Abstract
Objectives
We used existing data systems to examine sexually transmitted disease (STD) and HIV/AIDS diagnosis rates and explore potential county-level associations between HIV/AIDS diagnosis rates and socioeconomic disadvantage.
Methods
Using South Carolina county data, we constructed multivariate ring maps to spatially visualize syphilis, gonorrhea, chlamydia, and HIV/AIDS diagnosis rates; gender- and race-specific HIV/AIDS diagnosis rates; and three measures of socioeconomic disadvantage—an unemployment index, a poverty index, and the Townsend index of social deprivation. Statistical analyses were performed to quantitatively assess potential county-level associations between HIV/AIDS diagnosis rates and each of the three indexes of socioeconomic disadvantage.
Results
Ring maps revealed substantial spatial association in STD and HIV/AIDS diagnosis rates and highlighted large gender and racial disparities in HIV/AIDS across the state. The mean county-level HIV/AIDS diagnosis rate (per 100,000 population) was 24.2 for males vs. 11.2 for females, and 34.8 for African Americans vs. 5.2 for white people. In addition, ring map visualization suggested a county-level association between HIV/AIDS diagnosis rates and socioeconomic disadvantage. Significant positive bivariate relationships were found between HIV/AIDS rate categories and each increase in poverty index category (odds ratio [OR] = 2.03; p=0.006), as well as each increase in Townsend index of social deprivation category (OR=4.98; p<0.001). A multivariate ordered logistic regression model in which all three socioeconomic disadvantage indexes were included showed a significant positive association between HIV/AIDS and Townsend index categories (adjusted OR=6.10; p<0.001).
Conclusions
Ring maps graphically depicted the spatial coincidence of STD and HIV/AIDS and revealed large gender and racial disparities in HIV/AIDS across South Carolina counties. This spatial visualization method used existing data systems to highlight the importance of social determinants of health in program planning and decision-making processes.
Rates of sexually transmitted diseases (STDs) and human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) persist at elevated levels in the United States.1,2 Moreover, significant gender and racial/ethnic disparities in STD and HIV/AIDS rates remain, despite a commitment by public health leaders and the Healthy People 2010 initiative to eliminate health disparities.3 For example, the rate of primary- and secondary-stage syphilis (reported cases) is higher for men (7.8 per 100,000 population) than for women (1.4 per 100,000 population),2 while the rate of HIV diagnoses is higher among African Americans (66.6 per 100,000 population) than among white people (7.2 per 100,000 population).1
In accordance with program guidelines established by the Centers for Disease Control and Prevention (CDC), efforts to reduce STD and HIV/AIDS transmission and to address gender and racial/ethnic disparities in disease rates should be data driven.4–8 Disease surveillance data alone do not provide the contextual information necessary to guide the development of meaningful community interventions. Rather, successful STD and HIV/AIDS program planning and evaluation require the compilation, prioritization, and synthesis of wide-ranging information sets, including data on disease rates,1,2,5 modes of transmission,9–11 comorbid conditions,12–16 and treatment options and efficacy.13,16–18 Data on risk-taking behaviors;19–23 health-care-seeking and compliance behaviors;22,24–27 and sociocultural attitudes toward sex, STDs, and HIV/AIDS also are relevant to STD and HIV/AIDS programming efforts.9,20,28,29 Moreover, a growing body of literature cites a positive association between local disease rates and levels of socioeconomic disadvantage. For example, higher rates of syphilis, gonorrhea, and chlamydia have been found in impoverished areas of Massachusetts and Rhode Island;30 higher rates of AIDS have been noted in low-income neighborhoods in Los Angeles County in California31 and in census-block groups characterized by high levels of poverty in Massachusetts;32 and higher rates of HIV have been reported in high-poverty census tracts in Virginia.33 Based on such evidence, successful disease interventions must also consider the socioeconomic context of STDs and HIV/AIDS.
Increasingly, geographic information systems (GISs) contribute critical spatial information to strengthen STD and HIV/AIDS program planning and evaluation processes.34–38 GIS visualization products—typically maps—yield valuable insight into relevant spatial distributions, patterns, and associations not readily apparent in tabled data. As useful as maps can be to STD/HIV/AIDS program planners and evaluators, the comparison and synthesis of information across multiple maps can prove cumbersome. A recent cartographic innovation, the ring map, facilitates the visual assessment of multivariate spatial data by depicting individual datasets as separate rings of information surrounding a base map of a particular geographic region of interest.39 In this way, a ring map effectively summarizes multiple layers of data, presenting an array of regional attributes (e.g., information about local population composition, health status, and/or socioeconomic conditions) in a single spatially referenced graphic.
In this investigation, ring maps were created to spatially visualize county-level syphilis, gonorrhea, chlamydia, and HIV/AIDS diagnosis rate data for South Carolina, a state that ranks third in the nation in chlamydia rates per 100,000 women2 and seventh in the rate of HIV diagnoses (ninth overall, including Puerto Rico and the U.S. Virgin Islands).1 In addition, a ring map was developed to visually explore potential county-level associations between HIV/AIDS diagnosis rates and socioeconomic disadvantage in South Carolina.
METHODS
STD and HIV/AIDS data
We acquired the numbers of syphilis, gonorrhea, and chlamydia cases diagnosed in the years 2006–2008 per county from the South Carolina Department of Health and Environmental Control (SC DHEC).40 Three-year average annual diagnosis rates (cases per 100,000 population) by county were calculated for each of the three STDs according to the following formula: three-year total number of diagnoses per county divided by the estimated county population in 2007 (the midpoint of the time period assessed), multiplied by 100,000, and then divided by three. Three-year (2006–2008) average annual HIV/AIDS diagnosis rates (HIV and AIDS cases per 100,000 population) for South Carolina counties were obtained from SC DHEC.41 Multiple-year rates provide more stable estimates of the relative numbers of STD and HIV/AIDS diagnoses, particularly in counties with small populations, making them preferable to single-year rates.
