Abstract
Background
Observational studies have reported an inverse association between dietary protein intake and blood pressure (BP). We compared the effect of soy protein, milk protein, and carbohydrate supplementation on BP among healthy adults.
Methods and Results
We conducted a randomized double-blind crossover trial with 3-intervention phases among 352 adults with prehypertension or stage-1 hypertension in New Orleans, Louisiana and Jackson, Mississippi from September 2003 to April 2008. The trial participants were assigned to take 40 grams/day of soy protein, milk protein, or carbohydrate supplementation each for 8 weeks in a random order. A 3-week washout period was implemented between the interventions. Three BPs were measured at 2 baseline and 2 termination visits during each of 3 intervention phases using a random-zero sphygmomanometer. Compared to carbohydrate controls, soy protein and milk protein supplementations were significantly associated with −2.0 mmHg (95% confidence interval −3.2 to −0.7, p=0.002) and −2.3 mmHg (−3.7 to −1.0, p=0.0007) net change in systolic BP, respectively. Diastolic BP was also reduced but this change did not reach statistical significance. There was no significant difference in the BP reductions achieved between soy or milk protein supplementation.
Conclusions
The results from this randomized controlled trial indicate that both soy and milk protein intake reduce systolic BP compared to a high glycemic index refined carbohydrate among patients with prehypertension and stage-1 hypertension. Furthermore, these findings suggest that partially replacing carbohydrate with soy or milk protein might be an important component of nutrition intervention strategies for the prevention and treatment of hypertension.
Keywords: blood pressure, diet, clinical trials, nutrition, proteins
Hypertension is an important public health challenge in the US and other countries due to its high prevalence and the concomitant increased risk of cardiovascular disease and premature death (1–3). Primary prevention of hypertension provides an attractive opportunity to interrupt and prevent the continuing costly cycle of managing hypertension and its complications (4). National guidelines identify lifestyle modifications as important elements in the prevention and treatment of hypertension and recommend this approach to the entire population (4,5). Physical activity, weight reduction, dietary sodium reduction, moderation of alcohol consumption, potassium supplementation, and consumption of a diet rich in fruits, vegetables, and low-fat dairy products and reductions in saturated and total fat have been recommended as effective approaches for the prevention of hypertension (4).
Observational epidemiological studies have reported inconsistent findings on the relationship between dietary protein intake and blood pressure (BP) (6–8). For example, the INTERMAP study, a cross-sectional epidemiological study of 4,680 persons aged 40 to 59 years from 4 countries, found a significant inverse relationship between total vegetable protein intake and BP but no significant association between total animal protein and BP (8). There are very limited data from randomized controlled trials to assess the effect of dietary protein on BP (6,9,10). In most of these trials, change in BP was not the primary outcome of interest, the sample size was small, and only a single BP measurement was obtained at the baseline and termination visits (6,7). In addition, the effects of animal protein and vegetable protein on BP have not been compared in clinical trials. We report here the results from a randomized cross-over designed trial to test the effect of soy protein and milk protein supplementations on BP in men and women aged 22 years and older with prehypertension or stage-1 hypertension.
METHODS
Study Design
The Protein and Blood Pressure (ProBP) study was a randomized, double-blinded, and placebo-controlled phase III clinical trial designed to test whether a soy protein or milk protein supplementation would reduce systolic BP compared to a complex carbohydrate. The ProBP study utilized a cross-over study design with 3 intervention phases. Following a 2-week run-in period, eligible participants were allocated to receive 40 grams of soy protein per day, 40 grams of milk protein per day, and 40 grams of complex carbohydrate (placebo) per day in a random order, each for 8 weeks. During the run-in period, study participants received 40 grams of complex carbohydrate supplement. A 3-week washout period was implemented between each intervention period. Patient recruitment and the intervention occurred between September 2003 and April 2008.
Written informed consent was obtained from each participant before the initial screening visit and before randomization. The institutional review boards at the Tulane University Health Sciences Center and the University of Mississippi Medical Center approved the study protocol.
Study Participants
The study participants were men and women aged 22 years or older who had a mean systolic BP from 120 to 159 mmHg and a diastolic BP from 80 to 95 mmHg, based on six readings at two screening visits. Persons with a systolic BP ≥160 mmHg or a diastolic BP ≥95 mmHg or that were taking antihypertensive medications were excluded. In addition, persons with a self-reported history of clinical cardiovascular disease (CVD), cancer, chronic kidney disease (CKD, or a serum creatinine ≥1.7 mg/dL for men and ≥1.5 mg/dL for women), hypercholesterolemia (or serum total cholesterol ≥240 mg/dL), diabetes (or serum glucose ≥126 mg/dL), body mass index (BMI) ≥40 kg/m2, or consumption of more than 14 drinks of alcoholic beverages per week were excluded. Persons who consumed dietary protein ≥1.63 grams/kg/day (85th percentile of dietary protein intake in the US general population) based on two 24-hour dietary recalls were also excluded. Finally, women who were pregnant or who intended to become pregnant during the study were excluded.
