Abstract
Aim
The aim of this study was to determine whether oral, tactile/kinaesthetic (T/K), or combined (oral + T/K) interventions enhance oral feeding performance and whether combined (oral + T/K) interventions have an additive/synergistic effect.
Method
Seventy-five preterm infants (mean gestational age 29wk; standard error of the mean [SEM] 0.3wk; mean birthweight 1340.3g; SEM 52.5g; 49 males and 26 females) were randomly assigned to one of three intervention groups or a control group. The oral group received sensorimotor input to the oral structures, the T/K group received sensorimotor input to the trunk and limbs, and the combined (oral + T/K) group received both. The outcomes were time from introduction of nipple feeding to independent oral feeding (days), proficiency (intake in the first 5min, %), volume transfer (%), rate of transfer (ml/min), volume loss (%), and length of hospital stay (days).
Results
Infants in the three intervention groups achieved independent oral feeding 9 to 10 days earlier than those in the control group (p<0.001; effect size 1.9–2.1). Proficiency (p≤0.002; effect size 0.7–1.4) at the time of one to two and three to five oral feedings per day, volume transfer (p≤0.001; effect size 0.8–1.1) at one to two, three to five, and six to eight oral feedings per day, and overall rate of transfer (p≤0.018; effect size 0.8–1.1) were greater, and overall volume losses were less (p≤0.007; effect size 0.9–1.1), than in the control group (p≤0.042). The combined (oral + T/K) group attained independent oral feeding at a significantly younger postmenstrual age than controls (p=0.020) and had clinically greater proficiency than the T/K group (p=0.020; effect size 0.7) and oral group (p=0.109; effect size 0.5). Length of hospital stay was not significantly different between groups (p=0.792; effect size 0.02–0.3).
Interpretation
Oral and T/K interventions accelerated the transition from introduction to independent oral feeding and enhanced oral feeding skills. T/K has beneficial effects beyond the specific targeted system. The combined sensorimotor intervention led to an additive/synergistic effect for proficiency, further benefiting this population.
Advances in newborn intensive care have dramatically improved the survival of infants born preterm; however, many present with oral feeding difficulties.1 These difficulties are of concern to health professionals because they often impede the transition to independent oral feeding and thus delay hospital discharge,2 negatively affect mother-infant interactions,3 and potentially lead to childhood feeding disorders.4 Such consequences point to the need for efficacious early interventions to enhance preterm infants' oral feeding performance.5
Sensorimotor intervention is used to improve oral feeding. It is described as the provision of developmentally appropriate sensory inputs including oral, tactile, kinaesthetic, vestibular, and auditory to facilitate the development of existing rudimentary skills and to prevent/minimize the deleterious environmental effects.6–8 Oral sensorimotor interventions have been the major focus of studies because they provide direct, targeted input to the oral structures involved in feeding.9 Studies have shown that oral sensorimotor intervention for at least 15 minutes per day for 10 days improves oral feeding performance in preterm infants.9–12 However, oral feeding is a complex multisystem process that involves both the oral and other systems, including cardiorespiratory, gastrointestinal, and neurological.1 It is conceivable, therefore, that sensorimotor input targeting non-oral systems, such as trunk and limbs, may have distributed effects that go beyond the target system and improve oral feeding performance.6 Empirical evidence for the effectiveness of trunk and limb stimulation is limited. Two studies found that tactile/kinaesthetic (T/K) intervention, consisting of input to the trunk and limbs, for 15 minutes a day for 10 days, increased the volume of milk ingested by preterm infants.13,14 However, it was not specified whether the volume intake was via tube or oral feeding13 and there was no randomization.14 Further studies are needed to clearly establish the effect of T/K intervention on oral feeding performance. In addition, combined sensorimotor interventions may have an additive/synergistic effect. This notion is partially supported by White-Traut et al.,15 who demonstrated that a combined auditory, tactile, and vestibular stimulation accelerates the transition to complete oral feeding in preterm infants. However, individual contributions to additive/synergistic effects could not be determined because only combined stimulation was provided. A prospective study in which single and combined sensorimotor interventions are compared would be more conclusive.
Therefore, the following hypotheses are proposed: (1) preterm infants who receive oral, T/K, or combined (oral + T/K) interventions before the introduction of nipple feeding will demonstrate improved oral feeding performance over control infants. Specifically, compared with control infants, they will attain independent oral feeding sooner and demonstrate greater proficiency, volume transfer, rate of transfer, and less volume loss; and (2) preterm infants who receive a combined intervention will demonstrate better oral feeding performance than those who receive oral or a T/K intervention alone.