Socioeconomic measures
Relative socioeconomic disadvantage across South Carolina counties was evaluated using three separate indicators: (1) an unemployment index (percent of the civilian labor force that is unemployed), (2) a poverty index (percent of the population for whom poverty status is determined to be living below the federal poverty level), and (3) the Townsend index of social deprivation. The Townsend index is a composite measure based on four component indicators: unemployment (again, percent of the civilian labor force without jobs), vehicle access (percent of households with no vehicle available), household tenure (percent of households that rent rather than own a home), and household crowding (percent of households with more than one person per room). Social deprivation scores for geographic areas (e.g., counties, census tracts, and census-block groups) are calculated by deriving standardized z-scores based on each of the four component index distributions and by summing the resulting z-scores for each area.42 Studies have shown associations between numerous adverse health outcomes and local rates of poverty,30,43,44 unemployment,44–46 and social deprivation (as measured by the Townsend index).30,43,44 Thus, these indicators are appropriate for inclusion in an exploratory analysis of potential county-level associations between HIV/AIDS diagnosis rates and socioeconomic disadvantage.
County-level unemployment data for the single variable unemployment index were obtained from the U.S. Bureau of Labor Statistics.47 Annual unemployment rates from the years 2006–2008 were averaged to create the unemployment measure. Similarly, county-level annual poverty rates from the years 2006–2008, derived from U.S. Census Small Area Income and Poverty Estimates, were averaged to create the poverty index.48 Data for the county-level Townsend index of social deprivation were obtained from U.S. Census 2000 Summary File 3.49 Although the same data elements are available from the more recent American Community Survey 2006–2008 dataset, the restriction of data to geographic areas with populations of 20,000 or greater precluded their use, as several South Carolina counties have populations of less than 20,000.
Spatial visualization methods
We based our construction of county-level ring maps on Huang et al.'s original description of this innovative geovisualization method.39 Briefly, a core circle large enough to accommodate a base map of South Carolina counties was drawn to establish a graphic center for the ring map (Figure 1). A set of concentric circles then was drawn around the core. These circles were used to define individual rings around the base map, with each ring representing a separate layer of data. Next, 46 “spokes” of equal width—one for each of the state's counties—were distributed in radiating fashion at approximately 7.8-degree intervals (360 degrees divided by 46) on top of the ring set. Spokes were used to partition each ring into 46 county-level data visualization units. Finally, each ring was populated with a different county-level dataset, thereby creating a multivariate ring map graphic.
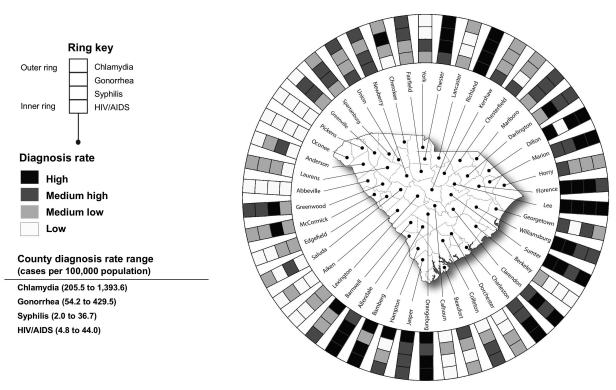
Figure 1.
Diagnosis rates of HIV/AIDS, syphilis, gonorrhea, and chlamydia in South Carolina by countya using a ring map spatial visualization methodb
aDiagnosis rate rankings are based on county rate distribution quartiles. Data source: South Carolina Department of Health and Environmental Control, 2006–2008.
bRing map available in a color presentation at http://ifs.sc.edu/PRMM/RingMaps
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
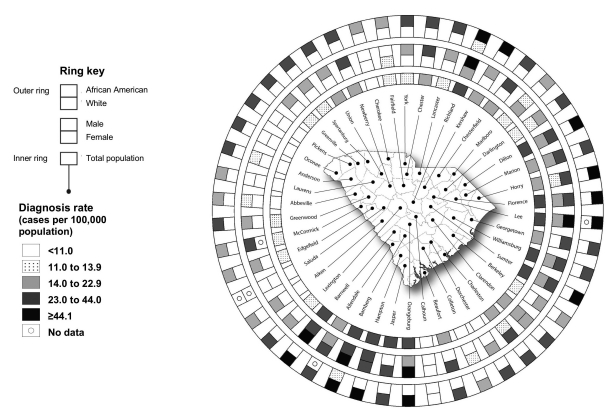
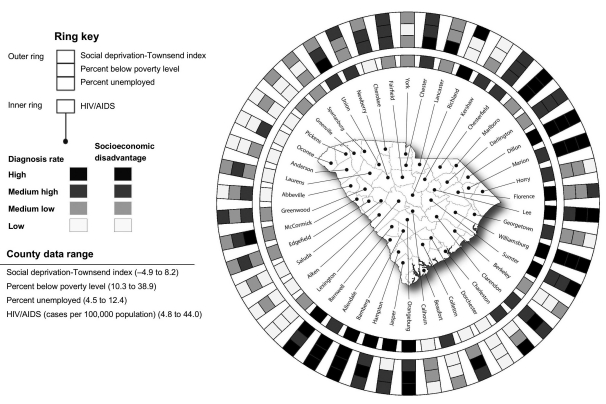
A total of three ring maps were created. In Figure 1, STD and HIV/AIDS diagnosis rate data were grouped into ordered, quartile categories (high, medium high, medium low, and low) to allow comparison of relative disease rates across counties. In Figure 2, disparities in gender- and race-specific HIV/AIDS diagnosis rates were examined. Diagnosis rate data for males, females, African Americans, and white people were grouped into four categories using quartile breaks from the total county-level HIV/AIDS diagnosis rate distribution, plus a fifth category representing values more than 2.8 standard deviations (SDs) above the total county-level population mean. Socioeconomic disadvantage (unemployment, poverty, and social deprivation) and HIV/AIDS diagnosis rate data were grouped into ordered quartiles in Figure 3 to facilitate visual exploration of the association between diagnosis rates and socioeconomic distress across counties. (The ring maps in Figures 1–3 are available in a color presentation at http://ifs.sc.edu/PRMM/RingMaps.) We developed the ring maps using ArcGIS® 9.3.1.50 For graphic enhancement, we added titles, legend information, and base map drop shadows to the maps using Adobe Photoshop® CS3 and Illustrator® CS3.51
Figure 2.
