Abstract
Objective
To test the hypothesis that pain patients differ from well children in their appraisal and coping with daily stressors and to test a model of the relation of stress appraisal and coping to symptoms and disability.
Methods
Pediatric patients with chronic abdominal pain (n = 143) and well children (n = 104) completed a 5-day diary study regarding their appraisal and coping with daily stressors. Somatic symptoms, depressive symptoms, and functional disability were assessed 2 months later.
Results
Compared to well children, pain patients were less confident of their ability either to change or to adapt to stress and were less likely to use accommodative coping strategies. Different patterns of stress appraisal were associated with active, passive, and accommodative coping. Both appraisals and coping were significantly related to symptoms and disability.
Conclusions
The relation between stress and symptoms in pediatric pain patients may be explained in part by their appraisal and coping with stressors. The relation between appraisal and coping was consistent with Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal, and Coping. New York: Springer.
Keywords: abdominal pain, accommodative coping, appraisal, passive coping, stress
Chronic abdominal pain, defined as long-lasting intermittent or constant abdominal pain (American Academy of Pediatrics and North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition, Subcommittee on Chronic Abdominal Pain, 2005), affects 5–20% of youth (Apley & Naish, 1958; Kristjansdottir, 1997; Oster, 1972), is associated with high levels of impairment and pediatric health service utilization (Campo, Comer, Jansen-McWilliams, Gardner, & Kelleher, 2002), and may continue into adolescence and adulthood (Campo et al., 2001; Walker, Guite, Duke, Barnard, & Greene, 1998). It is rarely associated with organic disease, but instead typically reflects a functional gastrointestinal disorder (Boyle, 1997; Walker, et al., 2004).
Several investigations have linked chronic abdominal pain to stressful life events. In prospective studies, higher levels of negative life events predicted symptom maintenance 3 months (Walker & Greene, 1991) and 1 year (Walker, Garber, & Greene, 1994) following children’s medical evaluation for abdominal pain. Moreover, results of a diary study showed that the intraindividual relation between daily stressors and somatic symptoms was significantly stronger in abdominal pain patients than in well children (Walker, Smith, Garber, Van Slyke, & Claar, 2001). Investigation of pain patients’ subjective experience and behavioral responses to stress might shed light on the relation between stress and somatic symptoms observed in these patients.
Theories of life stress emphasize that the manner in which individuals appraise and cope with stress determine the impact of stress on health (Lazarus & Folkman, 1984; Monroe & Kelly, 1995; Sandler, Wolchik, MacKinnon, Ayers, & Roosa, 1997). This perspective suggests that pediatric abdominal pain patients may differ from well children in the way that they appraise and cope with stress, and, moreover, their particular style of stress appraisal and coping may be associated with high levels of symptoms and disability. Accordingly, this study aimed to (a) examine stress appraisal and coping by pediatric abdominal pain patients in comparison to well children and (b) examine the relation of children’s appraisal and coping with daily stressors to their somatic and depressive symptoms and disability.
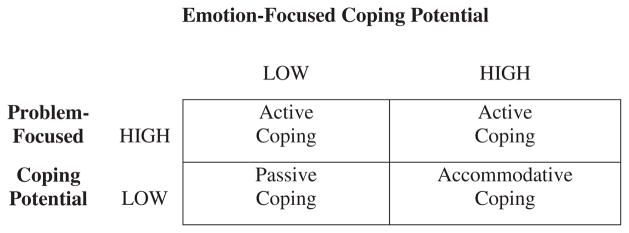
Our specific predictions were based on the model of stress appraisal and coping advanced by Lazarus & Folkman (1984) (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986), which asserts that individuals’ appraisals of stressor severity and their perceived coping potential predict the nature of the coping strategies they use when confronting a particular stressor. Those strategies, in turn, determine the impact of the stressor on their health (Lazarus & Folkman, 1984). Appraisals of coping potential can be differentiated into two major types: problem-focused coping potential (PFCP)—the perceived ability to alter the circumstances to make them more desirable—and emotion-focused coping potential (EFCP)—the perceived ability to handle or adjust to the circumstances, even if they cannot be improved (cf. Lazarus & Folkman, 1984; Smith & Lazarus, 1990; Walker, Smith, Garber, & Claar, 2005). We predicted that abdominal pain patients would appraise both their PFCP and EFCP as lower compared to well children.
