Abstract
Retropharyngeal calcific tendinitis is defined as inflammation of the longus colli muscle and is caused by the deposition of calcium hydroxyapatite crystals, which usually involves the superior oblique fibers of the longus colli muscle from C1-3. Diagnosis is usually made by detecting amorphous calcification and prevertebral soft tissue swelling on radiograph, CT or MRI. In this report, we introduce a case of this disease which was misdiagnosed as a retropharyngeal tuberculous abscess, or a muscle strain of the ongus colli muscle. No calcifications were visible along the vertical fibers of the longus colli muscle. The lesion was located anterior to the C4-5 disc, in a rheumatoid arthritis patient with atlantoaxial subluxation. Calcific tendinitis of the longus colli muscle at this location in a rheumatoid arthritis patient has not been reported in the English literature.
Keywords: Calcific tendinitis, Longus colli muscle, Magnetic resonance imaging (MRI), Computed tomography (CT), Rheumatoid arthritis
INTRODUCTION
Retropharyngeal calcific tendinitis is an uncommon benign process caused by calcium hydroxyapatite deposition and inflammation in the longus colli muscle (LCM), which is located on the anterior surface of the vertebral body, extending from the atlas to the third thoracic vertebra (1, 2). Clinical presentation of retropharyngeal calcific tendinitis is often characterized by non-specific symptoms such as acute or subacute neck pain, dysphagia or odynophagia, and low grade fever. Laboratory tests may demonstrate mild leukocystosis and slightly elevated erythrocyte sedimentation rate (ESR) (2). This set of conditions can easily be misdiagnosed due to their rather non-specific presentation and rare occurrence (2). Diagnosis is usually based on the recognition of amorphous calcification anterior to C1-3, and prevertebral soft tissue swelling on plain radiographs and computed tomography (CT) (1, 3-5). This is the first report of acute retropharyngeal calcific tendinitis with calcification anterior to the C4-5 disc and prevertebral fluid collection in a rheumatoid arthritis (RA) patient with atlantoaxial subluxation (AAS).The patient gave consent for data concerning the case to be published.
CASE REPORT
A 30-year-old woman was admitted to hospital principally complaining of severe neck pain and dysphagia over the course of one day prior. The woman was diagnosed with rheumatoid arthritis (RA) six years earlier, which had been well controlled with prednisolone and hydroxychloroquine and had no history of recent trauma or upper respiratory tract infection. On the day of admission, a physical examination revealed a tender cervical spine with severely limited range of motion in all directions. The pain was exacerbated by the action of swallowing and motion of the cervical spine. No mass or adenopathy was noted on either side of the neck. The mucosa of the oropharynx and nasopharynx were intact, without erythema or edema, and the patient was afebrile. Neurological findings were also normal. Laboratory tests revealed a white blood cell count of 9.0 × 103/mm3 (4.0-10.0 × 103) with a normal differential. The patient's C-reactive protein (CRP) level and ESR had risen to 1.4 mg/dL (0-0.3) and 47 mm/h (normal 0-22), respectively from 0.03 mg/dL and ESR 35 mmg/h, respectively, three months prior. Plain radiographs of the cervical spine (Fig. 1A) demonstrated AAS and soft-tissue swelling from C1 to C4 levels without definite calcification along the anterior border of the cervical spine. The next morning, magnetic resonance imaging (MRI) of the cervical spine (Fig. 1B-D) revealed prominent prevertebral soft tissue swelling with fluid collection from C1 to C6, as well as AAS, a small amount of fluid collection in the atlantoaxial joint, and bony erosions in the odontoid process. In addition, no definite evidence of calcification could be seen along the LCM in the cervical spine on the initial plain radiographs and MRI, and there was no osteomyelitis involving the atlas and axis on MRI. Possible differential diagnoses included tuberculous infection of the atlantoaxial joint, and strain of the LCM in conjunction with instability or acute retropharyngeal calcific tendinitis.
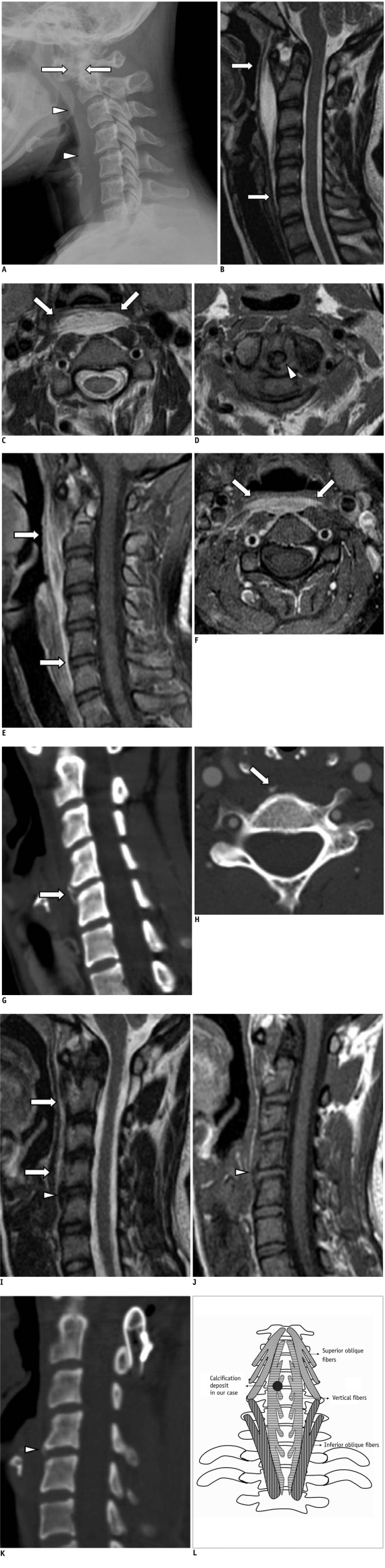
Fig. 1.