Diagnosis rate of HIV/AIDS in South Carolina counties by race and gendera using a ring map spatial visualization methodb
aData source: South Carolina Department of Health and Environmental Control, 2006–2008
bRing map available in a color presentation at http://ifs.sc.edu/PRMM/RingMaps
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Figure 3.
Diagnosis rate of HIV/AIDS and levels of socioeconomic disadvantagea in South Carolina by countyb,c, using a ring map spatial visualization methodd
aThree socioeconomic disadvantage measures are represented: Townsend index of social deprivation, percent below poverty level, and percent unemployed.
bDiagnosis rate and socioeconomic disadvantage rankings are based on county rate distribution quartiles.
cData sources: Census Bureau (US). Small area income and poverty estimates, county data, 2006–2008 [cited 2010 Apr 9]. Available from: http://www.census.gov/did/www/saipe; Census Bureau (US). Census 2000: summary file 3 [cited 2010 Apr 9]. Available from: URL: http://www.census.gov/main/www/cen2000.html; Bureau of Labor Statistics (US). Local area unemployment statistics, county data, 2006–2008 [cited 2010 Apr 9]. Available from: URL: http://www.bls.gov/lau/home.htm, 2006-2008; South Carolina Department of Environmental Control, 2006–2008
dRing map available in a color presentation at http://ifs.sc.edu/PRMM/RingMaps
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Statistical methods
Statistical analyses assessed potential county-level associations between HIV/AIDS diagnosis rates and each of the three indexes of socioeconomic disadvantage. In these analyses, HIV/AIDS diagnosis rates were grouped into ordered quartile categories; there were no tied diagnosis rates in the data. We investigated associations with the three disadvantage indexes using two scenarios: (1) treating each index as a continuous collection of quartile units, and (2) treating each measure as a continuous covariate in the original metric. Both bivariate and multivariate ordered logistic regression models were tested. Bivariate models assessed the association of each individual socioeconomic disadvantage index with HIV/AIDS diagnosis rate categories; multivariate models evaluated the association of socioeconomic disadvantage with HIV/AIDS diagnosis rate categories when all three disadvantage measures were considered simultaneously. We used Stata® version 11.052 for all statistical analyses.
RESULTS
For the years 2006–2008, average annual diagnosis rates (all rates are cases per 100,000 population) in South Carolina counties ranged from 2.0 to 36.7 for syphilis (mean = 10.4; SD=7.0), 54.2 to 429.5 for gonorrhea (mean = 214.7; SD=92.9), 205.5 to 1,393.6 for chlamydia (mean = 576.8; SD=237.2), and 4.8 to 44.0 for HIV/AIDS (mean = 17.5; SD=9.6). A ring map of diagnosis rate quartiles showed considerable spatial association in the rates of syphilis, gonorrhea, chlamydia, and HIV/AIDS across counties (Figure 1). Nine counties fell in the highest rate quartile on at least three of the four disease outcomes. Conversely, six counties were in the lowest quartile on at least three of the four conditions. Counties with relatively high diagnosis rates across conditions were predominantly found along a transection extending from Dillon County in the northeastern part of the state to Allendale County in the southwest. Counties with relatively low rates, on the other hand, were predominantly located in the state's northwestern region.
Gender disparities in HIV/AIDS were evident throughout the state. County-level diagnosis rates (again, all rates are cases per 100,000 population) for males ranged from 7.6 to 68.3 (mean = 24.2; SD=13.6), while rates among females ranged from 1.9 to 30.2 (mean = 11.2; SD=7.2). As shown in Figure 2, diagnosis rates for males were one or more class intervals higher than for females in 35 of the state's 45 counties with complete gender-specific data. Similarly, racial disparities in HIV/AIDS existed statewide. County-level diagnosis rates among African Americans ranged from 9.6 to 71.7 (mean = 34.8; SD=14.2), while rates for white people ranged from 0.8 to 13.5 (mean = 5.2; SD=2.8). As shown in Figure 2, diagnosis rates were one or more class intervals higher among African Americans than white people in 42 of the 43 counties with complete race-specific data.