METHOD
Participants
All participants were born between 26 weeks and 32 weeks gestational age, were an appropriate size for their gestational age, received all feedings by tube, and had no congenital anomalies or chronic medical complications, including bronchopulmonary dysplasia, intraventricular haemorrhages III or IV, periventricular leucomalacia, or necrotizing enterocolitis. They were enrolled from the nursery at Texas Children's Hospital (Houston).
The sample size estimate was derived from the average time from introduction of nipple feeding to attainment of independent oral feeding, which at this hospital is 18 days (SD 7).10 We calculated that a sample size of 64 infants was required to detect a decrease of 7 days (SD 1) with a type 1 error of 0.05 and a power of 0.80. The actual number enrolled was 30% higher (n=84) to allow for infants who may develop bronchopulmonary dysplasia, intraventricular haemorrhages (III/IV), periventricular leucomalacia, or necrotizing enterocolitis. Of the 84 participants enrolled, four were transferred to another hospital; in addition, four developed necrotizing enterocolitis and one was found to have a congenital heart defect, conditions that were diagnosed before the onset of the study. Thus, a total of 75 infants (mean age 29wk [SD 0.3]) completed the study. All participants had statistically similar baseline characteristics (Table I). The research protocol was approved by the Institutional Review Board for Human Subjects of Baylor College of Medicine and affiliated hospitals.
Table I.
Baseline characteristics and covariate distribution of preterm infants in the four groups
| O (n=19) | T/K (n=18) | O+T/K (n=18) | Control (n=20) | pa | |
|---|---|---|---|---|---|
| Gestational age | |||||
| 26–29wk | 10 | 8 | 11 | 9 | 0.266b |
| 30–32wk | 9 | 10 | 7 | 11 | – |
| Sex | |||||
| Male | 12 | 11 | 10 | 16 | 0.057b |
| Female | 7 | 7 | 8 | 4 | – |
| Ethnicity | |||||
| African American | 8 | 3 | 4 | 5 | 0.010b |
| White | 6 | 4 | 9 | 3 | – |
| Hispanic | 5 | 11 | 5 | 12 | – |
| Severity of illness (NBRS) | 2.6 (0.3) | 2.4 (0.3) | 2.3 (0.2) | 2.5 (0.2) | 0.916 |
| Number of infants breastfeeding | 4 | 8 | 5 | 6 | 0.241b |
| Number of infants with co-interventions | 10 | 15 | 13 | 14 | 0.117b |
| Number of parental visits | 18.6 (2.6) | 21.8 (2.1) | 21.6 (1.4) | 24.3 (1.5) | 0.577 |
Data presented as means (standard error of mean) or number of participants.
Analysis of variance (ANOVA) unless otherwise indicated.
Fisher's exact test. O, oral; T/K, tactile/kinaesthetic; NBRS, Nursery Neurobiologic Risk Score.
Procedures
After parents provided informed consent, infants were randomized to an oral, T/K, combined, or control group using a stratified blocked randomization. Stratification by gestational age (26–29wk vs 30–32wk) and time (every 3mo) was done to ensure equal gestational age and individual neonatologist distribution between each group.
The oral intervention consisted of twice-daily stroking of the cheeks, lips, gums, and tongue for 12 minutes and non-nutritive sucking for 3 minutes.10 The specific protocol can be found in Fucile et al.10 The T/K intervention consisted of twice-daily stroking of the head, neck, back, arms, and legs for 10 minutes and passive range of motion to the limbs for 5 minutes. The specific protocol can be found in Field et al.16 The combined intervention involved 15 minutes of oral or T/K, as above, each once a day, in random order. The controlled intervention consisted of the researcher placing her hands in the incubator but not touching the infant for 15 minutes, twice daily.
In addition to standard nursery care, infants received their assigned intervention, which was started 48 hours after discontinuation of nasal continuous positive airway pressure, and was administered in two 15-minute sessions/day for 10 days during a 14-day period.10,16 The sessions were provided 30 minutes before tube feedings, with a minimum 3-hour interval between each session. Interventions were provided to clinically stable infants as per nurses' recommendations. They were not provided if infants had had an increased occurrence of apnoea/bradycardia or oxygen desaturation within the previous 24 hours, or if there was a major disruption 30 minutes before the session (e.g. ophthalmological examination). Interventions were stopped if infants had an episode of apnoea, bradycardia, or oxygen desaturation, or demonstrated fussing (splaying arms/legs), crying, or spitting-up behaviours during the session. All interventions were administered by the same researcher (SF). A screen was placed around the isolette to blind parents and caregivers to group assignment.
