Abstract
Context
The familiality of borderline personality disorder (BPD) and its sectors of psychopathology are incompletely understood.
Objectives
To assess the familial aggregation of BPD and its 4 major sectors (affective, interpersonal, behavioral, and cognitive) and test whether the relationship of the familial and nonfamilial associations among these sectors can be accounted for by a latent BPD construct.
Design
Family study, with direct interviews of probands and relatives.
Setting
A psychiatric hospital (McLean Hospital) and the Boston-area community.
Participants
A total of 368 probands (132 with BPD, 134 without BPD, and 102 with major depressive disorder) and 885 siblings and parents of probands.
Main Assessments
The Diagnostic Interview for DSM-IV Personality Disorders and the Revised Diagnostic Interview for Borderlines (DIB-R) were used to assess borderline psychopathology, and the Structured Clinical Interview for DSM-IV was used to assess major depressive disorder.
Results
Borderline personality disorder meeting both DSM-IV and DIB-R criteria showed substantial familial aggregation for BPD in individuals with a family member with BPD vs those without a family member with BPD, using proband-relative pairs (risk ratio, 2.9; 95% confidence interval, 1.5–5.5) as well as using all pairs of family members (3.9; 1.7–9.0). All 4 sectors of BPD psychopathology aggregated significantly in families, using both DSM-IV and DIB-R definitions (correlation of traits among all pairs of family members ranged from 0.07 to 0.27), with the affective and interpersonal sectors showing the highest levels; however, the level of familial aggregation of BPD was higher than that of the individual sectors. The relationship among the sectors was best explained by a common pathway model in which the sectors represent manifestations of a latent BPD construct.
Conclusions
Familial factors contribute to BPD and its sectors of psychopathology. Borderline personality disorder may arise from a unitary liability that finds expression in its sectors of psychopathology.
Borderline personality disorder (BPD) is a common psychiatric disorder, estimated to affect 2% to 6% of adults in the United States,1–3 including approximately 19% of adult psychiatric inpatients and 11% of adult psychiatric outpatients.4 Borderline personality disorder is associated with high levels of mental health service use3–5 and often serious psychosocial impairment,3,6 rendering it a major public health problem.
Surprisingly, little is known about the role of familial factors (including both environmental factors in common to members of the same family and genetic factors) in the causation of BPD, particularly in contrast to the extensive literature of family and twin studies7–12 available for many other psychiatric disorders. Many studies13–21 have found an elevated risk of BPD in the relatives of probands with BPD, but these studies contain methodologic limitations (including sampling methods likely to produce bias, reliance on information from probands to determine a diagnosis in relatives rather than direct interviews of relatives, assessments of relatives who are aware of proband status, and small sample sizes) that render their results difficult to interpret.22 Twin studies, which are used to determine proportions of variance in a given entity resulting from additive genetic, common environmental (shared among family members), and unique environmental (nonshared among family members) influences, have reported heritability estimates of 37% to 69% for BPD23–26 and have found no evidence of significant effects of common family environment. Twin studies, however, have been limited by small numbers of individuals with full BPD (all studies), use of clinical probands only,25 and reliance on dimensional self-report measures rather than diagnostic interviews.23,24,26
Interest has focused not only on the diagnosis of BPD as a unitary entity but also on the sectors of psychopathology of BPD and on how they are related to the diagnosis of BPD. The present study examined the 4 sectors represented within the DSM-IV criteria and in the Revised Diagnostic Interview for Borderlines (DIB-R) criteria27 for BPD, ie, affective, interpersonal, behavioral, and cognitive. The first 3 of these sectors have been identified in factor analytic studies of BPD criteria28–33 and of personality traits in BPD samples.34 All of these have been proposed as “psychobiological dispositions” with neurobiological correlates.35–39 The fourth sector, cognitive, has been less extensively explored but has emerged in 2 recent factor studies.40,41
To our knowledge, no family studies have directly examined the familial aggregation of the sectors of BPD psychopathology, but 2 studies42,43 have reported that levels of affective, behavioral, and interpersonal sectors are elevated in the relatives of probands with BPD. Moreover, twin studies44–47 have reported heritability estimates for affective instability, cognitive, and impulsivity traits of 31% to 49%.
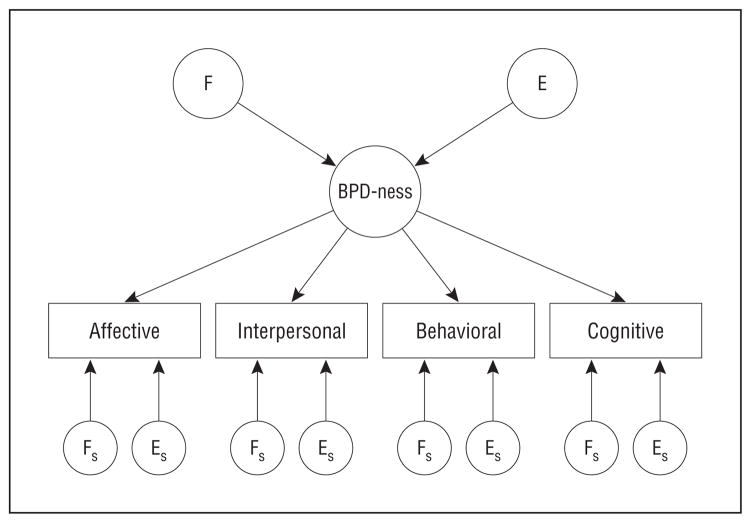
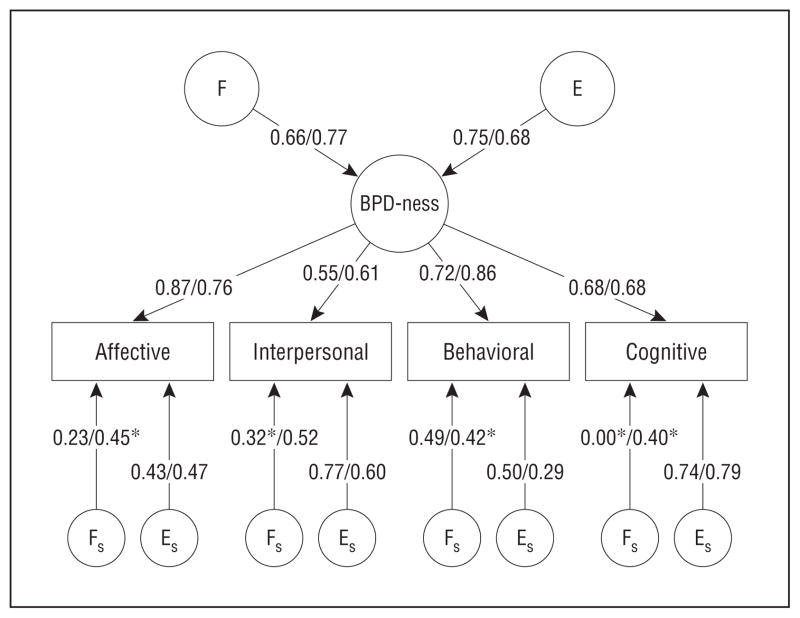
How are these postulated sectors related to the diagnosis of BPD? One hypothesis, derived from the historical psychoanalytic conceptualization of BPD, is that there is an underlying latent psychopathological construct that gives rise to these various sectors of BPD—a latent construct of “BPD-ness,” so to speak. This hypothesis corresponds to what is termed a common pathway model,48,49 as depicted in Figure 1, which is a causal diagram or directed acyclic graph that encodes the dependencies and independencies among variables and represents a non-parametric generalization of path diagrams.50,51
Figure 1.