A ring map display of ordered HIV/AIDS diagnosis rate quartiles—along with ordered unemployment, poverty, and Townsend index quartiles—revealed substantial spatial coincidence in relative rates of disease and socioeconomic disadvantage across counties (Figure 3). Of the 11 counties in the highest HIV/AIDS rate quartile, four also were in the highest unemployment rate quartile, six were in the highest poverty rate quartile, and eight were in the highest Townsend index social deprivation quartile. Eight of the 11 high HIV/AIDS rate counties fell in either the highest or second-highest unemployment rate quartile, nine fell in either the highest or second-highest poverty rate quartile, and all 11 fell in either the highest or second-highest social deprivation quartile. Conversely, four of the 11 counties in the lowest HIV/AIDS rate quartile also were in the lowest unemployment rate quartile, and eight were in the lowest social deprivation quartile. Moreover, eight of the low HIV/AIDS rate counties fell in either the lowest or second-lowest unemployment rate quartile, eight fell in either the lowest or second-lowest poverty rate quartile, and 10 fell in either the lowest or second-lowest social deprivation quartile.
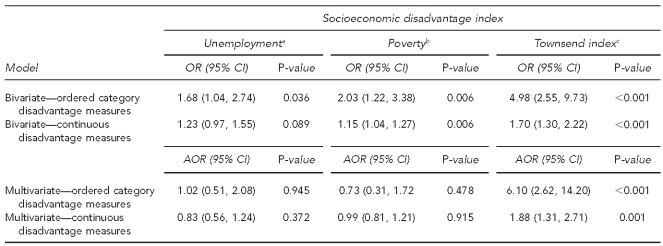
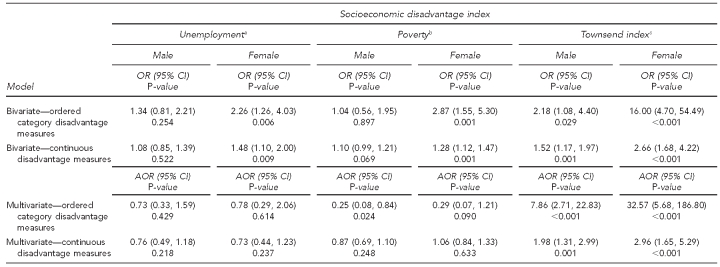
Bivariate statistical analyses of ordered categorical (quartile) data also suggested a county-level association between HIV/AIDS diagnosis rates and each of the three measures of socioeconomic disadvantage. All ordered logistic regression models assessing the bivariate relationship of HIV/AIDS diagnosis rate categories and socioeconomic disadvantage failed to reject the assumption of proportional odds/parallel lines (all p-values >0.1644). A significant positive relationship was found between HIV/AIDS rate categories and unemployment index categories at the α=0.05 level of significance (odds ratio [OR] = 1.68; p=0.036). That is, the odds of being in a higher HIV/AIDS diagnosis rate quartile were 1.68 times greater for each increase in quartile of the unemployment index. Likewise, significant positive bivariate relationships were found between HIV/AIDS rate categories and each increase in poverty index category (OR=2.03; p=0.006), as well as each increase in Townsend index of social deprivation category (OR=4.98; p<0.001).
In a multivariate ordered logistic regression model in which all of the socioeconomic disadvantage indexes were included as covariates, a significant positive association was found between HIV/AIDS diagnosis rate categories and Townsend index categories (adjusted OR [AOR] = 6.10; p<0.001). However, no significant associations emerged between HIV/AIDS rates and the other two socioeconomic disadvantage measures in the multivariate model. In bivariate models treating each socioeconomic measure as a continuous covariate in the original metric, significant positive associations were found between HIV/AIDS diagnosis rates and both the poverty index (OR=1.15; p=0.006) and the Townsend index (OR=1.70; p<0.001). Only the Townsend index of social deprivation was significantly associated with HIV/AIDS rates (AOR=1.88; p=0.001) in a multivariate model treating the socioeconomic measures as continuous covariates in the original metrics (Table 1).
Table 1.
County-level association between HIV/AIDS diagnosis rate categories (quartiles) and socioeconomic disadvantage in South Carolina, 2006–2008
aPercent of the civilian labor force that is unemployed
bPercent of the population for whom poverty status is determined to be living below the federal poverty level
cThe Townsend index is a composite measure based on four component indicators—unemployment (percent of the civilian labor force without jobs), vehicle access (percent of households with no vehicle available), household tenure (percent of households that rent rather than own a home), and household crowding (percent of households with more than one person per room). Social deprivation scores for South Carolina counties were calculated by deriving standardized z-scores based on each of the four component index distributions and by summing the resulting z-scores for each county.
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
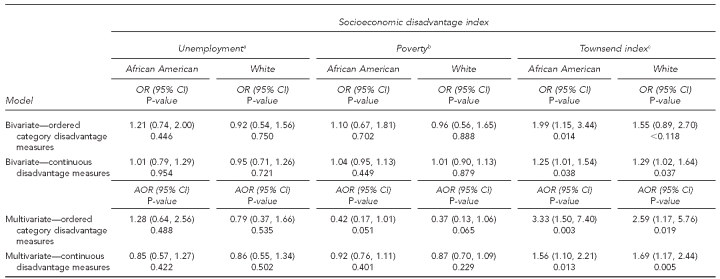
In bivariate statistical analyses stratified by gender, both unemployment and poverty were significantly positively associated with HIV/AIDS diagnosis rate categories among females; neither measure, however, was significantly associated with HIV/AIDS rate categories among males. For both males and females, a significant positive bivariate association was found between HIV/AIDS diagnosis rate categories and the Townsend index. Likewise, in multivariate models, the Townsend index was significantly positively associated with HIV/AIDS diagnosis rate categories for both males and females (Table 2). Finally, in both bivariate and multivariate statistical analyses stratified by race, the Townsend index was significantly positively associated with HIV/AIDS diagnosis rates among both African Americans and white people (Table 3).
Table 2.