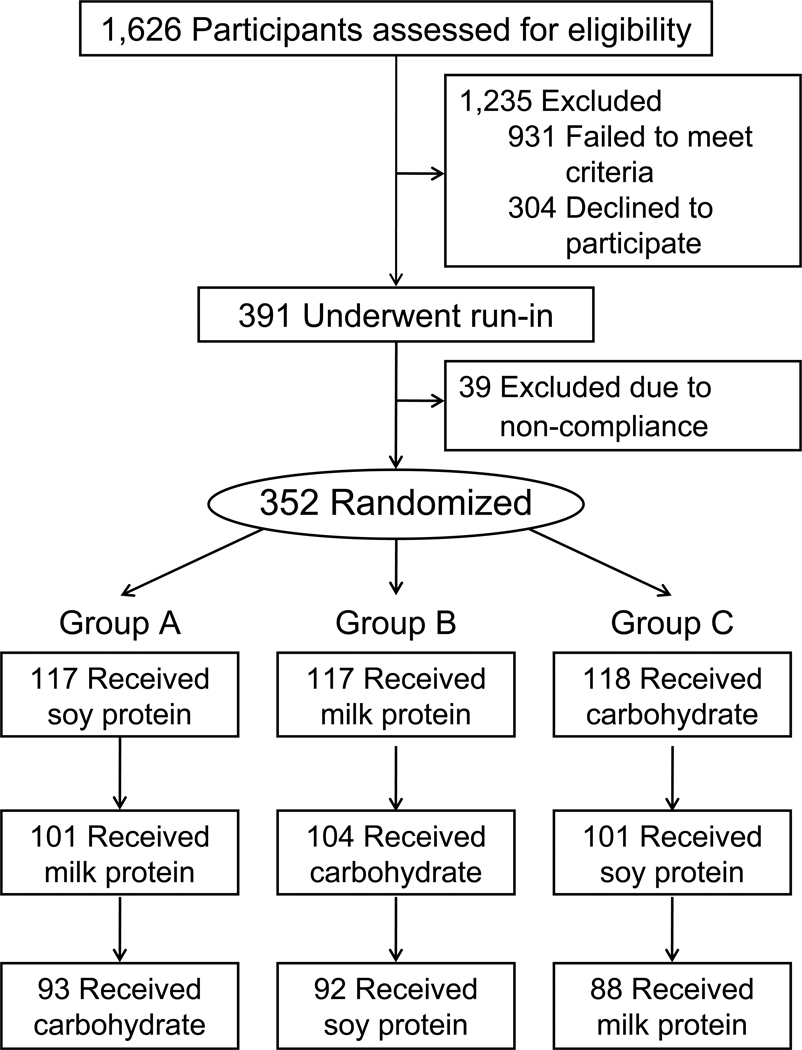
The study participants were recruited by mass mailing and work-site/community-based BP screenings in New Orleans, Louisiana and Jackson, Mississippi. We invited 1,626 persons to the study clinics for screening visits and 391 persons met all eligibility criteria (Figure 1). Of those ineligible, 27 individuals were taking antihypertensive medications, 61 had mean BP ≥160/95 mmHg, 686 had mean BP ≤120/80 mmHg, 23 had BMI ≥40 kg/m2, 96 had clinical CVD, CKD, dyslipidemia, or diabetes, 38 met other exclusion criteria, and 304 declined to participate. Among those who met inclusion criteria, 352 successfully completed a 2-week run-in (intake of ≥85% supplements) and were randomized to the intervention.
Figure 1.
Flow diagram of participants in the ProBP study.
Intervention
The study participants were randomly assigned to three sequences at a fixed 1:1:1 allocation ratio. The three groups received supplements in different orders; sequence A received 40 grams of soy protein for 8 weeks, then 40 grams of milk protein for 8 weeks, and finally 40 grams of complex carbohydrate for 8 weeks; those who were assigned to sequence B first received milk protein, then carbohydrate, and finally soy protein; and those who were assigned to sequence C first received carbohydrate, then soy protein, and finally milk protein. The randomization was stratified by clinic site, gender, and hypertension status and used a block size of 6. The randomization assignment was conducted centrally at the Data Coordinating Unit at Tulane University. After eligibility was determined, the study coordinator telephoned the Data Coordinating Unit to obtain the randomization assignment. The randomization assignment list was generated by a computer program which could only be accessed by the study data coordinator. Apart from the data coordinator, all research personnel, including study coordinators and BP technicians, and the study participants were unaware of treatment assignment.
The soy protein, milk protein, and complex carbohydrate supplements were provided for the ProBP study by Solae, LLC, St. Louis, Missouri. The contents of sodium, potassium, and calcium in soy-protein, milk-protein, and complex-carbohydrate were comparable (Table 1). Phosphorus was slightly higher in soy protein than milk protein and complex carbohydrate, while glycemic index was higher in complex carbohydrate than soy protein and milk protein. The average glycemic index of each supplement was calculated by summing up the products of carbohydrate contents (sucrose, fructose, and maltodextrin in grams, separately), multiplying their glycemic index, and then dividing by the total carbohydrate in each supplement (11). In addition, glutamic acid was slightly higher in soy protein compared to milk protein. The soy protein, milk protein, and complex carbohydrate powders looked and tasted the same and were provided to study participants in identical packets. The study participants were instructed to take the supplements twice per day; once in the morning and once in the evening in water or juice. Based on the participants’ two 24-hour dietary recalls during screening visits, individualized recommendations were given in order for participants’ total energy intake to remain consistent over the supplementation periods; for example, protein and carbohydrate supplement was recommended to partially replace breakfast, snack, or supper based on participants’ diet habits. Participants were also instructed to maintain their usual level of physical activity, alcohol intake, and dietary sodium intake. The study participants returned unconsumed packets at their follow-up clinical visits. The study coordinator counted the number of returned packets, and we used this to assess the participants’ adherence to their assigned intervention.
