by statistical power analysis) called for recruiting 400 participants at each site for a total of 800 volunteers. The inclusion and exclusion criteria for the POUNDS LOST study have been described in detail in other papers (Sacks et al. 2009; Williamson et al. 2010). Briefly, participants were men and women aged 30–70 years who were overweight or obese (body mass index ranged from 25 to 40) who were otherwise healthy and able to participate in a two-year clinical trial. For the present study, participants were included if they had recorded at least six dietary records in the computer tracking system (n = 683) as summarized in Fig. 1. Characteristics of these 683 participants at baseline are summarized in Table 1.
Fig. 1.
CONSORT flow chart that describes the recruitment of participants and development of the study sample for this ancillary study from the parent project called POUNDS LOST. The term “ancillary study sample” refers to the participants (N = 683) who met the criteria for inclusion in the ancillary study, i.e., had entered at least six food entry records
Table 1.
Characteristics of the sample at baseline
| Low fat, average protein | Low fat, high protein | Moderate fat, average protein | Moderate fat, high protein | Total sample | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of participants | 170 | 170 | 166 | 177 | 683 | |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| Age | 52 (9) | 50 (10) | 52 (9) | 51 (9) | 51 (9) | |||||
| n | % | n | % | n | % | n | % | n | % | |
| Gender | ||||||||||
| Female | 103 | 61 | 110 | 65 | 103 | 62 | 111 | 63 | 427 | 63 |
| Male | 67 | 39 | 60 | 35 | 63 | 38 | 66 | 37 | 256 | 37 |
| Race | ||||||||||
| White | 138 | 81 | 137 | 81 | 134 | 81 | 147 | 83 | 556 | 81 |
| Black/African American | 23 | 14 | 23 | 14 | 23 | 14 | 23 | 13 | 92 | 13 |
| Asian | 9 | 0 | 1 | 1 | 0 | 0 | 2 | 1 | 3 | 1 |
| Hispanic | 6 | 4 | 6 | 4 | 7 | 4 | 4 | 2 | 23 | 3 |
| Other | 3 | 2 | 3 | 2 | 2 | 1 | 1 | 1 | 9 | 1 |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| Body mass index (kg/m2) | 33 (4) | 33 (4) | 32 (4) | 33 (4) | 33 (4) | |||||
| n | % | n | % | n | % | n | % | n | % | |
| Body mass index (kg/m2) | ||||||||||
| Categories | ||||||||||
| 25–29.9 | 40 | 24 | 47 | 27 | 47 | 28 | 53 | 30 | 187 | 27 |
| ≥30 | 130 | 76 | 123 | 73 | 119 | 72 | 124 | 70 | 496 | 73 |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | ||||||
| Education | ||||||||||
| ≤ High school | 21 | 12 | 12 | 7 | 14 | 8 | 16 | 9 | 63 | 9 |
| Some college | 40 | 24 | 36 | 21 | 33 | 20 | 34 | 19 | 143 | 21 |
| ≥ College grad | 109 | 64 | 122 | 72 | 119 | 72 | 127 | 72 | 477 | 70 |
| Marital status | ||||||||||
| Married | 132 | 65 | 146 | 72 | 144 | 71 | 143 | 71 | 565 | 70 |
| Divorced/Separated | 36 | 18 | 24 | 12 | 33 | 16 | 29 | 14 | 122 | 15 |
| Widowed | 8 | 4 | 4 | 2 | 4 | 2 | 2 | 1 | 18 | 2 |
| Never married | 28 | 14 | 28 | 14 | 23 | 11 | 27 | 13 | 106 | 13 |
| Household income | ||||||||||
| < 50 K | 43 | 25 | 34 | 20 | 36 | 22 | 40 | 26 | 153 | 22 |
| 50–100 K | 70 | 41 | 69 | 41 | 63 | 38 | 71 | 40 | 273 | 40 |
| 100–150 K | 39 | 23 | 38 | 22 | 36 | 22 | 29 | 16 | 142 | 21 |
| > 150 K | 17 | 10 | 28 | 16 | 29 | 17 | 34 | 19 | 108 | 16 |
| Refused | 1 | 1 | 1 | 1 | 2 | 1 | 3 | 2 | 7 | 1 |
The baseline characteristics of this table represent the “ancillary study sample” that is represented in Fig. 1. SD Standard deviation, K $1000
Study design
The POUNDS LOST trial was designed to test the efficacy of four macronutrient diets for weight and fat reduction and improvement of health parameters during a two-year randomized controlled trial. The dietary goals for each of the four dietary interventions: (1) Low Fat (20% of energy), Average Protein (15% of energy); (2) Moderate Fat (40%), Average Protein (15%); (3) Low Fat (20%), High Protein (25%); (4) Moderate Fat (40%), High Protein (25%). All four dietary approaches were low in saturated fat and reduced in total energy intake based on the individual’s dietary prescription. A behavioral program of similar programmatic content and intensity across the four dietary interventions was also included. Participants were randomly assigned to the four treatment arms (macronutrient diets), stratified by gender. Randomization by computer occurred after the collection of baseline data and was managed by the study