Abstract
Purpose
Pharmacogenetic (PGx) testing can inform drug dosing and selection by aiding in estimating a patient’s genetic risk of adverse response and/or failure to respond. Some PGx tests may generate ancillary clinical information unrelated to the drug treatment question for which testing is done – an informational “side effect.” We aimed to assess public interest and concerns about PGx tests and ancillary information.
Methods
We conducted a random-digit-dial phone survey of a sample of the U.S. public.
Results
We achieved an overall response rate of 42% (n=1,139). When the potential for ancillary information was presented, 85% (±2.82%) of respondents expressed interest in PGx testing, compared to 82% (±3.02%) prior to discussion of ancillary information. Most respondents (89%±2.27%) indicated that physicians should inform patients that a PGx test may reveal ancillary risk information before testing is ordered. Respondents’ interest in actually learning of the ancillary risk finding significantly differed based on disease severity, availability of an intervention, and test validity, even after adjusting for age, gender, education and race.
Conclusion
Under the limited information conditions presented in the survey, the potential of ancillary information does not negatively impact public interest in PGx testing. Interest in learning ancillary information is well-aligned with the public’s desire to be informed about potential benefits and risks prior to testing, promoting patient autonomy.
INTRODUCTION
Genetic variation accounts for 20 to 95% of the variation in individual responses to medications.1 Based on the enhanced understanding of the role of genetic variation in drug response, many drug labels have been revised to include information about the impact of genetic variation on drug response and pharmacogenetic (PGx) testing.2 Specifically, PGx testing can inform therapeutic decision-making through awareness of a patient’s likelihood of an adverse event or responding poorly or not at all to a prescribed medication.
PGx tests have been considered to have fewer ethical and social implications than disease-based genetic testing given the immediate application of the test result to treatment decisions and reduced potential for stigmatization and discrimination.3, 4 One concern, however, is the potential for PGx tests to generate ancillary clinical information unrelated to the drug treatment question for which testing is performed and the associated harms and challenges related to management of the information – an informational “side effect.” Ancillary information may include insights about other disease predispositions, prognosis, and drug responses. For example, the APOE4 allele has been associated with decreased warfarin dose requirements5, 6 and statin response,7, 8 and hence can help guide warfarin dosing or statin selection; this PGx test can also provide information about risk of Alzheimer disease9 or age-related macular degeneration,10 diseases with few preventive interventions or available treatments.
The number of PGx tests that reveal ancillary information is uncertain. One study reported that more than half of validated PGx variants analyzed had an association with disease risk; 16% of the variants were linked with two different diseases, some of which are potentially stigmatizing conditions.11 Incidental findings occurring in other types of medical applications such as imaging present a somewhat comparable issue since highly sensitive imaging techniques generate a high prevalence of incidental findings in some tissues (e.g., kidney and adrenal gland), creating dilemmas for both patients and physicians.12–15
Several factors may contribute to the potential harm or benefit of learning of genetic susceptibility, such as the nature of disease, the test’s predictive value, and availability of interventions or treatment to reduce disease risk.16 While the obligation to disclose ancillary information or inform a patient of its existence will be influenced by legal standards and case law, clinical practice norms will likely be affected by patient expectations and preferences. A proposed framework to address some issues related to the use of PGx tests includes consideration of ancillary information.17 Currently, there are no reported studies about public perspectives regarding ancillary information and its effects on test uptake. We sought to fill this gap by conducting a national survey of the general public about PGx testing and ancillary information. We hypothesized that the public would be interested in being informed of ancillary information prior to deciding to undergo PGx testing given the emphasis on patient autonomy. However, interest in learning of the risk information would be influenced by the level of risk, the availability of a treatment/intervention for the disease, disease severity, and the accuracy of the predicted risk. We anticipate the data from this study will be helpful in informing physician practices regarding disclosure of ancillary information, potentially informing development of clinical guidelines regarding the management of such information.
MATERIALS AND METHODS
Survey Development
We developed a survey to explore public attitudes regarding PGx testing and the role ancillary information might play in decisions to undergo such tests. The survey questions were developed based on data collected from focus groups, a literature review, and a legal analysis of managing ancillary findings. Four focus groups were convened to explore public perceptions and attitudes about PGx testing, and specifically about the impact of ancillary information. We defined ancillary information for the focus group participants as “extra information such as your risk of developing a disease,” and that it was most likely “not related to your current health.” We then discussed a fictional case about an asthma patient who has PGx testing to predict her risk of a serious adverse effect associated with a new medication that her doctor wishes to prescribe; the PGx test could also reveal her risk of colon cancer. Many participants believed that their physician should disclose the potential of ancillary information prior to testing, however, their desire to actually learn of that information varied based on the whether an intervention was available and potential psychological burden (data unpublished). Although not a nationally representative sample, the focus groups served to increase our understanding of public attitudes toward PGx testing and ancillary information and inform development of the survey instrument.