The particular combination of perceived PFCP and EFCP is thought to predict one’s response to a stressor (Folkman, 1984; Lazarus & Folkman, 1984; Walker et al., 2005), as shown in Fig. 1. Individuals who appraise their PFCP as high are hypothesized to engage in strategies aimed at improving their circumstances—strategies that have been referred to as active coping in some typologies (e.g., Brown & Nicassio, 1987; Walker, Smith, Garber, & Van Slyke, 1997). Individuals who appraise their PFCP as low, in contrast, are hypothesized to engage in either accommodative or passive coping, depending on whether they appraise their EFCP as high or low. If they appraise their EFCP as high, and thus believe that they can accept and adjust to their circumstances, they are expected to engage in accommodative coping strategies such as acceptance and positive reappraisal, which theoretically foster adaptation to unchangeable stressful circumstances (see Lazarus, 1991; Smith & Lazarus, 1990). Conversely, if they appraise their EFCP as low, and thus believe that they cannot adjust to unchangeable stressful circumstances, they are expected to engage in passive coping strategies characterized by negative cognitions and lack of active problem-solving efforts (e.g., Brown & Nicassio, 1987; Walker et al., 1997). Thus, we predicted that, in comparison to well children, pediatric abdominal pain patients would report more passive coping strategies and fewer active and accommodative coping strategies when dealing with daily stressors.
Figure 1.
Hypothesized relations of appraised problem-focused coping potential (PFCP) and emotion-focused coping potential (EFCP) to active, passive, and accommodative coping.
We also examined the relation of children’s appraisal and coping with daily stressors to their symptoms and disability. We expected that appraisals of coping potential would predict the nature of coping strategies and that these strategies, in turn, would predict symptoms and disability. Thus, we hypothesized that coping strategies would mediate the relations between appraisals of coping potential and symptoms and disability. Specifically, we hypothesized that higher levels of passive coping, itself predicted by lower levels of both PFCP and EFCP, would be associated with greater functional disability and higher levels of somatic and depressive symptoms. In contrast, higher levels of active coping (itself predicted by higher levels of appraised PFCP) and higher levels of accommodative coping (itself predicted by higher levels of EFCP) would be associated with less disability and lower levels of somatic and depressive symptoms.
Methods
Sample
Abdominal Pain Patients (n = 143)
Patient participants were children between the ages of 8 and 15 who had been evaluated for abdominal pain by their primary care provider and were referred for further evaluation at a pediatric gastroenterology clinic in a tertiary care medical center. Consecutive new referral patients were eligible if they had experienced at least three episodes of abdominal pain severe enough to interrupt activities and occurring over a period of at least 3 months (Apley, 1975; Apley & Naish, 1958). Exclusionary criteria included a known chronic health condition, physical handicap, or mental retardation. Of the 229 patient families contacted, 57 (26%) failed to meet eligibility criteria and 18 (8%) declined. The sample was primarily Caucasian (95%) and female (57%). The mean age was 10.80 (SD = 2.10). Data from 11 of the 154 participants (7%) were excluded from these analyses because the hassles they reported over the course of the week involved abdominal pain and, thus, were confounded with group status. Therefore, the final sample of pain patients included 143 participants. Of these, 2-month follow-up data were obtained for 137 participants (96%).
Well Children (n = 104)
The well sample was recruited from children who had participated in a larger school-based survey of children’s health. Children were eligible to participate in this study if they had reported abdominal pain less than once a week and had scored below the sample median for well children on the Children’s Somatization Inventory (CSI) (Walker & Garber, 2003; Walker, Garber, & Greene, 1991) (the median was 11 for boys and 14 for girls). Parents of these children were contacted by telephone and screened for further exclusionary criteria including: (a) Chronic medical conditions (e.g., diabetes), (b) Organic disease involving abdominal pain (e.g., peptic ulcer, Crohn’s disease), and (c) Three or more episodes of unexplained abdominal pain severe enough to interrupt activities during the last 3 months. Recruitment was monitored to yield the same proportion of well children as pain patients with respect to gender, ethnicity, and age. Of the 124 families invited to participate, 11 (9%) declined and 4 (3%) were excluded because they did not meet eligibility criteria, leaving a total of 109 participating families. Data from 5 of the 109 participants (5%) were excluded from these analyses because the hassles they reported involved episodes of abdominal pain. The final sample of well children included 104 participants. Of these, 2-month follow-up data were obtained for 102 participants (98%). The well sample was similar to the pain sample in that it was primarily Caucasian (95%) and female (57%) and had a mean age of 10.84 (SD = 1.92).
