Abstract
MMP-3 is capable of degrading a variety of proteins, including agrin, which plays a critical role in neuromuscular signaling by controlling acetylcholine receptor clustering. High MMP-3 levels in a proportion of myasthenia gravis (MG) patients have been reported. A pathogenic role of MMP-3 in other neurological disorders has been suggested but not proven. We have therefore examined the levels of MMP-3 in 124 MG patients and compared them to 59 multiple sclerosis (MS) patients, 74 epilepsy patients, 33 acute stroke patients, and 90 healthy controls. 15.3% of the patients in the MG group were MMP-3-positive (defined as higher than cutoff value 48 ng/mL) with very high mean MMP-3 concentration (79.9 ng/mL), whereas the proportion of MMP-3 positive patients in the MS (3.4%), epilepsy (6.7%), stroke (0%), and the control group (4.4%) was significantly lower. Mean MMP-3 concentration in the total MG group (25.5 ng/mL) was significantly higher than in the MS (16.6 ng/mL) and stroke (11.7 ng/mL) groups, but did not differ significantly from the epilepsy (19.4 ng/mL) and the control group (23.4 ng/mL). MMP-3 may have a specific pathogenic effect in MG in addition to being associated with autoimmune diseases in general.
1. Introduction
Matrix metalloproteinase-3 (MMP-3) is a matrix enzyme capable of breaking down various extracellular components, including collagens (types III, IV, V, IX, and XI), matrix proteins, and proteoglycans. MMP-3 can also activate other MMPs such as MMP-9 [1, 2]. Agrin is a substrate for the endopeptidase MMP-3, stromelysin1 [3]. MMP-3 null mice have alterations to their neuromuscular junctions, including increased acetylcholine receptor (AChR) staining at the endplate and an increased number of junctional folds. An increased concentration of agrin occurs at the neuromuscular junction of such mice [4]. These observations indicate that MMP-3 is involved in controlling the structure of the neuromuscular junction via regulation of agrin levels.
Myasthenia gravis (MG) is an autoimmune disorder which causes skeletal muscle weakness. Antibodies targeting the AChR are present in 85% of patients with generalized MG (GMG) and in about 50% of patients with ocular MG (OMG) [5, 6]. MG with AChR antibodies is known as seropositive MG (SPMG). Thymoma is present in approximately 15% of MG patients [7]. Antibodies to AChR impair neuromuscular transmission by complement-mediated postsynaptic membrane damage, direct blockade of ligand-receptor interaction, and/or by an increased degradation of AChR [5, 8]. MG without detectable antibodies to the AChR is termed seronegative MG (SNMG) [9]. Antibodies to muscle-specific kinase (MuSK) are observed in a proportion of SNMG patients [10, 11]. MuSK is a key signaling protein controlling AChR clustering and the formation of the neuromuscular junction. These processes are triggered by the release of agrin from the nerve terminals. Agrin interaction with MuSK leads to the phosphorylation of AChR [12, 13].
Elevated serum MMP-3 levels have previously been reported in the autoimmune disorders systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) [14, 15]. A pathogenic role of MMP-3 in these connective tissue disorders could be related to its ability to degrade extracellular matrix components. SLE and RA have an increased incidence in MG patients [16, 17], indicating shared pathogenic mechanisms. These disorders are associated with localized autoimmune diseases such as Hashimoto's thyroiditis and Graves' disease [18].
In MG patients, an elevated MMP-3 level, in addition to promoting autoimmune disease in general, may cause damage to the neuromuscular junction due to increased degradation of agrin, and thereby contribute to an increased muscle weakness. In a previous study [19], we demonstrated a significant elevation in MMP-3 levels in a proportion of both SPMG and SNMG, indicating a pathogenic role for MMP-3 in MG. Little is known about MMP-3 in other autoimmune and nonautoimmune neurological disorders. We have therefore examined the levels of MMP-3 in sera from MG patients and compared them to those in multiple sclerosis (MS) patients, epilepsy patients, acute stroke patients, and healthy controls.