County-level association between HIV/AIDS diagnosis rate categories (quartiles) and socioeconomic disadvantage in South Carolina by gender, 2006–2008
aPercent of the civilian labor force that is unemployed
bPercent of the population for whom poverty status is determined to be living below the federal poverty level
cThe Townsend index is a composite measure based on four component indicators—unemployment (percent of the civilian labor force without jobs), vehicle access (percent of households with no vehicle available), household tenure (percent of households that rent rather than own a home), and household crowding (percent of households with more than one person per room). Social deprivation scores for South Carolina counties were calculated by deriving standardized z-scores based on each of the four component index distributions and by summing the resulting z-scores for each county.
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
Table 3.
County-level association between HIV/AIDS diagnosis rate categories (quartiles) and socioeconomic disadvantage in South Carolina by race, 2006–2008
aPercent of the civilian labor force that is unemployed
bPercent of the population for whom poverty status is determined to be living below the federal poverty level
cThe Townsend index is a composite measure based on four component indicators—unemployment (percent of the civilian labor force without jobs), vehicle access (percent of households with no vehicle available), household tenure (percent of households that rent rather than own a home), and household crowding (percent of households with more than one person per room). Social deprivation scores for South Carolina counties were calculated by deriving standardized z-scores based on each of the four component index distributions and by summing the resulting z-scores for each county.
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
DISCUSSION
Ring maps graphically depicted the spatial coincidence of syphilis, gonorrhea, chlamydia, and HIV/AIDS across South Carolina counties (Figure 1) and highlighted the large gender and racial disparities in HIV/AIDS diagnosis rates that exist in the state (Figure 2). Information about the spatial distribution of disease rates and rate disparities can be useful in targeting at-risk populations, allocating resources for HIV prevention, and allocating resources for HIV/AIDS care and service delivery. County-level data may be especially helpful when counties or county aggregations serve as primary public health planning units.
A multivariate ring map display suggests a spatial association between local HIV/AIDS diagnosis rates and socioeconomic disadvantage in the study region (Figure 3). Counties with high diagnosis rates and high or medium-high levels of unemployment, poverty, and social deprivation—Dillon, Lee, Williamsburg, Sumter, Orangeburg, Hampton, Bamberg, and Barnwell counties—are readily apparent in the graphic. Notably, the visual assessment of the same data shown in the ring map would require the comparison and synthesis of information across multiple conventional choropleth maps. The ring map effectively streamlines the presentation of large amounts of data and, further, integrates multiple related datasets, thus increasing the relevancy of data to public health policy makers, planners, and evaluators.8
Bivariate statistical analyses also suggest a county-level association between HIV/AIDS diagnosis rates and socioeconomic disadvantage. Higher HIV/AIDS diagnosis rates were associated with higher levels of socioeconomic disadvantage (ordered categories), regardless of the socioeconomic measure. The Townsend index of social deprivation was most strongly associated with HIV/AIDS diagnosis rates; the unemployment index, on the other hand, was significantly associated only at the α=0.05 level of significance. In multivariate models that included all three socioeconomic disadvantage measures, only the Townsend index was significantly associated with HIV/AIDS diagnosis rate categories. The Townsend index remained significantly associated with HIV/AIDS in multivariate models stratified by gender and, separately, by race/ethnicity. Based on these results, and on findings from other studies,30,43 the Townsend index of social deprivation—which is easily constructed using readily available Census data—seems well-suited to STD/HIV/AIDS program decision makers as a measure of local socioeconomic disadvantage.
A causal relationship between socioeconomic disadvantage and diagnosis rates of HIV/AIDS cannot be inferred from this examination. The findings presented, however, are consistent with other studies that note relatively higher rates of STD/HIV/AIDS in socioeconomically deprived locations.30–33 These results lend further support to a social epidemiologic perspective that emphasizes the deleterious effect of such factors as poverty, income inequality, segregation, sexism, and racism on health status. The findings support the role of social determinants as potential pathways toward the reduction of adverse health outcomes and health disparities.53,54
Limitations
A major limitation associated with ring maps is the loss of spatial topology (information about the spatial continuity of geographic units) in the rings. For example, Richland County (in the center of the state) is surrounded by six adjacent counties; it has only two adjacent neighbors (Lancaster and Kershaw counties) in the rings, however, and only one of these actually shares a border with Richland (notably, though, complete spatial topology is represented in the central base map). Furthermore, the number of rings, as well as the number of enumeration units (e.g., counties) that can be represented in a single ring map are limited, both from a practical design standpoint and in terms of user comprehension. Other limitations common to all static maps include the representation of spatial data using predetermined (unchanging) classes and symbolization methods. Potentially, such limitations might be overcome in a dynamic (e.g., Web-based) ring mapping environment that allows direct user input in the selection, visualization, and exploration of multivariate datasets.55
The statistical analyses performed in this study served to quantitatively evaluate the association between HIV/AIDS diagnosis rates and socioeconomic disadvantage suggested in Figure 3. As noted, the statistical results obtained do not demonstrate any causal relationships. The actual association between HIV/AIDS rates and local socioeconomic disadvantage is almost certainly a complex one56–58 involving the interplay of individual-level characteristics (e.g., race/ethnicity,20,29,59,60 literacy,27 and risk-taking behaviors19–23); community-level attributes (e.g., population mobility,61 residential segregation,57–59 incidence of violent crime,62 and decay of the built environment63); characteristics of the health-care delivery system;58 and broader sociocultural attitudes, laws, regulations, policies, and practices.57 In South Carolina and other Deep South states, HIV/AIDS diagnosis rates may reflect the region's unique history,64 which includes African American slavery, overt and more subtle forms of racial discrimination, persistent poverty, and poor access to health-care services. Multilevel statistical models that simultaneously evaluate individual- and contextual-level variables may prove useful in determining the relative influence of individual, small-area socioeconomic, and sociocultural factors—including historical legacy effects—on HIV/AIDS rates and in identifying factors amenable to change that will result in lower rates of HIV/AIDS infection. Moreover, multilevel statistical methods might be used to examine, separately, the relationship between social determinants of health (SDH) and HIV infection and AIDS incidence.