Survey Pilot
As described elsewhere,18 piloting and administration of the survey was led by the Survey Research Unit at the University of North Carolina, Chapel Hill. A pretest was conducted in August 2009 with 52 North Carolina residents to evaluate the quality of the computer-assisted telephone interviewing (CATI) programming and appropriateness of the content for telephone administration. The final survey contained 52 questions in five major categories: 1) demographics; 2) personal/family experience with prescription medications; 3) knowledge of genetic testing; 4) interest in PGx testing given certain risks and uses of testing; and 5) attitudes towards management of ancillary information revealed by PGx testing. We report here data regarding attitudes towards management of ancillary information; see ref. 18 for other survey findings.
Sampling methods
In summary, a stratified random digit dial sample of 20,848 telephone numbers in the U.S. was selected for this survey. Eligibility was based on reaching a household with an English-speaking resident 18 years of age or older. Households were classified as non-responsive (eligible but no interview; n=1,010), ineligible (non-residential numbers, non-English speaking households, or head of household under 18 years of age; n=14,335), or unknown (eligibility never verified; n=4,364). If more than one eligible adult resided in the household, one was randomly selected for participation via a computer-generated algorithm. We calculated a response rate of 42% (n=1139) based on the standards and definitions set by the American Association of Public Opinion Research.19
Data Collection
The survey was conducted from September 17 to November 20, 2009. A CATI interview software package (Blaise 4.6, 2003) was used to assist interviewers in the administration of the survey and to manage all call attempts. At least 12 call attempts were made per each telephone number at various times of the day and week. For quality control, all interviewers were monitored periodically and written feedback provided. This study was approved by the Institutional Review Boards at Duke University Medical Center and the University of North Carolina, Chapel Hill.
Data Analysis
Respondents tended to be older, White, and female to a greater extent than would be expected by chance alone. To correct for such sample imbalances and reduce the potential effects of bias, the survey data were adjusted by age (18–34, 35–54, 55 & older), White and non-White, and gender based on normative data from the 2008 American Community Survey.20 Questions using a 4-point Likert scale were dichotomized into “likely and “unlikely.” For logistic regression analyses, model building was based on hypothetically-related covariates with adjustment for demographic characteristics; final variable selection was conducted using the backward selection approach. Odds ratios and corresponding 95% confidence intervals were computed; significance level of 0.05 was used for all statistical tests. To adjust for control variables, Cochran-Mantel-Haenszel (CMH) test was applied when comparing two groups on a binary response. All analyses were conducted in SAS (Version 9.1.3 using Proc Frequency, Proc Logistic & Proc Regression).
RESULTS
Respondent Characteristics
After adjustment, respondents were 51% female, 78% White, and between the ages of 34–55 years (38%).18 Forty-two percent of respondents had a college degree or higher. In addition, the majority of respondents had some type of health insurance (86%), predominantly provided through their employer (75%). Forty-seven percent had experienced a side effect from a prescription drug; of those, 80% had stopped taking the drug of their own accord or by physician’s orders. Seventy-nine percent of respondents characterized their health status as excellent or good, comparable to national reports of self-rated health status.21, 22 Eighty percent of respondents had heard of genetic testing; 54% of those that had heard of genetic testing indicated they understood the uses of genetic testing ‘very well’ or ‘somewhat well.’
Disclosure of Potential Ancillary Information
We described to respondents how some PGx tests may reveal “additional” information, not related to their current condition using the following situational context: “Before having some minor surgery, your doctor wishes to order a genetic test to determine how much pain medication to give you. Because genes perform many jobs, the genetic test results may show other information in addition to drug response information your doctor needs. For example, the genetic drug response test may also show your risk for developing a certain disease during your lifetime.”
Overall, 89% (±2.27%) of respondents indicated that physicians should inform patients that a PGx test may reveal ancillary risk information unrelated to their current condition before a decision about PGx testing is made. Respondents who believed a doctor should inform patients about ancillary information prior to testing were more likely to have testing to predict drug response after hearing about the potential uses of PGx testing (OR=3.59, p<0.0001, 95% CI [2.12, 6.04]). No statistically significant relationships were detected between disclosure of potential for ancillary information prior to testing and age, education, race, health insurance status, health status, or being affected (self or family member) with a chronic condition.
