Abstract
Objective
To determine the effects of prenatal cocaine exposure on child development.
Methods
This prospective, longitudinal study recruited 154 pregnant cocaine users who were matched on race, parity, socioeconomic status, and perinatal risk to 154 noncocaine users. Drug use status was determined by maternal history and urine screening. At 3 years of age, the child subjects were assessed by an evaluator blinded to maternal drug use history. During a home visit at age 3, caregiver, family, and home assessments were administered.
Results
Structural equation modeling showed a direct effect of the amount of prenatal cocaine exposure on the adjusted birth head circumference which in turn directly affected preschool development.
Conclusions
We could not demonstrate a direct effect of prenatal cocaine exposure on preschool development, a result that is consistent with that of earlier work and now extending findings to age 3. However, cocaine continued to exert an indirect effect on development through its direct effect on the head circumference at birth.
Keywords: prenatal cocaine use, preschool development, structural equation modeling
The current cocaine epidemic has been in progress in this country since the early 1980s. With the ready availability and low cost of crack in the mid-1980s, its potency, increased potential for addiction, and frequent use by pregnant women gave rise to a new concern regarding potential affects on the developing fetus and child. Although a number of case reports, retrospective studies, and media articles heralded the dramatic effects of crack on a new generation of children, until more recently, no longitudinal, prospective studies were available to support or refute these initial concerns.
In 2001, Frank, Augustyn, Knight, Pell, and Zuckerman (2001) published a systematic review of the literature which included only studies that had enrolled prospectively, included a control group, and used evaluators blinded to drug group status. In addition, studies were excluded if subjects were exposed to opiates, other stimulants, and HIV. Of the 36 studies included in the review, only three reported psychomotor and cognitive outcomes at 3 years of age, with two studies involving the same cohort. In two of the studies there were no cocaine effects on cognitive and psychomotor assessments at age 3 (Azuma & Chasnoff, 1993; Kilbride, Castor, Hoffman, & Fuger, 2000). However, Griffith et al. using the Stanford-Binet, demonstrated that children who had been cocaine-exposed had lower Verbal Reasoning scores than children who had not been exposed (Griffith, Azuma, & Chasnoff, 1994). At the time of the review only two groups had published studies of cognitive and psychomotor development in children beyond age 3 that met the criteria for inclusion in the review and none of the studies demonstrated cocaine effects on psychomotor development (Hurt et al., 1997, 1998; Richardson, Conroy, & Day, 1996).
Since that time, additional studies evaluating psychomotor development and cognition have been published. Bennett, Bendersky, and Lewis (2002) demonstrated a differential gender effect of prenatal cocaine exposure on outcome, with boys who had been exposed to cocaine, but not girls, having lower IQ scores at age four when compared with their counterparts who were not exposed. Using a prospective cohort of children, Hurt, Malmud, Betancourt, Brodsky, and Giannetta (2001) demonstrated lower developmental scores at ages three and five due to postnatal environmental factors, but not due to prenatal cocaine exposure.
Scientists, clinicians, and caregivers are all eager to know what to expect about the outcome of children who have been cocaine exposed. It is important that a body of data be available at pivotal developmental time points to understand the evolution of the effects of prenatal exposure on long-term outcome. Age 3, before children enter the environment of the public school system, is a pivotal time point and thus this article describes the caregivers, families, home environment, and the psychomotor development of the children themselves, at this important age.
We hypothesized that children who were cocaine exposed would score more poorly on developmental measures at age 3 than their matched controls who were not cocaine exposed. In addition, we hypothesized that compared with the children who were not exposed, the psychosocial status of the caregiver and the quality of the family support and home environment would be less optimal for those who had been cocaine-exposed. Thus, we have used structural equation modeling to describe both the direct and indirect effects of prenatal cocaine exposure on preschool development at age 3, taking into account pertinent caregiver and environmental effects as well as important biologic factors of the child.
Methods
This study was approved by the Institutional Review Board of the University of Florida. A Certificate of Confidentiality from the National Institute on Drug Abuse, US Department of Health and Human Services (DA-91–45) protects the confidentiality of the research data collected. A project staff member approached all women for informed consent when they enrolled in prenatal care at the county public health department and were at least 15-weeks pregnant or in the case of little or no prenatal care, when they presented for delivery at our tertiary care center.