2. Materials and Methods
2.1. Patients and Sera
Serum samples from 124 MG patients (104 SPMG and 20 SNMG), 59 MS patients, 74 epilepsy patients, 33 acute stroke patients, and 90 healthy controls available in our biobank, taken from different individuals, were included (Table 1). The MG and MS sera were collected randomly at various disease phases from in and outpatients admitted to our department. The sera from the epilepsy patients and the acute stroke patients were obtained within 24 hours after last seizure or acute stroke, respectively, from inpatients admitted to our department. The MG group included patients with early-onset MG (MG onset before age 50 years), late-onset MG (MG onset at or after age 50 years), thymoma MG and nonthymoma MG, and patients with various antibodies including antiAChR, antiryanodine receptor and antititin antibodies, but none with MuSK antibodies. None of the patients had any confounding diseases, such as SLE or RA. The control sera were collected randomly from healthy individuals. All sera were stored at −20°C.
Table 1.
MMP-3 concentrations (ng/mL) in patients with neurological disorders and healthy controls.
| MG | MS | Epilepsy | Stroke | Healthy controls | |
|---|---|---|---|---|---|
| Number of patients | 124 | 59 | 74 | 33 | 90 |
| Mean MMP-3 concentration | 25.5 (±27.4) | 16.6 (±23.9) | 19.4 (±16.4) | 11.7 (±8.1) | 23.4 (±12.3) |
| Number of MMP-3-positives | 19 (15.3%) | 2 (3.4%) | 5 (6.7%) | 0 | 4 (4.4%) |
| Mean MMP-3 concentration of MMP-3-positives | 79.9 (±27.9) | 116.5 (±89.8) | 67.0 (±21.2) | 0 | 54.0 (±3.6) |
2.2. Serum MMP-3 Levels
Total MMP-3 levels were assessed using the Quantikine MMP-3 Elisa kit as per manufacturer's instructions (R&D Systems Europe Ltd. Abingdon, UK). Patient sera were assayed at a dilution of 1 : 10 in duplicate wells. A standard curve (0.156 ng/mL–20 ng/mL MMP-3) was produced and the MMP-3 concentration (ng/mL) determined.
The cut-off level between a normal and a high MMP-3 level (hereafter referred to as MMP-3-positive) was defined as the mean MMP-3 concentration for the 90 controls + 2 SDs, which equals 48 ng/mL (Figure 1).
Figure 1.
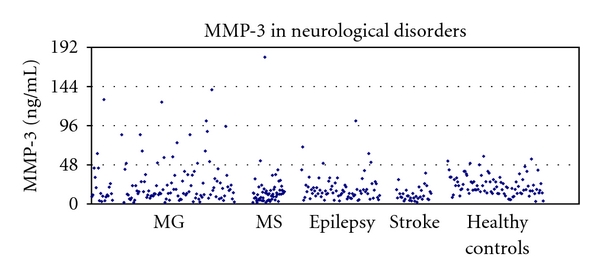
Scatter plot of the MMP-3 concentrations in patients with neurological disorders and healthy controls. The 2 SD cut-off at 48 ng/mL is indicated.
2.3. Statistical Analyses
The numbers of patients in the various groups were compared using the Chi-square test. The MMP-3 concentrations in the different groups were compared using the t-test for difference between population means.
3. Results
Nineteen (15.3%) MG patients were MMP-3-positive, whereas the numbers of MMP-3-positive patients in the MS, epilepsy and control groups were very low (3%, 6%, and 4%, resp.). There were no MMP-3-positive patients in the acute stroke group (Table 1, Figure 1). The number of MMP-3-positive patients in the MG group was significantly higher than the number of MMP-3-positive patients in the MS group (P = 0.034), the acute stroke group (P = 0.036), and the control group (P = 0.021), but did not reach significance for the epilepsy group (P = 0.118) (Table 1).
