Abstract
Introduction:
This study examined the pathways from smoking policies in the home (no ban, partial ban, and total ban on smoking) to psychological well-being (e.g., self-esteem) and psychological symptoms (e.g., depressive symptoms) as mediated by a healthy lifestyle (engaging in exercise, eating healthful foods, and sleeping enough) and cigarette smoking among a sample of urban Black and Puerto Rican Americans.
Methods:
Questionnaire data were collected from 816 participants (mean age = 32 years). Structural equation modeling (SEM) was employed to examine the pathways of restrictions on smoking in the home to a healthy lifestyle, cigarette smoking, psychological well-being, and psychological distress.
Results:
The SEM showed mediational pathways linking higher levels of restrictions on smoking in the home with a healthy lifestyle, which in turn was related negatively to psychological distress and positively to psychological well-being. Higher levels of restrictions on smoking in the home were also related inversely to cigarette smoking, which was related positively to psychological distress and negatively to psychological well-being.
Conclusions:
Findings show that higher levels of restrictions on smoking in the home are associated with a healthier lifestyle and less cigarette smoking, which in turn are associated with better psychological functioning. Greater restrictions on smoking in the home may thus support positive lifestyle choices, including exercise and nutrition, as well as psychological functioning.
Introduction
Restrictions on smoking in occupational and recreational settings have been expanded in the past decades (Eriksen & Chaloupka, 2007; Mills, Messer, Gilpin, & Pierce, 2009; Shields, 2007). Increasingly, individuals, including smokers, also place voluntary restrictions on smoking in their homes (Centers for Disease Control and Prevention [CDC], 2007; Levy, Romano, & Mumford, 2004), most likely due to growing social awareness about the health hazards of environmental tobacco smoke (ETS). According to the CDC (2007), the prevalence of smoke-free households nationwide increased from 43.2% during the period from 1992 to 1993 to 72.2% in 2003. This proliferation of homes that maintain a complete ban on smoking seems to have contributed to favorable smoking-related outcomes, including a reduction in exposure to ETS among children and nonsmoking adults (Gonzales, Malcoe, Kegler, & Espinoza, 2006).
However, the benefits of smoking restrictions may vary by socioeconomic status and ethnicity. For example, a recent study found that residential smoking restrictions in a sample of urban low-income Black mothers were not related to their children's ETS exposure nor did they relate to the mother's intention to quit smoking (Collins et al., 2010). Black and Latino Americans also seem to experience the most serious health consequences as a result of tobacco use and ETS (CDC, 1998; Forno & Celedón, 2009). For instance, the overall prevalence of current childhood asthma in the United States is 8.7% (Forno & Celedón, 2009). However, among Black and Latino Americans, the prevalence rates are 12.7% and 19.2%, respectively (Forno & Celedón, 2009). Thus, the study of benefits associated with smoking restrictions in the home and their association with well-being among urban Black and Latino Americans is of particular concern to public health.
In general, smoking restrictions have been found to result in less cigarette smoking among adults (Clark et al., 2006; Farkas, Gilpin, Distefan, & Pierce, 1999; Shavers et al., 2006). Smoking restrictions also increase the odds of quit attempts among smokers (Gilpin, White, Farkas, & Pierce, 1999; Pizacani et al., 2004; Shields, 2007) and decrease the odds of adolescents experimenting with cigarettes (e.g., Albers, Biener, Siegel, Cheng, & Rigotti, 2008; Proescholdbell, Chassin, & MacKinnon, 2000; Schultz, Nowatzki, Dunn, & Griffith, 2010; Szabo, White, & Hayman, 2006). Furthermore, young adults who grow up in parental households where smoking is banned are more likely to set up/move into independent living quarters that are smoke-free as well (Albers, Biener, Siegel, Cheng, & Rigotti, 2009). Smoking restrictions in the home may also prevent relapse among former smokers (Shields, 2007).
Restrictions on smoking in the home may also be related to better psychological health as smoking is related to psychological symptoms, notably depression and anxiety (Boden, Fergusson, & Horwood, 2010; Degenhardt & Hall, 2001). In addition, it is possible that living in a home with rules against smoking may heighten individuals’ awareness about their health and thus support the adoption of a healthy lifestyle that not only excludes smoking but also includes healthy nutrition, exercise, and sleeping habits. Less exposure to smoke and a healthier lifestyle, in turn, may contribute to greater psychological well-being (Hamer, Stamatakis, & Batty, 2010; Wainwright et al., 2007). Thus, the benefits of introducing smoking restrictions in one's home may extend to other areas of health. The main goal of this study was thus to empirically test the hypothesis that smoking restrictions in the home are related to engaging in a healthy lifestyle and, ultimately, to greater psychological well-being.
Support for this hypothesis is provided by research, which suggests that people tend to make improvements in several health behaviors (i.e., eating nutritious food, exercising, reducing substance use) concurrently (Unger, 1996). Implementation of one health-related behavior (here, introducing a smoking ban) may facilitate the adoption of other health behaviors (e.g., eating better food, exercising). For example, one study of middle-aged women found that those who had quit smoking reported higher levels of exercise and taking in a healthier diet (Perkins et al., 1993).