Study Design
This is a longitudinal, prospective study of the medical and developmental effects of prenatal cocaine exposure which enrolled subjects from 1991 to 1993. Mothers were recruited from a historically understudied population of rural public health department patients. A complete, detailed description of the longitudinal study has been published previously (Eyler, Behnke, Conlon, Woods, & Wobie, 1998). In summary, we prospectively enrolled prenatal cocaine users and a matched control group of noncocaine users when they first contacted the health care system for their pregnancy. This allowed us to minimize bias in participant enrollment and obtain the earliest drug history possible by enrolling subjects at either a prenatal clinic or the hospital in the case of no or limited prenatal care. We enrolled a sufficient sample size to allow for covariate analyses of possible confounding variables, and if necessary, to allow for an attrition rate of 33% over 3 years and still maintain needed statistical power to detect a significant difference of a third of a standard deviation between the exposed and nonexposed groups on measures of development. In addition, all assessments were made by appropriately trained, certified, or licensed professionals masked to study group membership of the mother and her child.
Subject matching criteria were chosen to minimize the effect on outcome of race, parity, socioeconomic status, and perinatal risk (that related to the location of prenatal care). Women were excluded a priori for the following reasons: (a) major illnesses that developed before pregnancy and were known to affect pregnancy outcome or developmental outcome of the fetus; (b) chronic use of prescription or over-the-counter drugs; (c) any illicit drug use other than marijuana and cocaine; (d) non-English-speaking; and (e) <18 years old. From over 2500 women who gave consent, were interviewed and not excluded, 154 were identified as cocaine users and continued in the longitudinal study. A pool of potential participants whose interviews and urine specimens indicated no evidence of prenatal cocaine use was maintained for each match category. As each target was identified, the longest held matched control was selected from the appropriate match category for study participation.
Identification/Documentation of Drug Use
Drug use was identified in the sample using two different methods. Drug histories adapted from Day, Wagener, and Taylor (1985) were elicited from all women at the end of each trimester of pregnancy. Experienced interviewers privately asked about the amount, frequency, and pattern of past drug use, defined as drug use during the previous trimester of pregnancy, thought to provide more accurate data by being less threatening (Day et al., 1985; Jacobson et al., 1991). In an effort to maximize the accuracy of subject classification, urine specimens were collected at two unanticipated times, study enrollment and at delivery. Urine screening included assessment for barbiturates, benzodiazepines, cocaine, marijuana, methamphetamines and amphetamines, opiates, phencyclidine, and propoxyphene using fluorescence polarization immunoassay (Mule & Casella, 1988). Cocaine was considered to be present when benzoylecgonine was detected at or above a cut-off of 300 ng/mL. All positive screens were confirmed using gas chromatography/mass spectrometry.
3-Year Evaluations
At 3 years of age, caregiver, family, and home assessments were performed in the child’s home. In addition, a standardized caregiver report of the child was obtained. The child was assessed at a separate visit for the purpose of evaluating overall development. The caregiver, family, and home assessments chosen for use in this study have been shown to be associated with maternal drug use, as well as, either directly or theoretically to child outcome. The measures have been fully described in previous publications (Behnke, Eyler, Woods, Wobie, & Conlon, 1997; Bradley & Caldwell, 1976; Woods, Behnke, Eyler, Conlon, & Wobie, 1995)
Specific caregiver measures included the Center for Epidemiologic Studies-Depression (CES-D) (Radloff, 1977), Levenson Locus of Control (LOC) (Levenson, 1974), Parenting Sense of Competence (PSOC) (Gilbaud-Wallston, 1977), Rosenberg Self-esteem Scale (RSS) (Rosenberg, 1989), Concepts of Development Questionnaire (CODQ) (Sameroff & Feil, 1986), and Life Experiences Survey (LES) (Sarason, Johnson, & Siegel, 1978). The family evaluation included the Family Adaptability and Cohesion Evaluation Scales-III (FACES-III) (Edman, Cole, & Howard, 1990; Green, Harris, Forte, & Robinson, 1991; Olson, 1986; Olson, 1989) and the Family Support Scale (FSS) (Dunst, Jenkins, & Trivette, 1984). A home assessment was made using the Home Observation for Measurement of the Environment (HOME) (Bradley & Caldwell, 1976; Caldwell & Bradley, 1984). Caregiver report of the child’s adaptive behavior was obtained using the Vineland Adaptive Behavior Scales (VABS) (Sparrow, Balla, & Cicchetti, 1984).
At a separate visit, an evaluation of the child was made by a licensed, experienced examiner blinded to maternal drug status. Assessments included the Mental (MDI) and Psychomotor (PDI) Developmental Indices of the Bayley Scales of Infant Development (Bayley, 1993).
Statistical Analyses
Group comparisons for continuous data were made using the Wilcoxon Rank Sum and for categorical data using the Chi-square tests. Structural equation modeling (SEM) was used to test theoretical models that specify causal relationships between observed variables that were organized into meaningful constructs. Power analysis indicated that the sample size is sufficient for the number of degrees of freedom available in the SEM analyses reported in this article with power >0.80 (MacCallum, Browne, & Sugawara, 1996). Statistical significance for tests of hypotheses was set at 0.05.