Acute retropharyngeal calcific tendinitis in 30-year-old woman.
A. Initial plain radiograph showing atlantoaxial subluxation (arrows) and prevertebral soft tissue swelling (arrowheads). There is no evidence of calcification along anterior border of the cervical spine. B, C. Sagittal (B) and axial T2-weighted (C) images show prominent prevertebral soft tissue swelling and fluid collection at C1-6 (arrows). D. Axial T1-weighted image at level C1-2 shows bony erosion in odontoid process (arrowhead). E, F. Enhanced sagittal (E) and axial T1-weighted (F) images with fat suppression showing markedly decreased amounts of fluid collection and prevertebral soft tissue swelling (arrows) after just 10 hours. G, H. Sagittal reformatted (G) and axial (H) images showing amorphous calcification (arrows) at right para-midline location anterior to C4-5 disc. I, J. Follow-up sagittal T2-weighted (I) and T1-weighted (J) MR images revealing minimal amounts of fluid collection (arrows) and minor low signal intensity calcification (arrowheads) anterior to C4-5 disc. K. Follow-up sagittal reformatted CT image after two months demonstrating almost complete resolution of calcification anterior to C4-5 disc (arrowhead). L. Anatomical illustration of longus colli muscles and site of retropharyngeal calcific tendinitis.
On the night of admission, an additional contrast enhanced MRI examination was carried out (Fig. 1E, F) to exclude the possibilities of retropharyngeal infection and strain. Contrast-enhanced T1-weighted MRI with fat suppression showed a significant reduction in the amount of prevertebral fluid collection, with peripheral enhancement in the prevertebral region of the cervical spine. Thus, the possibilities of tuberculous infection and strain could be excluded.
On the third day of admission, non-contrast and contrast CT scans of the cervical spine (Fig. 1G, H) were performed to exclude the possibility of retropharyngeal calcific tendinitis. CT scans demonstrated soft-tissue swelling and nodular calcification in the right para-midline LCM at the C4-5 disc (vertical fibers of the LCM). On the fourth day of admission, follow-up MRI (Fig. 1I, J) revealed a minimal amount of prevertebral fluid collection along the LCM. The patient's symptoms resolved rapidly with pain control by non-steroidal anti-inflammatory drugs (NSAIDs) over three days, along with a reduction in the CRP level (CRP 0.9 mg/dL). No microorganisms were cultured.
Two months later, a follow-up CT of the cervical spine (Fig. 1K) revealed a reduction in the size of calcification nodule anterior to the C4-5 disc. Based on the successive changes, namely rapid symptom improvement and rapid reduction of the calcification nodule in the anterior border of the C4-5 disc, the diagnosis was acute retropharyngeal calcific tendinitis in an unusual location of an RA patient.
DISCUSSION
Acute retropharyngeal calcific tendinitis of the LCM is a clinical syndrome that was first described by Hartley in 1964 (6). It occurs most frequently from the third to the sixth decades of life (7). Symptoms may include mild fever, which may be secondary to inflammation of the surrounding soft tissues. Laboratory data are usually normal, although inflammatory changes may be observed (8). The origin of the calcium hydroxyapatite crystal deposition observed in calcific tendinitis is still not entirely clear. This disease entity seems to be associated with certain genetic and metabolic circumstances, and the possible risk factors include chronic trauma, inflammation, and tendinous degeneration (9).
The LCM is an uncommon location for calcific tendinitis. Therefore, a diagnostic evaluation of the more common causes of neck pain, which include but are not limited to trauma, inflammation, infection, and neoplasia, should always be performed before the possibility of calcific tendinitis is considered (10). The LCM is located in the prevertebral space, extending from the anterior tubercle of the atlas to its inferior attachments at T3. It consists of the superior oblique, vertical, and inferior oblique fibers (11). The superior oblique fibers originate from the anterior tubercles of the transverse processes of C3-5 and insert by a tendon into the anterior tubercle on the ventral arch of the atlas. The vertical fibers arise from the bodies of C5-T3 and insert into the bodies of C2-4. The inferior oblique fibers originate from the bodies of T1-3 and insert into the anterior tubercles of the transverse processes of C5-6 (12). Cervical spine radiographs usually reveal calcification anterior to the C1-3 bodies and the prevertebral soft tissues, and this is a typical finding of calcific tendinitis of the LCM. However, calcification may not be evident on an initial plain radiograph, as illustrated in our patient, and only diffuse soft-tissue swelling in the prevertebral C1-4 area may provide a clue for diagnosis. Also, as illustrated in our patient, calcification may be evident on the right para-midline anterior to the C4-5 disc. Our case shows that calcifications causing retropharyngeal calcific tendinitis can occur in the right vertical fibers of the LCM (Fig. 1L).