The MG group had the highest mean MMP-3 concentration. It was significantly higher than the mean MMP-3 concentration in the MS group (P = 0.013), the epilepsy group (P = 0.026), and the acute stroke group (P < 0.001), but did not differ significantly from that in the control group (P = 0.225) (Table 1). Mean MMP-3 concentration of the 19 MMP-3-positive MG patients was significantly higher than mean MMP-3 concentration in the total MG group (P < 0.001) and in the total control group (P < 0.001). Mean MMP-3 concentration of the 19 MMP-3-positive MG patients was also significantly higher than mean MMP-3 concentration of the four MMP-3-positive controls (P = 0.001) but did not differ significantly from mean concentration of the five MMP-3-positive epilepsy patients (P = 0.148) (Table 1). Mean MMP-3 concentration was lowest in the acute stroke group. It was significantly lower than mean MMP-3 concentration in the MG group (P < 0.001), the epilepsy group (P < 0.001), and the control group (P < 0.001) and tended to be lower than that in the MS group (P = 0.078) (Table 1). The MS group had significantly higher mean MMP-3 concentration than the controls (P = 0.024), in contrast to the epilepsy group that had lower mean MMP-3 than the controls (P = 0.042) (Table 1).
4. Discussion
A proportion of MG patients (15.3%) had markedly increased MMP-3 levels. This was unique as compared to patients with other neurological disorders in this study. Similarly, the mean MMP-3 concentration in the MG group was increased. In a previous study [19], we demonstrated that elevated MMP-3 levels are present in both SPMG and SNMG and thus is linked to MG in general.
MMP-3-positive MG patients exhibited high mean MMP-3 concentrations (79.9 ng/mL) compared to the whole MG group (25.5 ng/mL) and controls (23.4 ng/mL), indicating that these patients represent a subgroup with differences in pathophysiology and/or clinical presentation. Our cohort comprised patients at different age, gender, disease severity, and disease types (SPMG, SNMG, early-onset MG, late-onset MG, thymoma MG, and nonthymoma MG). It was not possible to correlate MMP-3-positive patients with a specific subset of MG patients, perhaps due to low number of MMP-3-positive MG patients and large variation in disease entities. A similar subgroup with high MMP-3 levels in another MG cohort was recently reported, containing GMG, OMG, SPMG, and SNMG patients [20].
None of our acute stroke patients had elevated MMP-3 levels, and mean MMP-3 concentration was lower than in any other group examined. MMP-3 may play a role in the pathophysiology of acute stroke [21]. Thromboembolic mechanisms and MMP-3 consumption may be the cause of the low MMP-3 concentrations seen in acute stroke.
In an earlier study, Kanesaka et al. found elevated MMP-3 levels during the relapsing phase of relapsing-remitting MS compared to the remission phase [22]. In our study, MS and MG patients were included regardless of disease phase or severity. This may explain the discrepancy between our results and those of Kanesaka et al. Our conclusion is that MG patients have higher MMP-3 levels than MS patients when disease phase and severity are not taken into consideration.
Very high mean MMP-3 concentrations of 258 ± 35 ng/mL and 187 ± 14 ng/mL have previously been reported in SLE and RA patients, markedly higher than in our MG patients [14]. However, mean serum MMP-3 concentration in our control group is approximately half that observed for the controls in that previous study. Methodological variation may therefore explain this difference between MG and SLE/RA. Serum levels of MMP-3 may not represent the concentration of MMP-3 at the site(s) of tissue damage, since MMP-3 can be produced locally and there have a concentration higher than observed in the general circulation. Serum MMP-3 levels may be higher in systemic diseases such as SLE and RA compared to MG with more focal damage.
Since agrin is required for the clustering of AChR in the neuromuscular junction, increased degradation of agrin and subsequent disruption of MuSK signaling, may have important consequences for the correct formation and function of the neuromuscular junction and lead to a reduction in the safety factor for successful neuromuscular transmission. Agrin is also capable of inducing the expression of the ϵ subunit of the AChR [23, 24]. MMP-3 null mice show alterations to their neuromuscular junctions [4], probably via an effect on agrin.
An increased MMP-3 level as a cause of MG is unlikely, since MMP-3 levels are increased in patients with SLE and RA who do not have MG [14, 15]. The mechanism by which MMP-3 is upregulated and the significance of an increased level of MMP-3 in MG, SLE, and RA is unknown. By expanding our patient database, we hope to identify clinical or immunological associations with the observed increase in MMP-3, further elucidating mechanisms and significance.