Another study, applying the transtheoretical model (Prochaska & DiClemente, 1992), found that participants in the advanced stages of smoking cessation demonstrated more healthful behaviors than those in earlier stages (Unger, 1996). According to this model, individuals’ willingness to change their health behaviors can be classified into five stages along a continuum (precontemplation, contemplation, preparation, action, and maintenance). Unger's study, which examined the relationship between stages of smoking cessation and alcohol use, exercise, and safe driving practices, found that smokers who were not even considering quitting (i.e., precontemplators) also scored lower on other health behaviors. Specifically, precontemplators reported taking in more drinks per occasion than all other groups, binge-drank more frequently than all other groups, and exercised less than actors and maintainers (Unger, 1996). These findings show that not being willing to give up cigarette use is related to other health-compromising behaviors. Conversely, contemplating and preparing to quit smoking (by introducing restrictions in one's home) may not only reduce cigarette use but also effect a positive change in other health behaviors.
A healthy lifestyle, in turn, is related to greater psychological well-being and experiencing less psychological distress. Several investigators have reported that a healthy lifestyle including exercise, sufficient sleep, and a healthful diet is related to fewer psychological symptoms, such as anxiety and depression (De Moor, Beem, Stubbe, Boomsma, & De Gues, 2006; Dunn, Trivedi, Kampert, Clark, & Chambliss, 2005). A healthy lifestyle is also related to psychological well-being, including greater life satisfaction and higher levels of self-esteem (Rejeski & Mihalko, 2001; Spence, McGannon, & Poon, 2005).
A greater understanding of the range of potential benefits associated with placing restrictions on smoking in the home might result in a greater number of individuals adopting smoking bans at home. This study therefore examined the relationship of household smoking restrictions (i.e., no ban, partial ban, complete ban on smoking in the home) with other “unexpected” beneficial outcomes, specifically engaging in a healthy lifestyle (including exercising, eating healthful foods, and getting sufficient sleep) and psychological adjustment (fewer psychological symptoms and greater well-being).
Our hypotheses for the current study were as follows: (a) The relationship between restrictions on smoking in the home and symptoms of psychological distress and psychological well-being would be mediated by the individual's engaging in a healthy lifestyle, (b) there would be a mediational path between smoking restrictions in the home and symptoms of psychological distress via the individual's smoking, (c) a healthy lifestyle would be directly related to lower levels of psychological symptoms and higher levels of psychological well-being, (d) smoking would be related to higher levels of psychological symptoms and reduced psychological well-being, and (e) there would be an inverse relationship between psychological symptoms and psychological well-being. (f) We also expected that there would be an inverse relationship between engaging in a healthy lifestyle and cigarette smoking.
Methods
Participants
Data for this cross-sectional study came from the fifth wave (T5) of the Harlem Longitudinal Development Study, a longitudinal study of urbanBlack and Puerto Rican young adults (N = 816). The present analysis included only data collected at T5 because this wave was the only one during which participants were asked about smoking restrictions in their homes. The mean age of the sample at T5 was 32.6 (SD = 1.4; range: 26.5–38.7 years). The sample was 48.5% Black and 51.5% Puerto Rican. Sixty percent of the sample was female. The mean number of people living in the household, including the participant, was 3.25 (SD = 1.7) and 3.57 (SD = 1.5) for Black and Puerto Rican participants, respectively. Additional sample characteristics are presented in Table 1 separately by ethnicity. A description of the longitudinal sample through T4 can be found elsewhere (Brook, Pahl, & Ning, 2006).
Table 1.
Sample Characteristics for Black and Puerto Rican Young Adults (N = 816)
| Black, n (%) | Puerto Rican, n (%) | |
| Gender | ||
| Female | 250 (63.1) | 242 (57.6) |
| Male | 146 (36.9) | 178 (42.4) |
| Single | 245 (61.9) | 240 (57.3) |
| Marital status | ||
| Married | 126 (31.8) | 145 (34.6) |
| Divorced | 24 (6.1) | 33 (7.9) |
| Widowed | 1 (0.2) | 1 (0.2) |
| Living arrangementa | ||
| With spouse or partner | 188 (47.6) | 250 (59.5) |
| With relatives (parents, siblings, and/or other relatives) | 110 (27.8) | 68 (16.2) |
| With nonrelatives | 28 (7.1) | 29 (6.9) |
| Alone | 60 (15.2) | 29 (6.9) |
| Lives with child | ||
| Yes | 223 (56.5) | 284 (67.6) |
| No | ||
| Educational level | ||
| 12th grade or below | 123 (31.1) | 228 (54.3) |
| Business or technical school | 21 (5.3) | 17 (4.1) |
| Attended college | 146 (36.9) | 119 (28.3) |
| Bachelor's degree | 69 (17.4) | 40 (9.5) |
| Postgraduate business, law, medical, master, or doctoral program | 37 (9.3) | 16 (3.8) |
| Household smoking ban | ||
| No restrictions | 34 (8.6) | 19 (4.5) |
| Some restrictions | 142 (36.0) | 168 (40. 1) |
| Complete ban | 219 (55.4) | 232 (55.4) |
| Smoking status in the past thirty days | ||
| No smoking | 297 (75.0) | 277 (66.0) |
| Smoking | 99 (25.0) | 143 (34.0) |
| Partner smokes | ||
| Yes | 108 (27.5) | 128 (30.6) |
| No | 286 (72.6) | 291 (69.4) |
| Lives with partner who smokes | ||
| Yes | 44 (11.2) | 80 (19.1) |
| No | 349 (88.8) | 339 (80.9) |
Note. aCategories are not exclusive.