Procedure
The Daily Diary Interview (DDI; Walker et al., 2001) was administered to children by telephone in the evening on five consecutive school days. The DDI is a structured interview that assesses daily stressors (“hassles”) related to family, peers, and school. Interviewers prompted children’s recall of activities earlier in the day by referring to daily routines. On each day, children were asked about three time periods (morning, school, afternoon/evening). Questions for each time period began with an open-ended format, prompting children to describe events that occurred during that time period. Next, children were read a list of stressors that might have occurred during that period of the day. The list included stressors associated with family, friends, school, chores, and recreation.
Following administration of the list of stressors, children were asked to identify the “worst hassle” of the day. Children responded to a series of structured questions regarding appraisal and coping with that stressor. Total scores for the appraisal and coping variables were computed by averaging the variables across all eligible hassles reported by a particular child over the course of the 5 interview days.
Physical symptoms, depressive symptoms, and functional disability were assessed in follow-up interviews conducted by telephone 2 months following the daily interviews.
Measures
Appraisal of Stressor Severity
Following identification of the worst stressor of the day, children responded to the question, “How bad was it for you that (stressor) happened?” They rated the perceived severity of the stressor on a scale from “not at all” (0) to “a whole lot” (4).
Appraisal of Coping Potential
Two types of perceived coping potential were assessed: problem-focused and emotion-focused. Each type of coping potential was assessed with a two-part question. For example, to assess perceived problem-focused coping potential (PFCP), children were first asked to respond “yes” or “no” to the question, “When (stressor) happened, did you think you would be able to do something to make the situation better?” Next, children were asked to respond to the question, “How sure were you when (stressor) happened that you (would/would not) be able to make the situation better?” Responses to this question were rated on a 5-point scale ranging from “not at all” (“0”) to “a whole lot” (“4”). The score for PFCP was obtained by combining the responses to the two questions into a single 9-point scale that ranged from “−4” (indicating high degree of certainty that the child would not be able to make the situation better) to +4 (indicating a high degree of certainty that the child would indeed be able to make the situation better). Assessment of perceived emotion-focused coping potential (EFCP) was similar, except that the questions were reworded to read, “When (stressor) happened, did you think you would be able to deal with it or handle it, even if the situation didn’t get better?” and “How sure were you that you (could/could not) deal with it or handle it, even if the situation didn’t get better?”
Coping
Measures of active, passive, and accommodative coping with daily stressors were derived from the Pain Response Inventory (PRI; Walker et al. 1997), using items with the highest factor loadings. The item stem was worded to refer to coping with a stressor. Active coping was assessed with three items: “Try to figure out what to do about it;” “Ask someone for help,” and “Talk to someone who you thought would understand how you felt.” Passive coping was assessed with three items: “Go off by yourself;” “Think to yourself that the situation was going to get worse;” and “Think to yourself that there was nothing you could do, so you didn’t even try.” Accommodative coping was assessed with four items: “Try to accept it;” “Think of things to take your mind off the situation;” “Tell yourself that the situation was not that bad;” and “Tell yourself to keep going even though this was happening.” Children were asked how much they used each strategy in response to the worst stressor of the day; their responses were rated on a 5-point scale ranging from “not at all” (“0”) to “a whole lot” (“4”) (see Appendix: Reviewer’s Comment 1).
Children’s Somatic Symptoms
The CSI (Walker et al., 1991; Walker & Garber, 2003) assessed the severity of somatic symptoms (e.g., “headaches,” “chest pain,” and “feeling low in energy”). Respondents rated the extent to which they have experienced each of the 35 symptoms during the past 2 weeks using a 5-point scale ranging from “not at all” to “a whole lot”. The scale ranges from 0 to 140. Three-month test–retest reliability for the CSI is .50 for well patients and .66 for patients with chronic pain (Walker et al., 1991). The average score for a large referred sample of pediatric pain patients (n = 498) on this scale was 22.7 (SD 14.4; Range 3–81) with a median of 19 (Walker & Garber, 2003). Internal consistency of the CSI in this sample was .89.