Interest in Learning Ancillary Risk Information
We then asked respondents about their interest in learning of six potential types of ancillary risk information: 1) risk for a disease considered minor but treatable such as gum disease; 2) risk for a disease considered serious but treatable such as heart disease; 3) risk for a disease considered serious but untreatable such as dementia or Alzheimer’s; 4) risk for a disease that would not develop for at least 10 years; 5); a disease with a moderately low risk; and 6) risk that was unclear and uncertain. “Interest” was defined as “extremely interested” or “somewhat interested” in PGx testing. Respondents’ interest in learning of the different types of ancillary information ranged from a low of 69% (ancillary information of uncertain risk, ±3.40%) to a high of 96% (±1.23%) for risk of serious but treatable disease (Figure 1). Interest level was found to be significantly different between the ancillary risk information scenarios, even after adjusting for age, gender, education and race (CMH statistic of general association: 144.70, p<0.0001).
Figure 1.
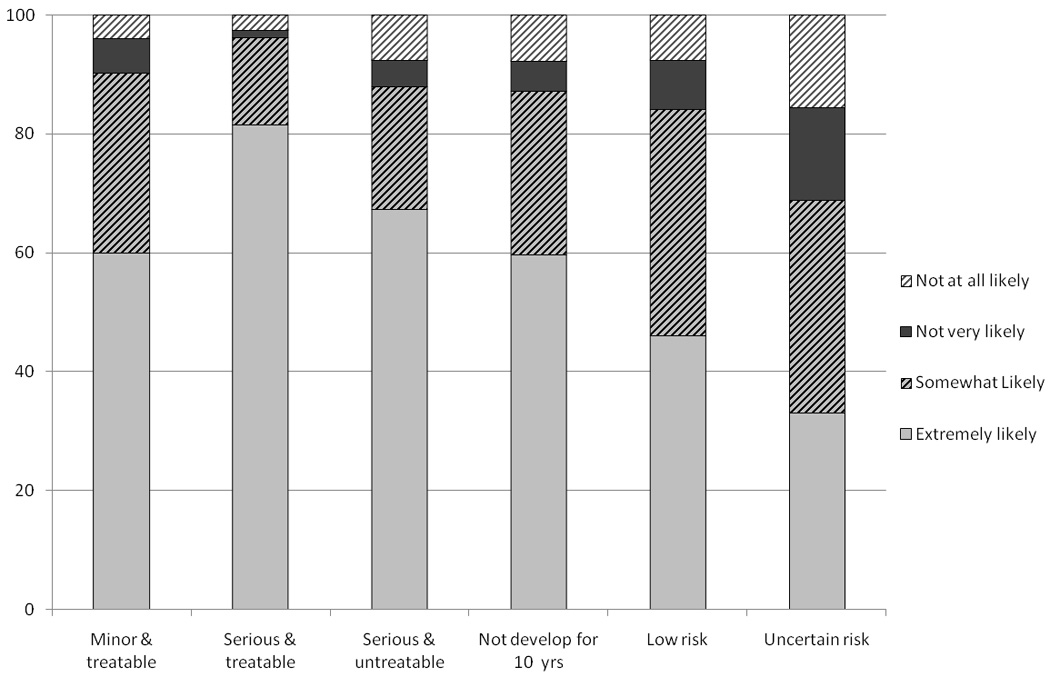
Survey respondents’ interest in learning of various types of ancillary risk information revealed by PGx testing. Interest level was significantly different between the ancillary information scenarios, even after adjusting for age, gender, education and race (based on Cochran-Mental-Haenszel test, p<0.0001).
Factors Associated with Interest in Learning Ancillary Risk Information
Women were less interested in learning of the ancillary risk information for four of the six scenarios presented: minor but treatable disease, serious but treatable disease, moderately low disease risk, and uncertain or unknown disease risk (Table 1). Respondents with a college degree were less likely to be interested in learning of ancillary risk information for serious and untreatable disease and diseases with uncertain risk. A history of side effects increased interest in only one scenario – for a minor but treatable disease. As compared to non-White respondents, White respondents were less likely to indicate interest in learning of a moderately low disease risk or uncertain disease risk.
Table 1.