Common pathway model in which genetic and environmental factors influence a single latent factor for liability to borderline personality disorder (BPD-ness) that accounts for the covariance among the 4 sectors. E indicatesunique environmental factor for BPD-ness; ES, unique environmental factor specific for a given sector; F, familial factor for BPD-ness; FS, familial factor specific for a given sector. Observed variables are in rectangles and latent variables are in circles.
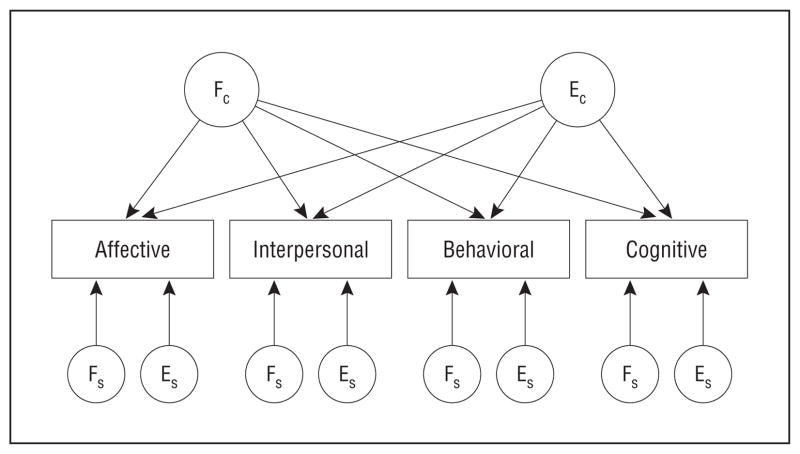
A second, alternative hypothesis suggests that there is no unitary BPD-ness linking the sectors, but rather that BPD is inherently heterogeneous.52,53 This hypothesis proposes that the sectors are the primary psychopathological entities and that BPD is diagnosed simply when psychopathology in these sectors rises to a certain level of severity and co-occurs. This hypothesis corresponds to an “independent pathway” model,48,49 whereby the familial and nonfamilial factors causing the association of these sectors within individuals and between family members are the result of a combination of common familial factors and common nonfamilial factors but without a latent construct of BPD-ness (see directed acyclic graph in Figure 2).
Figure 2.
Independent pathway model, which allows the covariance structure to differ among the 4 sectors; specifically, this model allows the 4 sector variables to load independently onto the latent genetic and environmental factors. ECindicates latent unique environmental factor common to all sectors; ES, unique environmental factor specific for a given sector; FC, familial factor common to all sectors; FS, familial factor specific for a given sector. Observed variables are in rectangles and latent variables are in circles.
Although family and twin studies cannot discriminate definitively between these 2 alternative causal models, one can examine the relative fit of each model to family study data to determine which model provides the best explanation for the association between BPD and its sectors. Two twin studies44,54 addressing this issue found that the relationship between the sectors of BPD assessed by the Personality Assessment Inventory–Borderline Features scale55 and 4 scales from the Dimensional Assessment of Personality Pathology–Basic Questionnaire56,57 were better explained by a common pathway model than by an independent pathway model, with an estimated heritability of the latent BPD construct of 51%44 and 60%.54 To further examine the familial aggregation of BPD and its sectors, we conducted a family study, using masked interviews of relatives. Our primary goal was to test the hypothesis that BPD aggregates in families; our secondary goals were to test the hypothesis that the 4 sectors of psychopathology aggregate in families individually and to explore whether the relationship between familial and nonfamilial associations among these sectors was better accounted for by a common pathway or independent pathway model.
METHODS
PARTICIPANTS
Three groups of female probands, aged 18 to 35 years, were recruited: (1) with BPD according to both DSM-IV and DIB-R criteria; (2) without a lifetime diagnosis of BPD; and (3) with a lifetime diagnosis of major depressive disorder (MDD), who may or may not have had a lifetime diagnosis of BPD (this last group, recruited for a separately planned analysis of coaggregation, was included because it provides, with suitable weighting, data applicable to the present analysis, as described in the “Statistical Analysis” subsection). For groups 1 and 3, we recruited from McLean Hospital inpatient units and partial hospital program and, for all groups, we recruited from the community, using advertisements on posters, radio, and the Internet. Regardless of the media selected, we sought participants with use of the following language. For the BPD group, we asked, “Are your relationships very painful and difficult? Are you often distrustful of others? Are you extremely moody? Do you frequently feel out of control?” For the non-BPD group, we sought individuals for “a family study of health and personality.” For the MDD group, we recruited individuals with “a history of major depression.” We screened respondents by telephone and determined whether they presumptively (later confirmed by interview) met criteria sought by the advertisement (ie, for the BPD advertisement, a diagnosis of BPD; for the general [non-BPD] advertisement, no BPD; and for the MDD advertisement, a diagnosis of MDD). All potential probands were also required to have at least 2 parents or siblings who were willing to participate and be without a lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar I disorder, or any organic condition that could cause serious psychiatric symptoms or mental retardation.
This study was approved by the McLean Hospital Institutional Review Board. Written informed consent was obtained from the participants after all aspects of the study were explained thoroughly and before the administration of any study procedures.
PROCEDURES
Clinically experienced raters administered 4 semistructured interviews to all participants (probands and relatives): (1) the Background Information Schedule,58 which assesses demographic information, psychosocial functioning, and history of psychiatric treatment; (2) the Structured Clinical Interview for DSM-IV Axis I Disorders59; (3) the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV),60 which assesses each criterion for all Axis II disorders on a 3-point scale (0, not present; 1, present but of uncertain clinical significance; and 2, present and clinically significant); and (4) the DIB-R,61 which yields dimensional scores in each of 4 sectors of BPD and a total score. Table 1 lists the components from the DIPD-IV and DIB-R used to assess the sectors of borderline psychopathology. Interviewers for relatives were masked to information about probands.
Table 1.
Traits Within Sectors of Psychopathology for DSM-IV and DIB-R Borderline Personality Disorder
| Sector | DSM-IV Traits | DIB-R Traits |
|---|---|---|
| Affective | Anger Affective instability Emptiness |
Depression Anger Loneliness/emptiness Anxiety Hopelessness/helplessness/worthlessness |
| Interpersonal | Intense, unstable relations Abandonment fears |
Abandonment/engulfment/annihilation fears Intolerance of aloneness Counter dependency Stormy relations Undue dependency/masochism Manipulation/devaluation/sadism Demandingness/entitlement Treatment regressions Counter transference difficulties |
| Behavioral | Self-harm/suicidality 2 Other forms of impulsivity |
Self-harm Suicide threats/acts Promiscuity Substance abuse Other impulsive patterns |
| Cognitive | Dissociation and brief paranoid episodes Self-image distortions |
Odd thinking/unusual perceptual experiences Nondelusional paranoid experiences Quasi-psychotic experiences |
Abbreviation: DIB-R, Revised Diagnostic Interview for Borderlines.
RELIABILITY OF ASSESSMENTS OF BORDERLINE PSYCHOPATHOLOGY
In a series of 18 interviews, the interrater reliability for the borderline diagnosis (as assessed by κ) was 1.0 for both the DIPD-IV and DIB-R. The interrater reliability (as assessed by the intra-class coefficient) for the DIPD-IV–defined sectors was 0.97 for affective, 1.0 for interpersonal, 0.76 for behavioral, and 0.98 for cognitive; interrater reliability for the DIB-R–defined sectors was 0.99 for affective, 0.99 for interpersonal, 0.97 for behavioral, and 0.93 for cognitive.
STATISTICAL ANALYSIS
To compare demographic characteristics of probands and relatives between the proband groups, we used linear regression for continuous variables and the Fisher exact test for categorical variables.