Child Impairment
The functional disability inventory (FDI; Claar & Walker, 2006; Walker & Greene, 1991) consists of 15 items concerning the intensity of children’s self-reported impairment in physical and psychosocial functioning due to their physical health during the past 2 weeks. Behaviors measured by this instrument include walking up stairs, playing with friends, and doing activities in gym. For each item, the five response options range from “No Trouble” (0) to “Impossible” (4). Total scores are computed as the sum of responses and can range from 0 to 60. The FDI has good internal consistency and 3-month test–retest reliability estimates exceeding .60 for patients with chronic abdominal pain (Claar & Walker, 2006; Walker & Greene, 1991). Scores on the child report FDI correlate significantly (r = .44) with school absence (Walker & Greene, 1991). Coefficient alpha for the FDI in this sample was .88.
Depressive Symptoms
The children’s depression inventory (CDI; Kovacs, 1985), a 27-item self-report questionnaire, assesses children’s depressive symptoms in the past 2 weeks. Items are rated on a 3-point scale. Total scores can range from 0 to 54. Reliability and validity have been established (Kovacs, 1992). Cronbach’s alpha on a normative sample of 1,266 children aged 7–16 was .86; it was .85 in the current sample.
Results
Overview
The analyses reported below are organized into two major sections. First, after reporting the number of stressors reported by participants during the 5 days of diary interviews, a series of analyses of variance (ANOVAs) is reported to examine whether the stress appraisals and coping activities associated with the stressors differed as a function of patient status or gender. Next, using a series of regression analyses, the interrelations among appraisal, coping, symptoms, and disability are examined. The regression analyses were structured to examine the degree to which the data were consistent with a mediational model in which the effects of appraisal on symptoms and disability were mediated by coping.
Frequency of Daily Stressors
The number of eligible stressors reported by each child ranged between 1 and 5, with a mean of 3.65 (SD = 1.37). Thirty-six percent of the sample reported at least one stressor on each of the 5 interview days. The number of stressors reported did not vary as a function of group, F (1, 253) < 1.00, ns; sex, F(1, 253) = 1.74, p = .19, or their interaction, F (1, 253) < 1.00, ns.
Appraisals
Primary Appraisal: Stresser Severity
A group X sex ANOVA examined children’s ratings of the severity of their daily stressors. Significant effects were found for group, F(1,239) = 7.86, p <.005, sex, F(1,239) = 16.24, p < .001, and the interaction of group and sex, F(1,239) = 4.02, p < .05. Examination of the group means indicated that girls with abdominal pain appraised their stressors as more severe (M = 2.35) than well girls (M = 1.82) and than boys both with (M = 1.69) and without (M = 1.60) abdominal pain. A contrast pitting the girls with abdominal pain against the other three groups was significant, F (1, 239) = 11.06, p < .001.
Secondary Appraisal: PFCP and EFCP
A group X sex multivariate ANOVA was conducted with type of coping potential (emotion-focused, problem-focused) as a repeated measure (see Appendix: Reviewer’s Comment 2). Results indicated a significant within-subject effect for type of coping potential, multivariate F(1,241) = 72.91, p < .001. Children rated their EFCP as significantly greater than their PFCP (for EFCP, M = 1.84, SD = 1.98; for PFCP, M = .51, SD = 2.29). The main effect for group also was significant, F(1,242) = 8.51, p < .01. As expected, pain patients rated both their EFCP (M = 1.69, SD = 1.61) and their PFCP (M = .13, SD = 1.65) significantly lower than well children (for EFCP, M = 2.18, SD = 1.46; for PFCP, M = .79, SD = 1.76). Neither the main effect for sex, F(1, 242) = 2.60, p = .11, nor the group by sex interaction, F (1, 242) = 1.91, p = .17, was significant, nor did any of these effects interact with the type of coping potential, all three Fs (1, 242) < 1.00, ns.
Coping with Daily Stressors
Next, we conducted group X sex multivariate ANOVAs with type of coping (passive, active, and accomodative) as a repeated measure. Results indicated a significant effect for type of coping, multivariate F(2, 242) = 191.30, p < .001. Subsequent post hoc paired t-tests indicated that children reported using accommodative coping significantly more than active coping, t(246) = 11.12, p < .001, and active coping significantly more than passive coping, t(246) = 10.28, p < .001 (accommodative coping, M = 1.66, SD = .79; active coping, M = 1.06, SD = .65; passive coping, M = .56, SD = .58).