Comparison of respondent characteristics with interest in learning of six different types of ancillary risk information, OR [95% CI]
| Minor & treatable |
Serious & treatable |
Serious & untreatable |
Would not develop for 10 years |
Moderately low disease risk |
Uncertain risk |
|
|---|---|---|---|---|---|---|
|
Age Group 2 vs. 1 (35–54 years vs. 18– 34 years) |
1.09, [0.67, 1.80] |
0.89, [0.40, 1.95] |
1.33, [0.86, 2.07] |
0.77, [0.48, 1.23] |
0.86, [0.58, 1.29] |
0.83, [0.60, 1.15] |
|
Age Group 3 vs. 1 (+55 years vs. 18– 34 years) |
0.86, [0.52, 1.42] |
0.65, [0.30, 1.44] |
1.58, [0.97, 2.56] |
0.64, [0.39, 1.04] |
0.98, [0.63, 1.51] |
0.98, [0.69, 1.40] |
|
Education (At least a college degree vs. Less than a college degree) |
1.22, [0.79, 1.89] |
1.65, [0.82, 3.33] |
0.63, [0.43, 0.94] p=0.02 |
1.02, [0.68, 1.54] |
0.83, [0.58, 1.17] |
0.64, [0.48, 0.85] p=0.002 |
|
Race (White vs. Non- White) |
0.71, [0.42, 1.20] |
0.67, [0.29, 1.53] |
0.71, [0.44, 1.16] |
1.17, [0.75, 1.80] |
0.61, [0.39, 0.96] p=0.03 |
0.40, [0.27, 0.58] p<0.0001 |
| Sex (F vs. M) | 0.61, [0.40, 0.92] p=0.02 |
0.42, [0.22, 0.83] p=0.01 |
1.06, [0.73, 1.53] |
1.07, [0.74, 1.54] |
0.70, [0.50, 0.98] p=0.04 |
0.58, [0.44, 0.76] p<0.0001 |
|
Self-Rated Health Status (Excellent/Good vs. Fair/Poor) |
0.65, [0.36, 1.15] |
0.53, [0.21, 1.34] |
1.05, [0.64, 1.72] |
0.85, [0.53, 1.37] |
0.77, [0.49, 1.21] |
0.75, [0.52, 1.08] |
|
History of Side Effects (Yes vs. No) |
1.62, [1.07, 2.47] p=0.02 |
1.87, [0.97, 3.63] |
1.09, [0.75, 1.60] |
1.12, [0.77, 1.63] |
1.03, [0.73, 1.44] |
1.30, [0.99, 1.71] |
|
Awareness of Genetic testing (Aware vs. Not aware) |
1.26, [0.77, 2.07] |
1.28, [0.61, 2.69] |
1.34, [0.85, 2.13] |
2.47, [1.65, 3.70] p<0.0001 |
1.34, [0.89, 2.03] |
0.81, [0.57, 1.16] |
Impact of Potential Ancillary Information on Overall Interest in PGx testing
Prior to introduction of the potential for ancillary information and the different types of ancillary information, 82% (±3.02%) of respondents expressed strong interest in PGx testing after learning of some of the general risks and uses of testing.18 After learning of the potential for and the different types of ancillary information, 85% (±2.82%) of respondents indicated that they would be extremely or somewhat likely to have PGx testing. After adjusting for age, level of education, race and sex, interest in PGx testing increased significantly when compared to interest assessed after learning of potential risks only (CMH statistic of general association: 162.62, p<0.0001) and risks and potential uses (CMH statistic of general association: 358.95, p<0.0001).
DISCUSSION
The management of ancillary information from PGx testing raises many issues for both physicians and patients. From the patient perspective, questions arise as to whether patients should be informed about ancillary information prior to testing, their desire to learn of the risk information, and what factors influence these decisions. In addition, the potential of ancillary findings unrelated to the drug treatment question for which testing is performed may impact patient and physician interest in these tests. Physician enthusiasm for PGx testing for smoking cessation treatments has been reported to be lessened by the potential for ancillary risk information, especially for stigmatizing conditions.23–25 We found this was not the case for the general public; interest in PGx testing remained high after respondents were informed about the potential for ancillary information. The high interest suggests that the public is more interested in PGx testing than their physicians might anticipate and do not consider ancillary information to be a major drawback of testing, and may, in some cases, consider it an added benefit.
Most respondents felt physicians should inform patients about potential ancillary information prior to PGx testing. The strong interest in being informed prior to testing is in line with the increasingly active role of patients in the decision-making process for medical care.26 However, disclosure of ancillary information leaves uncertainties with respect to informed consent standards of liability. For example, what types of ancillary information should the patient be informed about prior to their decision to undergo PGx testing – any type of ancillary information or only that for diseases with available interventions?