Table 1.
Nutrient composition of soy protein, milk protein, and complex carbohydrate supplements, per day*
| Soy protein | Milk protein | Carbohydrate | |
|---|---|---|---|
| Energy, kcal | 200 | 200 | 200 |
| Protein, g | 40 | 40 | 0.4 |
| Carbohydrate, g | 8 | 10 | 50 |
| Fat, g | 1.2 | 0.2 | 0 |
| Saturated fat, g | 0 | 0 | 0 |
| Sodium, mg | 428 | 464 | 420 |
| Potassium, mg | 480 | 420 | 380 |
| Calcium, mg | 160 | 160 | 160 |
| Phosphorus, mg | 120 | 90 | 90 |
| Glutamic acid, g | 8.6 | 7.8 | <0.1 |
| Isoflavone, mg | 84 | 0 | 0 |
| Glycemic index† | 47.7 | 67.2 | 98.9 |
Nutrient composition of soy protein, milk protein, and complex carbohydrate supplements was provided by Solae, LLC, St. Louis, Missouri.
Glycemic index was calculated by using the scale in which glucose equaled 100.
Measurements
Two baseline and two termination visits were conducted during each intervention/control phase. At each visit, three BP readings were measured using the Hawksley random-zero sphygmomanometer by trained and certified observers who were masked to group assignment. BP readings were taken from the right arm with appropriately sized cuffs after the participant had been seated quietly for 5 minutes. The participant was instructed not to eat, smoke, drink alcohol, or exercise for at least 30 minutes prior to their BP measurements. Body weight, height, and waist circumference were measured by trained staff using a standard protocol and BMI was calculated as kg/m2. Two 24-hour dietary recalls were conducted at the screening visits and at the termination visits during each intervention/control phase. Computer software (Nutrition Data System for Research) was used to conduct 24-hour dietary recalls and calculate nutrient intakes (12). An overnight timed urinary sample was collected at the baseline and termination visits to measure urinary excretion of sodium, potassium, urea nitrogen, and creatinine. Side-effects and compliance were assessed using a questionnaire, packet counts, and self-reported supplement calendar report.
Statistical Analysis
The ProBP study was designed to provide greater than 90% statistical power to detect a 2.0 mmHg reduction in systolic BP at a significance level of 0.0167 (0.05/3 for the Bonferroni correction of multiple-comparisons) using a two-tailed test. The 24-hour dietary nutrient intake, urinary excretion of sodium, potassium, urea nitrogen, and creatinine were compared among 3 phases by using repeated measures analysis of variance.
The primary outcome of interest was the net difference in change of systolic and diastolic BP among the 3 intervention phases. The change of BP was calculated as termination value minus baseline value within each intervention phase. Means of 6 BP readings taken during the 2 baseline visits and during the 2 termination visits were used for analysis. A mixed effects model was used to assess the effects of protein supplementation on the change of BP, in which participants were assumed to be random effects and treatment, sequence, and period were assumed to be estimable fixed effects. PROC MIXED of SAS version 9.2 (SAS Institute Inc., Cary, North Carolina) was used to obtain point estimates and standard errors of the treatment, sequence, and period effects and to test for differences between treatments. An autoregressive correlation matrix was used to correct within subject correlation for repeated measurements. We examined the carryover effect by testing period × treatment interaction, and the interaction was not statistically significant. The intention-to-treat principle was used for all primary analyses. If a participant withdrew or was lost to follow-up from the study, the baseline BP was used as the termination value (change in BP equal to 0) within each phase. In a secondary analysis, we repeated the analysis in only participants who fully completed the study.
RESULTS
The baseline characteristics of our study participants by randomization groups are displayed in Table 2. Mean systolic/diastolic BP was 126.7/82.4 mmHg, and the proportion with hypertension was 18.5%. Of 352 study participants, 284 (80.7%) had BPs measured at the end of the soy protein supplementation phase, 286 (81.3%) had BPs measured at the end of the milk protein supplementation phase, and 287 (81.5%) had BPs measured at the end of the carbohydrate supplementation phase (Figure 1). Based on returned packet counts and supplement calendar report, the study participants who completed the supplementation intervention consumed over 85% of their supplements during the corresponding intervention phase.
Table 2.