Participants were monitored from study onset to hospital discharge (July 2006 to July 2007). Management of oral feeding was left to the discretion of the attending neonatologist, and nurses administered the feedings with no assistance, for example without chin or cheek support. All infants were fed with the same type of nipple. Time to attainment of independent oral feeding was monitored on the day that infants achieved eight successful oral feedings a day for 2 consecutive days using chart review. The secondary outcomes were recorded once when infants were taking one to two, three to five, and six to eight oral feedings a day. The three monitored oral feedings were scheduled so that they did not interfere with parents' opportunity to breast or bottle-feed their infants.
Outcomes
Time to attainment of independent oral feeding (the number of days from introduction to eight successful oral feedings/day for two consecutive days) was the primary outcome of testing because it is a hospital discharge criterion. The secondary outcomes were proficiency (volume of milk taken during the first 5min as a percentage of the total); volume transfer (volume consumed as a percentage of the prescribed volume); rate of transfer (volume of milk consumed relative to the duration of the oral feeding session [ml/min]); volume loss (volume of milk spilled from the lips as a percentage of the total milk transferred, determined by subtracting the weight of a bib before from the weight after the feeding session); and length of hospital stay (days).
The following covariates were recorded: severity of illness using the nursery Neurobiological Risk Score,17 number of infants receiving breast feeding and co-interventions (occupational, physical, and/or speech therapy), and number of parental visits. At each feeding session, we also recorded postmenstrual age (PMA) and weight and, at 5-minute intervals, behavioural state using a three-point scale (1=asleep, 2=drowsy/awake, 3=fussy/crying), as well as episodes of apnoea, bradycardia, and/or oxygen desaturation. Data on the primary outcome were also gathered from the charts of 10 additional infants to assess for any potential Hawthorne effect (Hawthorne group).
Statistical analyses
A two-way analysis of variance and repeated measures analysis of variance, with gestational age and group as factors and sex, number of breast-fed infants, and parental visits as covariates, were used to compare the effect of the interventions on the primary and secondary outcomes respectively. Post-hoc Tukey tests were applied for all significant group, time, or group by time significant effects. Significance was defined at the 0.05 level. Effect sizes were calculated for all feeding parameters using Cohen's definition. Effect sizes of 0.2, 0.5, and 0.8 were considered small, moderate, and large respectively.18 Analyses were done with the Statistical Program for Social Sciences software version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Infants in the three intervention groups achieved independent oral feeding significantly sooner than those in the control group (Table II; p<0.001; effect size: O, 1.9; T/K, 1.8; oral + T/K, 2.1). The combined group attained independent oral feeding at a significantly younger PMA than the control group (p=0.020). There was no significant difference in time to achieve independent oral feeding among the three intervention groups (p≥0.336; effect size ≤0.3), nor between the Hawthorne (19.8d [SD 2.5]) and control groups (20.7d [SD 1.5]; p=0.458; effect size 0.1).
Table II.
Number of days to transition from introduction to independent oral feeding
| Group | Introduction of oral feeding | Independent oral feeding | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PMA | DOL | Weight | PMA | DOL | Weight | Number of days of independent oral feeding | Effect size vs control | Effect size vs O+T/K | |
| 0 (n=19) | 34.2 (0.4) | 33.8 (3.8) | 2001.3 (63.3) | 35.9 (0.4) | 44.7 (3.7) | 2345.8 (67.1) | 11.1 (0.8)b | 1.9 | 0.3 |
| T/K (n=18) | 34.1 (0.4) | 36.6 (5.2) | 2065.6 (108.7) | 35.4 (0.8) | 46.5 (5.1) | 2442.0 (103.4) | 11.4 (0.8)b | 1.8 | 0.3 |
| O+T/K (n=18) | 33.2 (0.3) | 30.4 (3.2) | 1952.1 (48.7) | 34.7 (0.3)b | 40.1 (3.0) | 2305.7 (60.0) | 10.0 (0.8)b | 2.1 | – |
| Control (n=20) | 33.8 (0.3) | 30.4 (3.7) | 1885.2 (61.5) | 36.2 (0.4) | 49.3 (4.8) | 2465.8 (87.3) | 20.7 (1.5) | – | – |
| a p | 0.197 | 0.659 | 0.331 | 0.020 | 0.487 | 0.454 | 0.000 | – | – |
Data presented as means (standard error of mean).