Ring map visualization strengths
Ring map visualization represents an innovative method by which existing data systems can be used to highlight the importance of SDH in program planning and decision-making processes. The ring maps presented in this article serve only to introduce this multivariate cartographic tool to STD, HIV/AIDS, and other public health professionals. Ring maps may be adapted to spatially visualize wide-ranging datasets at multiple geographic scales. In addition to visualizing measures such as STD and HIV/AIDS diagnosis rates, poverty, and unemployment, ring maps might be used to display such small-area characteristics as income inequality, residential segregation, age structure, educational attainment, family fragmentation, linguistic isolation, housing affordability, and population mobility. Spatial data in rings can be summarized at the county level, as shown in Figures 1–3, or at other relevant geographic levels, including census tract, ZIP code area, or public health service area.55 Notably, the base map itself can be used to display a layer of information. In Figure 1, for example, the base map might highlight counties meeting specific evaluation criteria—perhaps those in the highest or second-highest HIV/AIDS diagnosis rate quartile and in the lowest syphilis rate quartile. Moreover, ring maps can convey time-series data for a single health condition. A map with 10 rings, for instance, might show annual incidence rates of HIV over a 10-year period, while a map with 12 rings might depict the weekly incidence of cases associated with a syphilis outbreak over a 12-week time frame. Ring maps, thus, can be used to visualize and explore diverse data elements across both space and time.39,55,65
CONCLUSIONS
A ring map depicts and integrates multiple layers of region-specific data in a single spatially referenced graphic. Ring map visualization can be used to identify spatial and temporal trends in STD and HIV/AIDS diagnosis rates; highlight gender and racial/ethnic disparities in STD and HIV/AIDS; and explore potential contextual associations between HIV/AIDS and such SDH as poverty, unemployment, income inequality, and residential segregation. Rather than serving as stand-alone information products, ring maps can supplement and summarize other map products, suggest specific spatial analytical approaches (e.g., a network analysis to evaluate geographic access to health care in low- vs. high-poverty neighborhoods), aid in the formulation of statistical hypotheses, and generate questions to be followed up in surveys or focus groups. Using existing data systems, ring maps can strengthen a multi-methodological strategy aimed at reducing the burden of STD and HIV/AIDS across gender, racial/ethnic, and socioeconomic categories.
REFERENCES
- 1.Centers for Disease Control and Prevention (US). Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2009. Atlanta: CDC; 2011. [[cited 2011 Apr 5]]. Also available from: URL: http://www.cdc.gov/hiv/surveillance/resources/reports/2009report/index.htm.
- 2.CDC (US). 2009 sexually transmitted disease surveillance. Atlanta: CDC; 2010. [[cited 2011 Apr 5]]. Also available from: URL: http://www.cdc.gov/std/stats09/default.htm.
- 3.Department of Health and Human Services (US). Healthy People 2010. Washington: HHS; 2000. [[cited 2010 Apr 9]]. Also available from: URL: http://www.healthypeople.gov/2010/About/goals.htm.
- 4.CDC (US). 2003–2008 HIV prevention community planning guidance. Atlanta: CDC; 2003. [[cited 2010 Apr 9]]. Also available from: URL: http://www.cdc.gov/hiv/topics/cba/resources/guidelines/hiv-cp/pdf/hiv-cp.pdf.
- 5.Jenkins RA, Carey JW. Decision making for HIV prevention planning: organizational considerations and influencing factors. AIDS Behav. 2005;9(2 Suppl):S1–8. doi: 10.1007/s10461-005-3941-8. [DOI] [PubMed] [Google Scholar]
- 6.Amaro H, Blake SM, Morrill AC, Cranston K, Logan J, Conron KJ, et al. HIV prevention community planning: challenges and opportunities for data-informed decision-making. AIDS Behav. 2005;9(2 Suppl):S9–27. doi: 10.1007/s10461-005-3942-8. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins RA, Robbins A, Cranston K, Batchelor K, Freeman AC, Averbach AR, et al. Bridging data and decision making: development of techniques for improving the HIV prevention community planning process. AIDS Behav. 2005;9(2 Suppl):S41–53. doi: 10.1007/s10461-005-3944-5. [DOI] [PubMed] [Google Scholar]
- 8.Jenkins RA, Averbach AR, Robbins A, Cranston K, Amaro H, Morrill AC, et al. Improving the use of data for HIV prevention decision making: lessons learned. AIDS Behav. 2005;9(2 Suppl):S87–99. doi: 10.1007/s10461-005-3947-8. [DOI] [PubMed] [Google Scholar]
- 9.Morison L. The global epidemiology of HIV/AIDS. Br Med Bull. 2001;58:7–18. doi: 10.1093/bmb/58.1.7. [DOI] [PubMed] [Google Scholar]
- 10.Adler MW. ABC of AIDS: development of the epidemic. BMJ. 2001;322:1226–9. doi: 10.1136/bmj.322.7296.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beckwith CG, Moreira CC, Aboshady HM, Zaller N, Rich JD, Flanigan TP. A success story: HIV prevention for injection drug users in Rhode Island. Subst Abuse Treat Prev Policy. 2006;1:34. doi: 10.1186/1747-597X-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albalak R, O'Brien RJ, Kammerer JS, O'Brien SM, Marks SM, Castro KG, et al. Trends in tuberculosis/human immunodeficiency virus comorbidity, United States, 1993–2004. Arch Intern Med. 2007;167:2443–52. doi: 10.1001/archinte.167.22.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain MK, Comanor L, White C, Kipnis P, Elkin C, Leung K, et al. Treatment of hepatitis B with lamivudine and tenofovir in HIV/HBV-coinfected patients: factors associated with response. J Viral Hepat. 2007;14:176–82. doi: 10.1111/j.1365-2893.2006.00797.x. [DOI] [PubMed] [Google Scholar]
- 14.Israelski DM, Prentiss DE, Lubega S, Balmas G, Garcia P, Muhammad M, et al. Psychiatric co-morbidity in vulnerable populations receiving primary care for HIV/AIDS. AIDS Care. 2007;19:220–5. doi: 10.1080/09540120600774230. [DOI] [PubMed] [Google Scholar]