Baseline characteristics* of 352 trial participants
| Characteristics | Randomization groups | ||
|---|---|---|---|
| A | B | C | |
| Age, years | 48.4 (11.5) | 46.7 (10.7) | 48.1 (8.7) |
| Male, % | 59.0 | 58.1 | 57.6 |
| African-American, % | 33.3 | 32.5 | 37.3 |
| Some college education, % | 92.3 | 89.7 | 86.4 |
| Current smoking, % | 5.1 | 11.1 | 5.1 |
| Alcohol drinking, % | 39.3 | 48.7 | 48.3 |
| Physical activity ≥ 3 times/week, % | 56.9 | 55.7 | 58.8 |
| Body-mass index, kg/m2 | 29.0 (4.5) | 29.5 (4.5) | 29.3 (4.6) |
| Systolic blood pressure, mm Hg | 127.2 (9.3) | 126.7 (11.0) | 126.1 (9.7) |
| Diastolic blood pressure, mm Hg | 81.6 (5.9) | 82.4 (5.8) | 83.1 (6.2) |
Mean (standard deviation) or percentage
Table 3 presents daily dietary nutrient intake according to intervention phases from 24-hour dietary recall. On average, dietary protein intake was significantly increased in soy protein (30.5 grams/day) and milk protein (32.8 gram/day) supplementation phases compared to carbohydrate supplementation while carbohydrate intake was significantly decreased in soy protein (30.7 grams/day) and milk protein (30.6 grams/day) supplementation phases. The dietary intakes of total energy, fat, saturated fat, sodium, potassium and calcium were not significantly different among the 3 intervention/control phases. During the intervention period, urinary excretion of urea nitrogen was significantly increased in the soy protein and milk protein supplementation phases compared to carbohydrate supplementation phase (Table 3). Mean overnight urinary excretion of sodium, potassium, and creatinine were not significantly different among the 3 intervention phases. In addition, body weight, fasting plasma glucose, total cholesterol, LDL-cholesterol, and triglyceride were not significantly differed among the 3 intervention/control phases. HDL-cholesterol was significantly higher in the soy protein supplementation group (Table 4).
Table 3.
Mean (standard deviation) daily dietary nutrient intake and urinary overnight excretion of sodium, potassium and urea nitrogen according to intervention phase
| Soy protein | Milk protein | Carbohydrate | p-values | |
|---|---|---|---|---|
| Dietary intake Energy, kcal/24-hr |
2,095 (666) | 2,091 (628) | 2,057 (621) | 0.80 |
| Protein, g/24 | 108.4 (31.3) | 110.7 (33.8) | 77.9 (30.8) | <0.001 |
| Carbohydrate, g/24 | 236.4 (85.4) | 236.5 (84.4) | 267.1 (88.5) | <0.001 |
| Fat, g/24 | 78.7 (35.1) | 77.6 (31.5) | 75.3 (29.9) | 0.56 |
| Saturated fat, g/24 | 25.3 (12.7) | 25.7 (11.8) | 24.5 (11.5) | 0.56 |
| Sodium, mg/24 | 3,509 (1,285) | 3,448 (1,218) | 3,475 (1,156) | 0.88 |
| Potassium, mg/24 | 2,897 (965) | 2,852 (863) | 2,898 (964) | 0.86 |
| Calcium, mg/24 | 1,967 (614) | 1,939 (635) | 2,054 (635) | 0.16 |
| Urinary excretion Sodium, mmol/8 |
53.0 (33.2) | 57.2 (36.3) | 59.4 (37.8) | 0.24 |
| Potassium, mmol/8 | 12.6 (7.7) | 13.8 (12.0) | 14.4 (8.6) | 0.20 |
| Urea nitrogen, mg/8 | 444 (276) | 467 (259) | 357 (194) | <0.001 |
| Creatinine, mg/8 | 40.1 (30.1) | 41.0 (29.5) | 40.9 (28.4) | 0.95 |
Table 4.
Mean (95% confidence intervals) body weight, fasting plasma glucose, and serum lipids according to intervention phase
| Soy protein | Milk protein | Carbohydrate | p- values |
|
|---|---|---|---|---|
| Weight, kg | 86.2 (84.4, 88.0) |
86.6 (84.9, 88.4) |
86.7 (84.9, 88.5) |
0.12 |
| Plasma glucose, mg/dL | 98.0 (96.1, 99.9) |
96.4 (94.5, 98.3) |
96.2 (94.2, 98.1) |
0.09 |
| Total cholesterol, mg/dL | 192.2 (188.7, 195.8) |
193.7 (190.1, 197.2) |
196.2 (192.7, 199.8) |
0.09 |