Procedures
The sample was originally selected from Grades 7–10 in school districts serving the East Harlem area of New York City. The objective was to constitute a sample of urban Black and Puerto Rican adolescents. Data were collected by trained interviewers who were matched on sex and ethnicity whenever possible. Participants were reimbursed for the participation in the study ($75.00). The Institutional Review Board at New York University School of Medicine approved all procedures for the study's data collection.
Measures
Smoking restrictions in the home and healthy lifestyle were manifest variables, while psychological symptoms and psychological well-being were latent variables.
Smoking Restrictions in the Home
This variable reflected the current policies about smoking in the respondents’ homes (Al-Delaimy et al., 2008; Schultz et al., 2010). Responses to the question: “What are the smoking rules or restrictions in your household, if any?” included (a) no restrictions (“there are no restrictions on smoking”), (b) some restrictions on smoking (e.g., “smoking is allowed in some rooms only” or “smoking is generally banned for everyone, with a few exceptions”), and (c) a complete ban on smoking (“smoking is completely banned for everyone”; Gilpin et al., 1999; Schultz et al., 2010).
Cigarette Smoking
This dichotomous variable reflected the participant's smoking status in the past thirty days (1 = current smoking; 0 = no current smoking).
Healthy Lifestyle
This variable consisted of 10 questions asking about the frequency of health-related behaviors, including nutrition, exercise, and sleeping habits (Johnston, Bachman, O’Malley, & Schulenberg, 2006). Sample items included “how often do you exercise vigorously,” “how often do you eat at least some green vegetables,” and “how often do you get at least 7 hours of sleep?” Answering options ranged from 0 = never to 5 = every day. Cronbach's alpha for this scale was α = .76.
Psychological Symptoms
This latent variable consisted of three multiitem scales, which assessed the frequency of psychological symptoms. They included (a) depression (α = .76), a six-item scale that asked about the frequency of depressed affect (e.g., “feeling hopeless”); (b) anxiety (α = .77), a three-item scale that inquired about the frequency of symptoms of anxiety (e.g., “feeling fearful”); and (c) interpersonal difficulties (α = .80), a scale that assessed the frequency of interpersonal problems reported by the participant (e.g., “feeling easily irritated or annoyed”). Response options for all three scales ranged from not at all (0) to extremely (4). All three scales were adapted from the Hopkins Symptoms Checklist (Derogatis, 1977).
Psychological Well-Being
This latent variable consisted of three multiitem scales, which reflected a sense of well-being and psychological adjustment. Adult Transitions (α = .67) was a nine-item scale assessing the participant's success at achieving certain milestones of adulthood (e.g., “Have you been able to establish financial independence?”). Answering options were 0 = no and 1 = yes. The scale summed all questions that were answered affirmatively. The self-esteem scale consisted of four items (α = .67) adapted from Rosenberg's Self-Esteem Scale (Rosenberg, 1965). A sample item read “you feel that your life is very useful.” Response options ranged from “always false” (1) to “always true” (4). Life satisfaction, a 13-item scale (α = .87), adapted from Endicott, Nee, Harrison, and Blumenthal (1993), assessed the participant's satisfaction with a number of areas in his/her life, including relationships, financial situation, and physical and psychological health. Sample items included “Over the last few years, how satisfied have you been with your mood,” “ … social relationships,” and “ … financial status?” Response options ranged from “not at all satisfied” (1) to “very satisfied” (5).
Data Analyses
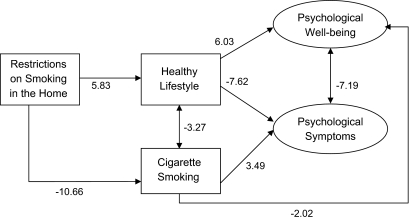
We used structural equation modeling (SEM) to test our hypothesized model illustrated in Figure 1. SEM is a regression-based technique that allows for the empirical validation of hypothesized relationships between hypothetical latent constructs (Kline, 2010). A latent construct cannot be observed directly but is represented by manifest (observed) variables. SEM allows multiple measures to be associated with a single latent construct (Card & Little, 2007; Kline, 2010). One of the major of advantages of SEM is that it can produce unbiased estimates by adjusting for measurement error (Card & Little, 2007). SEM estimates a system of linear equation simultaneously and can model direct, indirect, mediated, and moderated relationships between variables (Card & Little, 2007).
Figure 1.
Pathways from restrictions on smoking in the home to psychological well-being and psychological symptoms (N = 816). Note. (1) Comparative fit index = 0.98; root mean squared error of approximation = 0.057. (2) Ethnicity, gender, and status of living with children were statistically controlled.