- 15.Yu J, Appel PW, Warren BE, Rubin S, Gutierrez R, Larson B, et al. Substance abuse intervention services in public STD clinics: a pilot experience. J Subst Abuse Treat. 2008;34:356–62. doi: 10.1016/j.jsat.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Cohen MS, Hellman N, Levy JA, DeCock K, Lange J. The spread, treatment, and prevention of HIV-1: evolution of a global pandemic. J Clin Invest. 2008;118:1244–54. doi: 10.1172/JCI34706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simon V, Ho DD, Abdool Karim Q. HIV/AIDS epidemiology, pathogenesis, prevention, and treatment. Lancet. 2006;368:489–504. doi: 10.1016/S0140-6736(06)69157-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Workowski KA, Berman SM. Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis. 2007;44(Suppl 3):S73–6. doi: 10.1086/511430. [DOI] [PubMed] [Google Scholar]
- 19.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV/STD racial disparities: the need for new directions. Am J Public Health. 2007;97:125–32. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herbst JH, Kay LS, Passin WF, Lyles CM, Crepaz N, Marin BV. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11:25–47. doi: 10.1007/s10461-006-9151-1. [DOI] [PubMed] [Google Scholar]
- 21.Jemmott LS, Jemmott JB, 3rd, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health. 2007;97:1034–40. doi: 10.2105/AJPH.2003.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lansky A, Sullivan PS, Gallagher KM, Fleming PL. HIV behavioral surveillance in the U.S.: a conceptual framework. Public Health Rep. 2007;122(Suppl 1):16–23. doi: 10.1177/00333549071220S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cavazos-Rehg PA, Spitznagel EL, Schootman M, Strickland JR, Afful SE, Cottler LB, et al. Risky sexual behaviors and STDs: a comparison study of cocaine-dependent individuals in treatment versus a community matched sample. AIDS Patient Care STDS. 2009;23:727–34. doi: 10.1089/apc.2008.0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kellerman SE, Lehman JS, Lansky A, Stevens MR, Hecht FM, Bindman AB, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J Acquir Immune Defic Syndr. 2002;31:202–10. doi: 10.1097/00126334-200210010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Rajabiun S, Mallinson RK, McCoy K, Coleman S, Drainoni ML, Rebholz C, et al. “Getting me back on track”: the role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical care. AIDS Patient Care STDS. 2007;21(Suppl 1):S20–9. doi: 10.1089/apc.2007.9990. [DOI] [PubMed] [Google Scholar]
- 26.Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, et al. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007;26:40–9. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalichman SC, Pope H, White D, Cherry C, Amaral CM, Swetzes C, et al. Association between health literacy and HIV treatment adherence: further evidence from objectively measured medication adherence. J Int Assoc Physicians AIDS Care (Chic) 2008;7:317–23. doi: 10.1177/1545109708328130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 29.Valentine JA. Impact of attitudes and beliefs regarding African American sexual behavior on STD prevention and control in African American communities: unintended consequences. Sex Transm Dis. 2008;35(12 Suppl):S23–9. doi: 10.1097/OLQ.0b013e31818d3cc7. [DOI] [PubMed] [Google Scholar]
- 30.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infection, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US) Public Health Rep. 2003;118:240–60. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Simon PA, Hu DJ, Diaz T, Kerndt PR. Income and AIDS rates in Los Angeles County. AIDS. 1995;9:281–4. [PubMed] [Google Scholar]
- 32.Zierler S, Krieger N, Tang Y, Coady W, Siegfried E, DeMaria A, et al. Economic deprivation and AIDS incidence in Massachusetts. Am J Public Health. 2000;90:1064–73. doi: 10.2105/ajph.90.7.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dolan C, Delcher C. Monitoring health inequities and planning in Virginia: poverty, human immunodeficiency virus, and sexually transmitted infections. Sex Transm Dis. 2008;35:981–4. doi: 10.1097/OLQ.0b013e318182a571. [DOI] [PubMed] [Google Scholar]
- 34.Bissette JM, Stover JA, Newman LM, Delcher PC, Bernstein KT, Matthews L. Assessment of geographic information systems and data confidentiality guidelines in STD programs. Public Health Rep. 2009;124(Suppl 2):58–64. doi: 10.1177/00333549091240S209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zenilman JM, Glass G, Shields T, Jenkins PR, Gaydos JC, McKee KT., Jr. Geographic epidemiology of gonorrhea and chlamydia on a large military installation: application of a GIS system. Sex Transm Infect. 2002;78:40–4. doi: 10.1136/sti.78.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Winter AJ, Sriskandabalan P, Wade AA, Cummins C, Barker P. Sociodemography of genital chlamydia trachomatis in Coventry, UK, 1992–6. Sex Transm Infect. 2000;76:103–9. doi: 10.1136/sti.76.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zenilman JM, Ellish N, Fresia A, Glass G. The geography of sexual partnerships in Baltimore: applications of core theory dynamics using a geographic information system. Sex Transm Dis. 1999;26:75–81. doi: 10.1097/00007435-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Geanuracos CG, Cunningham SD, Weiss G, Forte D, Reid LM, Ellen JM. Use of geographic information systems for planning HIV prevention interventions for high-risk youths. Am J Public Health. 2007;97:1974–81. doi: 10.2105/AJPH.2005.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang G, Govoni S, Choi J, Hartley DM, Wilson JM. Geovisualizing data with ring maps. [[cited 2010 Feb 23]];ArcUser. 2008 11:54–5. Also available from: URL: http://www.esri.com/news/arcuser/0408/files/ringmaps.pdf. [Google Scholar]
- 40.South Carolina Department of Health and Environmental Control. South Carolina's STD/HIV/AIDS data, STD/HIV Division surveillance report. Columbia (SC): South Carolina Department of Health and Environmental Control; 2008. [[cited 2010 Apr 9]]. Also available from: URL: http://www.scdhec.gov/health/disease/sts/docs/HIVSTD_SurvRpt_Dec2008.pdf.