For analyses related to familial aggregation and structural equation models, we used information from all probands and relatives from the 3 proband groups that we corrected for the effects of oversampling probands with BPD and MDD compared with their representation in the source population by weighting participants proportionally to the inverse probability of their selection. Calculation of the selection probabilities requires knowing the prevalence of BPD from the source population from which our sample was drawn. To calculate the prevalence of BPD, we used a method developed for estimating prevalence from relatives of case and control probands62 that has been used in other studies.51,63–65 This method assumes that families are singly evaluated, that proband selection is independent of relative characteristics, and that family size is not associated with the proportion of family members with BPD. To calculate the prevalence of MDD (to weight families selected by the presence of a proband with MDD), we used the prevalence of MDD from the weighted sample of probands and relatives from the BPD and non-BPD proband groups. The effect of these procedures was to create, by assigning weights based on inverse probability of selection to all probands and relatives, a pseudosample that is representative of families from the underlying source population.
To evaluate the familial aggregation of BPD, we estimated the risk ratio and the tetrachoric correlation coefficient using proband-relative pairs and all pairs of family members (except mother-father pairs, thereby restricting the analysis to first-degree relatives). For the risk ratio, we fitted a generalized linear model with a log-link function and a binary distribution.51 For the analysis involving proband-relative pairs (the traditional proband predictive model for familial aggregation66), the outcome was the presence of BPD in a relative and the predictor was BPD in the corresponding proband. For the analysis involving all pairs of family members (which uses all available information in the data set), the outcome was the presence of BPD in one family member and the predictor was BPD in another family member.
To evaluate the familial aggregation of sectors, we estimated the Pearson product moment correlation coefficient using proband-relative pairs and all pairs of family members (except mother-father pairs).
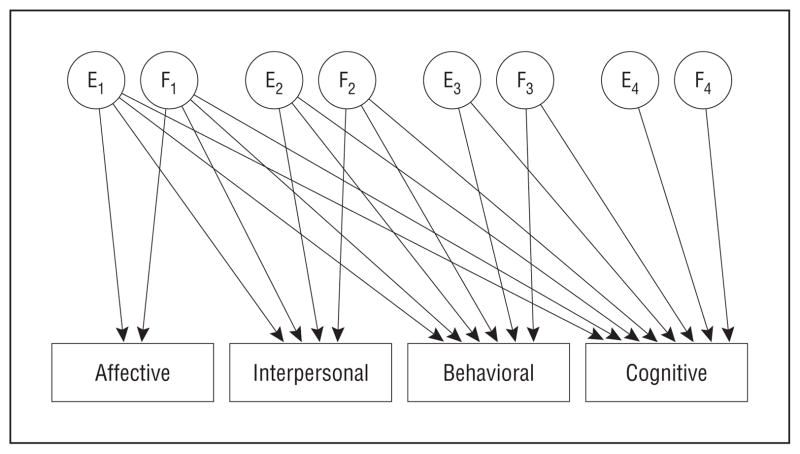
To examine the structure of the familial and nonfamilial associations of the 4 sectors of BPD within individuals and between family members, we evaluated 3 models: a Cholesky decomposition (Figure 3), which represents a fully saturated model against which to compare subsequent models; an independent pathway model (Figure 2); and a common pathway model (Figure 1). We evaluated separate sets of models based on sectors assessed by DSM-IV criteria and by DIB-R criteria. We fitted structural equation models to the models depicted by the directed acyclic graphs, which assume that the variables have a multivariate normal distribution and are additive in their effects on each other (ie, no interactions).
Figure 3.
Cholesky decomposition model, which decomposes the covariance among the 4 sectors into familial and environmental influences and imposes no underlying structure on the covariance. E1–E4 indicate unique environmental factors; F1–F4, familial factors. Observed variables are in rectangles and latent variables are in circles.
We evaluated the relative fit of models using the χ2 difference test67,68 based on the Yuan-Bentler T2* statistic,69 which has a χ2 distribution and adjusts for the nonindependence of observations within families (primary method for nested models), and the difference in Akaike information criterion (AIC)70 (primary method for nonnested models) and Bayesian information criterion (BIC)71 based on the T2* statistic. Note that the fit of the Cholesky and independent pathways models changes slightly, depending on the relative contribution of additive genetic and common family environment to the influence of familial factors. We fitted these models under the assumption that there was no contribution of common family environment because twin studies44,47,72 have found the effects of the common family environment to be negligible. We also performed a sensitivity analysis in which we assumed that the contribution of additive genetics effects and common environmental effects were equal; the relative fits for the models were virtually unchanged and were qualitatively the same (ie, produced the same best-fitting models).
All the analyses are based on the assumption that, other than the effects related to the outcome variables, there are no important differences in measures of familial aggregation between pairs of relatives. We performed analyses of interactions, using regression models for familial aggregation of BPD and of the sectors to test this assumption regarding 4 potential sources of differences: (1) sampling source (patient vs community), (2) type of relative pair (mother-daughter vs father-daughter vs sister-sister vs sister-brother; there were insufficient data to evaluate father-son and brother-brother pairs), (3) generational effects (parent-child vs sibling-sibling pairs), and (4) sex effects (female-female vs female-male; there were insufficient data to evaluate male-male pairs). The only statistically significant interactions were of generation and type with the cognitive sector by DSM-IV criteria (both the result of decreased correlation among parent-child pairs), but significant interactions were not found with the cognitive sector by DIB-R criteria; given the large number of tests performed and the lack of consistency of these potential effects, they are likely explainable by chance (however, if they were true associations, they would be consistent with either common family environmental factors or dominant genetic effects).
We performed statistical analyses using commercial software (Stata 9.2; StataCorp LP, College Station, Texas) with a separate product for estimating correlation coefficients and fitting structural equation modeling (Mplus, version 6).68 All analyses, except for demographic characteristics, adjusted standard errors for the correlation of observations within families. We set the 2-tailed α level at .05.
The analyses reported herein used data from interviewed relatives because information about noninterviewed relatives provided by the interviewed relatives is likely to be of poorer quality than information obtained from direct interviews and because information given by informants may depend on the informants’ outcome and thus may introduce bias.73,74
RESULTS
CHARACTERISTICS OF PARTICIPANTS
Data were collected between August 22, 2005, and August 12, 2009. We interviewed 368 probands: the BPD group included 132 participants (61 patients [46.2%] and 71 individuals [53.8%] from the community); the non-BPD group was composed of 134 residents, all of whom were from the community; and the MDD group included 102 participants (6 patients [5.9%] and 96 individuals [94.1%] from the community). We interviewed 885 parents and siblings of the probands: 314 in the BPD group, 337 in the non-BPD group, and 234 in the MDD group. Demographic characteristics of the participants are presented in Table 2. The only significant differences between groups were in the mean age of probands, with the 3 groups showing statistically significant but scientifically unimportant differences of 1.3 to 3.1 years.
Table 2.