After hypothesizing a theoretical model, specifying the relationships between constructs, and choosing indicator variables that operationalized the constructs, a two-step approach was followed. First, an acceptable measurement model was developed in which all constructs were allowed to correlate with each other. After verifying that the measurement model displayed an acceptable fit to the data, a structural model was developed by making modifications that specified the causal relationships between the latent constructs themselves.
To assess structural model fit, the indices recommended by Hoyle and Panter (1995) were used. The PROC CALIS procedure in SAS (SAS Institute, 1989) was chosen to perform all SEM path analyses. The maximum likelihood method was used to estimate free parameters. All models were estimated in covariance metric.
The model originally included eight constructs: amount of prenatal cocaine use, other prenatal substance use, adjusted birth head circumference, number of caregiver changes by age 3, caregiver problems at age 3, environmental factors at age 3, gender, and psychomotor development at age 3. Variables were considered a priori for inclusion in each construct based upon research theories, empirical data, and the constraints of the statistical methodology (Behnke et al., 1997; Behnke, Eyler, Garvan, Wobie, & Hou, 2002; Bradley & Caldwell, 1976; Woods et al., 1995). Ultimate variable selection was dependent upon significant factor loadings on the latent constructs as well as acceptable residual values to construct well-fitting measurement models (Hatcher, 1994). Previously established imputation methods were used to estimate missing data (Behnke et al., 2002) and accounted for <0.05% of the data available for any individual variable in the analysis.
Details concerning variable selection for each construct are as follows. A frequency measure of prenatal cocaine exposure was derived from the interview data to quantify the amount of cocaine exposure for the Amount of Cocaine Use variable. The number of weeks that the mother reported using cocaine during the 12 weeks prior to pregnancy through the end of her pregnancy was divided by the total number of weeks of her pregnancy plus the 12 weeks prior to conception. Average daily use of tobacco (cigarettes smoked per day), alcohol (ounces of absolute alcohol per day) and marijuana (joints smoked per day) were considered for the Other Substance Use variable. Marijuana use did not have significant factor loading and was not retained in the model. On the basis of previous work from our group (Behnke et al., 2002), the Adjusted Birth Head Circumference variable included the head circumference as measured at birth, standardized across varying gestational ages. The Number of Caregiver Changes variable was a measure of the number of times the child changed caregivers during the first 3 years of life. This was thought to be a potentially important variable given the fact that 56% of the cocaine-exposed children (n = 77) were not living with their biological mother compared to only 6% of the nonexposed children (n = 8). The following measures were considered for inclusion in the variable Caregiver Problems: CES-D, LOC (Internal, Chance, and Powerful Others subscales), PSOC (Self-efficacy and Value of Parenting subscales), FSS (Number of Supports and Value of Supports subscales), and RSS. The LOC Internality subscale and the PSOC Self-efficacy subscale did not have significant factor loadings and were not retained in the model. Because the two FSS subscales did not load on the same factor as the other variables in the Caregiver Problems variable, a separate construct was developed entitled Family Support. For the Quality of the Environment variable, the following measures were considered for inclusion: the HOME (total score), LES (Balance subscale), and the CODQ (Categorical and Perspectivistic subscales). The LES Balance subscale and the CODQ Perspectivistic subscale were not retained in the model due to nonsignificant factor loadings. The Gender variable included male and female, which were assigned 1 and 0, respectively. The Bayley MDI and PDI and the Communication subscale and Motor Skills subscale of the VABS were included in the Preschool Development variable.
Data exhibiting skewness and high kurtosis were transformed prior to fitting of the measurement model. These included the Total HOME score, the amount of tobacco use, and the amount of alcohol use. The initial measurement model could not be fit. This was thought to be due to inclusion of the Number of Caregiver Changes and the Family Support latent constructs. These were eliminated and a measurement model was able to be fit to the data (see Table I).
Table I.
Fit Statistics for the Measurement and Structural Equation Models
| Model | χ2 | df | p | GFI | RMSEA | CFI | NNFI | Comparison to measurement model
|
||
|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p | ||||||||
| Measurement model | 125.31 | 83 | .0019 | 0.943 | 0.045 | 0.956 | 0.937 | — | — | — |
| Structural equation model | 140.05 | 96 | .0023 | 0.936 | 0.043 | 0.955 | 0.943 | 14.74 | 13 | .324 |
CFI = comparative fit index; GFI = goodness of fit index; NNF = nonnormed fit index; and RMSEA = root mean squared error of approximation.