| HDL-cholesterol, mg/dL | 54.1 (51.9, 56.2) |
51.4 (49.3, 53.5) |
52.5 (50.4, 54.7) |
0.03 |
| LDL-cholesterol, mg/dL | 114.4 (110.7, 118.0) |
117.7 (114.1, 121.3) |
118.0 (114.4, 121.6) |
0.09 |
| Triglyceride, mg/dL | 118.7 (110.1, 127.3) |
122.5 (114.0, 131.1) |
127.3 (118.7, 135.9) |
0.22 |
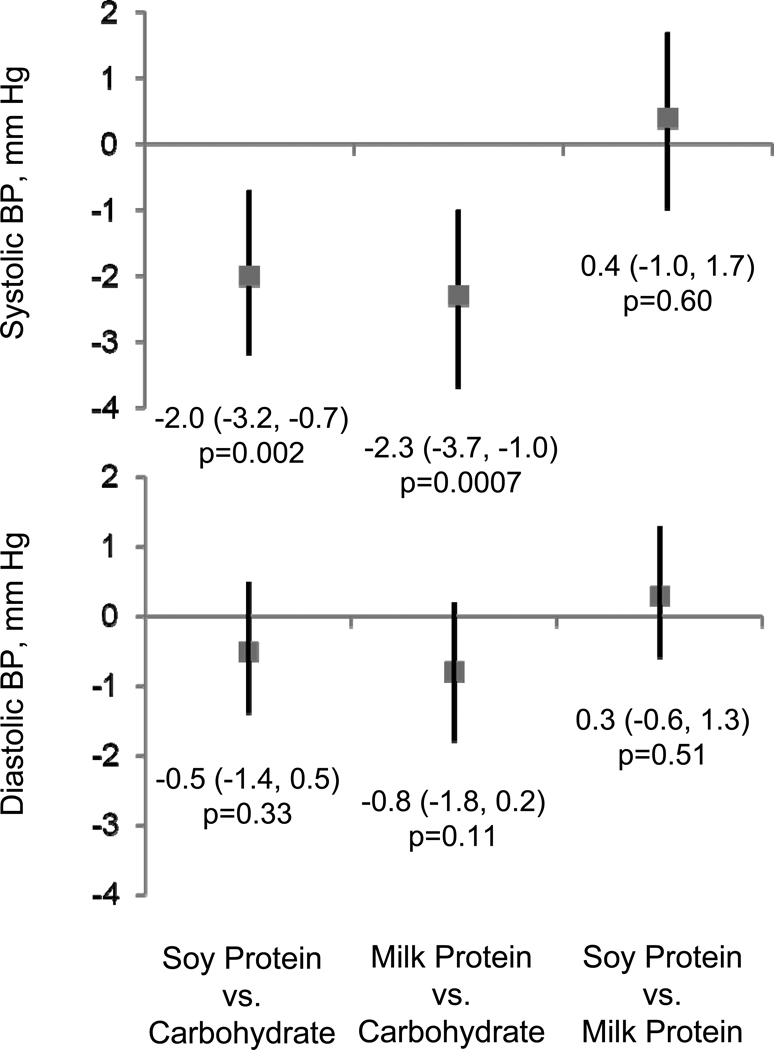
Mean systolic BP was reduced by 1.5 mmHg [95% confidence interval (CI) −2.4, −0.6; p=0.002] from baseline during soy protein supplementation and by 1.8 mmHg (95% CI −2.7, −1.0; p<0.001) from baseline during milk protein supplementation while systolic BP did not significantly change during carbohydrate supplementation (Table 5). Diastolic BP was not significantly changed during soy protein, milk protein, or carbohydrate supplementations. Compared to the carbohydrate control experience, soy protein supplementation was significantly associated with −2.0 mmHg (95% CI −3.2 to −0.7, p=0.002) net change in systolic BP and milk protein supplementation was significantly associated with −2.3 mmHg (−3.7 to −1.0, p=0.0007) net change in systolic BP (Figure 2). There was no significant difference between the BP reductions achieved with soy or milk protein supplementation.
Table 5.
Mean (95% confidence interval) systolic and diastolic blood pressure according to intervention phase
| Soy protein | Milk protein | Carbohydrate | p-values | ||
|---|---|---|---|---|---|
| Systolic BP, mm Hg | Beginning | 126.1 (125.0, 127.3) |
125.9 (124.7, 127.0) |
125.2 (124.1, 126.3) |
0.26 |
| Termination | 124.6 (123.4, 125.8) |
124.3 (123.1, 125.5) |
125.9 (124.7, 127.1) |
0.002 | |
| Differences (95% CI) |
−1.5 (−2.4, −0.6) |
−1.8 (−2.7, −1.0) |
0.5 (−0.4, 1.3) |
0.0007 | |
| Diastolic BP, mm Hg | Beginning | 81.4 (80.7, 82.2) |
81.7 80.9, 82.4) |
81.5 (80.8, 82.2) |
0.81 |
| Termination | 81.0 80.3, 81.8) |
81.1 (80.3, 81.9) |
81.8 (81.0, 82.5) |
0.13 | |
| Differences (95% CI) |
−0.2 (−0.9, 0.5) |
−0.5 (−1.2, 0.2) |
0.3 (−0.4, 0.9) |
0.27 |
Figure 2.
Net changes (95% confidence interval) in systolic and diastolic blood pressure associated with dietary protein supplementations.
In a secondary analysis limited to participants who completed the entire trial, mean systolic BP was reduced by 1.6 mmHg (95% CI −2.5, −0.7; p=0.003) from baseline during soy protein supplementation and by 1.5 mmHg (95% CI −2.4, −0.6; p=0.009) from baseline during milk protein supplementation. Systolic BP did not significantly change during carbohydrate supplementation (0.4 mmHg; 95% CI −0.6, 1.3; p=0.85). Diastolic BP did not significantly change during any of the three interventions.
Side effects were similar among the three groups. Percentages of self-reported change in appetite (28.0%, 26.1%, and 22.0%; p=0.24), stomach upset or nausea (10.1%, 9.8%, and 7.7%; p=0.55), stomach pain or burning (4.6%, 3.8%, and 4.9%; p=0.82), diarrhea (4.9%, 2.8%, and 4.2%; p=0.42), constipation (14.0%, 15.0%, and 11.9%; p=0.54), red blood in the stool or blackened stools (1.4%, 2.1%, and 1.1%; p=0.69), frequent urination (11.2%, 14.3%, and 9.8%; p=0.23), excessive gas (19.2%, 16.4%, and 15.0%; p=0.38), excessive thirst (12.2%, 10.5%, and 11.2%; p=0.79), and change in sexual drive (4.9%, 2.8%, and 3.1%; p=0.35) were similar in the soy protein, milk protein, and carbohydrate supplementation phases, respectively. Participants reported more bad taste in their mouth during soy protein supplementation (16.4%, 10.5%, and 8.0%; p=0.005), and more belching during soy protein and milk protein supplementation (16.5%, 15.7%, and 7.7%; p=0.003) compared to carbohydrate control.