statistician. The timeframe for the study was October 2004 to December 2007. The primary results of the study have been reported (Sacks et al. 2009). The study found that changes in weight, waist circumference, and cardiovascular disease risk factors did not differ as a function of macro-nutrient diet assignment with only two exceptions (greater improvement of high-density lipoprotein and low-density lipoprotein cholesterol in treatment arms associated with prescriptions of low fat diets). The POUNDS LOST study found that all four diets resulted in improved health over a two-year period of intervention. One unique feature of the study was that a computer tracking system was developed to track behavioral indicators of adherence, as reported by counselors and participants, during the two-year randomized controlled trial. This feature of the study allowed for a rigorous test of co-variation among eight indicators of adherence in four different diet programs.
Assessment of adherence using a computer tracking system
A computer tracking system was developed specifically for use in this study and was described in detail in an earlier paper (Williamson et al. 2010). One of the functions of the computer tracking system was to track behavioral indicators related to adherence to the four dietary interventions: attendance at group and individual counseling sessions, for self-monitoring of behaviors and providing feedback to participants and researchers. Dietitians and other study staff members entered data into the computer tracking system via a web-based application each time contact was made with a participant (individual or group sessions, or via telephone, email, or mail). The counselor also entered data consisting of body weight (measured at an intervention session), attendance, and intervention make-up sessions. The counselors based their reports upon direct observation of attendance and self-report records. Participants also used the computer tracking system to enter their self-reported food intake from diet records. The computer tracking system automatically calculated kilocalories from fat, protein, carbohydrate, as well as total kilocalories using nutrient data from the most current US Department of Agriculture database. Participants also entered data related to number of minutes of physical activity per day and number of days of physical activity per week. The formula used to calculate percent deviation from macronutrient and calorie goals was: [(Actual value − Prescribed value)/Prescribed value] × 100. Deviation scores for fat, carbohydrate, and protein were calculated using percent of calories based upon self-reported information obtained via the computer tracking system. This procedure was designed to evaluate adherence to each diet intervention for each participant based upon his or her unique caloric and macronutrient goals. It should be noted, that since adherence to dietary goals was based upon deviations from prescribed values (not percentages) the macronutrient and caloric deviation scores were mathematically independent.
Dietary treatment interventions
Prior to introduction of dietary interventions, estimated energy needs were calculated using indirect calorimetry to determine resting energy expenditure. Estimated total energy was calculated by multiplying resting energy expenditure by an activity factor (Baecke et al. 1982). For the weight loss phase of the study, the participant’s diet prescription represented an approximate 750 kcal/day deficit from his/her estimated energy intake. The 750 kcal deficit was then rounded to the nearest 200 to provide dietary prescriptions ranging from 1,200 to 3,200 kcal.
After a cohort of ~48–80 participants was recruited, the four interventions were initiated by randomly assigning participants to one of the four diet interventions. During the intense weight loss phase (Weeks 1–26), participants were offered group sessions 3 out of 4 weeks, whereas during the weight maintenance phase (Weeks 27–104), participants were offered group sessions 2 out of 4 weeks. During the entire two-year program, participants scheduled individual one-on-one visits with a dietitian every 8 weeks. The group sessions, lasting 1 h, provided nutrition education, included behavioral methods to reinforce dietary and behavioral goals, and also provided social support.