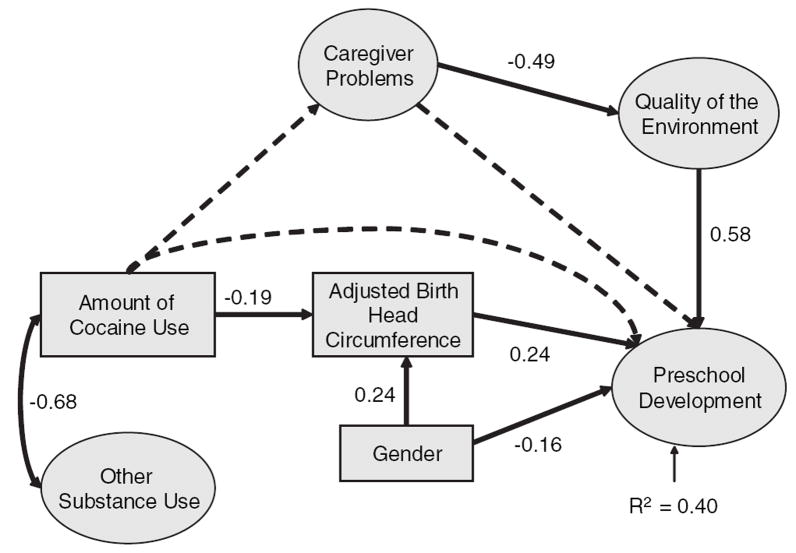
Next, the theoretical structure model of hypothesized relationships between the latent variables represented in Figure 1 was tested. Model fit was improved by first eliminating nonsignificant paths one at a time (Bentler & Chou, 1987). The modification indices were inspected to determine whether there were any additional paths that needed to be estimated, and there were not. See Table I for fit statistics.
Figure 1.
SEM Analysis at Age 3 for Preschool Development Latent constructs are represented with ovals and manifest constructs with rectangles. Curved, double-headed arrows indicate constructs allowed to covary and single-headed arrows indicate directional pathways. Pathways that lacked statistical significance are indicated by dotted lines. Solid lines indicate significant pathways from the theoretical model.
To quantify the magnitude of relationship between latent variables, all latent variables were set to the same unit of measurement (i.e., all latent variables were scaled to have a standard deviation of 1.00). This allowed the comparison of the relative sizes of standardized path coefficients to determine which independent variables had the largest effect on the dependent variable. The R2 value, which reflects the extent to which independent variables in the model account for variability in the dependent variable, was calculated for the Preschool Development outcome. Table II includes a list of parameter estimates and standard errors.
Table II.
Path Coefficients, Standard Errors, and t Values for the Structural Equation Model
| Unstandardized path coefficient | Standard error | t value | Standardized path coefficient | |
|---|---|---|---|---|
| Adjusted birth head circumference | ||||
| Amount of cocaine use | −0.9290 | 0.2895 | −3.2090 | −0. 1932 |
| Gender | 0.7210 | 0.1811 | 3.9813 | 0.2397 |
| Quality of the environment | ||||
| Caregiver problems | −0.0441 | 0.0081 | −5.4528 | −0.4879 |
| Preschool development | ||||
| Quality of the Environment | 11.3346 | 2.2856 | 4.9592 | 0.5830 |
| Adjusted birth head circumference | 1.8017 | 0.5131 | 3.5114 | 0.2414 |
| Gender | −3.4813 | 1.4971 | −2.3254 | −0.1551 |
To interpret the results of the SEM, the loading of one indicator in each latent variable was constrained to unity (set to 1.00). This equates the scale of the latent variable with the scale of the constrained indicator variable. The indicator variables chosen to be constrained to unity were generally those with the highest loading on their factor and included amount of tobacco use for Other Substance Use, CES-D for Caregiver Problems, Total HOME score for Quality of the Environment, and MDI for Preschool Development. Owing to data transformations, the scale for the Other Substance Use latent variable is inversely proportional to tobacco use (a higher score represents less other drug use), the scale for the Caregiver Problems latent variable is the same as that of the CES-D (a higher score represents more caregiver problems), the scale for the Quality of the Environment latent variable is the same as the Total HOME score (a higher score represents a higher quality environment), and the scale for the Preschool Development latent variable is the same as the Bayley MDI (a higher score represents better development).