DISCUSSION
This randomized controlled trial indicates that, compared to carbohydrate intake, both soy protein and milk protein supplementation reduces systolic BP among individuals with pre-hypertension or stage-1 hypertension. The effect on BP reduction is not significantly different between soy protein and milk protein. To our knowledge, this is the first randomized controlled trial aimed at directly comparing the effect of vegetable protein (soy), dairy protein (milk), and carbohydrate on BP. These study findings may have important public health and clinical implications. It was estimated that a 2 mmHg reduction in population systolic BP could lead to a 6% reduction in stroke mortality, 4% reduction in coronary heart disease mortality, and 3% reduction in all-cause mortality (4).
The effect of soy protein on serum lipids has been well documented (13). However, the effect of soy protein on BP has not been well studied. Washburn and colleagues compared the effect of 20 grams of soy protein given either in 1 dose or in 2 doses with that of 20 grams of complex carbohydrates on cardiovascular disease risk factors and menopausal symptoms among 51 women in a randomized controlled trial (14). They observed a significant reduction in diastolic, but not systolic BP in the twice-daily soy protein group only. Burke and colleagues reported that mean 24-hour ambulatory systolic and diastolic BP significantly decreased in those assigned to soy protein supplementation compared with the controls on a low-protein diet among 41 treated hypertensive patients in a randomized controlled trial (15). He and colleagues reported a significant reduction in systolic and diastolic BP among participants assigned to 40 grams of soy protein per day compared to those assigned to carbohydrate control in a randomized controlled trial of 302 Chinese participants with pre-hypertension or stage-1 hypertension (10). The current study provides further evidence that soy protein supplementation reduces BP and supports the notion that vegetable protein intake can be an important component of nutritional interventions for the prevention of hypertension (7).
A diet which is rich in low-fat dairy products has been shown to reduce BP in clinical trials (16,17). The BP lowering effect of dairy products has been hypothesized to be due to the high content of calcium and potassium in dairy products (18). To our knowledge, this is the first clinical trial to document that milk protein lowers BP in pre-hypertension and stage-1 hypertension individuals. In our study, calcium and potassium were matched among the soy protein, milk protein, and carbohydrate control groups. Therefore, the observed BP reduction in our study was due to milk protein, not the calcium or potassium in these supplements. The OmniHeart randomized trial demonstrated that partial replacement of carbohydrate with protein (about half vegetable and half animal protein) reduced BP in adults with prehypertension or stage-1 hypertension (19). In addition, an 8-week randomized parallel-design trial documented that modest substitution of carbohydrate intake with animal protein intake from lean red meat lowered BP in hypertensive persons (20).
There are inconsistent reports regarding whether vegetable or animal protein provides a better BP-lowering effect (6–8, 21–26). Some observational epidemiologic studies have identified an inverse association between dietary vegetable protein intake and BP (8,21–23). In contrast, other studies observed an inverse association between dietary animal protein intake and BP (24–26). Higher levels of dietary fiber, antioxidant vitamins, and potassium and lower levels of fat and sodium in vegetable protein rich foods might confound the relationship between vegetable protein intake and BP (6). Likewise, higher levels of potassium, calcium and magnesium in dairy products might confound the relationship between animal protein intake and BP. In this randomized controlled trial, with the exception of dietary protein and carbohydrate, other macro- and micronutrients were not changed during the 3-phase interventions with soy protein, milk protein, and carbohydrate supplementations. Our study indicates that both vegetable protein (soy) and dairy protein (milk) lower BP.
Isoflavones in soy protein have been reported to lower BP in clinical trials (27). However, this effect has been found to be inconsistent and not dose-dependent. Dietary phosphorus is high in soy protein and phosphorus has been inversely associated with BP in the INTERMAP study, a cross-sectional epidemiologic study of 4680 adults ages 40–59 from 4 countries (28). Milk protein is a rich source of angiotensin-I-converting enzyme inhibitory peptides. Animal experiments and human studies showed that these casokinins and lactokinins can significantly reduce BP (29). In addition, some amino acids might have direct BP-lowering effects (6). For example, a strong inverse association between dietary glutamic acid intake and BP has been observed in the INTERMAP study (30). Glutamic acid is a very common amino acid and constitutes 21.5% of soy protein and 19.5% of milk protein intakes. Future studies should test the effects of individual amino acids on BP.
This randomized controlled trial used a 3-phase cross-over design and BP measurements were carefully obtained during multiple visits at the baseline and termination of each phase. This design maximally minimized the influences of variations in lifestyle and diet among individual participants on BP changes during intervention. A prolonged washout period (3 weeks) and collection of baseline BP at each phase reduced the carryover effects of intervention. Limitations of this study include the relatively short duration of the intervention and the use of a high glycemic index refined carbohydrate supplement as control. Additional limitations include the lack of testing for a dose-response relationship between dietary protein intake and BP. Further studies should test the dose-response relationship between protein intake and BP. In addition,
Although a low-protein diet is widely used for patients with CKD, its efficacy has been long debated (31). The Modification of Diet in Renal Disease Study randomized CKD patient to diets containing different amounts of protein and did not find a significant difference in mean decline in glomerular filtration rate (32). A meta-analysis of 13 randomized trials indicates that the effect of dietary protein restriction on retarding the rate of renal function decline is relatively weak and inconclusive (33).