If ancillary risk information for untreatable or potentially stigmatizing conditions could be revealed by a PGx test, such as Alzheimer’s disease5–9 or mental illness,11 the test may be considered “high” risk requiring a detailed consent process.4, 27 It is not only the existence of ancillary information, but the characteristics of that information that would dictate the appropriate level of consent.28 Furthermore, in addition to discussing the potential of the ancillary information prior to making a decision to undergo PGx testing, it may be prudent to also discuss the potential benefits and harms of learning of the information. For example, potential clinical follow-up of ancillary risks may lead to costly and/or potentially risky interventions.29–31 In research settings, some scholars have recommended that the potential for ancillary information should be disclosed to research subjects during the informed consent.32 While informed consent is standard practice for most clinical research studies, it is not routinely obtained for PGx testing in general,33 particularly for tests considered standard of care,34, 35 and therefore, would result in a major change in practice.
Although most respondents wished to know about ancillary information prior to testing, interest in learning of the information varied between respondents. Some of this variability may be attributed to differences in interpretation of the descriptors used in the survey (serious versus moderate risk), or treatable. In addition, our presentation of risk (i.e., low) could have influenced respondents’ interest given that different ways of presenting risk (numerical risks such as relative risk versus descriptive risks) can impact response and understanding.36 As it was not feasible to ask about their interest in ancillary information based on a combination of factors that would be disclosed in an actual clinical situation (e.g., level of uncertainty and availability of treatment and disease characteristics), we might expect even greater differences in attitudinal responses. Such limited information scenarios may account for differences between higher expressed levels of interest and lower rates of actual test uptake37, 38 as well as disparities in physician and public attitudes regarding ancillary information.
Not surprisingly, respondents were most interested in learning of risks for serious but treatable diseases and least interested in learning of uncertain risks. College graduates were the only group who were less likely to want to learn of their risk for serious but untreatable diseases. Two possible reasons that may account for this finding are fear of discrimination or desire to avoid potential anxiety and stress. A recent study of personalized genomic risk assessments reported that 82% would want to know of risks for serious diseases that could not be prevented.39
Women were less likely to want to learn of ancillary risks for several scenarios. These findings comport with previous work suggesting that women have greater dread of risks,40 and specifically, greater concerns about personalized genomic risk assessments.39 Positive carrier test results for women have also been shown to result in greater anxiety than for positive male carriers,41, 42 perhaps due to the greater perceived value and benefits of testing for women given the implications for reproductive decision-making.43 The trend toward not wanting to learn of certain types of ancillary risk appears in contrast with the understanding that women are typically active health information seekers.44 Women pre-dominantly make most of the health care decisions for themselves and family members,45 based on a combination of personal values, beliefs, and past experiences.46 Perceived lack of control has been associated with failure to partake in some beneficial health behaviors,47 but this reasoning does not explain our finding that women were less interested in genomic-based risk for treatable diseases (mild or serious) compared to untreatable. Few studies have examined interest or experience in genetic risk information for serious, non-treatable disease. A study involving APOE genotyping for Alzheimer’s risk in individuals with a family history of Alzheimer reported that a high proportion of interested participants were female and well-educated,48 suggesting that treatability may only be one criterion considered when deciding to learn of such risk information.
As PGx testing progresses in clinical practice, it is essential to consider the consequences of informational side effects for the patient and their care. The issue of ancillary or incidental findings, particularly in genome research,49 has garnered recent attention due to the volumes of data that can be generated in a single study from sequencing or other technology platforms and concerns about how the data should be appropriately managed.50–52 The strong interest in learning about ancillary information is well-aligned with the public’s desire to be informed about benefits and risks of testing, thus empowering them with the autonomy to make an informed decision about testing. Awareness of the potential for ancillary information may be considered material to patients’ decisions about PGx testing. However, despite their interest, from an ethical and legal perspective, it is still uncertain whether all types of ancillary information should be disclosed. Thus, further study is warranted to examine the types of ancillary information that should be disclosed to patients during discussion of PGx testing, whether patients choose to learn of the information and the benefits and harms associated with learning it, and the delivery of ancillary information.