Results
Sample Description
Of the original 308 subject pairs enrolled in the study, 10 children died (5 exposed and 5 nonexposed), and 22 children did not return for the 3-year visit (14 exposed and 8 nonexposed), leaving 276 caregivers and their offspring (a return rate of 92.6% of those still living at age 3). This included 135 children who had been cocaine exposed and 141 controls who were not cocaine exposed. The children were predominantly African-American (82% in both groups) and of low socioeconomic status (97% in both groups). There was not a significant difference in the number of female children who had been cocaine-exposed and those who had not (52% vs. 44%; p = .1902) nor was there a significant difference in the age at evaluation (3.1 years in both groups).
Caregiver, Family, and Home Assessments
There were no significant group differences on the LOC, RSS, FACES-III, or seven of the eight HOME subscales. However, caregivers of the children who were cocaine exposed had significantly lower scores on the CES-D, Positive Events subscale of the LES, Balance (number of positive – number of negative events) subscale of the LES, Total score on the CODQ, and Number of Family Supports subscale of the FSS than the caregivers of the children who were not exposed. In addition, caregivers of children who were cocaine exposed had significantly higher scores on the Self-efficacy subscale of the PSOC and the Warmth and Acceptance subscale of the HOME. There were significantly more caregiver changes on average during the first 3 years of life for the children who were cocaine exposed than for those who were not (see Table III).
Table III.
Caregiver, Family, and Home Assessments
| Cocaine-exposed
|
Nonexposed
|
|||
|---|---|---|---|---|
| M ± SD | Mdn | M ± SD | Mdn | |
| Depression (CES-D)-total scorea | 20.0 ± 10.6 | 20.0* | 22.2 ±9.2 | 22.0 |
| Locus of Control (LOC) | ||||
| External chancea | 26.7 ± 5.2 | 27.0 | 27.5 ± 4.6 | 27.0 |
| Internality | 33.8 ± 4.7 | 33.0 | 34.3 ± 4.6 | 34.0 |
| External powerful othersa | 25.9 ± 4.8 | 26.0 | 24.8 ± 5.4 | 25.0 |
| Parenting self-esteem (PSOC) | ||||
| Self-efficacy | 20.2 ± 4.8 | 21.0* | 19.1 ± 5.1 | 19.0 |
| Comfort/value of parenting | 32.8 ± 5.6 | 33.0 | 33.2 ± 5.2 | 33.0 |
| Overall parental functioning | 53.0 ± 6.4 | 55.0 | 52.3 ± 6.2 | 53.0 |
| Personal self-esteem (RSS)-total | 31.4 ± 3.9 | 30.0 | 31.9 ± 4.0 | 31.0 |
| Concepts of development (CODQ) | ||||
| Categoricala | 1.4 ± 0.4 | 1.4 | 1.4 ± 0.4 | 1.3 |
| Perspectivistic | 1.9 ± 0.2 | 1.9 | 2.0 ± 0.3 | 1.9 |
| Total | 1.8 ± 0.2 | 1.7* | 1.8 ± 0.2 | 1.8 |
| Life stress (LES) | ||||
| Positive events | 11.6 ± 10.7 | 9.0* | 14.5 ± 11.5 | 12.0 |
| Negative eventsa | 10.2 ± 10.4 | 7.0 | 9.8 ± 9.3 | 7.0 |
| Total events | 21.7 ± 7.1 | 18.0 | 24.3 ± 16.7 | 19.0 |
| Balance (positive – negative events) | 1.4 ±12.4 | 2.0* | 4.8 ± 12.6 | 4.0 |
| Family support (FSS) | ||||
| Number of supports | 11.5 ± 2.8 | 11.0* | 12.3 ± 2.2 | 12.0 |
| Value of supports | 37.7 ± 12.2 | 37.0 | 38.6 ± 10.6 | 38.0 |
| Family functioning (FACES-III)b | ||||
| Adaptability | 4.3 ± 1.7 | 4.0 | 4.0 ± 1.8 | 4.0 |
| Cohesion | 3.5 ± 1.7 | 3.0 | 3.5 ± 1.8 | 3.0 |
| Family type | 3.9 ± 1.3 | 3.5 | 3.7 ± 1.4 | 3.5 |
| HOME | ||||
| Learning stimulation | 6.3 ± 2.8 | 6.0 | 5.8 ± 2.6 | 6.0 |
| Language stimulation | 6.3 ± 1.1 | 7.0 | 6.3 ± 1.0 | 7.0 |
| Physical environment | 5.3 ± 1.9 | 6.0 | 5.6 ± 1.7 | 6.0 |
| Warmth and acceptance | 5.5 ± 1.7 | 6.0* | 5.3 ± 1.5 | 5.0 |
| Academic stimulation | 4.0 ± 1.1 | 4.0 | 3.8 ± 1.2 | 4.0 |
| Modeling | 3.0 ± 1.3 | 3.0 | 3.2 ± 1.2 | 3.0 |
| Variety in experience | 5.7 ± 1.7 | 6.0 | 5.8 ± 1.7 | 6.0 |
| Acceptance | 2.7 ± 1.1 | 3.0 | 2.8 ± 1.2 | 3.0 |
| Total | 38.8 ± 8.8 | 40.0 | 38.4 ± 8.0 | 40.0 |
| Number of caregiver changesa | 0.6 ± 1.0 | 0** | 0.1 ± 0.4 | 0 |
Lower scores are better;
central scores are optimal.
p < 0.05.
p < 0.0001.