Two-way analysis of variance (ANOVA), post-hoc Tukey tests vs control.
p≤0.05. PMA, postmenstrual age (weeks); DOL, days of life; O+T/K, oral and tactile/kinaesthetic.
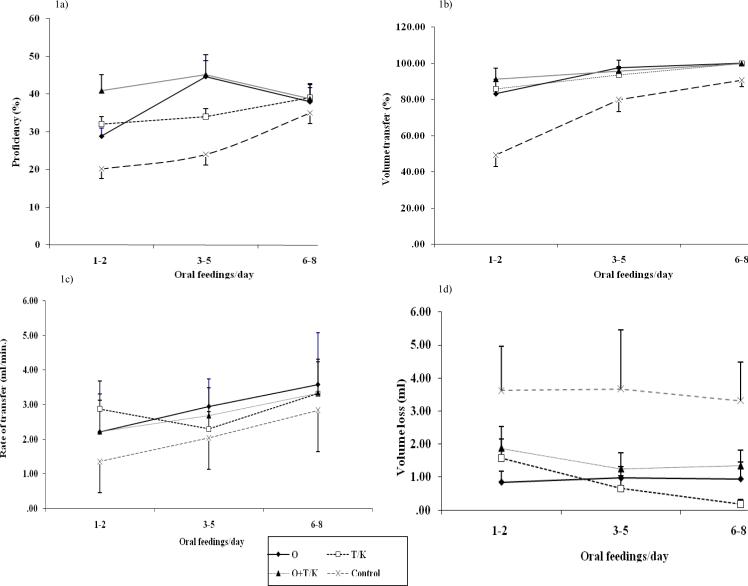
Proficiency analysis (Fig. 1a) indicated a significant group effect (F3,69=7.738; p<0.001), time effect (F2,138=6.602; p=0.005), and group × time interaction (F6,141=2.836; p=0.029). Note that in some cases a feeding session was not recorded because of a scheduling conflict, which accounts for the missing values indicated in the F-statistics. Post-hoc group tests indicated that all three intervention groups had a significantly greater proficiency than the control group (p≤0.002; effect size: oral group, 0.7; T/K group, 1.2; oral + T/K, 1.4). The combined group had a significantly greater proficiency than the T/K group (p=0.020; effect size 0.7) and a clinically greater proficiency than the oral group (p=0.109; effect size 0.5). Post-hoc time tests indicated that proficiency increased significantly from one to two, to three to five oral feedings a day (p≤0.002; effect size 0.4), but not from three to five, to six to eight oral feedings a day (p=0.747; 3–5 0.1). Post-hoc interaction tests indicated that the three intervention groups had a significantly greater proficiency than the control group at one to two oral feedings a day (p≤0.022; effect size for the oral group=0.7, for the T/K group=1.2, and for the combined group=1.4), the oral and combined groups had significantly greater proficiency at three to five oral feedings a day than the control group (p≤0.000; effect size: oral group, 1.2; T/K group, 1.0; combined group, 1.6), and there was no longer any significant difference among the four groups at six to eight oral feedings a day (p>0.83; effect size ≤0.3).
Figure 1.
(a) Proficiency (%) at the three oral feeding sessions. Data presented as means±(standard error of the mean, SEM). At one to two oral feedings a day, the three intervention groups had significantly greater proficiency than controls, and at three to five oral feedings a day the O and combined (O+T/K) groups had significantly greater proficiency than controls (p≤0.022, ES≥0.7). (b) Volume transfer (%) at the three oral feeding sessions. Data presented as means±(SEM). At one to two and six to eight oral feedings a day, the three intervention groups had significantly greater volume transfer than controls (p≤0.040, ES O≥0.7), and at three to five oral feedings a day only the O group demonstrated marginally greater volume transfer than controls (p=0.07, ES≥0.6). (c) Rate of transfer (ml/min) at the three oral feeding sessions. Data presented as means±(SEM). All three interventions had significantly faster rate of transfer than controls (p≤0.018, ES≥1.0). (d) Volume loss (%) at the three oral feeding sessions. Data presented as means±(SEM). All three interventions had significantly less volume loss than controls (p≤0.007, ES≥1.0).