Following randomization to one of the four dietary interventions, each participant met one-on-one with a registered dietitian, who instructed the participant on following a specific macronutrient diet prescription. To aid participants in achieving the goals of their assigned dietary regimen, 14 days of individualized menus were developed for each of the four diet treatment arms. At the first group counseling session, the participants received a shopping list, which was designed for their assigned diet to support efforts in purchasing appropriate foods. Each participant was counseled to use the computer tracking system to track food and drink consumed each week, as well as minutes of physical activity. Body weight was measured at each intervention visit.
Data collection
Computer tracking system
Data related to adherence were recorded on the computer tracking system by either counselors or participants over the course of the study. For the purposes of this study, eight behavioral indicators of adherence to the prescribed interventions were measured: (1) attendance to individual sessions, (2) attendance to group sessions, (3) frequency of submitting dietary self-monitoring records, (4) frequency of submitting physical activity records, (5) deviation from total daily kilocalorie goal, (6) deviation from daily protein goal, (7) deviation from daily fat goal, and 8) deviation from daily carbohydrate goal. Each of these variables was summarized over the first 6 months2 of this two-year study in terms of an average using absolute values (e.g., mean discrepancy from a dietary prescription), or a percentage (e.g., percent of groups attended or percent of self-monitoring records submitted).
Measures of body weight, waist circumference, percent body fat and cardiovascular disease risk factors.3
The primary outcome variable of the study was change in body weight from baseline to 24 months. Measurements of body weight were also obtained at 6, 12, and 18 months. Waist circumference was measured at baseline, 6, 12, 18, and 24 months. Measurements of body fat were obtained at baseline, 6 and 24 months, and were collected in a 50% random sample using dual x-ray absorptiometry. Cardiovascular disease risk factors (i.e., total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides, glucose levels, and insulin levels) were measured at baseline, 6 and 24 months. Blood pressure was measured at baseline, 6, 18, and 24 months.
Statistical methods
As reported by Williamson and colleagues (2010), of the 811 participants enrolled in the study, 683 participants had six or more food intake entries across the initial 6 months and were included as participants. The current study also analyzed only data from these 683 participants. There were similar numbers of participants in each of the four treatment arms (range = 166–177 participants per arm) that met this criterion (see Fig. 1).
Williamson et al. used exploratory and confirmatory factor analyses to investigate co-variation among the eight indicators of adherence. They reported that the factor structure was very similar across the four treatment arms, with two factors emerging for each treatment with identical indicators for each diet type. The two factors that were identified by principal components analysis and found to be stable using confirmatory factor analysis were named: (1) behavioral adherence (defined by attendance to individual sessions, attendance to group sessions, frequency of submitting dietary self-monitoring records, and frequency of submitting physical activity records) and (2) dietary adherence (defined by deviation from total daily kilocalorie goal, deviation from daily protein goal, deviation from daily fat goal, and deviation from daily carbohydrate goal).
The two measures of adherence were defined by summing the scores for each factor using a factor loading of 1.0 for each indicator (percentages for indicators of behavioral adherence and deviation scores for dietary adherence). It should be noted that both factors can be conceptualized as types of “behavioral adherence” in weight management programs and that we selected the terms “behavioral and dietary adherence” to represent the content of the two factors identified by Williamson et al. (2010).
The primary aim of this study was to test the predictive relationship between the two dimensions/factors of adherence identified in the earlier study (behavioral and dietary adherence) with changes in body weight, waist circumference, and cardiovascular disease risk factors (i.e., blood pressure, cholesterol, triglycerides, glucose, and insulin). Measurement periods were baseline, 6 and 24 months for all health outcome measures. Additional measurements for body weight, waist circumference, and blood pressure were collected at Month 12 and body weight and waist circumference were also measured at Month 18. To test for associations at each 6 months interval, Pearson Product Moment Correlations were used for all correlations between early adherence factors and changes (from baseline) in health outcomes at each relevant measurement point. Measures of adiposity and cardiovascular disease risk factors were found to be significantly inter-correlated. To control for these inter-correlations and to reduce the total number of correlations that were calculated, canonical correlations between the two adherence measures and changes in measures of adiposity and cardiovascular disease risk factors at 6 and 24 month measurement points were calculated. The results from these canonical correlations were used to test the primary aims of this study since this multivariate approach controls for inter-correlations among outcome variables and includes data from all available participants at two important measurement points (i.e., 6 and 24 months). This statistical approach required the calculation of only two correlations to test the primary aims of the study. All statistical analyses were performed using SAS 9.1.