Using the MPlus software (Muthén & Muthén, 2010), we tested the hypothesized measurement and conceptual models. In order to account for the influences of the participants’ gender, ethnicity, and status of living with children on the measurement and structural models, we used partial covariance matrices as the input matrices, which were created by statistically partialling out the effects of these demographic factors on each of the original manifest variables. According to Newcomb and Bentler (1988), this strategy allows one to statistically control for the effects of these variables without hypothesizing exactly where they influence the model. The correlations among the variables derived from the covariance matrices are available from the authors. We employed maximum likelihood methods to estimate the models. We chose two fit indices to assess the fit of the models: (a) Bentler's comparative fit index (CFI); and (b) the root mean squared error of approximation (RMSEA; Bentler, 1990). According to Kelloway (1998), for the CFI, values between 0.90 and 1.0 indicate that the model provides a good fit for the data; for the RMSEA, values lower than 0.06 indicate a good fit.
Results
Preliminary Analyses
As shown in Table 1, just over half of both Black and Puerto Rican participants reported a complete smoking ban in their homes. However, a higher percentage of Black than Puerto Rican participants reported no restrictions on smoking their homes, and a higher percentage of Puerto Rican than Black participants reported a partial ban on smoking (χ2 = 6.1, p < .05). More Puerto Rican than Black participants tobacco use in the past thirty days (χ2 = 8.0, p < .01). In addition, among those who reported living with their partners, more Puerto Rican than Black participants reported that their partner smoked (χ2 = 3.9, p < .05).
Structural Equation Modeling
We tested the measurement model as well as the structural model, controlling for the participants’ ethnicity and status of living with children. For the measurement model, all factor loadings were statistically significant (p < .0001). The following fit indices were obtained: CFI = 0.98 and RMSEA = 0.057. These results reflect a satisfactory model fit. For the structural model, standardized parameter estimates, z statistics for the sample, are presented in Figure 1. All z tests were statistically significant at p < .05 or less.
As shown in Figure 1, the data were consistent with the hypothesized model. Specifically, our findings suggested that smoking restrictions in the home were positively related to the participants’ healthy lifestyles (z = 5.82), which in turn were positively related to the participants’ psychological well-being (z = 6.03) and negatively associated with their reports of psychological symptoms (z = −7.62). Smoking restrictions in the home were also negatively related to the participants’ current cigarette smoking (z = −10.66), which in turn was associated with their psychological symptoms (z = 3.49) and negatively associated with their psychological well-being (z = −2.02). There was a negative correlation between a healthy lifestyle and cigarette smoking (z = −3.27),
Discussion
To our knowledge, this is the first study to examine the relationship of smoking restrictions in the home with its psychological concomitants, psychological symptoms, and psychological well-being in a community sample of urban Black and Puerto Rican young adults. The study is also unique because (a) it focused on the psychological concomitants of smoking restrictions in the home (i.e., psychological symptoms and psychological well-being) and (b) it examined engaging in a healthy lifestyle and cigarette smoking as mediators of the relationship between smoking restrictions in the home and psychological adjustment as proposed by a conceptual model (Figure 1).
The results of our preliminary analyses showed that the percentage of smoke-free homes in this sample of urban Black and Puerto Rican young adults was lower than the national average of smoke-free homes reported by the CDC (2007; 55% compared with 72%). Given evidence that urban Black and Latino Americans seem to experience disproportionately severe consequences as a result of ETS (e.g., CDC, 1998; Perera et al., 2002; Wilson, Kahn, Khoury, & Lanphear, 2005), this finding constitutes an important concern for public health.
The results of our SEM support our hypothesized model and suggest two major pathways from smoking restrictions in the home to psychological symptoms and well-being. The first pathway indicates that smoking restrictions at home are associated with both psychological well-being and less psychological distress via engaging in a healthy lifestyle, including exercise, a healthful diet, and getting enough sleep. The second pathway demonstrates that greater restrictions on smoking in the home are negatively related to smoking, which in turn is linked with more psychological symptoms and less psychological well-being. As expected, psychological symptoms and psychological well-being were inversely related.
The pathway between smoking restrictions in the home and lower levels of tobacco use is consistent with other studies finding a link between restrictions on smoking in the household and lower levels of smoking (Clark et al., 2006; Gilpin et al., 1999; Pizacani et al., 2004). Thus, maintaining a smoke-free home seems to be an effective tool for reducing cigarette smoking among urban Black and Puerto Rican young adults. Research has established that restricting smoking in the home decreases the risk of being a smoker (Clark et al., 2006) and supports smoking cessation attempts (Gilpin et al., 1999; Pizacani et al., 2004). Home smoking bans also decrease the likelihood of adolescent smoking (Albers et al., 2008; Fisher, Winickoff, Camargo, Colditz, & Frazier, 2007; Proescholdbell et al., 2000; Schultz et al., 2010; Szabo et al., 2006). A ban on smoking in the household not only creates a concrete barrier to using tobacco but also gives support to those who are attempting to quit smoking by creating an environment, which is free of stimuli that may trigger the desire to smoke (Mills et al., 2009). Thus, introducing a ban on smoking at home, for smokers, may be considered part of the preparation stage as defined by the transtheoretical model (Prochaska & DiClemente, 1992).
The negative relationship between cigarette smoking and psychological symptoms, most notably anxiety and depression, has also been demonstrated repeatedly (Breslau, Peterson Schultz, Chilcoat, & Andreski, 1998; Campo-Arias, Martinez, & Rueda-Jaimes, 2004). Nicotine addiction and related withdrawal symptoms can lead to an increased number of psychological symptoms, including anxiety and depression (West & Hajek, 1997). Additionally, the impaired respiratory functioning associated with smoking such as wheezing and shortness of breath (Moore, Augustson, Moser, & Budney, 2005) and the anxiogenic effects of sustained nicotine intake can give rise to symptoms of anxiety (Pine et al., 2000; West & Hajek, 1997).