Demographic Characteristics of Probands and Relatives by Proband Group
| Characteristic | BPD | Non-BPD | MDD | P Valuea | |
|---|---|---|---|---|---|
| Probands | |||||
| Total, No. | 132 | 134 | 102 |
|
<.001b |
| Age, mean (SD), y | 23.9 (4.6) | 25.7 (4.7) | 27.0 (5.1) | ||
| Female sex, No. (%) | 132 (100) | 134 (100) | 102 (100) | ||
| Race/ethnicity, No. (%) | |||||
| White | 91 (68.9) | 86 (64.2) | 64 (62.8) |
|
.58 |
| African American | 15 (11.4) | 24 (17.9) | 19 (18.6) | ||
| Hispanic | 23 (17.4) | 22 (16.4) | 15 (14.7) | ||
| Other | 3 (2.3) | 2 (1.5) | 4 (3.9) | ||
| Socioeconomic status, mean (SD)c | 2.6 (1.2) | 2.6 (1.0) | 2.7 (1.2) | .85 | |
|
| |||||
| Relatives | |||||
| Total, No. | 314 | 337 | 234 |
|
.39 |
| Age, mean (SD), y | 41.5 (14.8) | 40.5 (15.5) | 41.4 (16.1) | ||
| Relationship to proband, No. (%) | |||||
| Mother | 113 (35.9) | 109 (32.3) | 84 (35.9) |
|
.13 |
| Father | 73 (23.2) | 56 (16.6) | 38 (16.2) | ||
| Sister | 78 (24.8) | 110 (32.6) | 73 (31.2) | ||
| Brother | 50 (15.9) | 62 (18.4) | 39 (16.7) | ||
Abbreviations: BPD, borderline personality disorder; MDD, major depressive disorder.
P value for test of no differences between 3 groups (linear regression for continuous variables; Fisher exact test for categorical variables).
Pairwise contrasts: BPD vs non-BPD (P = .003), BPD vs MDD (P < .001), and non-BPD vs MDD (P = .03).
Determined according to the Hollingshead-Redlich 5-point scale (1 indicates the highest socioeconomic status and 5, the lowest).75
FAMILIAL AGGREGATION OF BPD AND SECTORS OF PSYCHOPATHOLOGY
The prevalence of BPD was 14.1% in relatives of probands with BPD and 4.9% in relatives of probands without BPD. Borderline personality disorder aggregated strongly and significantly in families in analyses using proband-relative pairs (risk ratio=2.9; r=0.28) and using all pairs of family members (risk ratio=3.9; r=0.37) (Table 3).
Table 3.
Familial Aggregation of Borderline Personality Disorder
| Analysis | Risk Ratioa |
ρb |
||
|---|---|---|---|---|
| Estimate (95% CI) | P Value | Estimate (95% CI) | P Value | |
| Proband-relative pairs | 2.9 (1.5–5.5) | <.001 | 0.28 (0.11–0.44) | <.001 |
| All pairsc | 3.9 (1.7–9.0) | <.001 | 0.37 (0.11–0.64) | .006 |
Abbreviation: CI, confidence interval.
For proband-relative pairs: risk of borderline personality disorder (BPD) diagnosis in relative of proband with BPD (by both DSM-IV and Revised Diagnostic Interview for Borderlines [DIB-R] criteria) vs risk of diagnosis in relative of proband without BPD (by DSM-IV plus DIB-R criteria), using entire sample weighted by inverse probability of selection; for all pairs, risk of BPD in a relative of a family member with BPD vs risk of BPD in a relative of a family member without BPD diagnosis.
Tetrachoric correlation coefficient.
Pairs of first-degree relatives (excludes mother-father pairs).
All 4 of the sectors (assessed either by DSM-IV or DIB-R criteria) showed statistically significant levels of familial aggregation, with the correlations ranging from 0.09 to 0.30 for proband-relative pairs and from 0.07 to 0.27 for all pairs of family members (Table 4). The sectors assessed by DIB-R criteria had higher correlations than those assessed by DSM-IV criteria as measured by the DIPD-IV, and the affective and interpersonal sectors exhibited higher correlations than did the behavioral and cognitive sectors. The correlation within individuals between the DSM-IV and DIB-R measurements of the sectors was 0.74 for affective, 0.74 for interpersonal, 0.78 for behavioral, and 0.45 for cognitive.
Table 4.
Familial Aggregation of Sectors of Borderline Personality Disorder Psychopathology
| Sector | Proband-Relative Pairs
|
All Pairs of Family Membersa |
||
|---|---|---|---|---|
|
rb |
rb |
|||
| Estimate (95% CI) | P Value | Estimate (95% CI) | P | |
| DSM-IV | ||||
| Affective | 0.13 (0.04–0.22) | .004 | 0.18 (0.08–0.27) | <.001 |
| Interpersonal | 0.22 (0.12–0.32) | <.001 | 0.20 (0.11–0.30) | <.001 |
| Behavioral | 0.09 (0.01–0.17) | .03 | 0.09 (0.02–0.15) | .01 |
| Cognitive | 0.13 (0.03–0.23) | .02 | 0.07 (0.00–0.15) | .049 |
| DIB-R | ||||
| Affective | 0.19 (0.09–0.29) | <.001 | 0.21 (0.13–0.29) | <.001 |
| Interpersonal | 0.30 (0.23–0.37) | <.001 | 0.27 (0.17–0.36) | <.001 |
| Behavioral | 0.14 (0.08–0.22) | .003 | 0.13 (0.05–0.21) | .002 |
| Cognitive | 0.17 (0.09–0.26) | <.001 | 0.18 (0.10–0.26) | <.001 |
Abbreviations: CI, confidence interval; DIB-R, Revised Diagnostic Interview for Borderlines.
Pairs of first-degree relatives (excludes mother-father pairs).
Pearson product moment correlation coefficient.
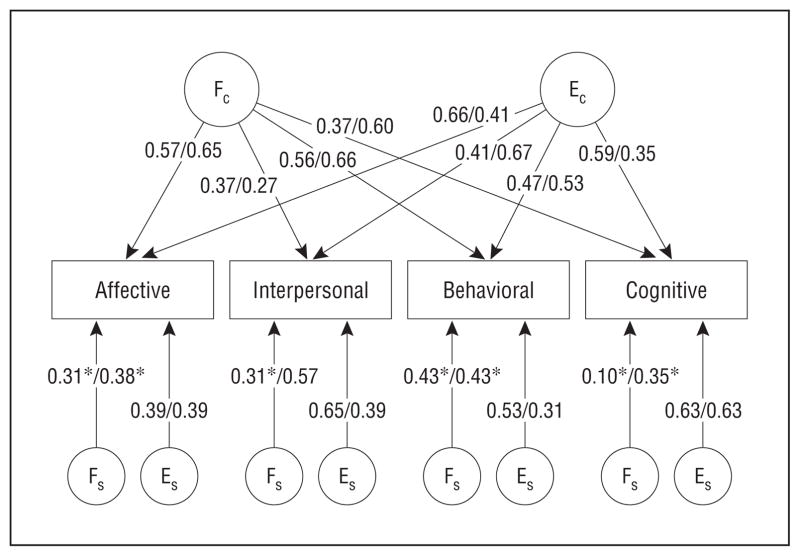
INDEPENDENT vs COMMON PATHWAY MODELS
For analyses using sectors defined by DSM-IV criteria and by DIB-R criteria, the common pathway model provided the most satisfactory fit to the data by all measures (Table 5). Specifically, the common pathway and independent pathway models were preferred over the Cholesky model by the χ2 difference test, AIC, and BIC. Furthermore, the common pathway model was slightly preferred over the independent pathway model by AIC (although for DIB-R–defined sectors, the goodness of fit was virtually equivalent) and strongly preferred by BIC. The path coefficients for the independent and common pathway models are shown in Figure 4 and Figure 5.
Table 5.