Results
Changes in body weight, waist circumference, body fat, and health outcomes
Table 2 summarizes average baseline levels and changes from baseline in body weight, body fat, waist circumference, and cardiovascular disease risk factors at Months 6, 12, 18, and 24.4 Note that some measures were not collected at Months 12 and 18, and percent body fat was only measured in a subsample. Weight, waist, and blood pressure were lowest at Month 12, with some recidivism by Month 24.
Table 2.
Means and standard deviations of outcome variables related to adiposity and health at baseline and follow-up visits
| Baseline | Change from baseline at M6 | Change from baseline at M12 | Change from baseline at M18 | Change from baseline at M24 | |
|---|---|---|---|---|---|
| Weight (kg) | 93.0(15.4) | −7.7(5.7) | −7.8(7.4) | −6.4(7.7) | −4.9(7.7) |
| Waist circumference (cm) | 103.6(13.1) | −7.5(6.1) | −8.1(7.7) | −7.5(7.9) | −6.3(7.9) |
| Body fat* | 37.3(6.8) | −3.0(2.8) | −2.3(3.4) | ||
| Systolic BP (mmHg) | 119.5(13.5) | −2.7(9.9) | −3.6(10.9) | −1.9(11.0) | |
| Diastolic BP (mmHg) | 75.4(9.4) | −2.2(7.2) | −2.2(7.5) | −1.2(7.8) | |
| Glucose (mg/dL) | 92.2(14.0) | −2.5(9.0) | 1.9(8.8) | ||
| Insulin (lU/mL) | 12.1(7.6) | −2.8(6.7) | −1.4(6.6) | ||
| LDL cholesterol (mg/dL) | 124.8(31.6) | −6.1(24.7) | −4.6(27.4) | ||
| HDL cholesterol (mg/dL) | 49.1(14.4) | 1.4(7.1) | 4.9(7.6) | ||
| Triglycerides (mg/dL) | 143.6(86.2) | −32.4(61.7) | −29.0(67.3) |
The sample size N is 652–657 at baseline, 593–633 at Month 6, 578–582 at Month 12, 515–525 at Month 18, and 502–567 at Month 24
Body fat was measured in the subsample group with sample size of 358/309/223 for baseline/Month 6/Month 24. BP Blood Pressure, LDL low-density lipoprotein, HDL high-density lipoprotein
Correlations between adherence factors and health outcomes
Table 3 summarizes the correlations between the behavioral and dietary adherence with changes in health outcomes at each relevant measurement point. These analyses indicated that behavioral adherence was consistently negatively correlated with changes in body weight, waist circumference, and percent body fat at each relevant measurement point. These correlations indicate that greater behavioral adherence (attendance and self-monitoring) during the first 6 months of the two-year study predicted reductions of body weight, waist circumference, and body fat at every relevant measurement period throughout the POUNDS LOST trial. The magnitude of these significant negative correlations ranged from −0.28 to −0.52. Behavioral adherence was also significantly negatively correlated with cardiovascular disease risk factors, but there was less consistency across risk factors and correlations were generally smaller in magnitude (ranging from −0.11 to −0.27).
Table 3.
Correlations of behavioral and dietary adherence with measures of adiposity and health outcomes
| ΔWT% | ΔWC | Δ% FAT* | ΔSBP | ΔDBP | ΔGLU | ΔINS | ΔLDL | ΔHDL | ΔTRIG | |
|---|---|---|---|---|---|---|---|---|---|---|
| Behavioural | ||||||||||
| M6 | −0.52** | −0.41** | −0.45** | −0.22** | −0.27** | −0.07 | −0.18** | −0.10* | −0.00 | −0.16** |
| M12 | −0.47** | −0.39** | −0.11* | −0.20** | ||||||
| M18 | −0.39** | −0.35** | ||||||||
| M24 | −0.35** | −0.28** | −0.41** | −0.13* | −0.20** | −0.06 | −0.18** | −0.04 | 0.20** | −0.13* |
| Dietary | ||||||||||
| M6 | 0.24** | 0.16** | 0.24** | 0.11* | 0.14** | 0.06 | 0.21** | 0.01 | −0.03 | 0.15** |
| M12 | 0.21** | 0.14** | 0.07 | 0.11 | ||||||
| M18 | 0.19** | 0.13* | ||||||||
| M24 | 0.11* | 0.04 | 0.19* | 0.05 | 0.08 | 0.01 | 0.03 | −0.01 | −0.04 | 0.07 |
Bold type indicates a significant correlation (P < 0.01).