Smokers may also experience greater difficulties in social relationships because of their smoking. As smoking continues to become less acceptable, smokers experience an increase in negative reactions to their smoking. This may create actual conflict in relationships or increase smokers’ perceptions of conflict. Woolf, Rothemich, Johnson, and Marsland (1999) also found that smokers reported lower levels of social functioning and role functioning than did nonsmokers. Furthermore, higher levels of smoking are associated with indices of poor psychological well-being, such as reporting lower levels of life satisfaction and failing to make transitions to adult roles (e.g., getting married; Chassin, Presson, Pitts, & Sherman, 2000; Nystedt, 2006).
An important finding of this research was that stricter rules about smoking in the home were related to fewer psychological symptoms and psychological well-being via engaging in a healthy lifestyle, including exercise, a healthful diet, and getting enough sleep. This relationship suggests the existence of a “generalization effect” of attitudes and behaviors toward health, whereby becoming aware of the health benefits of one behavior (here, restricting smoking in one's home) may “spill over” into other areas of one's life (Perkins et al., 1993; Unger, 1996). “Individuals in the process of improving one health behavior may be more receptive to information about health and more willing to change their attitudes and behaviors relative to another domain of health” (Unger, 1996, p. 134). Living in a smoke-free environment with clear antismoking rules may give rise to a greater awareness about health issues among smokers and nonsmokers alike. This awareness may encompass not only the benefits of refraining from tobacco use but also the health benefits of engaging in exercise, adhering to a healthy diet, and sleeping an adequate number of hours every night.
The relationship between exercise, good nutrition, and sleep and better psychological adjustment has been demonstrated repeatedly. Numerous investigators have shown that a healthy lifestyle, incorporating regular exercise, sufficient sleep, and healthy nutrition, is related to fewer symptoms of psychological distress (De Moor et al., 2006; Dunn et al., 2005; Tsuno, Besset, & Ritchie, 2005). In particular, many studies have shown that exercise is related to lower levels of depressive symptoms (e.g., Dunn et al., 2005; Nabkasorn et al., 2005). A healthy lifestyle is also associated with greater psychological well-being (e.g., self-esteem and life satisfaction; Rejeski & Mihalko, 2001; Spence et al., 2005).
The mechanisms linking a healthy lifestyle with better psychological functioning are likely physical as well as psychological in nature. For example, neuroendocrine changes and endorphin release have been suggested as explanations for the reduction in depression observed with regular exercise (Ferrauti, Neumann, Weber, & Keul, 2001). Similar mechanisms are likely to be operative linking nutrition and sufficient sleep with subjective feelings of well-being and fewer symptoms of distress. In addition, given growing awareness of the benefits of regular exercise and a healthful diet, it is likely that engaging in a healthy lifestyle confers psychological benefits (e.g., higher levels of self-esteem, greater life satisfaction) by providing a sense of accomplishment to the individual. A sense of increased self-efficacy and mastery may result from engaging in a healthy lifestyle (Nabkasorn et al., 2005).
Limitations
The results reported here must be interpreted in light of several limitations. First, psychological functioning is predicted not only by the constructs under investigation in this study (i.e., restrictions of smoking in the home, a healthy lifestyle, and cigarette smoking) but also by factors not included in this study, such as other environmental as well as genetic factors. Second, the sample for this study was exclusively Black and Puerto Rican, thus limiting the generalizability of our findings to these populations. Third, the test of our cross-sectional model can only present relations among the variables studied but cannot prove causality. Alternative pathways must also be considered. For example, it is possible that adopting a healthier lifestyle may lead individuals to ban smoking in their homes. However, there are several points in support of the model we presented in this research. First, introducing smoking restrictions in one's house is often the very first step people take in adopting a healthier lifestyle (followed by attempting cessation; Okah, Choi, Okuyemi, & Ahluwalia, 2002; Pizacani et al., 2008; Shields, 2007). This is probably a direct result of increased antitobacco legislation, policies, and media campaigns that have been put into place in recent years (Haw & Gruer, 2007; Levy et al., 2004). Second, alternative statistical models that placed a healthy lifestyle before household restrictions on smoking did not fit the data better than our hypothesized model. Given the focus of this research to examine other “unexpected” correlates of smoking restrictions in the home, we decided to place the smoking restrictions construct as antecedent to reduced tobacco use, a healthy lifestyle, and psychological distress and well-being.
Conclusions
The strength of this study is the finding that the benefits of placing smoking restrictions in one's home may go beyond a reduction in tobacco use and ETS by influencing both other health behaviors (exercise, sleep, and nutrition) and psychological functioning among Black and Puerto Rican young adults. If individuals become aware of these less obvious benefits of introducing smoking restrictions into their homes, they may be more willing to take this important step in creating a healthier environment for themselves and their families, thereby reducing the risks (e.g., asthma) associated with ETS. This is of particular importance among Blacks and Latinos as they seem to suffer particularly severe consequences as a result of exposure to ETS (CDC, 1998; Perera et al., 2002; Wilson et al., 2005). The dissemination of these findings by clinicians, public health advocates, and smoking cessation experts is therefore of vital importance in contributing to the expansion of smoke-free environments in urban Black and Latino communities.