Child Assessments
There were no significant group differences on the MDI or PDI of the Bayley Scales of Infant Development. Nor were there any significant group differences on the Communication subscale and Motor Skills subscale of the VABS (see Table IV).
Table IV.
Child Assessments at Age 3
| Cocaine-exposed
|
Nonexposed
|
|||
|---|---|---|---|---|
| M±SD | Mdn | M±SD | Mdn | |
| Bayley Scales of Infant | ||||
| Development (BSID)a | ||||
| MDI | 83.6 ±16.7 | 83.0 | 84.8 ±17.9 | 86.0 |
| PDI | 91.8 ±18.8 | 96.0 | 94.9 ±19.6 | 100.0 |
| Vineland Adaptive | ||||
| Behavior Scales (VABS)a | ||||
| Communication | 101.0 ±14.8 | 105.0 | 98.8 ±14.2 | 99.0 |
| Motor skills | 96.6 ±15.4 | 96.5 | 95.5 ±13.3 | 93.3 |
No significant group differences for any of the child assessments at age 3.
Higher scores are better.
Structural Equation Modeling
For the SEM analyses, 251 subjects had complete data for all the indicator variables included in the Preschool Development latent variable. Figure 1 represents the final model developed.
As seen in Figure 1, the amount of prenatal cocaine use was significantly correlated with other substance use during pregnancy (correlation coefficient = −0.68). Gender significantly predicted both adjusted birth head circumference (standardized path coefficient = 0.24) and preschool development at age 3 (standardized path coefficient = −0.16). The directionality of the standardized path coefficients indicates that being a male was associated with a larger head circumference and being a female was associated with better preschool development. Caregiver problems demonstrated an indirect influence on preschool development through the quality of the environment. The adjusted birth head circumference directly predicted preschool development (standardized path coefficient = 0.24). Finally, the amount of prenatal cocaine exposure did not significantly predict preschool development. However, it directly affected the adjusted birth head circumference (standardized path coefficient = −0.19) which in turn directly affected preschool development.
Discussion
The extant literature regarding the psychomotor and cognitive effects of prenatal cocaine exposure on the outcome of children who have been exposed has been inconclusive to date. Although early case reports raised concerns and predicted that there might be significant damage to the central nervous system of children who had been prenatally cocaine exposed, prospective studies have yielded conflicting results and many have documented only subtle differences in outcome.
Recent studies have helped further our understanding of the effects of prenatal cocaine exposure. For example, in the studies by Hurt et al. (2001), findings included group differences in outcome due to environmental factors with no effect of prenatal cocaine exposure, whereas Bennett et al. (2002) found significant gender differences in IQ based on the exposure status of the children.
This study supports the idea that there is no discernable direct effect of cocaine on preschool development at age 3. This was demonstrated in the univariate analyses as well as in the SEM. In addition, this study supports the findings from other studies of prenatal cocaine exposure that environmental factors, gender, and head circumference play a role in the long-term outcome.
Most importantly, this study identifies a direct effect of prenatal cocaine exposure on the adjusted birth head circumference, which in turn directly affects preschool development. This has been a robust finding in this cohort, as we have documented this effect in earlier analyses (Behnke et al., 2002) and now again at age 3. This is similar to the findings of Azuma and Chasnoff (1993) that cocaine influenced IQ scores at age 3 through the head circumference at age 3. The crucial difference is that in our sample, we have found an effect of cocaine on the adjusted birth head circumference, not the head circumference at age 3. Also unlike the Chicago sample, by 1 month of age, children in our sample who were cocaine exposed no longer had a significantly smaller mean head circumference than those who were not cocaine exposed. This finding of no drug group difference in head circumference has held true for our cohort from 1 month through age 3 (Sinha, Behnke, Garvan, & Wobie, 1998). It is yet unknown whether this association between adjusted birth head circumference and outcome represents a direct effect of cocaine at the cellular level, decreasing brain growth and thus head circumference, or whether it is merely a marker for the effect of drugs and other risk factors on overall fetal brain development.