Significant at .01 level;
significant at .001 level
Also, note that higher scores for behavioral adherence indicate greater adherence and for dietary adherence, lower scores indicate greater adherence. Δ Change, WT% percent weight, WC waist circumference, SBP systolic blood pressure, DBP diastolic blood pressure, GLU glucose, INS insulin, LDL low-density lipoprotein cholesterol, HDL high-density lipoprotein cholesterol, TRIG triglycerides
As can be seen in Table 3, correlations between dietary adherence and changes in body weight, waist circumference, and body fat were also significant for most statistical tests, but were smaller in magnitude in comparison to similar correlations involving behavioral adherence (correlations ranged from 0.04 to 0.24). Correlations between dietary adherence and changes in cardiovascular disease risk factors were also smaller and less consistently significant (correlations ranged from −0.04 to 0.15).
Canonical correlations between adherence factors and health outcomes
There was considerable co-variation among the health outcome variables, with correlations at each measurement point ranging from 0.00 to 0.82 at Month 6 and 0.00 to 0.88 at Month 24. We computed canonical correlations to statistically control for co-variation among adherence variables and health outcome variables5 at Months 6 and 24 and to reduce the total number of correlations. Table 4 summarizes the findings at Month 6. Two significant canonical correlations were found between early (first 6 months) adherence and health outcomes after this time period, i.e., Month 6. The first canonical correlation (R = 0.52) was between behavioral adherence and changes in body weight and waist circumference. The second significant canonical correlation (R = 0.20) was between early dietary adherence and changes in insulin levels at Month 6.
Table 4.
Canonical correlations (6 months)
| Canonical correlation 1 | Canonical correlation 2 | |
|---|---|---|
| Canonical correlation | 0.52* | 0.20* |
| Adherence factors | ||
| Dietary adherence | 0.47 | 0.88 |
| Behavioral adherence | −0.99 | 0.08 |
| Changes in adiposity and health outcomes | ||
| Percent weight loss | 0.97 | −0.10 |
| Waist circumference | 0.75 | −0.32 |
| Glucose | 0.13 | 0.14 |
| Insulin | 0.37 | 0.69 |
| HDL cholesterol | 0.01 | −0.15 |
| LDL cholesterol | 0.20 | −0.29 |
| Triglycerides | 0.33 | 0.43 |
| Systolic blood pressure | 0.43 | −0.06 |
| Diastolic blood pressure | 0.55 | −0.02 |
P < 0.05; correlations of variables with canonical functions > 0.60 are shown by bold print. HDL high-density lipoprotein, LDL low-density lipoprotein
Table 5 summarizes the results of the canonical correlation analysis at Month 24. Only one significant correlation was found (R = 0.37). This correlation was between early behavioral adherence and changes in body weight and waist circumference at Month 24. The correlation between dietary adherence and health outcomes was not statistically significant (R = 0.08).
Table 5.