Funding
This study was supported by the National Cancer Institute (Grant #CA084063) awarded to JSB and KP and the National Institute on Drug Abuse (Research Scientist Award #K05 DA00244) awarded to JSB.
Declaration of Interests
None declared.
References
- Al-Delaimy WK, White MM, Trinidad DR, Messer K, Gilmer T, Zhu SH, et al. The California Tobsacco Control Program: Can we maintain the progress? Results from the California Tobacco Survey, 1990–2005. 2008. Retrieved from http://www.cdph.ca.gov/programs/tobacco/Documents/CTCP-CTSReport1990-2005.pdf. [Google Scholar]
- Albers AB, Biener L, Siegel M, Cheng DM, Rigotti N. Household smoking bans and adolescent antismoking attitudes and smoking initiation: Findings from a longitudinal study of a Massachusetts youth cohort. American Journal of Public Health. 2008;98:1886–1893. doi: 10.2105/AJPH.2007.129320. doi:10.2105/AJPH.2007.129320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers AB, Biener L, Siegel M, Cheng DM, Rigotti NA. Impact of parental home smoking policies on policy choices of independently living young adults. Tobacco Control. 2009;18:245–248. doi: 10.1136/tc.2008.025478. doi:10.1136/tc.2008.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. doi:10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Cigarette smoking and depression: Tests of causal linkages using a longitudinal birth cohort. British Journal of Psychiatry. 2010;196:440–446. doi: 10.1192/bjp.bp.109.065912. doi:10.1192/bjp.bp.109.065912. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking. American Journal of Public Health. 1998;55:161–166. doi: 10.1001/archpsyc.55.2.161. doi:10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- Brook JS, Pahl K, Ning Y. Peer and parental influences on longitudinal trajectories of smoking among African Americans and Puerto Ricans. Nicotine & Tobacco Research. 2006;28:639–651. doi: 10.1080/14622200600789627. doi:10.1080/14622200600789627. [DOI] [PubMed] [Google Scholar]
- Campo-Arias A, Martinez LA, Rueda-Jaimes GE. Anxiety and depressive symptoms among smokers: A population study. MedUNAB. 2004;7:4–8. Retrieved from http://revistas.unab.edu.co/index.php?journal=medunab. [Google Scholar]
- Card NA, Little TD. Studying aggression with structural equation modeling. In: Flannery DJ, Vazsonyi AT, Waldman ID, editors. The Cambridge handbook of violent behavior and aggression. New York: Cambridge University Press; 2007. pp. 727–739. [Google Scholar]
- Centers for Disease Control and Prevention. Tobacco use among U.S. racial/ethnic groups—African Americans, American Indian and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1998. Retrieved from http://www.cdc.gov/tobacco/data_statistics/sgr/1998/complete_report/index.htm. [Google Scholar]
- Centers for Disease Control and Prevention. State-specific prevalence of smoke-free home rules—United States, 1992–2003. Journal of the American Medical Association. 2007;298:169–170. doi:10.1001/jama.298.2.169. [Google Scholar]
- Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: Multiple trajectories and their psychosocial correlates. Health Psychology. 2000;19:223–231. doi:10.1037//0278-6133.19.3.223. [PubMed] [Google Scholar]
- Clark PI, Schooley MW, Pierce B, Schulman J, Hartman AM, Schmitt CL. Impact of home smoking rules on smoking patterns among adolescents and young adults. Preventing Chronic Disease. 2006;3:1–13. Retrieved from http://www.cdc.gov/pcd/ [PMC free article] [PubMed] [Google Scholar]
- Collins BN, Ibrahim JK, Hovell M, Tolley NM, Nair US, Jaffe K, et al. Residential smoking restrictions are not associated with reduced child SHS exposure in a baseline sample of low-income, urban African Americans. Health. 2010;2:1264–1271. doi: 10.4236/health.2010.211188. doi:10.4236/health.2010.211188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Moor MHM, Beem AL, Stubbe JH, Boomsma DI, De Gues IJC. Regular exercise, anxiety, depression and personality: A population-based study. Preventive Medicine. 2006;42:273–279. doi: 10.1016/j.ypmed.2005.12.002. doi:10.1016/j.ypmed.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W. The relationship between tobacco use, substance-use disorders and mental health: Results from the National Survey of Mental Health and Well-Being. Nicotine & Tobacco Research. 2001;3:225–234. doi: 10.1080/14622200110050457. doi:10.1080/14622200110050457. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring and procedures manual. Baltimore, MD: Clinical Psychometric Institute; 1977. [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: Efficacy and dose response. American Journal of Preventive Medicine. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. doi:10.1016/S0197-2456(02)00226-X. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacology Bulletin. 1993;29:321–326. Retrieved from http://www.medworksmedia.com/ [PubMed] [Google Scholar]