Relative Fit for Pairs of Models for Sectors of Psychopathology
| Pairs of Models Compared | Δdfa | χ2b | P Value | ΔAICc | ΔBICd |
|---|---|---|---|---|---|
| DSM-IV–defined sectors | |||||
| Cholesky vs independent pathway | 4 | 1.16 | .88 | −6.84 | −28.08 |
| Cholesky vs common pathway | 7 | 2.75 | .91 | −11.25 | −48.43 |
| Independent pathway vs common pathway | 3 | … | … | −4.54 | −20.47 |
| DIB-R–defined sectors | |||||
| Cholesky vs independent pathway | 4 | 7.15 | .13 | −0.85 | −22.10 |
| Cholesky vs common pathway | 7 | 12.70 | .08 | −1.30 | −38.48 |
| Independent pathway vs common pathway | 3 | … | … | −0.51 | −16.45 |
Abbreviations: AIC, Akaike information criterion; BIC, Bayesian information criterion; DIB-R, Revised Diagnostic Interview for Borderlines; ellipses, models are not nested, therefore, χ2 and corresponding P value cannot be calculated.
Difference in df (larger model minus smaller model).
Based on Yuan-Bentler T2 * statistic, which asymptotically has χ2 distribution.
ΔAIC = χ2 − 2Δdf, which represents difference in AIC (larger model minus smaller model); positive values favor larger model (listed first) and negative values favor smaller model (listed second).
ΔBIC = χ2 − Δdf *log(n) (with n = number of pairs of first-degree relatives [1498]), which represents difference in BIC (larger model minus smaller model); positive values favor larger model (listed first) and negative values favor smaller model (listed second).
Figure 4.
Estimated path coefficients for independent pathway model for sectors (DSM-IV–defined/Revised Diagnostic Interview for Borderlines-R–defined). EC indicates latent unique environmental factor common to all sectors; ES, unique environmental factor specific for a given sector; FC, familial factor common to all sectors; FS, familial factor specific for a given sector. Observed variables are in rectangles and latent variables are in circles. *Not significantly different from zero.
Figure 5.
Estimated path coefficients for common pathway model for sectors (DSM-IV–defined/Revised Diagnostic Interview for borderlines–defined). F, familial factor for borderline personality disorder (BPD-ness); E, unique environmental factor for BPD-ness; BPD-ness, factor representing liability to BPD; FS, familial factor specific for a given sector; ES, unique environmental factor specific for a given sector. Observed variables are in rectangles and latent variables are in circles. *Not significantly different from zero.
COMMENT
The main findings of this family interview study of BPD were that BPD and its 4 sectors of psychopathology aggregate in families and that the relationship among these sectors is best explained by a common pathway model in which the sectors represent manifestations of a latent BPD construct.
We discuss these findings in turn. Our primary hypothesis—that BPD (meeting both DSM-IV and DIB-R criteria) is caused in part by familial factors—was strongly supported. An individual with a first-degree relative showing BPD exhibited a statistically significant 3- to 4-fold increase in risk of BPD compared with an individual without a first-degree relative with BPD. In addition, we found a substantial and statistically significant correlation of 0.28 to 0.37 for the presence of BPD between pairs of first-degree relatives. These results are consistent with previous, less methodologically rigorous, family studies13–22 that have also found evidence of familial aggregation of BPD and with twin studies23–26 that have found evidence of substantial heritability of BPD. Taken together, these results indicate that familial factors contribute importantly to the development of BPD.
We also found that each of the 4 sectors of BPD psychopathology aggregated in families. The correlation between family members was greater for the affective and interpersonal sectors (using the DIB-R but not the DSM-IV definition) than for the behavioral and cognitive sectors. These differences could reflect differences in the strength of familial factors for different sectors but also could be the result of differences in the ability of the measures to tap the underlying construct of interest or heterogeneity within the sectors. Notably, the level of familial aggregation, as assessed by the correlation between pairs of relatives, was less for each of the sectors than it was for BPD. As with the diagnosis of BPD, the level of familial aggregation for sectors was higher for DIB-R–derived definitions than it was for DSM-IV–derived definitions.
Although family study data, unlike twin study data, cannot be used to identify the proportion of familial factors caused by genetic factors and those caused by the common family environmental factors without strong additional assumptions,76 there are 2 reasons to suspect that genetic factors largely account for the familiality of BPD. First, most importantly, twin studies of BPD23–26 and of the sectors of BPD psychopathology,44,45,47,72 have found no evidence of a significant contribution of common family environment. Similarly, we found no consistent differences in the level of familial aggregation between types of relative pairs (eg, siblings vs parent-child), whereas such differences would be expected if common family environmental factors were present. However, this latter argument is tentative because of inherent limitations of the family study design to address this issue; furthermore, to the extent that family study data can be used for this purpose, we had limited power to detect effects of interest.
Based on the reasonable likelihood that common family environmental factors are negligible, our data can be used to derive estimates of heritability. By doubling the observed correlation coefficients (because first-degree relatives share, on average, 50% of their genes, the correlation due to sharing 100% of genes would be twice that observed among first-degree relatives), we obtain heritability estimates for BPD of 55% (using proband-relative pairs) and 74% (using all pairs of relatives) and estimates for sectors ranging from 26% to 60% using the DIB-R definitions and 14% to 44% using the DSM-IV definition. Estimates from twin studies for the heritability of BPD range from 37% to 69%23–26 and estimates of the sectors’ affective instability, impulsiveness (similar to behavioral in this study), and cognitive range from 31% to 49%44–47; all of these estimates lie within the 95% confidence intervals of our estimates.
We note further that the findings from our family study and those from registry-based twin studies23,24,26 are not only convergent but also complementary with respect to the methodologic strengths of the 2 designs, with our study providing evidence based on more rigorous assessments using direct interviews and more information derived from full cases of BPD, and the twin studies providing data that are less vulnerable to selection bias and evidence that the familial effects are due to genetic factors.
Although genetic factors likely play a role in BPD, no genetic mechanisms underlying BPD or specific genes associated with BPD have been identified. However, one linkage study77 has found an association of BPD with a region on chromosome 9 that contains a number of plausible candidate genes.
Addressing the relationship among the 4 sectors of BPD psychopathology, we found that the pattern of co-occurrence of sectors within individuals and aggregation of sectors between family members was better explained by a common pathway model than by an independent pathway model. For the models with DIB-R–defined sectors, the difference in AIC was very modest and thus indicated an essentially equivalent overall fit. The overall fit evaluated by BIC, which penalizes lack of parsimony more than the AIC, was much better with the common pathway model for both sets of models. On balance, our data suggest that the common pathway model is the best-fitting model.
Under the plausible assumption that the contribution of common family environment is negligible, the heritability of the latent factor of BPD-ness from the common pathway model was 43.9% using DSM-IV–defined sectors and 58.6% using DIB-R–defined sectors. Two other studies that performed this type of analysis also found support for the common pathway model over the independent pathway model and yielded similar estimates (51%44 and 60%54) for the heritability of the latent BPD construct. Distel and associates44 assessed 4 sectors of BPD derived from the Personality Assessment Inventory Borderline Features scale (affective instability, negative relationships, identity problems, and self-harm), and Kendler and colleagues54 assessed 4 sectors derived from the Dimensional Assessment of Personality Pathology–Basic Questionnaire (affective lability, insecure attachment, cognitive dysregulation, and identity problems). Taking the findings of these studies together with those of our study (which again are not only convergent but also stem from methodologically complementary designs) favors the hypothesis that the relationship between the sectors is better explained by their being manifestations of an underlying latent BPD construct rather than the alternative hypothesis that the sectors themselves are the primary psychopathological entities.
Our modeling results should be interpreted with caution. The number of sectors was small and, although major sectors of BPD were captured, other potentially important elements of BPD psychopathology were not assessed. Therefore, it was possible to fit only 1 independent pathway model with a single common familial factor and a single common environmental factor. With a larger sample and a more fine-grained analysis, using a larger number of sectors (and even exploration of traits within the sectors, since each sector embraces a broad range of traits), it is possible that an independent pathway model with more than 1 common familial or environmental factor would provide a better fit. Furthermore, the latent construct of BPD might prove to be better conceptualized as a liability to more general personality psychopathology. For example, Distel and associates78 found considerable overlap in the genetic and environmental factors for BPD and for 4 of the 5 dimensions of the 5-factor model.79,80 In addition, Livesley and colleagues46 identified, through factor analysis and multivariate twin analyses, a higher-order personality factor, termed emotional dysregulation, that included not only affective instability, cognitive dysregulation, and other features in common with BPD but also a broader range of psychopathology.