Canonical correlations (24 months)
| Canonical correlation 1 | Canonical correlation 2 | |
|---|---|---|
| Canonicalcorrelation | 0.37* | 0.08 |
| Adherence factors | ||
| Dietary adherence | 0.34 | 0.94 |
| Behavioral adherence | −0.99 | −0.05 |
| Changes in adiposity and health outcomes | ||
| Percent weight loss | 0.93 | −0.01 |
| Waist circumference | 0.79 | −0.31 |
| Glucose | 0.16 | −0.01 |
| Insulin | 0.48 | −0.43 |
| HDL cholesterol | −0.54 | 0.01 |
| LDL cholesterol | 0.08 | −0.27 |
| Triglycerides | 0.36 | 0.36 |
| Systolic blood pressure | 0.30 | 0.17 |
| Diastolic blood pressure | 0.51 | 0.20 |
P < 0.05; correlations of variables with canonical functions > 0.60 are shown in bold print. HDL high-density lipoprotein, LDL low-density lipoprotein
Discussion
Adherence to lifestyle interventions is generally viewed as central to their efficacy for weight management (Fappa et al. 2008). Because lifestyle interventions involve multiple behaviors as targets for change, it is unclear which aspects of adherence are most important for long-term weight loss and weight loss maintenance. The primary aim of this study was to test the association between early (first 6 months) adherence to the interventions tested in the two-year study and weight and health outcomes measured at 6 and 24 months. A previous study (Williamson, et al., 2010) identified two factors of adherence associated with the POUNDS LOST study and they were named behavioral and dietary adherence. In this follow-up study, we tested the predictive validity of these two dimensions of adherence for weight loss and improvement of health outcomes at 6 month intervals across the two-year study. Correlations between behavioral adherence and changes in body weight, waist circumference, and body fat percent were statistically significant at each measurement point. Correlations between dietary change and changes in body weight, etc. were much weaker. Canonical correlation analyses confirmed these associations between behavioral adherence and changes in body weight and waist circumference at Months 6 and 24. Canonical correlation analysis also found that dietary adherence was uniquely correlated with reductions in insulin levels at Month 6, but not Month 24.
Based upon these findings, we concluded that early adherence (in this case, the first 6 months) to structured interventions that target improved nutrition, increased physical activity, and weight loss are important for achieving both short and long-term weight management. This observation begs the question: Why is early adherence a strong predictor of later weight loss outcomes? Although the findings of this study do not offer a definitive answer to this question, our findings support the view of many behavioral experts who believe that following the guidelines of a weight management program during the initial period of treatment has a variety of long-term effects that ultimately result in a favorable weight loss outcome (Fappa et al. 2008; The Look AHEAD Research Group 2006; Wing 1998). However, few research studies have directly addressed this question. Some of the possible consequences of early adherence have been discussed and some of the more plausible explanations include: (1) early adherence strengthens healthy lifestyle habits that are later maintained by changes in the physical and social environment (Wing 1998), (2) early adherence improves self-efficacy that ultimately yields better long-term weight management (Warziski et al. 2008), and/or (3) executive function resources are strengthened by adhering to the program, thereby resulting in long-term weight management self-regulatory skills that were previously weaker (Hall et al. 2008). An alternative hypothesis is that pre-existing psychological factors, e.g., conscientiousness, favor the establishment of early adherence in individuals that are predisposed to engage in healthy behavior (Bogg and Roberts 2004). Further research on these potential mediating factors between early adherence and weight management will be required to investigate these hypotheses.
Another intriguing aspect of the study concerns the finding that a set (i.e., not just one behavior) of behavioral indicators of adherence predicted short and long-term weight loss. This finding raises the question of whether one behavioral indicator might be more important than others in predicting long-term weight loss. An answer to this question comes from the factor analytic findings of Williamson et al. (2010). This study reported the identification of the behavioral adherence dimension using both exploratory and confirmatory factor analysis. Internal consistency for the four indicators of behavioral adherence (i.e., attendance to individual sessions, attendance to group sessions, frequency of submitting dietary self-monitoring records, and frequency of submitting physical activity records) was high (Cronbach’s alpha = 0.77), with relatively similar factor loadings for the four indicators (i.e., 0.57, 0.78, 0.82, 0.82). As noted by Williamson et al. (2010), the factor analytic results suggest that co-variation among these four indicators was remarkably high. This finding of strong co-variation suggests that if an individual is likely to attend counseling sessions, the person is also likely to regularly engage in self-monitoring of his/her dietary and physical activity behaviors. From a clinical perspective, the finding of strong co-variation among these behaviors suggests that a program that promotes and reinforces any one of the behaviors will yield improvement in the other behaviors. This intriguing possibility warrants further investigation.
In summary, early behavioral adherence was found to be consistently associated with short-term and long-term weight management. This finding suggests that regular attendance to counseling sessions and self-monitoring of diet and exercise during the first 6 months of intervention significantly predicted changes in body composition in a two-year clinical trial. These results suggest that promotion of optimal adherence to behavioral components of the intervention may be very important for both immediate and long-term changes in body weight and other indicators of adiposity, e.g., waist circumference and percent body fat.