For volume transfer (Fig. 1b) there was a significant group effect (F3,69=17.018; p<0.001), time effect (F2,138=30.668; p<0.001), and group × time interaction (F6,141=4.879; p<0.001). Post-hoc group tests indicated that the three intervention groups had greater volume transfer than the control group (p≤0.001; effect size: oral group, 1.1; T/K group, 1.0; combined group, 0.8). There was no significant difference between any of the three intervention groups (p>0.481; effect size ≤0.2). Post-hoc time tests indicated that volume transfer increased significantly from one to two, to three to five oral feedings a day (p<0.001; effect size 1.0) and from three to five, to six to eight oral feedings a day (p≤0.044; effect size 0.5). Post-hoc interaction tests indicated that the three intervention groups had significantly greater volume transfer than the control group at one to two oral feedings a day (p<0.003; effect size for the oral group=1.3, for the T/K group=1.5, and for the combined group=1.9) and at six to eight oral feedings a day (p≤0.040; effect size for all intervention groups=0.7), but at three to five oral feedings a day only the oral group demonstrated marginally greater volume transfer than the control group (p=0.07; effect size for the oral group=0.9, for the T/K group=0.6, and for the combined group=0.8).
The rate of transfer analysis (Fig. 1c) indicated that there was a significant group effect (F3,69=4.634; p=0.009) and time effect (F2,138=17.385; p<0.001) only. Post-hoc group tests indicated that rate of transfer was higher in all three intervention groups than in the control group (p≤0.018; effect size for the oral group=1.1, for the T/K group=1.0, and for the combined group=0.8). There was no significant difference between the three intervention groups (p≤0.332; effect size ≤0.2). Post-hoc time tests indicated that the rate of transfer increased significantly from one to two, to three to five oral feedings a day (p<0.001; effect size=0.3) and from three to five, to six to eight oral feedings a day (p≤0.001; effect size 0.6).
For volume loss (Fig. 1d) there was a significant group effect only (F3,69 =4.567; p=0.001). Post-hoc tests indicated that volume loss was significantly lower in all three intervention groups than in the control group (p≤0.007; effect size: oral group, 1.1; T/K group, 1.0; combined group, 0.9). There was no significant difference between the three intervention groups (p≥0.305; effect size ≤0.2).
Of 1100 administered interventions, 13 (1.1%) were stopped because of apnoea, bradycardia, or oxygen desaturation episodes, all of which resolved spontaneously (Table III). There were no significant differences in PMA, days of life, or weight among the four groups (p≥0.072) either before or after the interventions.
Table III.
Characteristics of preterm infants at the start and end of the sensorimotor interventions and occurrence of physiological signs and behavioural events of distress during the sensorimotor interventions
| 0 (n=19) | T/K (n=18) | O+T/K (n=18) | Control (n=20) | pa | |
|---|---|---|---|---|---|
| Start intervention | |||||
| PMA (weeks) | 32.7 (0.3) | 32.1 (0.3) | 31.7 (0.4) | 32.5 (0.3) | 0.079 |
| DOL (days) | 23.4 (3.8) | 24.3 (4.1) | 19.6 (3.5) | 23.0 (4.1) | 0.851 |
| Weight (g) | 1676.3 (64.5) | 1673.4 (55.7) | 1615.8 (67.7) | 1709.5 (63.6) | 0.742 |
| End intervention | |||||
| PMA (wk) | 34.3 (0.3) | 33.6 (0.2) | 33.1 (0.2) | 34.0 (0.1) | 0.072 |
| DOL (d) | 33.8 (3.8) | 35.1 (2.8) | 30.3 (2.0) | 33.6 (2.0) | 0.854 |
| Weight (g) | 1987.4 (66.9) | 1994.2 (49.2) | 1905.0 (42.6) | 2000.0 (38.9) | 0.749 |
| Episodes of apnoea, bradycardia, or oxygen desaturation | 4 | 4 | 5 | 0 | 0.205 |
| Episodes of fussy/crying/spitting up | 0 | 0 | 0 | 0 | 1.000 |
Data presented as means (standard error of mean) or number of participants.
Analysis of variance (ANOVA) unless otherwise indicated.
Fisher's exact test. O, oral; T/K, tactile/kinaesthetic; PMA, postmenstrual age; DOL, days of life.