A significant group X type of coping interaction effect also was obtained, multivariate F(2, 242) = 5.97, p < .01. Subsequent univariate analyses indicated that, as expected, pain patients reported significantly less accommodative coping compared to well children, F(1, 245) = 5.13, p < .01 (pain patients, M = 1.54, SD = .76; well children, M = 1.83, SD = .79). Contrary to expectations, the groups did not differ significantly in their reported use of active, F (1, 245) = 1.08, p = .30, or passive coping, F (1, 245) < 1.00, ns. No further effects of group, sex, their interaction, or of interactions with type of coping were significant (all ps > .13).
Relations of Appraisal and Coping to Symptoms and Disability
A final set of analyses examined whether children’s appraisals and coping with daily stressors were associated with their symptoms and disability at the 2-month follow-up. We were particularly interested in the degree to which the data were consistent with a mediational model predicted by appraisal theory (Lazarus & Folkman, 1980, 1984; Smith & Lazarus, 1990), in which stress appraisals are associated with symptoms and disability through their influence on coping.
These relations were examined with a series of hierarchical regressions that reflected the logic of mediational analyses as outlined by Baron and Kenny (1986). When the three appraisal variables (stressor severity, PFCP, and EFCP) were used as predictor variables, they were entered into the regression equations simultaneously as a set, such that their joint contribution to the regression equation could be assessed. The three coping variables (i.e., active, passive, and accommodative coping) also were treated as a set. In the first step of all analyses, the participants’ sex and diagnostic group were entered into the equations as control variables.
For the prediction of each outcome (CSI, FDI, and CDI), analyses were organized into three groups. The first analyses examined the degree to which appraisal predicted coping. This was done by regressing each of the three coping variables on the set of appraisal variables. In a second group of analyses, both the appraisal and coping variables were used to predict each of the three outcomes, with the set of appraisal variables entered in a second step, before the set of coping variables was entered in a third step. The third and final group of analyses was similar to the second group, except that the set of coping variables was entered into the equation in a second step before the appraisal variables were entered in the third step. To be consistent with a mediational model, first, appraisal should be found to reliably predict the outcomes when considered by itself (i.e., step 2 of the second group of analyses), and appraisal should be found to predict coping (the hypothesized mediator) in the first group of analyses. In addition, when both the coping variables and appraisal variables are used to predict the outcome together (and thus when the two sets of variables are used to control for one another), significant relations between the coping variables (the purported mediator) and the outcome should still be evident (step 3 of the second set of analyses). In contrast, the relations between the appraisal variables and the outcome (step 3 of the third group of analyses) should be substantially weakened (for partial mediation) or no longer evident (for full mediation).
The zero-order correlations among the variables entering into these analyses are summarized in Table I. The results of the three groups of regression analyses are summarized in the three panels of Table II and, controlling for sex and diagnostic group, provide some support that the relation of appraisal to symptoms (CSI and CDI) and disability (FDI) is partially mediated by coping. First, as shown in Panel A of Table II, the appraisal variables predict all three types of coping. Thus, in accord with Baron and Kenny (1986), the hypothesized antecedent (appraisal) variables reliably predict the hypothesized mediators (coping). Moreover, the relations between appraisals and coping are highly consistent with theoretical predictions. The appraised severity of the stressors predicted each type of coping, indicating a higher likelihood of engaging in all three types of coping when the stressors were appraised as more severe. In addition, appraisals of EFCP and PFCP predicted all three types of coping in theoretically consistent, different ways. As expected, active coping was positively associated with appraisals of PFCP. Also as expected, accommodative coping was positively associated with appraisals of EFCP but was not associated with PFCP. Passive coping, in contrast and as expected, was associated with low levels of both PFCP and EFCP.
Table I.
Intercorrelations among variables entering into the regression analyses
| Sex | Group | Severity | EFCP | PFCP | Active cope | Accom-cope | Passive cope | CSI | FDI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group | .01 | – | – | – | – | – | – | – | – | – |
| Severity | .25 | .20 | – | – | – | – | – | – | – | – |
| EFCP | −.12 | −.15 | −.22 | – | – | – | – | – | – | – |
| PFCP | .08 | −.18 | −.09 | .48 | – | – | – | – | – | – |
| Active-cope | .08 | .11 | .25 | .02 | .21 | – | – | – | – | – |
| Accom-cope | −.07 | −.15 | .02 | .37 | .15 | .29 | – | – | – | – |
| Passive-cope | .11 | .08 | .40 | −.31 | −.26 | .22 | .13 | – | – | – |
| CSI | .22 | .40 | .36 | −.25 | −.25 | .15 | −.02 | .36 | – | – |
| FDI | .19 | .32 | .28 | −.18 | −.18 | .15 | .04 | .28 | .77 | – |
| CDI | .18 | .21 | .36 | −.29 | −.28 | .09 | .08 | .29 | .54 | .47 |
Accom, accommodative; CDI, children’s depression inventory; CSI, children’s somatization inventory; EFCP, emotion-focused coping potential; FDI, functional disability inventory; PFCP, problem-focused coping potential.
n = 228. All correlations with a magnitude of .13 or greater are significantly different from 0 at p < .05.