This study also begins to tease out the potential effect of environment on the long-term development and how this factor might be associated with prenatal cocaine exposure. The quality of environment was negatively impacted by caregiver problems, and improved preschool development was associated with better quality of the environment. However, prenatal cocaine use did not directly impact either the caregiver problems or the quality of the environment as we originally hypothesized. It is possible that out-of-home placement plays a role in this finding as over half of the exposed children in our sample no longer live with their biological mother. We speculate that the better scores of the caregivers of the cocaine-exposed children on a few measures may relate to the fact that many of the current guardians are older, perhaps more experienced caregivers. However, our attempts to measure the effect of out-of-home placement by creating a latent variable using the number of caregiver changes during the first 3 years of life did not result in a measurement model with acceptable fit. Thus, this latent variable was dropped from the final model. Further exploration of this important area is ongoing.
Finally, we were interested to discover a relatively large R2 value for the preschool development outcome. This indicated that the final model accounted for 40% of the variance in developmental outcome at age 3. Although prenatal cocaine exposure contributed to the variance through the adjusted birth head circumference, there was an even greater impact in this model of environment on preschool development.
In summary, in this prospective, longitudinal study of prenatal cocaine exposure, we found no direct effects of prenatal cocaine exposure on preschool development at age 3. In addition, there were no direct effects of prenatal cocaine exposure on caregiver problems or the quality of the environment. However, prenatal cocaine exposure directly affected the adjusted birth head circumference, a result that is consistent with that of earlier studies, and thus through this variable had an indirect effect on preschool development at age 3.
Acknowledgments
Supported by the National Institutes of Health, National Institute on Drug Abuse grant RO1-DA05854.
References
- Azuma SD, Chasnoff IJ. Outcome of children prenatally exposed to cocaine and other drugs: A path analysis of three-year data. Pediatrics. 1993;92:396–402. [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development. 2. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Behnke M, Eyler FD, Garvan CW, Wobie K, Hou W. Cocaine exposure and developmental outcome from birth to 6 months. Neurotoxicology and Teratology. 2002;24:283–295. doi: 10.1016/s0892-0362(02)00191-5. [DOI] [PubMed] [Google Scholar]
- Behnke M, Eyler FD, Woods NS, Wobie K, Conlon M. Rural pregnant cocaine users: An in-depth sociodemographic comparison. Journal of Drug Issues. 1997;27:501–524. [Google Scholar]
- Bennett DS, Bendersky M, Lewis M. Children’s intellectual and emotional-behavioral adjustment at 4 years as a function of cocaine exposure, maternal characteristics, and environmental risk. Developmental Psychology. 2002;38:648–658. doi: 10.1037//0012-1649.38.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender PM, Chou CP. Practical issues in structural modeling. Sociological Methods and Research. 1987;16:78–117. [Google Scholar]
- Bradley RH, Caldwell BM. The relationship of infants’ home environments to mental test performance at fifty-four months: A follow-up study. Child Development. 1976;47:1172–1174. [Google Scholar]
- Caldwell BM, Bradley RH. Home observation for measurement of the environment. Little Rock, AR: University of Arkansas Press; 1984. [Google Scholar]
- Day NL, Wagener DK, Taylor PM. Measurement of substance use during pregnancy: Methodologic issues. NIDA Research Monograph. 1985;59:36–47. [PubMed] [Google Scholar]
- Dunst CJ, Jenkins V, Trivette CM. The Family Support Scale: Reliability and validity. Journal of Individual, Family, and Community Wellness. 1984;1:45–52. [Google Scholar]
- Edman SO, Cole DA, Howard GS. Convergent and discriminant validity of FACES III: Family adaptability and cohesion. Family Process. 1990;29:95–103. doi: 10.1111/j.1545-5300.1990.00095.x. [DOI] [PubMed] [Google Scholar]
- Eyler FD, Behnke M, Conlon M, Woods NS, Wobie K. Birth outcome from a prospective, matched study of prenatal crack/cocaine use: I. Interactive and dose effects on health and growth. Pediatrics. 1998;101:229–237. doi: 10.1542/peds.101.2.229. [DOI] [PubMed] [Google Scholar]