These caveats notwithstanding, the evidence for a common pathway model with a unitary liability to BPD, combined with our finding that the familiality of BPD is greater than that of its individual sectors, has 3 implications. First, there should be efforts to identify endophenotypes associated not only with individual sectors of BPD37,72 but also with a more global tendency toward dysregulation that involves several sectors. Second, treatments should be developed to target multiple sectors of BPD, and, conversely, treatments directed at individual sectors of BPD may not be optimally targeting factors that underlie those sectors. Third, the proposed radical change to either a dimensional or a prototypic definition of BPD for DSM-581,82 should await evidence that the proposed revisions define a construct with better clinical usefulness, familiality/heritability, and psychometric coherence than the definition of BPD in DSM-IV. Based on these indices, a better definition might be one that requires psychopathology—rated for severity in addition to presence or absence—in at least 3 of 4 sectors for the diagnosis of BPD.83
There are several limitations of the study that should be considered. First, we did not sample probands randomly from a defined source population. Thus, our sampling method may have introduced selection bias if the probands were not representative of individuals in the source population in the 3 groups sampled (ie, individuals with and without BPD, and individuals with MDD). However, the finding that there was no significant interaction between the source of the BPD proband (patient vs community) and measures of the familial aggregation of BPD suggests that the 2 sources of individuals with BPD were similar. We also took care to select individuals without BPD in a manner that did not involve knowledge of whether they had any attributes, such as other forms of psychopathology (except for those that were excluded in all proband groups), that might influence familial aggregation patterns. Because we had very few patient probands with MDD, we were unable to test for such an interaction involving that population. Second, we used weighting based on the inverse probability of selection using a novel estimator of the prevalence of BPD derived from the data on relatives rather than a direct assessment of prevalence. Any additional uncertainty attributable to use of this method is not reflected in the confidence intervals, but any such uncertainty would, in any event, be expected to be small relative to other sources. Furthermore, the weighting method could have introduced bias. However, it is reassuring that the sensitivity analysis showed that the estimates for the familial aggregation of BPD did not change substantially when the analysis was unweighted and was confined to families in the BPD proband group and the non-BPD proband group. Third, to obtain the maximum amount of data from our sample, we used information from families in which the proband was recruited for MDD, but it is possible that either the selection or weighting of this group could have introduced bias. However, the results did not change appreciably when this group was excluded. Fourth, not all eligible parents and siblings chose to participate; the missing data could have introduced bias if the characteristics of the relatives not interviewed were different from those who were interviewed. However, serious bias would be unlikely unless there were a differential effect among proband groups (eg, if ill relatives of BPD probands were more likely to participate than were equally ill relatives of non-BPD probands). Fifth, the lifetime diagnosis of BPD, including its various sectors, is difficult to assess. However, misclassification of this type would be expected to be nondifferential across groups and therefore would likely cause bias toward the null. Sixth, although we found no statistically significant differences in measures of familial aggregation related to sampling source, type of relative, generation, or sex, we had little power to detect such differences; therefore, we may have failed to identify some important differences. Future studies should be large enough to test for these differences, which may have relevance to the causation of the disorder and to treatment approaches. Of additional reassurance is that twin studies have found no evidence of sex effects for BPD,23 for BPD sectors,44 and overall, for cluster B personality disorders.84
In conclusion, BPD and its sectors of psychopathology show substantial familial aggregation, suggesting a causal role for familial factors for the diagnosis of BPD and for each of the sectors. Furthermore, these results, in combination with those from twin studies, suggest that BPD has moderate heritability and that the individual sectors of psychopathology have a somewhat lower level of heritability. Finally, the relationship of BPD to its sectors of psychopathology is best explained by a model whereby the sectors are manifestations of a unitary liability to BPD.
Acknowledgments
Funding/Support: This study was supported by grant MH 400130 (R01) from the National Institute of Mental Health.
Footnotes
Financial Disclosure: None reported.
Additional Contributions: Kenneth Kendler, MD, provided helpful comments on the manuscript.
References
- 1.Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, Dawson DA, Pulay AJ, Pickering RP, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;62(6):553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swartz M, Blazer D, George L, Winfield I. Estimating the prevalence of borderline personality disorder in the community. J Pers Disord. 1990;4(3):257–272. doi: 10.1521/pedi.1990.4.3.257. [DOI] [Google Scholar]
- 4.Widiger TA, Frances AJ. Epidemiology, diagnosis, and comorbidity of borderline personality disorder. In: Tasman A, Hales RE, Frances AJ, editors. Review of Psychiatry. Vol. 8. Washington, DC: American Psychiatric Press; 1989. [Google Scholar]
- 5.Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- 6.Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, Grilo CM, Shea MT, Zanarini MC, Morey LC, Sanislow CA, Oldham JM. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276–283. doi: 10.1176/appi.ajp.159.2.276. [DOI] [PubMed] [Google Scholar]
- 7.Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang H, O’Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998;55(11):973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- 8.Merikangas KR, Swendsen JD. Genetic epidemiology of psychiatric disorders. Epidemiol Rev. 1997;19(1):144–155. doi: 10.1093/oxfordjournals.epirev.a017937. [DOI] [PubMed] [Google Scholar]
- 9.Hudson JI, Lalonde JK, Berry JM, Pindyck LJ, Bulik CM, Crow SJ, McElroy SL, Laird NM, Tsuang MT, Walsh BT, Rosenthal NR, Pope HG., Jr Binge-eating disorder as a distinct familial phenotype in obese individuals. Arch Gen Psychiatry. 2006;63(3):313–319. doi: 10.1001/archpsyc.63.3.313. [DOI] [PubMed] [Google Scholar]
- 10.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry. 2001;158(10):1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157(10):1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 12.Wade TD, Keski-Rahkonen A, Hudson JI. Epidemiology of eating disorders. In: Tsuang MT, Tohen M, Jones P, editors. Textbook in Psychiatric Epidemiology. 3. New York, NY: John Wiley & Sons; 2011. pp. 343–360. [Google Scholar]
- 13.Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR. DSM-III disorders in the families of borderline outpatients. J Pers Disord. 1988;2 (4):292–302. doi: 10.1521/pedi.1988.2.4.292. [DOI] [Google Scholar]