- 41.South Carolina Department of Health and Environmental Control. HIV/AIDS/STD surveillance reports. [[cited 2010 Mar 15]]. Available from: URL: http://www.scdhec.gov/health/disease/sts/index.htm.
- 42.Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the north. London: Croom Helm Ltd.; 1987. [Google Scholar]
- 43.Lopez De Fede A, Stewart JE, Harris MJ, Mayfield-Smith K. Tuberculosis in socio-economically deprived neighborhoods: missed opportunities for prevention. Int J Tuberc Lung Dis. 2008;12:1425–30. [PubMed] [Google Scholar]
- 44.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area-based socioeconomic measures to monitor social inequalities in low birthweight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Campo P, Gielen AC, Faden RR, Xue X, Kass N, Wang MC. Violence by male partners against women during the childbearing year: a contextual analysis. Am J Public Health. 1995;85(8 Pt 1):1092–7. doi: 10.2105/ajph.85.8_pt_1.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62:2061–71. doi: 10.1016/j.socscimed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 47.Bureau of Labor Statistics (US). Local area unemployment statistics, county data, 2006–2008. [[cited 2010 Apr 9]]. Available from: URL: http://www.bls.gov/lau/home.htm.
- 48.Census Bureau (US). Small area income and poverty estimates, county data, 2006–2008. [[cited 2010 Apr 9]]. Available from: URL: http://www.census.gov/did/www/saipe.
- 49.Census Bureau (US). Census 2000: summary file 3. [[cited 2010 Apr 9]]. Available from: URL: http://www.census.gov/main/www/cen2000.html.
- 50.ESRI . ArcGIS®: Version 9.3.1. Redlands (CA): ESRI; 2009. [Google Scholar]
- 51.Adobe Systems Inc. Photoshop® CS3 and Illustrator® CS3. San Jose (CA): Adobe Systems Inc.; 2007. [Google Scholar]
- 52.StataCorp LP. Stata®: Version 11.0. College Station (TX): StataCorp LP; 2009. [Google Scholar]
- 53.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30:668–77. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 54.Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. 2001;55:693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stewart JE, Battersby SE, Lopez-De Fede A, Remington KC, Hardin JW, Mayfield-Smith K. Diabetes and the socioeconomic and built environment: geovisualization of disease prevalence and potential contextual associations using ring maps. Int J Health Geogr. 2011;10:18. doi: 10.1186/1476-072X-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.CDC (US). Addressing social determinants of health: accelerating the prevention and control of HIV/AIDS, viral hepatitis, STD and TB. External consultation meeting report, 2008 Dec 9–10. Atlanta: CDC; 2009. [[cited 2010 Apr 9]]. Also available from: URL: http://www.cdc.gov/socialdeterminants/docs/final_SDHConsultation_ForWeb_061109.pdf.
- 57.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 58.Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35(12 Suppl):S13–8. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 59.Barrow RY, Newman LM, Douglas JM. Taking positive steps to address STD disparities for African-American communities. Sex Transm Dis. 2008;35(12 Suppl):S1–3. doi: 10.1097/OLQ.0b013e31818fbc92. [DOI] [PubMed] [Google Scholar]
- 60.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. 2008;372:337–40. doi: 10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- 61.Aral SO, Lipshutz J, Blanchard J. Drivers of STD/HIV epidemiology and the timing and targets of STD/HIV prevention. Sex Transm Infect. 2007;83(Suppl 1):1–14. doi: 10.1136/sti.2007.027169. [DOI] [PubMed] [Google Scholar]
- 62.Wallace R, Wallace D. Socioeconomic determinants of health: community marginalisation and the diffusion of disease and disorder in the United States. BMJ. 1997;314:1341–5. doi: 10.1136/bmj.314.7090.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. Am J Public Health. 2003;93:467–71. doi: 10.2105/ajph.93.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reif S, Geonnotti KL, Whetten K. HIV infection and AIDS in the Deep South. Am J Public Health. 2006;96:970–3. doi: 10.2105/AJPH.2005.063149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Johnson S; Ontario Agency for Health Protection and Promotion (Canada). Ring maps: a useful visualization technique for pandemic H1N1. Presented at Public Health GIS Projects Across Ontario; Toronto, Ontario: 2009. Nov 30, [[cited 2010 Apr 9]]. Also available from: URL: http://www.oahpp.ca/resources/documents/presentations/2009nov30/4%20OAHPP_Ring_Maps_SJ_112509.pdf. [Google Scholar]