Acknowledgement
This work was supported by the National Institutes of Health (R01 GM081416-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Evans WE, McLeod HL. Pharmacogenomics--drug disposition, drug targets, and side effects. N Engl J Med. 2003 Feb 6;348(6):538–549. doi: 10.1056/NEJMra020526. [DOI] [PubMed] [Google Scholar]
- 2.Frueh FW, Amur S, Mummaneni P, et al. Pharmacogenomic biomarker information in drug labels approved by the United States food and drug administration: prevalence of related drug use. Pharmacotherapy. 2008 Aug;28(8):992–998. doi: 10.1592/phco.28.8.992. [DOI] [PubMed] [Google Scholar]
- 3.Roses AD. Pharmacogenetics and the practice of medicine. Nature. 2000 Jun 15;405(6788):857–865. doi: 10.1038/35015728. [DOI] [PubMed] [Google Scholar]
- 4.Robertson JA. Consent and privacy in pharmacogenetic testing. Nat Genet. 2001 Jul;28(3):207–209. doi: 10.1038/90032. [DOI] [PubMed] [Google Scholar]
- 5.Visser LE, Trienekens PH, De Smet PA, et al. Patients with an ApoE epsilon4 allele require lower doses of coumarin anticoagulants. Pharmacogenet Genomics. 2005 Feb;15(2):69–74. doi: 10.1097/01213011-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Sconce EA, Daly AK, Khan TI, Wynne HA, Kamali F. APOE genotype makes a small contribution to warfarin dose requirements. Pharmacogenet Genomics. 2006 Aug;16(8):609–611. doi: 10.1097/01.fpc.0000220567.98089.b5. [DOI] [PubMed] [Google Scholar]
- 7.Ordovas JM, Lopez-Miranda J, Perez-Jimenez F, et al. Effect of apolipoprotein E and A-IV phenotypes on the low density lipoprotein response to HMG CoA reductase inhibitor therapy. Atherosclerosis. 1995 Mar;113(2):157–166. doi: 10.1016/0021-9150(94)05439-p. [DOI] [PubMed] [Google Scholar]
- 8.Gerdes LU, Gerdes C, Kervinen K, et al. The apolipoprotein epsilon4 allele determines prognosis and the effect on prognosis of simvastatin in survivors of myocardial infarction : a substudy of the Scandinavian simvastatin survival study. Circulation. 2000 Mar 28;101(12):1366–1371. doi: 10.1161/01.cir.101.12.1366. [DOI] [PubMed] [Google Scholar]
- 9.Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science. 1993 Aug 13;261(5123):921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 10.Thakkinstian A, Bowe S, McEvoy M, Smith W, Attia J. Association between apolipoprotein E polymorphisms and age-related macular degeneration: A HuGE review and meta-analysis. Am J Epidemiol. 2006 Nov 1;164(9):813–822. doi: 10.1093/aje/kwj279. [DOI] [PubMed] [Google Scholar]
- 11.Henrikson NB, Burke W, Veenstra DL. Ancillary risk information and pharmacogenetic tests: social and policy implications. Pharmacogenomics J. 2008 Apr;8(2):85–89. doi: 10.1038/sj.tpj.6500457. [DOI] [PubMed] [Google Scholar]
- 12.Orme NM, Fletcher JG, Siddiki HA, et al. Incidental findings in imaging research: evaluating incidence, benefit, and burden. Arch Intern Med. 2010 Sep 27;170(17):1525–1532. doi: 10.1001/archinternmed.2010.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ravine D, Gibson RN, Donlan J, Sheffield LJ. An ultrasound renal cyst prevalence survey: specificity data for inherited renal cystic diseases. Am J Kidney Dis. 1993 Dec;22(6):803–807. doi: 10.1016/s0272-6386(12)70338-4. [DOI] [PubMed] [Google Scholar]
- 14.Grumbach MM, Biller BM, Braunstein GD, et al. Management of the clinically inapparent adrenal mass ("incidentaloma") Ann Intern Med. 2003 Mar 4;138(5):424–429. doi: 10.7326/0003-4819-138-5-200303040-00013. [DOI] [PubMed] [Google Scholar]
- 15.Nawar R, Aron D. Adrenal incidentalomas -- a continuing management dilemma. Endocr Relat Cancer. 2005 Sep;12(3):585–598. doi: 10.1677/erc.1.00951. [DOI] [PubMed] [Google Scholar]
- 16.Post SG, Whitehouse PJ, Binstock RH, et al. The clinical introduction of genetic testing for Alzheimer disease. An ethical perspective. JAMA. 1997 Mar 12;277(10):832–836. doi: 10.1001/jama.277.10.832. [DOI] [PubMed] [Google Scholar]