Some MG patients have high MMP-3 serum concentrations, and this may reflect a subgroup with different pathophysiology and/or different clinical presentation. Dysregulation of MMP-3 could be a common feature of autoimmune diseases, including MG, SLE, and RA, but not MS as examined in this study. The mechanism(s) by which altered MMP-3 levels in MG and acute stroke occurs, and its pathological significance remain to be established. MMP-3 testing might be useful as an indicator of acute cerebral ischemia in its very early phase.
Acknowledgments
This study was funded by a grant from the Norwegian Foundation for Muscle Disease Research. The authors declare no conflict of interests.
Abbreviations
- AChR:
Acetylcholine receptor,
- MG:
Myasthenia gravis,
- MMP-3:
Matrix metalloproteinase-3,
- MS:
Multiple sclerosis,
- MuSK:
Muscle specific kinase,
- RA:
Rheumatoid arthritis,
- SLE:
Systemic lupus erythematosus,
- SNMG:
Seronegative myasthenia gravis,
- SPMG:
Seropositive myasthenia gravis.
References
- 1.Sternlicht MD, Werb Z. ECM proteinases. In: Kreis T, Vale R, editors. Guidebook to the Extracellular Matrix and Adhesion Proteins. New York, NY, USA: Oxford University Press; 1999. pp. 503–562. [Google Scholar]
- 2.Yong VW, Agrawal SM, Stirling DP. Targeting MMPs in acute and chronic neurological conditions. Neurotherapeutics. 2007;4(4):580–589. doi: 10.1016/j.nurt.2007.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.VanSaun M, Werle MJ. Matrix metalloproteinase-3 removes agrin from synaptic basal lamina. Journal of Neurobiology. 2000;43(2):140–149. [PubMed] [Google Scholar]
- 4.VanSaun M, Herrera AA, Werle MJ. Structural alterations at the neuromuscular junctions of matrix metalloproteinase 3 null mutant mice. Brain Cell Biology. 2003;32(9):1129–1142. doi: 10.1023/B:NEUR.0000021907.68461.9c. [DOI] [PubMed] [Google Scholar]
- 5.Lindstrøm JM, Seybold ME, Lennon VA, Whittingham S, Duane DD. Antibody to acetylcholine receptor in myasthenia gravis: prevalence, clinical correlates, and diagnostic value. Neurology. 1998;51:933–939. doi: 10.1212/wnl.51.4.933-a. [DOI] [PubMed] [Google Scholar]
- 6.Evoli A, Batocchi AP, Minisci C, Di Schino C, Tonali P. Therapeutic options in ocular myasthenia gravis. Neuromuscular Disorders. 2001;11(2):208–216. doi: 10.1016/s0960-8966(00)00173-5. [DOI] [PubMed] [Google Scholar]
- 7.Wilcox N. Myasthenia gravis. Current Opinion in Immunology. 1993;5:910–917. doi: 10.1016/0952-7915(93)90105-2. [DOI] [PubMed] [Google Scholar]
- 8.Li Z, Forester N, Vincent A. Modulation of acetylcholine receptor function in TE671 (rhabdomyocyosarcoma) cells by non-AchR ligands: possible relevance to seronegative myasthenia gravis. Journal of Neuroimmunology. 1996;64(2):179–183. doi: 10.1016/0165-5728(95)00169-7. [DOI] [PubMed] [Google Scholar]
- 9.Mossman S, Vincent A, Newsom-Davis J. Myasthenia gravis without acetylcholine receptor antibody: a distinct disease entity. The Lancet. 1986;1(8473):116–118. doi: 10.1016/s0140-6736(86)92259-2. [DOI] [PubMed] [Google Scholar]
- 10.Hoch W, Mcconville J, Helms S, Newsom-Davis J, Melms A, Vincent A. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nature Medicine. 2001;7(3):365–368. doi: 10.1038/85520. [DOI] [PubMed] [Google Scholar]
- 11.McConville J, Farrugia ME, Beeson D, et al. Detection and characterization of MuSK antibodies in seronegative myasthenia gravis. Annals of Neurology. 2004;55(4):580–584. doi: 10.1002/ana.20061. [DOI] [PubMed] [Google Scholar]