- 14.Baron M, Gruen R, Asnis L, Lord S. Familial transmission of schizotypal and borderline personality disorders. Am J Psychiatry. 1985;142(8):927–934. doi: 10.1176/ajp.142.8.927. [DOI] [PubMed] [Google Scholar]
- 15.Johnson BA, Brent DA, Connolly J, Bridge J, Matta J, Constantine D, Rather C, White T. Familial aggregation of adolescent personality disorders. J Am Acad Child Adolesc Psychiatry. 1995;34(6):798–804. doi: 10.1097/00004583-199506000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Links PS, Steiner M, Huxley G. The occurrence of borderline personality disorder in the families of borderline patients. J Pers Disord. 1988;2(1):14–20. doi: 10.1521/pedi.1988.2.1.14. [DOI] [Google Scholar]
- 17.Loranger AW, Oldham JM, Tulis EH. Familial transmission of DSM-III borderline personality disorder. Arch Gen Psychiatry. 1982;39(7):795–799. doi: 10.1001/archpsyc.1982.04290070031007. [DOI] [PubMed] [Google Scholar]
- 18.Pope HG, Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG. The validity of DSM-III borderline personality disorder: a phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry. 1983;40(1):23–30. doi: 10.1001/archpsyc.1983.01790010025003. [DOI] [PubMed] [Google Scholar]
- 19.Reich JH. Familiality of DSM-III dramatic and anxious personality clusters. J Nerv Ment Dis. 1989;177(2):96–100. doi: 10.1097/00005053-198902000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Riso LP, Klein DN, Anderson RL, Ouimette PC. A family study of outpatients with borderline personality disorder and no history of mood disorder. J Pers Disord. 2000;14(3):208–217. doi: 10.1521/pedi.2000.14.3.208. [DOI] [PubMed] [Google Scholar]
- 21.Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: description of 6-year course and prediction to time-to-remission. Acta Psychiatr Scand. 2004;110(6):416–420. doi: 10.1111/j.1600-0447.2004.00362.x. [DOI] [PubMed] [Google Scholar]
- 22.White CN, Gunderson JG, Zanarini MC, Hudson JI. Family studies of borderline personality disorder: a review. Harv Rev Psychiatry. 2003;11(1):8–19. doi: 10.1080/10673220303937. [DOI] [PubMed] [Google Scholar]
- 23.Distel MA, Trull TJ, Derom CA, Thiery EW, Grimmer MA, Martin NG, Willemsen G, Boomsma DI. Heritability of borderline personality disorder features is similar across three countries. Psychol Med. 2008;38(9):1219–1229. doi: 10.1017/S0033291707002024. [DOI] [PubMed] [Google Scholar]
- 24.Kendler KS, Aggen SH, Czajkowski N, Røysamb E, Tambs K, Torgersen S, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for DSM-IV personality disorders: a multivariate twin study. Arch Gen Psychiatry. 2008;65(12):1438–1446. doi: 10.1001/archpsyc.65.12.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Torgersen S, Lygren S, Oien PA, Skre I, Onstad S, Edvardsen J, Tambs K, Kringlen E. A twin study of personality disorders. Compr Psychiatry. 2000;41(6):416–425. doi: 10.1053/comp.2000.16560. [DOI] [PubMed] [Google Scholar]
- 26.Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: a longitudinal twin study. Dev Psychopathol. 2009;21(4):1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zanarini MC, Frankenburg FR, Vujanovic AA. Inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines. J Pers Disord. 2002;16(3):270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- 28.Blais MA, Hilsenroth MJ, Castlebury FD. Content validity of the DSM-IV borderline and narcissistic personality disorder criteria sets. Compr Psychiatry. 1997;38(1):31–37. doi: 10.1016/s0010-440x(97)90050-x. [DOI] [PubMed] [Google Scholar]
- 29.Hurt SW, Hyler SE, Frances A, Clarkin JF, Brent R. Assessing borderline personality disorder with self-report, clinical interview, or semistructured interview. Am J Psychiatry. 1984;141(10):1228–1231. doi: 10.1176/ajp.141.10.1228. [DOI] [PubMed] [Google Scholar]
- 30.Sanislow CA, Grilo CM, McGlashan TH. Factor analysis of the DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry. 2000;157(10):1629–1633. doi: 10.1176/appi.ajp.157.10.1629. [DOI] [PubMed] [Google Scholar]
- 31.Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, Shea MT, Stout RL, Zanarini MC, McGlashan TH. Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the collaborative longitudinal personality disorders study. Am J Psychiatry. 2002;159(2):284–290. doi: 10.1176/appi.ajp.159.2.284. [DOI] [PubMed] [Google Scholar]
- 32.Taylor J, Reeves M. Structure of borderline personality disorder symptoms in a nonclinical sample. J Clin Psychol. 2007;63(9):805–816. doi: 10.1002/jclp.20398. [DOI] [PubMed] [Google Scholar]
- 33.Clarkin JF, Hull JW, Hurt SW. Factor structure of borderline personality disorder criteria. J Pers Disord. 1993;7(2):137–143. doi: 10.1521/pedi.1993.7.2.137. [DOI] [Google Scholar]
- 34.Livesley WJ, Schroeder ML. Dimensions of personality disorder: the DSM-III-R cluster B diagnoses. J Nerv Ment Dis. 1991;179(6):317–328. [PubMed] [Google Scholar]
- 35.Oquendo MA, Mann JJ. Identifying and managing suicide risk in bipolar patients. J Clin Psychiatry. 2001;62(suppl 25):31–34. [PubMed] [Google Scholar]
- 36.Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry. 1991;148(12):1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- 37.Siever LJ, Torgersen S, Gunderson JG, Livesley WJ, Kendler KS. The borderline diagnosis III: identifying endophenotypes for genetic studies. Biol Psychiatry. 2002;51(12):964–968. doi: 10.1016/s0006-3223(02)01326-4. [DOI] [PubMed] [Google Scholar]
- 38.Stanley B, Siever LJ. The interpersonal dimension of borderline personality disorder: toward a neuropeptide model. Am J Psychiatry. 2010;167(1):24–39. doi: 10.1176/appi.ajp.2009.09050744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silk KR. Borderline personality disorder: overview of biologic factors. Psychiatr Clin North Am. 2000;23(1):61–75. doi: 10.1016/s0193-953x(05)70143-x. [DOI] [PubMed] [Google Scholar]
- 40.Becker DF, McGlashan TH, Grilo CM. Exploratory factor analysis of borderline personality disorder criteria in hospitalized adolescents. Compr Psychiatry. 2006;47(2):99–105. doi: 10.1016/j.comppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 41.De Moor MH, Distel MA, Trull TJ, Boomsma DI. Assessment of borderline personality features in population samples: is the Personality Assessment Inventory–Borderline Features scale measurement invariant across sex and age? Psychol Assess. 2009;21(1):125–130. doi: 10.1037/a0014502. [DOI] [PubMed] [Google Scholar]
- 42.Silverman JM, Pinkham L, Horvath TB, Coccaro EF, Klar H, Schear S, Apter S, Davidson M, Mohs RC, Siever LJ. Affective and impulsive personality disorder traits in the relatives of patients with borderline personality disorder. Am J Psychiatry. 1991;148(10):1378–1385. doi: 10.1176/ajp.148.10.1378. [DOI] [PubMed] [Google Scholar]
- 43.Zanarini MC, Frankenburg FR, Yong L, Raviola G, Bradford Reich D, Hennen J, Hudson JI, Gunderson JG. Borderline psychopathology in the first-degree relatives of borderline and Axis II comparison probands. J Pers Disord. 2004;18 (5):439–447. doi: 10.1521/pedi.18.5.439.51327. [DOI] [PubMed] [Google Scholar]
- 44.Distel MA, Willemsen G, Ligthart L, Derom CA, Martin NG, Neale MC, Trull TJ, Boomsma DI. Genetic covariance structure of the four main features of borderline personality disorder. J Pers Disord. 2010;24(4):427–444. doi: 10.1521/pedi.2010.24.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Livesley WJ, Jang KL, Jackson DN, Vernon PA. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150 (12):1826–1831. doi: 10.1176/ajp.150.12.1826. [DOI] [PubMed] [Google Scholar]