- 17.Haga SB, Burke W. Pharmacogenetic testing: not as simple as it seems. Genet Med. 2008 Jun;10(6):391–395. doi: 10.1097/GIM.0b013e31817701d4. [DOI] [PubMed] [Google Scholar]
- 18.Haga S, O'Daniel J, Tindall G, Lipkus IM, Agans R. Survey of U.S. Public Attitudes Towards Pharmacogenetic Testing. The Pharmacogenomics Journal. doi: 10.1038/tpj.2011.1. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 7th ed. Lenexa, Kansas: AAPOR; 2011. [Google Scholar]
- 20.US Census Bureau. American Community Survey 2008. [Accessed June, 2010];2008 http://www.census.gov/acs/www/
- 21.Zahran HS, Kobau R, Moriarty DG, Zack MM, Holt J, Donehoo R. Health-related quality of life surveillance--United States, 1993–2002. MMWR Surveill Summ. 2005 Oct 28;54(4):1–35. [PubMed] [Google Scholar]
- 22.Self-rated fair or poor health among adults with diabetes--United States, 1996–2005. MMWR Morb Mortal Wkly Rep. 2006 Nov 17;55(45):1224–1227. [PubMed] [Google Scholar]
- 23.Levy DE, Youatt EJ, Shields AE. Primary care physicians' concerns about offering a genetic test to tailor smoking cessation treatment. Genet Med. 2007 Dec;9(12):842–849. doi: 10.1097/gim.0b013e31815bf953. [DOI] [PubMed] [Google Scholar]
- 24.Park ER, Kleimann S, Pelan JA, Shields AE. Anticipating clinical integration of genetically tailored tobacco dependence treatment: perspectives of primary care physicians. Nicotine Tob Res. 2007 Feb;9(2):271–279. doi: 10.1080/14622200601078574. [DOI] [PubMed] [Google Scholar]
- 25.Shields AE, Levy DE, Blumenthal D, et al. Primary care physicians' willingness to offer a new genetic test to tailor smoking treatment, according to test characteristics. Nicotine Tob Res. 2008 Jun;10(6):1037–1045. doi: 10.1080/14622200802087580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kon AA. The shared decision-making continuum. JAMA. 2010 Aug 25;304(8):903–904. doi: 10.1001/jama.2010.1208. [DOI] [PubMed] [Google Scholar]
- 27.Buchanan A, Califano A, Kahn J, McPherson E, Robertson J, Brody B. Pharmacogenetics: ethical issues and policy options. Kennedy Inst Ethics J. 2002 Mar;12(1):1–15. doi: 10.1353/ken.2002.0001. [DOI] [PubMed] [Google Scholar]
- 28.Haga S. Pharmacogenomics: Applicaitons to Patient Care. Second Edition. United States of America: American College of Clinical Pharmacy; 2009. Ethical, legal, and social challenges to applied pharmacogenetics. [Google Scholar]
- 29.NIH state-of-the-science statement on management of the clinically inapparent adrenal mass ("incidentaloma"). NIH Consens State Sci Statements. 2002 Feb 4–6;19(2):1–25. [PubMed] [Google Scholar]
- 30.Stone JH. Incidentalomas--clinical correlation and translational science required. N Engl J Med. 2006 Jun 29;354(26):2748–2749. doi: 10.1056/NEJMp058264. [DOI] [PubMed] [Google Scholar]
- 31.Silverman SG, Israel GM, Herts BR, Richie JP. Management of the incidental renal mass. Radiology. 2008 Oct;249(1):16–31. doi: 10.1148/radiol.2491070783. [DOI] [PubMed] [Google Scholar]
- 32.Wolf SM, Paradise J, Caga-anan C. The law of incidental findings in human subjects research: establishing researchers' duties. J Law Med Ethics. 2008 Summer;36(2):361–383. 214. doi: 10.1111/j.1748-720X.2008.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woelderink A, Ibarreta D, Hopkins MM, Rodriguez-Cerezo E. The current clinical practice of pharmacogenetic testing in Europe: TPMT and HER2 as case studies. Pharmacogenomics J. 2006 Jan#x02013;Feb;6(1):3–7. doi: 10.1038/sj.tpj.6500341. [DOI] [PubMed] [Google Scholar]