- Eriksen M, Chaloupka F. The economic impact of clean indoor air laws. Cancer Journal for Clinicians. 2007;57:367–378. doi: 10.3322/CA.57.6.367. doi:10.3322/CA.57.6.367. [DOI] [PubMed] [Google Scholar]
- Farkas AJ, Gilpin EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviours. Tobacco Control. 1999;8:261–265. doi: 10.1136/tc.8.3.261. doi:10.1136/tc.8.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrauti A, Neumann G, Weber K, Keul J. Urine catecholamine concentrations and psychophysical stress in elite tennis under practice and tournament conditions. Journal of Sports Medicine and Physical Fitness. 2001;41:269–274. Retrieved from http://www.minervamedica.it/en/journals/sports-med-physical-fitness/index.php. [PubMed] [Google Scholar]
- Fisher LB, Winickoff JP, Camargo CA, Jr., Colditz GA, Frazier AL. Household smoking restrictions and adolescent smoking. American Journal of Health Promotion. 2007;22:15–21. doi: 10.4278/0890-1171-22.1.15. [DOI] [PubMed] [Google Scholar]
- Forno E, Celedón JC. Asthma and ethnic minorities: Socioeconomic status and beyond. Current Opinion in Allergy and Clinical Immunology. 2009;9:154–160. doi: 10.1097/aci.0b013e3283292207. doi:10.1097/ACI.0b013e3283292207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin EA, White MM, Farkas AJ, Pierce JP. Home smoking restrictions: Which smokers have them and how they are associated with smoking behavior? Nicotine & Tobacco Research. 1999;1:153–162. doi: 10.1080/14622299050011261. doi:10.1080/14622299050011261. [DOI] [PubMed] [Google Scholar]
- Gonzales M, Malcoe LH, Kegler MC, Espinoza J. Prevalence and predictors of home and automobile smoking bans and child environmental tobacco smoke exposure: A cross-sectional study of U.S. and Mexico-born Hispanic women with young children. BMC Public Health. 2006;6:265. doi: 10.1186/1471-2458-6-265. doi:10.1186/1471-2458-6-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Stamatakis E, Batty GD. Objectively assessed second-hand smoke exposure and mental health in adults. Archives of General Psychiatry. 2010;67:850–855. doi: 10.1001/archgenpsychiatry.2010.76. doi:10.1001/archgenpsychiatry.2010.76. [DOI] [PubMed] [Google Scholar]
- Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: National cross sectional survey. British Medical Journal. 2007;335:549–552. doi: 10.1136/bmj.39315.670208.47. doi:10.1136/bmj.39315.670208.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston JD, Bachman JG, O’Malley PM, Schulenberg JE. The monitoring the future project after thirty-two years: Design and procedures. Ann Arbor, MI: Institute for Social Research; 2006. (Monitoring the Future Occasional Paper No. 64) Retrieved from http://monitoringthefuture.org/pubs/occpapers/occ64.pdf. [Google Scholar]
- Kelloway EK. Using LISREL for structural equation modeling: A researcher's guide. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3rd ed. New York, NY: Guilford Press; 2010. [Google Scholar]
- Levy DT, Romano E, Mumford EA. Recent trends in home and work smoking bans. Tobacco Control. 2004;13:258–263. doi: 10.1136/tc.2003.006056. doi:10.1136/tc.2003.006056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills AL, Messer K, Gilpin EA, Pierce JP. The effect of smoke-free homes on adult smoking behavior: A review. Nicotine & Tobacco Research. 2009;11:1131–1141. doi: 10.1093/ntr/ntp122. doi:10.1093/ntr/ntp122. [DOI] [PubMed] [Google Scholar]
- Moore BA, Augustson EM, Moser RP, Budney AJ. Respiratory effects of marijuana and tobacco use in a US sample. Journal of General Internal Medicine. 2005;20:33–37. doi: 10.1111/j.1525-1497.2004.40081.x. doi:10.1111/j.1525-1497.2004.40081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 6th ed. Los Angeles, CA: Author; 2010. Retrieved from http://www.statmodel.com/download/usersguide/Mplus%20Users%20Guide%20v6.pdf. [Google Scholar]
- Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, et al. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. European Journal of Public Health. 2005;16:179–184. doi: 10.1093/eurpub/cki159. doi:10.1093/eurpub/cki159. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Bentler PM. Impact of adolescent drug use and social support on problems of young adults: A longitudinal study. Journal of Abnormal Psychology. 1988;97:64–75. doi: 10.1037//0021-843x.97.1.64. doi:10.1037//0021-843X.97.1.64. [DOI] [PubMed] [Google Scholar]
- Nystedt P. Marital life course events and smoking behavior in Sweden 1980–2000. Social Science & Medicine. 2006;62:1427–1442. doi: 10.1016/j.socscimed.2005.08.009. doi:10.1016/j.socscimed.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Okah FA, Choi WS, Okuyemi KS, Ahluwalia JS. Effect of children on home smoking restriction by inner-city smokers. Pediatrics. 2002;109:244–249. doi: 10.1542/peds.109.2.244. doi:10.1542/peds.109.2.244. [DOI] [PubMed] [Google Scholar]