- Frank DA, Augustyn M, Knight WG, Pell T, Zuckerman B. Growth, development, and behavior in early childhood following prenatal cocaine exposure: A systematic review. Journal of the American Medical Association. 2001;285:1613–1625. doi: 10.1001/jama.285.12.1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbaud-Wallston J. Dissertation Abstracts International. Vol. 39. 1977. Self-esteem and situational stress: Factors related to sense of competence in new parents; p. 379B. [Google Scholar]
- Green RG, Harris RN, Forte JA, Robinson M. Evaluating FACES III and the Circumplex Model: 2440 families. Family Process. 1991;30:55–73. doi: 10.1111/j.1545-5300.1991.00055.x. [DOI] [PubMed] [Google Scholar]
- Griffith DR, Azuma SD, Chasnoff IJ. Three-year outcome of children exposed prenatally to drugs. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:20–27. doi: 10.1097/00004583-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Hatcher L. A step-by-step approach to using the SAS System for factor analysis and structural equation modeling. Cary, NC: SAS Institute; 1994. [Google Scholar]
- Hoyle R, Panter A. Writing about structural equation models. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues and applications. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Hurt H, Malmud E, Betancourt L, Braitman LE, Brodsky NL, Giannetta J. Children with in utero cocaine exposure do not differ from control subjects on intelligence testing. Archives of Pediatrics and Adolescent Medicine. 1997;151:1237–1241. doi: 10.1001/archpedi.1997.02170490063011. [DOI] [PubMed] [Google Scholar]
- Hurt H, Malmud E, Betancourt LM, Brodsky NL, Giannetta JM. A prospective comparison of developmental outcome of children with in utero cocaine exposure and controls using the Battelle Developmental Inventory. Journal of Developmental and Behavioral Pediatrics. 2001;22:27–34. doi: 10.1097/00004703-200102000-00005. [DOI] [PubMed] [Google Scholar]
- Hurt H, Malmud E, Braitman LE, Betancourt LM, Brodsky NL, Giannetta JM. Innercity achievers: Who are they? Archives of Pediatrics and Adolescent Medicine. 1998;152:993–997. doi: 10.1001/archpedi.152.10.993. [DOI] [PubMed] [Google Scholar]
- Jacobson SW, Jacobson JL, Sokol RJ, Martier SS, Ager JW, Kaplan MG. Maternal recall of alcohol, cocaine, and marijuana use during pregnancy. Neurotoxicology and Teratology. 1991;13:535–540. doi: 10.1016/0892-0362(91)90062-2. [DOI] [PubMed] [Google Scholar]
- Kilbride H, Castor C, Hoffman E, Fuger KL. Thirty-six-month outcome of prenatal cocaine exposure for term or near-term infants: Impact of early case management. Journal of Developmental and Behavioral Pediatrics. 2000;21:19–26. doi: 10.1097/00004703-200002000-00004. [DOI] [PubMed] [Google Scholar]
- Levenson H. Activism and powerful others: Distinctions within the concept of internal-external control. Journal of Personality Assessment. 1974;38:377–383. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- Mule SJ, Casella GA. Confirmation of marijuana, cocaine, morphine, codeine, amphetamine, methamphetamine, phencyclidine by GC/MS in urine following immunoassay screening. Journal of Analytical Toxicology. 1988;12:102–107. doi: 10.1093/jat/12.2.102. [DOI] [PubMed] [Google Scholar]
- Olson DH. Circumplex Model VII: Validation studies and FACES III. Family Process. 1986;25:337–351. doi: 10.1111/j.1545-5300.1986.00337.x. [DOI] [PubMed] [Google Scholar]
- Olson DH. Circumplex Model of Family Systems VIII: Family assessment and intervention. In: Olson DH, Russell CS, Sprenkle DH, editors. Circumplex Model: Systemic assessment and treatment of families. New York: Haworth Press; 1989. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Richardson GA, Conroy ML, Day NL. Prenatal cocaine exposure: Effects on the development of school-age children. Neurotoxicology and Teratology. 1996;18:627–633. doi: 10.1016/s0892-0362(96)00121-3. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Middletown, CT: Wesleyan University Press; 1989. [Google Scholar]
- Sameroff AJ, Feil LA. Parental concepts of development. In: Sigel I, editor. Parental belief Systems: the Psychological consequences for children. Hillsdale: Lawrence Erlbaum; 1986. [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS/STAT user’s guide, Version 6. 4. Vol. 1. Cary, NC: SAS Institute, Inc; 1989. [Google Scholar]
- Sinha I, Behnke M, Eyler FD, Garvan C, Wobie K. Cocaine-exposed children in foster/kinship care: Effects on longitudinal growth patterns. Pediatric Research. 1998;43:1338A. [Google Scholar]
- Sparrow SS, Balla DA, Cicchetti DV. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- Woods NS, Behnke M, Eyler FD, Conlon M, Wobie K. Cocaine use among pregnant women: Socioeconomic, obstetrical, and psychological issues. In: Lewis M, Bendersky M, editors. Mothers, babies, and cocaine: the role of toxins in development. Hillsdale, NJ: Lawrence Erlbaum; 1995. [Google Scholar]