There was no significant difference in length of hospital stay between the oral (53.4d [SD 4.3]; effect size 0.1), T/K (55.7d [SD 3.7]; effect size 0.02), combined (50.3d [SD 1.9]; effect size 0.3), and control groups (55.3d [SD 2.6]; p=0.792).
DISCUSSION
The results support our first hypothesis that preterm infants who received an oral, T/K, or combined sensorimotor intervention attained independent oral feeding sooner than infants who received no such intervention. All four groups were introduced to oral feeding at similar PMA, days of life, and weight, decreasing the possibility that infants in the intervention groups achieved independent oral feeding faster because they were more mature than controls. Although race/ethnicity appears to be unequally distributed among groups, to our knowledge there is no evidence that this factor influences oral feeding skills. The lack of a Hawthorne effect demonstrates that our results were not influenced by any change in routine care. These findings suggest that the lower number of days to transition from tube to independent oral feeding in the three intervention groups resulted from specific targeted sensorimotor input that enhanced the function of one or more of the systems involved in the oral feeding process.
To identify these underlying mechanisms, proficiency, volume transfer, rate of transfer, and volume loss were monitored because they are indicators of specific oral feeding skills. Proficiency reflects infants' intrinsic nutritive sucking skills because it is monitored during the first 5 minutes of the feeding when fatigue is presumed to be minimal.19 Volume transfer and rate of transfer tap into infants' overall nutritive sucking skills, suck–swallow–respiration coordination, and endurance.19 Volume loss reflects infants' perioral musculature function.
Compared with no intervention, oral intervention improved proficiency at the stage of one to two and three to five oral feedings a day, volume transfer at all three oral feeding stages, and overall rate of transfer, and resulted in less overall volume loss. The oral intervention probably facilitated the neuromotor development of the oral musculoskeletal system. Indeed, we previously demonstrated that 15 minutes of oral intervention improves the nutritive sucking pattern/stages and sucking pressure at the one to two oral feedings a day.20 Several studies have corroborated these findings9,11,12 However, in contrast, Bragelien et al.21 and Boiron et al.22 did not find any improvement in oral feeding progression, possibly because of differences in protocol administration. The oral intervention in the present study may also have enhanced suck–swallow–respiration coordination by providing a patterned input to the brainstem central pattern generator circuitry, promoting its neuronal development.23
The T/K intervention improved proficiency at one to two oral feedings a day, volume transfer at one to two and six to eight oral feedings a day, and overall rate of transfer, and resulted in less volume loss than in the control group. The T/K intervention probably facilitated motor development of the trunk and limbs, which may have contributed to the advancement of oral feeding performance. Proper trunk control and postural alignment provide a stable base for sucking, swallowing, and respiration and thereby may facilitate their function and coordination.24 The effect of oral and T/K intervention on suck–swallow–respiration coordination is currently being investigated. These findings demonstrate that sensorimotor interventions had systemic effects that went beyond the specific target of input, which led to improved oral feeding performance.25
The combined intervention enhanced proficiency at one to two and three to five oral feedings a day, volume transfer at one to two and six to eight oral feedings a day, and overall rate of transfer, and also led to less overall volume loss than that experienced by control infants. In addition, the PMA of infants in the combined group was lower, that is they were less mature than infants in the control group, when they attained independent oral feeding, supporting the notion that oral feeding is an integrated multiple systems process that may be enhanced through early oral and non-oral sensorimotor input. Moreover, the combined intervention led to greater proficiency than the T/K intervention and a moderate effect size compared with the oral intervention, which partially supports our second hypothesis. However, the combined intervention did not lead to additive/synergistic effects for volume transfer, rate of transfer, and volume loss, which may be related to the neural integrity and maturation of controls associated with the suck–swallow–respiration cycle, which may be the step limiting progression to oral feeding.23 Another possibility may be inferior endurance owing to the shorter duration of each intervention in the combined group, which received only 15 rather than 30 minutes of oral + T/K intervention each day. Perhaps if both interventions had been administered simultaneously, additive/synergistic effects might have been seen in these outcomes.