In conclusion, our study indicates that both soy and milk protein supplement reduce systolic BP compared to a high glycemic index refined carbohydrate supplement among patients with prehypertension and stage-1 hypertension. Previous studies have suggested that partial substitution of carbohydrate intake with protein intake lowers BP levels in patients with hypertension or prehypertension (19,20). Further randomized controlled trials are required to examine the effect of various dietary proteins on BP in order to recommend an overall increase in dietary protein intake as part of a nutrition intervention strategy for the prevention and treatment of hypertension.
CLINICAL PERSPECTIVE.
Observational epidemiological studies have reported an inverse association between dietary protein intake and blood pressure. We compared the effect of soy protein, milk protein, and complex carbohydrate supplementation on blood pressure in a randomized double-blind crossover trial among 352 adults with prehypertension or stage-1 hypertension. The trial participants were assigned to take 40 grams/day of soy protein, milk protein, or complex carbohydrate supplementation each for 8 weeks in a random order. A 3-week washout period was implemented between the interventions. Three blood pressure measurements were obtained at 2 baseline and 2 termination visits during each of the 3 intervention phases using a random-zero sphygmomanometer. Compared to carbohydrate controls, soy protein and milk protein supplementations were significantly associated with −2.0 mmHg (95% confidence interval −3.2 to −0.7, p=0.002) and −2.3 mmHg (−3.7 to −1.0, p=0.0007) net change in systolic blood pressure, respectively. The results from this randomized controlled trial indicate that both soy and milk protein intake reduce systolic blood pressure compared to carbohydrate intake among patients with prehypertension and stage-1 hypertension. Furthermore, these findings suggest that partially replacing carbohydrate with soy or milk protein might be an important component of nutrition intervention strategies for the prevention and treatment of hypertension.
Acknowledgements
We acknowledge the exemplary contributions of the staff of the ProBP Study at Tulane University School of Public Health and Tropical Medicine: Deborah Bujnowski, Catherine Cooke, Linda Gaines, Lisa A. Harewood, Jorge Melara, Lora R. Nolen, Lindsey Powers, Kate Reed, Kathryn E. Royse, and Ji-Hua Xu; and at University of Mississippi Medical Center: Cathy Adair, Bettie Davis, Olivia R. Henry, Maggie Ingram, Valerie McNair, Shannon M. Parham, Susie Pepper, and Mary R. Pfeifer. Each named individual was compensated for his or her contribution as part of the grant support.
Funding Sources
This work was supported by Award Number R01 HL68057 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. Study supplements were provided for the ProBP study by Solae, LLC (St. Louis, Missouri). The National Heart, Lung, and Blood Institute or Solae, LLC had no role in the design and conduct of the study; the collection, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures
None
REFERENCES
- 1.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J National High Blood Pressure Education Program Coordinating Committee. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288:1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 5.Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure: The Seventh Report of the Joint National Committee on the Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 6.Obarzanek E, Velletri PA, Cutler JA. Dietary protein and blood pressure. JAMA. 1996;275:1598–1603. doi: 10.1001/jama.1996.03530440078040. [DOI] [PubMed] [Google Scholar]
- 7.Altorf-van der Kuil W, Engberink MF, Brink EJ, van Baak MA, Bakker SJ, Navis G, van 't Veer P, Geleijnse JM. Dietary protein and blood pressure: a systematic review. PLoS One. 2010;5:e12102. doi: 10.1371/journal.pone.0012102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elliott P, Stamler J, Dyer AR, Appel L, Dennis B, Kesteloot H, Ueshima H, Okayama A, Chan Q, Garside DB, Zhou B. Association between protein intake and blood pressure: the INTERMAP Study. Arch Intern Med. 2006;166:79–87. doi: 10.1001/archinte.166.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke V, Hodgson JM, Beilin LJ, Giangiulioi N, Rogers P, Puddey IB. Dietary protein and soluble fiber reduce ambulatory blood pressure in treated hypertensives. Hypertension. 2001;38:821–826. doi: 10.1161/hy1001.092614. [DOI] [PubMed] [Google Scholar]
- 10.He J, Gu D, Wu X, Chen J, Duan X, Chen J, Whelton PK. Effect of soybean protein on blood pressure: a randomized, controlled trial. Ann Intern Med. 2005;143:1–9. doi: 10.7326/0003-4819-143-1-200507050-00004. [DOI] [PubMed] [Google Scholar]
- 11.Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr. 2002;76:5–56. doi: 10.1093/ajcn/76.1.5. [DOI] [PubMed] [Google Scholar]
- 12.The Minnesota Nutrition Data System. University of Minnesota: NCC; 2002. [Google Scholar]