- Perera FP, Illman SM, Kinney PL, Whyatt RM, Kelvin EA, Shepard P, et al. The challenge of preventing environmentally related disease in youth children: Community-based research in New York City. Environmental Health Perspective. 2002;110:197–204. doi: 10.1289/ehp.02110197. doi:10.1289/ehp.02110197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Rohay J, Meilahn EN, Wing RR, Matthews KA, Kuller LH. Diet, alcohol, and physical activity as a function of smoking status in middle-aged women. Health Psychology. 1993;12:410–415. doi: 10.1037//0278-6133.12.5.410. doi:10.1037//0278-6133.12.5.410. [DOI] [PubMed] [Google Scholar]
- Pine DS, Klein RG, Coplan JD, Papp LA, Hoven CW, Martinez M, et al. Differential carbon dioxide sensitivity in childhood anxiety disorders and nonill comparison group. Archives of General Psychiatry. 2000;57:960–967. doi: 10.1001/archpsyc.57.10.960. doi:10.1001/archpsyc.57.10.960. [DOI] [PubMed] [Google Scholar]
- Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. A prospective study of household smoking bans and subsequent cessation related behaviour: The role of stage of change. Tobacco Control. 2004;13:23–28. doi: 10.1136/tc.2003.003038. doi:10.1136/tc.2003.003038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. Longitudinal study of household smoking ban adoption among households with at least one smoker: Associated factors, barriers, and smoker support. Nicotine & Tobacco Research. 2008;10:533–540. doi: 10.1080/14622200801902003. doi:10.1080/14622200801902003. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. In: Hersen M, Eisler RM, Miller PM, editors. Progress on behavior modification. Sycamore, IL: Sycamore Press; 1992. pp. 184–219. [PubMed] [Google Scholar]
- Proescholdbell RJ, Chassin L, MacKinnon DP. Home smoking restrictions and adolescent smoking. Nicotine & Tobacco Research. 2000;2:159–167. doi: 10.1080/713688125. doi:10.1080/713688125. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 2001;56(Suppl. 2):S23–S35. doi: 10.1093/gerona/56.suppl_2.23. doi:10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Schultz ASH, Nowatzki J, Dunn DA, Griffith EJ. Effects of socialization in the household on youth susceptibility to smoking: A secondary analysis of the 2004/05 Canadian Youth Smoking Survey. Chronic Diseases in Canada. 2010;30:71–77. Retrieved from http://www.phac-aspc.gc.ca/publicat/cdic-mcc/30-3/pdf/10-022_ASPC_Vol30n3_Article1_EN.pdf. [PubMed] [Google Scholar]
- Shavers VL, Fagan P, Alexander LA, Claytron R, Doucet J, Baezconde-Garbanati L. Workplace and home smoking restrictions and racial/ethnic variation in the prevalence and intensity of current cigarette smoking among women by poverty status, TUS-CPS 1998–1999 and 2001–2002. Journal of Epidemiology & Community Health. 2006;60:34–43. doi: 10.1136/jech.2006.046979. doi:10.1136/jech.2006.046979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields M. Smoking bans: Influence on smoking prevalence. Health Reports. 2007;18:9–24. Retrieved from http://www.statcan.gc.ca.ezproxy.med.nyu.edu/pub/82-003-x/4060784-eng.htm. [PubMed] [Google Scholar]
- Spence JC, McGannon KR, Poon P. The effect of exercise on global self-esteem: A quantitative review. Journal of Sport & Exercise Psychology. 2005;27:311–334. Retrieved from http://journals.humankinetics.com/jsep. [Google Scholar]
- Szabo E, White V, Hayman J. Can home smoking restrictions influence adolescents’ smoking behaviors if their parents and friends smoke? Addictive Behaviors. 2006;31:2298–2303. doi: 10.1016/j.addbeh.2006.02.025. doi:10.1016/j.addbeh.2006.02.025. [DOI] [PubMed] [Google Scholar]
- Tsuno A, Besset A, Ritchie K. Sleep and depression. Journal of Clinical Psychiatry. 2005;66:1254–1269. doi: 10.4088/jcp.v66n1008. doi:10.4088/JCP.v66n1008. [DOI] [PubMed] [Google Scholar]
- Unger JB. Stages of change of smoking cessation: Relationships with other health behaviors. American Journal of Preventive Medicine. 1996;12:134–138. Retrieved from http://www.ajpm-online.net/ [PubMed] [Google Scholar]
- Wainwright NWJ, Surtees PG, Welch AA, Luben RN, Khaw KT, Bingham SA. Healthy lifestyle choices: Could sense of coherence aid health promotion? Journal of Epidemiology & Community Health. 2007;61:871–876. doi: 10.1136/jech.2006.056275. doi:10.1136/jech.2006.056275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West R, Hajek P. What happens to anxiety levels on giving up smoking? American Journal of Psychiatry. 1997;154:1589–1592. doi: 10.1176/ajp.154.11.1589. Retrieved from http://ajp.psychiatryonline.org/ [DOI] [PubMed] [Google Scholar]
- Wilson SE, Kahn RS, Khoury J, Lanphear BP. Racial differences in exposure to environmental tobacco smoke among children. Environmental Health Perspectives. 2005;113:362–367. doi: 10.1289/ehp.7379. doi:10.1289/ehp.7379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Rothemich SF, Johnson RE, Marsland DW. Is cigarette smoking associated with impaired physical and mental functional status? An office-based survey of primary care patients. American Journal of Preventive Medicine. 1999;17:134–137. doi: 10.1016/s0749-3797(99)00060-4. doi:10.1016/S0749-3797(99)00060-4. [DOI] [PubMed] [Google Scholar]