The increase in proficiency, volume transfer, and rate of transfer noted over time reflects the infants' improved musculoskeletal function and strength, enhanced neuronal maturation of the critical networks involved in the sucking–swallowing–respiration cycle, and endurance. We also observed that the effects on proficiency and volume transfer changed over time. Specifically, proficiency was clinically better in the three intervention groups than in the control group at one to two and three to five oral feedings a day, but there was no longer a significant group difference at six to eight oral feedings a day. In the case of volume transfer, this was higher in the three intervention groups than in the control group at all three monitored oral feeding stages. The finding that the control group caught up with the intervention groups in terms of proficiency, but not volume transfer, by the time of achieving six to eight oral feedings a day suggests that control infants attained the same level of nutritive sucking as those in the intervention groups, but at a much slower pace and only during the first 5 minutes of feeding. This may be due to their immaturity and/or decreased endurance.
The oral, T/K, and combined sensorimotor interventions improved oral feeding performance. However, they did not lead to improved weight gain following the sensorimotor intervention period. This finding probably reflects the stringent clinical practices at this hospital to ensure adequate daily weight gain of these infants, whereby a neonatal nutritionist reviews the medical charts daily and prescribes the necessary volume to achieve a minimum daily weight gain.
Contrary to other studies,11,16 the three interventions did not decrease the number of days of hospitalization owing to the lack of a specific protocol for discharge planning in our study, which is a limitation. Another limitation relates to the advancement of oral feeding, which was left to the attending neonatologist's discretion. The implementation of guidelines for both oral feeding advancement and a discharge protocol may have allowed for better discrimination between groups.
CONCLUSION
Oral and non-oral sensorimotor interventions provided singly or in combination shortened the transition time to independent oral feeding in preterm infants. These findings demonstrate that sensorimotor interventions have beneficial effects beyond their specific site of input. The combined sensorimotor intervention had an additive/synergistic beneficial effect on proficiency, further benefiting this vulnerable population.
What this paper adds.
Oral and non-oral sensorimotor interventions (i.e. oral and tactile/kinaesthetic) accelerated the transition from introduction of oral feeding to independent oral feeding and enhanced oral feeding skills.
Sensorimotor interventions (tactile/kinaesthetic) had beneficial effects beyond the specific targeted system.
Combined (oral + tactile/kinaesthetic) sensorimotor intervention had an additive/synergistic effect on oral feeding performance over single sensorimotor interventions
ACKNOWLEDGEMENTS
The authors would like to thank the nurses at Texas Children's Hospital for their assistance in the data collection, and E O Smith for statistical expertise. This study was supported by the Fonds de la Recherche en Santé du Québec and National Institute of Child Health and Human Development grant R01-HD 044469. Contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
ABBREVIATIONS
- PMA
Postmenstrual age
- T/K
Tactile/kinaesthetic
REFERENCES
- 1.Burklow KA, McGrath AM, Valerius KS, Rudolph C. Relationship between feeding difficulties, medical complexity, and gestational age. Nutr Clin Pract. 2002;17:373–8. doi: 10.1177/0115426502017006373. [DOI] [PubMed] [Google Scholar]
- 2.Schanler RJ, Shulman RJ, Lau C, Smith EO, Heitkemper MM. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics. 1999;103:434–9. doi: 10.1542/peds.103.2.434. [DOI] [PubMed] [Google Scholar]
- 3.Silberstein D, Geva R, Feldman R, et al. The transition to oral feeding in low-risk premature infants: relation to infant neurobehavioral functioning and mother-infant feeding interaction. Early Hum Dev. 2009;85:157–62. doi: 10.1016/j.earlhumdev.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Rommel N, De Meyer AM, Feenstra L, Veereman-Wauters G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J Pediatr Gastroenterol Nutr. 2003;37:75–84. doi: 10.1097/00005176-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Blauw-Hospers CH, Hadders-Algra M. A systematic review of the effects of early intervention on motor development. Dev Med Child Neurol. 2005;47:421–32. doi: 10.1017/s0012162205000824. [DOI] [PubMed] [Google Scholar]