- 34.Hedgecoe A. 'At the point at which you can do something about it, then it becomes more relevant': informed consent in the pharmacogenetic clinic. Soc Sci Med. 2005 Sep;61(6):1201–1210. doi: 10.1016/j.socscimed.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 35.Hedgecoe AM. Context, ethics and pharmacogenetics. Stud Hist Philos Biol Biomed Sci. 2006 Sep;37(3):566–582. doi: 10.1016/j.shpsc.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making. 2007 Sep–Oct;27(5):696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 37.Persky S, Kaphingst KA, Condit CM, McBride CM. Assessing hypothetical scenario methodology in genetic susceptibility testing analog studies: a quantitative review. Genet Med. 2007 Nov;9(11):727–738. doi: 10.1097/gim.0b013e318159a344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ropka ME, Wenzel J, Phillips EK, Siadaty M, Philbrick JT. Uptake rates for breast cancer genetic testing: a systematic review. Cancer Epidemiol Biomarkers Prev. 2006 May;15(5):840–855. doi: 10.1158/1055-9965.EPI-05-0002. [DOI] [PubMed] [Google Scholar]
- 39.Bloss CS, Ornowski L, Silver E, et al. Consumer perceptions of direct-to-consumer personalized genomic risk assessments. Genet Med. 2010 Sep;12(9):556–566. doi: 10.1097/GIM.0b013e3181eb51c6. [DOI] [PubMed] [Google Scholar]
- 40.Savage I. Demographic influences on risk perceptions. Risk Anal. 1993 Aug;13(4):413–420. doi: 10.1111/j.1539-6924.1993.tb00741.x. [DOI] [PubMed] [Google Scholar]
- 41.Axworthy D, Brock DJ, Bobrow M, Marteau TM. Psychological impact of population-based carrier testing for cystic fibrosis: 3-year follow-up. UK Cystic Fibrosis Follow-Up Study Group. Lancet. 1996 May 25;347(9013):1443–1446. doi: 10.1016/s0140-6736(96)91683-9. [DOI] [PubMed] [Google Scholar]
- 42.Marteau TM, Dundas R, Axworthy D. Long-term cognitive and emotional impact of genetic testing for carriers of cystic fibrosis: the effects of test result and gender. Health Psychol. 1997 Jan;16(1):51–62. doi: 10.1037//0278-6133.16.1.51. [DOI] [PubMed] [Google Scholar]
- 43.Shiloh S, Saxe L. Perception of risk in genetic counseling. Psychology & Health. 1989;3(1):45–61. [Google Scholar]
- 44.Warner D, Procaccino JD. Toward wellness: Women seeking health information. Journal of the American Society for Information Science and Technology. 2004;55(8):709–730. [Google Scholar]
- 45.Ignagni K. Women's primary health care and the search for quality--panel discussion. Women's Health Issues. 2001;11(4):309–313. doi: 10.1016/s1049-3867(01)00095-0. [DOI] [PubMed] [Google Scholar]
- 46.Brown JB, Carroll J, Boon H, Marmoreo J. Women's decision-making about their health care: views over the life cycle. Patient Educ Couns. 2002 Dec;48(3):225–231. doi: 10.1016/s0738-3991(02)00175-1. [DOI] [PubMed] [Google Scholar]
- 47.MacInnes JD. The illness perceptions of women following acute myocardial infarction: implications for behaviour change and attendance at cardiac rehabilitation. Women Health. 2005;42(4):105–121. doi: 10.1300/j013v42n04_06. [DOI] [PubMed] [Google Scholar]
- 48.Roberts JS, Barber M, Brown TM, et al. Who seeks genetic susceptibility testing for Alzheimer's disease? Findings from a multisite, randomized clinical trial. Genet Med. 2004 Jul–Aug;6(4):197–203. doi: 10.1097/01.gim.0000132688.55591.77. [DOI] [PubMed] [Google Scholar]
- 49.Johnson AD, Bhimavarapu A, Benjamin EJ, et al. CLIA-tested genetic variants on commercial SNP arrays: potential for incidental findings in genome-wide association studies. Genet Med. 2010 Jun;12(6):355–363. doi: 10.1097/GIM.0b013e3181e1e2a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kohane IS, Masys DR, Altman RB. The incidentalome: a threat to genomic medicine. JAMA. 2006 Jul 12;296(2):212–215. doi: 10.1001/jama.296.2.212. [DOI] [PubMed] [Google Scholar]
- 51.Cho MK. Understanding incidental findings in the context of genetics and genomics. J Law Med Ethics. 2008 Summer;36(2):280–285. 212. doi: 10.1111/j.1748-720X.2008.00270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Ness B. Genomic research and incidental findings. J Law Med Ethics. 2008 Summer;36(2):292–297. 212. doi: 10.1111/j.1748-720X.2008.00272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