- 46.Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry. 1998;55(10):941–948. doi: 10.1001/archpsyc.55.10.941. [DOI] [PubMed] [Google Scholar]
- 47.Jang KL, Livesley WJ, Vernon PA, Jackson DN. Heritability of personality disorder traits: a twin study. Acta Psychiatr Scand. 1996;94(6):438–444. doi: 10.1111/j.1600-0447.1996.tb09887.x. [DOI] [PubMed] [Google Scholar]
- 48.Kendler KS, Heath AC, Martin NG, Eaves LJ. Symptoms of anxiety and symptoms of depression: same genes, different environments? Arch Gen Psychiatry. 1987;44(5):451–457. doi: 10.1001/archpsyc.1987.01800170073010. [DOI] [PubMed] [Google Scholar]
- 49.Neale MC, Cardon LR. Methodology for Genetic Studies of Twins and Families. Dordrecht, the Netherlands: Kluwer Academic Publishers; 1992. [Google Scholar]
- 50.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. [PubMed] [Google Scholar]
- 51.Hudson JI, Javaras KN, Laird NM, VanderWeele TJ, Pope HG, Jr, Hernán MA. A structural approach to the familial coaggregation of disorders. Epidemiology. 2008;19(3):431–439. doi: 10.1097/EDE.0b013e31816a9de7. [DOI] [PubMed] [Google Scholar]
- 52.Clarkin JF, Widiger TA, Frances A, Hurt SW, Gilmore M. Prototypic typology and the borderline personality disorder. J Abnorm Psychol. 1983;92(3):263–275. doi: 10.1037//0021-843x.92.3.263. [DOI] [PubMed] [Google Scholar]
- 53.Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biol Psychiatry. 2002;51(12):936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- 54.Kendler KS, Myers J, Reichborn-Kjennerud T. Borderline personality disorder traits and their relationship with dimensions of normative personality: a Web-based cohort and twin study [published online December 28, 2010] Acta Psychiatr Scand. :21198457. doi: 10.1111/j.1600-0447.2010.01653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morey LC. The Personality Assessment Inventory: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 56.Livesley J. The Dimensional Assessment of Personality Pathology (DAPP) approach to personality disorder. In: Strack S, editor. Differentiating Normal and Abnormal Personality. 2. New York, NY: Springer; 2006. pp. 401–425. [Google Scholar]
- 57.Livesley J, Jackson DN. Dimensional Assessment of Personality Pathology–Basic Questionnaire (DAPP-BQ) Technical Manual. Port Huron, MI: Sigma Assessment Systems; 2009. [Google Scholar]
- 58.Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Compr Psychiatry. 2001;42(2):144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- 59.First MB, Spitzer RL, Gibbons M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- 60.Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 61.Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: discriminating BPD from other Axis II disorders. J Pers Disord. 1989;3(1):10–18. doi: 10.1521/pedi.1989.3.1.10. [DOI] [Google Scholar]
- 62.Javaras KN, Laird NM, Hudson JI, Ripley BD. Estimating disease prevalence using relatives of case and control probands. Biometrics. 2010;66(1):214–221. doi: 10.1111/j.1541-0420.2009.01272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Arnold LM, Hudson JI, Keck PE, Auchenbach MB, Javaras KN, Hess EV. Comorbidity of fibromyalgia and psychiatric disorders. J Clin Psychiatry. 2006;67 (8):1219–1225. doi: 10.4088/jcp.v67n0807. [DOI] [PubMed] [Google Scholar]
- 64.Javaras KN, Pope HG, Lalonde JK, Roberts JL, Nillni YI, Laird NM, Bulik CM, Crow SJ, McElroy SL, Walsh BT, Tsuang MT, Rosenthal NR, Hudson JI. Co-occurrence of binge eating disorder with psychiatric and medical disorders. J Clin Psychiatry. 2008;69(2):266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- 65.Javaras KN, Laird NM, Reichborn-Kjennerud T, Bulik CM, Pope HG, Jr, Hudson JI. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. Int J Eat Disord. 2008;41(2):174–179. doi: 10.1002/eat.20484. [DOI] [PubMed] [Google Scholar]
- 66.Hudson JI, Laird NM, Betensky RA. Multivariate logistic regression for familial aggregation of two disorders, I: development of models and methods. Am J Epidemiol. 2001;153(5):500–505. doi: 10.1093/aje/153.5.500. [DOI] [PubMed] [Google Scholar]
- 67.Muthén LK, Muthén BO. [Accessed November 22, 2010.];Chi-square difference testing using the Satorra-Bentler scaled chi-square. http://www.Statmodel.Com/chidiff.Shtml.
- 68.Muthén LK, Muthén BO. Mplus User’s Guide: Statistical Analysis With Latent Variables. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 69.Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal data. Sociol Methodol. 2000;30(1):165–200. doi: 10.1111/0081-1750.00078. [DOI] [Google Scholar]
- 70.Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–723. doi: 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- 71.Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 72.Livesley WJ, Jang KL. The behavioral genetics of personality disorder. Annu Rev Clin Psychol. 2008;4:247–274. doi: 10.1146/annurev.clinpsy.4.022007.141203. [DOI] [PubMed] [Google Scholar]
- 73.Kendler KS, Silberg JL, Neale MC, Kessler RC, Heath AC, Eaves LJ. The family history method: whose psychiatric history is measured? Am J Psychiatry. 1991;148(11):1501–1504. doi: 10.1176/ajp.148.11.1501. [DOI] [PubMed] [Google Scholar]
- 74.Roy MA, Walsh D, Kendler KS. Accuracies and inaccuracies of the family history method: a multivariate approach. Acta Psychiatr Scand. 1996;93(4):224–234. doi: 10.1111/j.1600-0447.1996.tb10639.x. [DOI] [PubMed] [Google Scholar]
- 75.Hollingshead AB. Two Factor Index of Social Position. New Haven, CT: Yale University; 1957. [Google Scholar]
- 76.Javaras KN, Hudson JI, Laird NM. Fitting ACE structural equation models to case-control family data. Genet Epidemiol. 2010;34(3):238–245. doi: 10.1002/gepi.20454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Distel MA, Hottenga JJ, Trull TJ, Boomsma DI. Chromosome 9: linkage for borderline personality disorder features. Psychiatr Genet. 2008;18(6):302–307. doi: 10.1097/YPG.0b013e3283118468. [DOI] [PubMed] [Google Scholar]
- 78.Distel MA, Trull TJ, Willemsen G, Vink JM, Derom CA, Lynskey M, Martin NG, Boomsma DI. The five-factor model of personality and borderline personality disorder: a genetic analysis of comorbidity. Biol Psychiatry. 2009;66(12):1131–1138. doi: 10.1016/j.biopsych.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 79.Costa PT, McCrae RR. Professional Manual: Revised NEO Personality Inventory (NEO-PI-R) and Neo Five-Factor Inventory (NEO-FFI) Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 80.Widiger TA, Costa PT. Five-factor model personality disorder research. In: Costa PT, Widiger TA, editors. Personality Disorders and the Five-Factor Model of Personality. 2. Washington, DC: American Psychological Association; 2002. pp. 59–87. [Google Scholar]
- 81.American Psychiatric Association. 301.83: borderline personality disorder. [Accessed November 22, 2010.];DSM-5 Development Web site. http://www.Dsm5.Org/proposedrevisions/pages/proposedrevision.Aspx?Rid=17.
- 82.Trull TJ, Distel MA, Carpenter RW. DSM-5 borderline personality disorder: at the border between a dimensional and a categorical view. Curr Psychiatry Rep. 2011;13(1):43–49. doi: 10.1007/s11920-010-0170-2. [DOI] [PubMed] [Google Scholar]
- 83.Gunderson JG. Revising the borderline diagnosis for DSM-V: an alternative proposal. J Pers Disord. 2010;24(6):694–708. doi: 10.1521/pedi.2010.24.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Røysamb E, Neale MC, Kendler KS. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: a multivariate study. Psychol Med. 2008;38(11):1617–1625. doi: 10.1017/S0033291708002924. [DOI] [PubMed] [Google Scholar]