Limitations of the study include: (1) the study focused exclusively upon adherence to a weight management program with four different types of macronutrient diets, (2) a limited number (eight) of indicators of adherence were selected for study, (3) the self-reported caloric intakes may have been underestimated, (4) the study sample was highly selected and recruited at two clinical research sites and cannot be regarded as a representative sample of adults or even overweight/obese adults in the US e.g., the study sample had a majority of women and Caucasian participants, (5) physical activity was not adequately studied due to the design of the parent study that intentionally deemphasized changes in physical activity and emphasized adherence to the four macronutrient diets that provided very specific dietary prescriptions, and (6) the four dietary interventions of this study were, by definition, designed to enhance adherence to all aspects of the intervention. It is, therefore, unknown whether the same factor structure would have emerged in a less structured medical, dietary, or behavioral regimen, e.g., only providing brief counseling to change diet and exercise. These findings require replication in other health behavior change trials and clinical settings that focus on other health concerns and employ different interventions and study different indicators of adherence. Based upon these preliminary results from the POUNDS LOST study, we conclude that early behavioral adherence was predictive of short-term and long-term changes in indicators of adiposity (i.e., body weight and waist circumference). We encourage investigators to test this predictive relationship in new studies that require adherence to a variety of medical procedures and include other behavioral prescriptions, e.g., explicit instructions to increase physical activity and/or improve physical fitness.
Acknowledgments
Supported by a cooperative agreement award HL073286 from National Heart, Lung, and Blood Institute, National Institutes of Health; and NIH General Clinical Research Center grant RR-02635.
Ethical standards This study was approved by the appropriate ethics committees and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study.
Footnotes
It should be noted that the study did not emphasize changes in physical activity and it did not involve the use of medications or other medical approaches. Williamson and colleagues (2010) hypothesized that if the study had included these other tools or strategies, they would have identified dimensions of adherence related to these other behavioral features of weight management programs.
As reported by Williamson et al. (2010), computer tracking data from the first 6 months (but not from Months 7 to 24) were analyzed for two reasons: (1) the functionality of the computer tracking system was changed mid-way through the study (after all participants had at least 6 months in the study) and (2) utilization of the computer tracking system diminished over the course of the 24 month study, such that information from the computer tracking system during Months 7–24, is likely from a non-representative sample.
Comprehensive descriptions of the methods used to measure these outcome variables are provided in the paper authored by Sacks et al. (2009). The experimental design of the study called for measurement of percent body fat in a randomly selected sample (50% of the total sample, stratified by site and gender) due to budget constraints and guidance by tests of statistical power. Change scores were selected as the variables to be predicted by early adherence since the principal question concerned the prediction of relative improvement from baseline (by early adherence), not actual levels of outcomes at one or more assessment points in the study.
Comparison of the data shown in Table 2 to the data reported by Sacks et al. (2009 in Table 2 and Figs. 1, 2) shows that the mean changes in measures of adiposity and health for the subsample in this ancillary study may have been slightly greater than those reported for the full cohort (from either completer or intent-to-treat analyses). We did not test for statistical differences between the subsample and the full cohort, but it is logical based upon the results reported in this paper that a subsample that was more adherent (i.e., entered at least six computer tracking records) in the first 6 months of the intervention would have slightly greater improvement in outcomes related to adiposity and health.
As noted in the statistical methods section and as illustrated in Tables 2 and 3, data for body weight, waist circumference, and all health outcome variables were only collected at Months 6 and 24. Furthermore, percent body fat was only measured on 50% of the cohort. For these reasons, the canonical correlations were computed only at Months 6 and 24 and did not include percent body fat as a measure of changes in adiposity. It is noteworthy that in this smaller sample, changes in percent body fat were correlated with behavioral adherence at Month 6 (r = −0.45) and at Month 24 (r = −0.41). Also, the investigators calculated separate canonical correlations for participants in each of the four treatment arms of the POUNDS LOST study and found very similar results, i.e., two canonical correlations for both 6 and 24 month measurement periods, with behavioral adherence predicting adiposity outcomes, but not cardiovascular disease outcomes (R values at 6 months ranged from 0.51 to 0.58, P values < 0.001; R values at 24 months ranged from 0.41 to 0.43, P values < 0.07). With one exception, the canonical correlations for dietary adherence were not significant (R values ranged from 0.16 to 0.34, P values > 0.20). The only exception was in the Moderate Fat/High Protein treatment arm at 6 months; dietary adherence was associated with changes in insulin (R = 0.40, P < 0.01). It is important to note that statistical power for these within-treatment arm correlations was substantially lower than the primary findings reported for the entire study cohort. Nevertheless, the overall pattern of findings, especially pertaining to the relationship between early behavioral adherence and changes in adiposity is remarkably similar across all levels of analysis.