- 12.Fuhrer C, Sugiyama JE, Taylor RG, Hall ZW. Association of muscle-specific kinase MuSK with the acetylcholine receptor in mammalian muscle. European Molecular Biology Organization Journal. 1997;16(16):4951–4960. doi: 10.1093/emboj/16.16.4951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borges LS, Ferns M. Agrin-induced phosphorylation of the acetylcholine receptor regulates cytoskeletal anchoring and clustering. Journal of Cell Biology. 2001;153(1):1–11. doi: 10.1083/jcb.153.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zucker S, Lysik RM, Zarrabi MH, et al. Elevated plasma stromelysin levels in arthritis. Journal of Rheumatology. 1994;21(12):2329–2333. [PubMed] [Google Scholar]
- 15.Kotajima L, Aotsuka S, Fujimani M, et al. Increased levels of matrix metalloproteinase-3 in sera from patients with active lupus nephritis. Clinical and Experimental Rheumatology. 1998;16(4):409–415. [PubMed] [Google Scholar]
- 16.Christensen PB, Jensen TS, Tsiropoulos I, et al. Associated autoimmune diseases in myasthenia gravis. A population-based study. Acta Neurologica Scandinavica. 1995;91(3):192–195. doi: 10.1111/j.1600-0404.1995.tb00432.x. [DOI] [PubMed] [Google Scholar]
- 17.Sthoeger Z, Neiman A, Elbirt D, et al. High prevalence of systemic lupus erythematosus in 78 myasthenia gravis patients: a clinical and serologic study. American Journal of the Medical Sciences. 2006;331(1):4–9. doi: 10.1097/00000441-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Biró E, Szekanecz Z, Czirják L, et al. Association of systemic and thyroid autoimmune diseases. Clinical Rheumatology. 2006;25(2):240–245. doi: 10.1007/s10067-005-1165-y. [DOI] [PubMed] [Google Scholar]
- 19.Romi FR, Gilhus NE, Luckman SP. Serum matrix metalloproteinase-3 (MMP-3) levels are elevated in myasthenia gravis. Journal of Neuroimmunology. 2008;195(1-2):96–99. doi: 10.1016/j.jneuroim.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 20.Helgeland G, Petzold A, Luckman SP, Gilhus NE, Plant GT, Romi FR. Matrix metalloproteinases in Myasthenia Gravis. European Neurology. 2011;65(1):53–58. doi: 10.1159/000322737. [DOI] [PubMed] [Google Scholar]
- 21.Lien LM, Hsieh YC, Bai CH, et al. Association of blood active matrix metalloproteinase-3 with carotid plaque score from a community population in Taiwan. Atherosclerosis. 2010;212(2):595–600. doi: 10.1016/j.atherosclerosis.2010.05.040. [DOI] [PubMed] [Google Scholar]
- 22.Kanesaka T, Mori M, Hattori T, Oki T, Kuwabara S. Serum matrix metalloproteinase-3 levels correlate with disease activity in relapsing-remitting multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry. 2006;77(2):185–188. doi: 10.1136/jnnp.2005.068619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones G, Herczeg A, Ruegg MA, Lichtsteiner M, Kröger S, Brenner HR. Substrate-bound agrin induces expression of acetylcholine receptor-subunit gene in cultured mammalian muscle cells. Proceedings of the National Academy of Sciences of the United States of America. 1996;93(12):5985–5990. doi: 10.1073/pnas.93.12.5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meier T, Masciulli F, Moore C, et al. Agrin can mediate acetylcholine receptor gene expression by aggregation of muscle-derived neuregulins. Journal of Cell Biology. 1998;141(3):715–726. doi: 10.1083/jcb.141.3.715. [DOI] [PMC free article] [PubMed] [Google Scholar]