- 6.Dieter JN, Emory EK. Supplemental stimulation of premature infants: a treatment model. J Pediatr Psychol. 1997;22:281–95. doi: 10.1093/jpepsy/22.3.281. [DOI] [PubMed] [Google Scholar]
- 7.Liaw JJ. Tactile stimulation and preterm infants. J Perinat Neonatal Nurs. 2000;14:84–103. doi: 10.1097/00005237-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Korner AF. Infant stimulation. Issues of theory and research. Clin Perinatol. 1990;17:173–95. [PubMed] [Google Scholar]
- 9.Lessen BS. Effect of oral stimulation on feeding progression in preterm infants. Adv Neonatal Care. 2009;9:187. doi: 10.1097/ANC.0b013e3182115a2a. [DOI] [PubMed] [Google Scholar]
- 10.Fucile S, Gisel E, Lau C. Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. J Pediatr. 2002;141:230–6. doi: 10.1067/mpd.2002.125731. [DOI] [PubMed] [Google Scholar]
- 11.Rocha AD, Moreira ME, Pimenta HP, Ramos JR, Lucena SL. A randomized study of the efficacy of sensory–motor-oral stimulation and non-nutritive sucking in very low birthweight infant. Early Hum Dev. 2007;83:385–8. doi: 10.1016/j.earlhumdev.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Hwang YS, Vergara E, Lin CH, Coster WJ, Bigsby R, Tsai WH. Effects of prefeeding oral stimulation on feeding performance of preterm infants. [accessed 3 September 2010];Indian J Pediatr. doi: 10.1007/s12098-010-0001-9. [Internet]. Available from: http://www.springerlink.com/content/n6w3751330444452/ [DOI] [PubMed] [Google Scholar]
- 13.Rausch PB. Effects of tactile and kinesthetic stimulation on premature infants. J Obstet Gynecol Neonatal Nurs. 1981;10:34–7. doi: 10.1111/j.1552-6909.1981.tb00629.x. [DOI] [PubMed] [Google Scholar]
- 14.White JL, Labarba RC. The effects of tactile and kinesthetic stimulation on neonatal development in the premature infant. Dev Psychobiol. 1976;9:569–77. doi: 10.1002/dev.420090610. [DOI] [PubMed] [Google Scholar]
- 15.White-Traut RC, Nelson MN, Silvestri JM, et al. Effect of auditory, tactile, visual, and vestibular intervention on length of stay, alertness, and feeding progression in preterm infants. Dev Med Child Neurol. 2002;44:91–7. doi: 10.1017/s0012162201001736. [DOI] [PubMed] [Google Scholar]
- 16.Field TM, Schanberg SM, Scafidi F, et al. Tactile/kinesthetic stimulation effects on preterm neonates. Pediatrics. 1986;77:654–8. [PubMed] [Google Scholar]
- 17.Brazy JE, Eckerman CO, Oehler JM, Goldstein RF, O'Rand AM. Nursery Neurobiologic Risk Score: important factor in predicting outcome in very low birth weight infants. J Pediatr. 1991;118:783–92. doi: 10.1016/s0022-3476(05)80047-2. [DOI] [PubMed] [Google Scholar]
- 18.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd edn. Prentice Hall; Upper Saddle River, NJ: 2003. [Google Scholar]
- 19.Lau C, Sheena HR, Shulman RJ, Schanler RJ. Oral feeding in low birth weight infants. J Pediatr. 1997;130:561–9. doi: 10.1016/s0022-3476(97)70240-3. [DOI] [PubMed] [Google Scholar]
- 20.Fucile S, Gisel EG, Lau C. Effect of an oral stimulation program on sucking skill maturation of preterm infants. Dev Med Child Neurol. 2005;47:158–62. doi: 10.1017/s0012162205000290. [DOI] [PubMed] [Google Scholar]
- 21.Bragelien R, Rokke Q, Markestad T. Stimulation of sucking and swallowing to promote oral feeding in premature infants. Acta Pediatr. 2007;96:1430–2. doi: 10.1111/j.1651-2227.2007.00448.x. [DOI] [PubMed] [Google Scholar]
- 22.Boiron M, Da Nobrega L, Roux S, Henrot A, Saliba E. Effects of oral stimulation and oral support on non-nutritive sucking and feeding performance in preterm infants. Dev Med Child Neurol. 2007;49:439–44. doi: 10.1111/j.1469-8749.2007.00439.x. [DOI] [PubMed] [Google Scholar]
- 23.Barlow SM. Oral and respiratory control for preterm feeding. Curr Opin Otolaryngol Head Neck Surg. 2009;17:179–86. doi: 10.1097/MOO.0b013e32832b36fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redstone F, West JF. The importance of postural control for feeding. Pediatr Nurs. 2004;30:97–100. [PubMed] [Google Scholar]
- 25.McFarland DH, Tremblay P. Clinical implications of cross–system interactions. Semin Speech Lang. 2006;27:300–9. doi: 10.1055/s-2006-955119. [DOI] [PubMed] [Google Scholar]