- 13.Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J. A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol. 2006;98:633–640. doi: 10.1016/j.amjcard.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 14.Washburn S, Burke GL, Morgan T, Anthony M. Effect of soy protein supplementation on serum lipoproteins, blood pressure, and menopausal symptoms in perimenopausal women. Menopause. 1999;6:7–13. [PubMed] [Google Scholar]
- 15.Burke V, Hodgson JM, Beilin LJ, Giangiulioi N, Rogers P, Puddey IB. Dietary protein and soluble fiber reduce ambulatory blood pressure in treated hypertensives. Hypertension. 2001;38:821–826. doi: 10.1161/hy1001.092614. [DOI] [PubMed] [Google Scholar]
- 16.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 17.van Meijl LE, Mensink RP. Low-fat dairy consumption reduces systolic blood pressure, but does not improve other metabolic risk parameters in overweight and obese subjects. Nutr Metab Cardiovasc Dis. 2010 Feb 11; doi: 10.1016/j.numecd.2009.10.008. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Kris-Etherton PM, Grieger JA, Hilpert KF, West SG. Milk products, dietary patterns and blood pressure management. J Am Coll Nutr. 2009;28 Suppl 1:103S–119S. doi: 10.1080/07315724.2009.10719804. [DOI] [PubMed] [Google Scholar]
- 19.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–2464. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 20.Hodgson JM, Burke V, Beilin LJ, Puddey IB. Partial substitution of carbohydrate intake with protein intake from lean red meat lowers blood pressure in hypertensive persons. Am J Clin Nutr. 2006;83:780–787. doi: 10.1093/ajcn/83.4.780. [DOI] [PubMed] [Google Scholar]
- 21.He J, Klag MJ, Whelton PK, Chen JY, Qian MC, He GQ. Dietary macronutrients and blood pressure in Southwest China. J Hypertension. 1995;13:1267–1274. doi: 10.1097/00004872-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Stamler J, Liu K, Ruth KJ, Pryer J, Greenland P. Eight-year blood pressure change in middle-aged men: relationship to multiple nutrients. Hypertension. 2002;39:1000–1006. doi: 10.1161/01.hyp.0000016178.80811.d9. [DOI] [PubMed] [Google Scholar]
- 23.Wang YF, Yancy WS, Jr, Yu D, Champagne C, Appel LJ, Lin PH. The relationship between dietary protein intake and blood pressure: results from the PREMIER study. J Hum Hypertens. 2008;22:745–754. doi: 10.1038/jhh.2008.64. [DOI] [PubMed] [Google Scholar]
- 24.Umesawa M, Sato S, Imano H, Kitamura A, Shimamoto T, Yamagishi K, Tanigawa T, Iso H. Relations between protein intake and blood pressure in Japanese men and women: the Circulatory Risk in Communities Study (CIRCS) Am J Clin Nutr. 2009;90:377–384. doi: 10.3945/ajcn.2008.27109. [DOI] [PubMed] [Google Scholar]
- 25.Liu L, Ikeda K, Yamori Y. Inverse relationship between urinary markers of animal protein intake and blood pressure in Chinese: results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) Study. Int J Epidemiol. 2002;31:227–233. doi: 10.1093/ije/31.1.227. [DOI] [PubMed] [Google Scholar]
- 26.Zhou B, Zhang X, Zhu A, Zhao L, Zhu S, Ruan L, Zhu L, Liang S. The relationship of dietary animal protein and electrolytes to blood pressure: a study on three Chinese populations. Int J Epidemiol. 1994;23:716–722. doi: 10.1093/ije/23.4.716. [DOI] [PubMed] [Google Scholar]
- 27.Taku K, Lin N, Cai D, Hu J, Zhao X, Zhang Y, Wang P, Melby MK, Hooper L, Kurzer MS, Mizuno S, Ishimi Y, Watanabe S. Effects of soy isoflavone extract supplements on blood pressure in adult humans: systematic review and meta-analysis of randomized placebo-controlled trials. J Hypertens. 2010;28:1971–1982. doi: 10.1097/HJH.0b013e32833c6edb. [DOI] [PubMed] [Google Scholar]
- 28.Elliott P, Kesteloot H, Appel LJ, Dyer AR, Ueshima H, Chan Q, Brown IJ, Zhao L, Stamler J. INTERMAP Cooperative Research Group. Dietary phosphorus and blood pressure: international study of macro- and micro-nutrients and blood pressure. Hypertension. 2008;51:669–675. doi: 10.1161/HYPERTENSIONAHA.107.103747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.FitzGerald RJ, Murray BA, Walsh DJ. Hypotensive peptides from milk proteins. J Nutr. 2004;134:980S–988S. doi: 10.1093/jn/134.4.980S. [DOI] [PubMed] [Google Scholar]
- 30.Stamler J, Brown IJ, Daviglus ML, Chan Q, Kesteloot H, Ueshima H, Zhao L, Elliott P. INTERMAP Research Group. Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP Study (International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure) Circulation. 2009;120:221–228. doi: 10.1161/CIRCULATIONAHA.108.839241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martinez-Maldonado M, Sattin RD. Rate of progression of renal disease and low-protein diet. Am J Kidney Dis. 1998;31:1048–1049. doi: 10.1053/ajkd.1998.v31.pm9631853. [DOI] [PubMed] [Google Scholar]
- 32.Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, Striker G Modification of Diet in Renal Disease Study Group. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N Engl J Med. 1994;330:877–884. doi: 10.1056/NEJM199403313301301. [DOI] [PubMed] [Google Scholar]
- 33.Kasiske BL, Lakatus JDA, Ma JZ, Louis T. A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am J Kidney Dis. 1998;31:954–961. doi: 10.1053/ajkd.1998.v31.pm9631839. [DOI] [PubMed] [Google Scholar]