By identifying calcifications, CT may be more helpful for diagnosis than MRI, and MRI may be more useful for demonstrating soft tissue edema or fluid collection, and may reveal marrow edema in the adjacent vertebrae (1). The symptom of neck pain was important in our RA patient because the cervical spine is involved in 30-50% of patients with RA. The pathological lesions of RA include chronic inflammation of the synovial membrane, bone erosion, and weakening of ligament insertions. These can lead to instability, with potential impingement by AAS on the spinal cord. Radiographic imaging in our patient showed AAS and pannus in the atlantoaxial joint with bony erosion involving the odontoid process. To our knowledge, this is the first report describing calcific tendinitis involving an unusual location of the LCM in a patient with RA and AAS.
Acute calcific tendinitis of the LCM is a self-limiting condition that resolves spontaneously after 1-2 weeks. Conservative treatment combined with, for example with NSAIDs or analgesics, and immobilization, can provide symptomatic relief. Apart from the typical calcification involving the LCM, and soft-tissue swelling, rapid improvement of all symptoms with conservative treatment can confirm the diagnosis of acute calcific tendinitis of the LCM.
In conclusion, we describe the first case of retropharyngeal calcific tendinitis anterior to the C4-5 disc, which is an unusual location, in a patient with RA and AAS. We suggest that in RA patients with AAS, a cervical spine CT must be performed to exclude the possibility of retropharyngeal calcific tendinitis, even though the calcification may not be seen or may be unusually located in the prevertebral space.
References
- 1.Mihmanli I, Karaarslan E, Kanberoglu K. Inflammation of vertebral bone associated with acute calcific tendinitis of the longus colli muscle. Neuroradiology. 2001;43:1098–1101. doi: 10.1007/s002340100644. [DOI] [PubMed] [Google Scholar]
- 2.Chung T, Rebello R, Gooden EA. Retropharyngeal calcific tendinitis: case report and review of literature. Emerg Radiol. 2005;11:375–380. doi: 10.1007/s10140-005-0427-y. [DOI] [PubMed] [Google Scholar]
- 3.Offiah CE, Hall E. Acute calcific tendinitis of the longus colli muscle: spectrum of CT appearances and anatomical correlation. Br J Radiol. 2009;82:e117–e121. doi: 10.1259/bjr/19797697. [DOI] [PubMed] [Google Scholar]
- 4.Southwell K, Hornibrook J, O'Neill-Kerr D. Acute longus colli calcific tendonitis causing neck pain and dysphagia. Otolaryngol Head Neck Surg. 2008;138:405–406. doi: 10.1016/j.otohns.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Smith RV, Rinaldi J, Hood DR, Troost T. Hydroxyapatite deposition disease: an uncommon cause of acute odynophagia. Otolaryngol Head Neck Surg. 1996;114:321–323. doi: 10.1016/S0194-59989670195-X. [DOI] [PubMed] [Google Scholar]
- 6.Hartley J. Acute Cervical Pain Associated with Retropharyngeal Calcium Deposit. A Case Report. J Bone Joint Surg Am. 1964;46:1753–1754. [PubMed] [Google Scholar]
- 7.Kaplan MJ, Eavey RD. Calcific tendinitis of the longus colli muscle. Ann Otol Rhinol Laryngol. 1984;93:215–219. doi: 10.1177/000348948409300305. [DOI] [PubMed] [Google Scholar]
- 8.Diaw AM, De Maeseneer M, Shahabpour M, Machiels F, Osteaux M. Calcium hydroxyapatite deposition disease of the neck: finding in three patients. J Belge Radiol. 1998;81:73–74. [PubMed] [Google Scholar]
- 9.De Maeseneer M, Vreugde S, Laureys S, Sartoris DJ, De Ridder F, Osteaux M. Calcific tendinitis of the longus colli muscle. Head Neck. 1997;19:545–548. doi: 10.1002/(sici)1097-0347(199709)19:6<545::aid-hed13>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 10.Fahlgren H. Retropharyngeal tendinitis: three probable cases with an unusually low epicentre. Cephalalgia. 1988;8:105–110. doi: 10.1046/j.1468-2982.1988.0802105.x. [DOI] [PubMed] [Google Scholar]
- 11.Hall FM, Docken WP, Curtis HW. Calcific tendinitis of the longus coli: diagnosis by CT. AJR Am J Roentgenol. 1986;147:742–743. doi: 10.2214/ajr.147.4.742. [DOI] [PubMed] [Google Scholar]
- 12.Park SY, Jin W, Lee SH, Park JS, Yang DM, Ryu KN. Acute retropharyngeal calcific tendinitis: a case report with unusual location of calcification. Skeletal Radiol. 2010;39:817–820. doi: 10.1007/s00256-010-0879-3. [DOI] [PubMed] [Google Scholar]