Contributor Information
Donald A. Williamson, Email: williada@pbrc.edu, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Stephen D. Anton, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Hongmei Han, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Catherine M. Champagne, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Ray Allen, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Eric LeBlanc, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Donna H. Ryan, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Jennifer Rood, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Katherine McManus, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA.
Nancy Laranjo, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA.
Vincent J. Carey, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA
Catherine M. Loria, National Heart, Lung, and Blood Institute, Bethesda, MD, USA
George A. Bray, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Frank M. Sacks, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA
References
- Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: Results from the A TO Z weight loss study. International Journal of Obesity (London) 2008;32(6):985–991. doi: 10.1038/ijo.2008.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. American Journal of Clinical Nutrition. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130(6):887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Fappa E, Yannakoulia M, Pitsavos C, Skoumas I, Valourdou S, Stefanadis C. Lifestyle intervention in the management of metabolic syndrome: Could we improve adherence issues? Nutrition. 2008;24(3):286–291. doi: 10.1016/j.nut.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Hall PA, Fong GT, Epp LJ, Elias LJ. Executive function moderates the intention-behavior link for physical activity and dietary behavior. Psychological Health. 2008;23(3):309–326. doi: 10.1080/14768320701212099. [DOI] [PubMed] [Google Scholar]
- Heiby EM, Lukens C. Identifying and addressing barriers to treatment adherence using behavioral analysis and modification techniques. In: O’Donahue WT, Levensky ER, editors. Promoting treatment adherence: A practical handbook for health care providers. Thousand Oaks, CA: Sage Publications; 2006. pp. 47–68. [Google Scholar]
- Levensky ER, O’Donahue WT. Patient adherence and nonadherence to treatments: An overview for health care providers. In: O’Donahue WT, Levensky ER, editors. Promoting treatment adherence: A practical handbook for health care providers. Thousand Oaks, CA: Sage Publications; 2006. pp. 47–68. [Google Scholar]
- Prochaska JM, Prochaska JO, Johnson SS. Assessing readiness for adherence to treatment. In: O’Donahue WT, Levensky ER, editors. Promoting treatment adherence: A practical handbook for health care providers. Thousand Oaks, CA: Sage Publications; 2006. pp. 47–68. [Google Scholar]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. New England Journal of Medicine. 2009;360(9):859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Look AHEAD Research Group. The Look AHEAD study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14(5):737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: The impact on weight loss in the PREFER study. Journal of Behavioral Medicine. 2008;31(1):81–92. doi: 10.1007/s10865-007-9135-2. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Anton SD, Han H, Champagne CM, Allen HR, LeBlanc E, et al. Adherence is a multidimensional construct in the POUNDS LOST trial. Journal of Behavioral Medicine. 2010;33(1):35–46. doi: 10.1007/s10865-009-9230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, Martin CK, Stewart TM. Behavioral weight control treatments. In: Hersen M, editor. Encyclopedia of Behavior Modification and Therapy. Vol. 1. Thousand Oaks, CA: Sage; 2005. pp. 167–171. Adult clinical applications. [Google Scholar]
- Williamson DA, Martin CK, Stewart TM. Behavioral strategies for controlling obesity. In: Bray GA, Ryan DH, editors. Overweight and the metabolic syndrome: From bench to bedside. New York: Springer; 2007. pp. 219–232. [Google Scholar]
- Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bouchard C, James WPT, editors. Handbook of obesity. New York: Marcel Dekker, Inc; 1998. pp. 855–873. [Google Scholar]