Table II.
Hierarchical regression analyses
| Panel A | ||||
|---|---|---|---|---|
| Analysis 1: Predicting coping from appraisals
| ||||
| Step 2
|
||||
| Beta weights
| ||||
| Severity | EFCP | PFCP | ΔR2 | |
| Active | .26*** | −.04 | .28*** | .12*** |
| Passive | .37*** | −.17* | −.16* | .23*** |
| Accommodative | .13* | .39*** | −.03 | .13*** |
| Panel B | ||||||||
|---|---|---|---|---|---|---|---|---|
| Predicting outcomes from appraisals and coping | ||||||||
| Analysis 2: Appraisals entered before coping
| ||||||||
| Step 2: Appraisals entered
|
Step 3: Coping entered
|
|||||||
| Beta weights
|
Beta weights
|
|||||||
| Severity | EFCP | PFCP | ΔR2 | Active | Passive | Accommodative | ΔR2 | |
| CSI | .23*** | −.07 | −.12* | .11*** | .03 | .20** | .04 | .04** |
| FDI | .18** | −.03 | −.09 | .06** | .04 | .16* | .08 | .04* |
| CDI | .28*** | −.12* | −.17* | .15*** | .03 | .10 | −.03 | .01 |
| Panel C | ||||||||
|---|---|---|---|---|---|---|---|---|
| Analysis 3: Coping entered before appraisals
| ||||||||
| Step 2: Coping entered
|
Step 3: Appraisals entered
|
|||||||
| Beta weights
|
Beta weights
|
|||||||
| Active | Passive | Accommodative | ΔR2 | Severity | EFCP | PFCP | ΔR2 | |
| CSI | .04 | .30*** | .00 | .11*** | .15* | −.05 | −.10 | .03* |
| FDI | .05 | .23*** | .05 | .08*** | .11 | −.04 | −.07 | .02 |
| CDI | −.09 | .27*** | .04 | .08*** | .24*** | −.09 | −.16* | .08* |
p < .05.
p < .01.
p < .001.
CDI, children’s depression inventory; CSI, children’s somatization inventory; EFCP, emotion-focused coping potential; FDI, functional disability inventory; PFCP, problem-focused coping potential.
In the first step (not depicted) of each analysis, participant sex and diagnostic group were entered into the regressions as control variables.
The next groups of analyses predicted symptoms and disability from appraisals and coping, as shown in Panels B and C of Table II. First, when considered by themselves, the appraisal variables (the second step of the second group of analyses) predicted all three outcomes. Thus, there is evidence that the hypothesized antecedent variables are associated with the outcomes, which is a key prerequisite for mediation (Baron & Kenny, 1986). In addition, the coping variables, considered by themselves (the second step of the third group of analyses), also were associated with the three outcomes. Thus, the purported mediators were also associated with the outcomes, which is also a prerequisite for mediation. It should be noted, however, that in these analyses, one variable within each set dominated the prediction. For the appraisal variables, appraised severity was the strongest predictor of all three outcomes, whereas for the coping variables, passive coping was the only variable that made a unique contribution to the prediction of the outcomes.
The third step of the analyses predicting outcomes (with appraisal and coping being controlled for one another) yielded some support for the proposed mediational model, although this support was equivocal. For both the CSI and the FDI, the relations with passive coping remained significant after accounting for the effects of the appraisal variables. However, no such evidence for mediation was found for the CDI. In addition, appraisals of severity continued to predict both the CSI and the CDI after including the coping variables in the equation (see Panel C of Table II), and for both variables, the relations with passive coping was weakened (CSI) or eliminated (CDI) by the addition of the appraisal variables (see the Panel B of Table II). Thus, these results are equally consistent with an alternative model in which the effects of coping on symptoms and disability are mediated by appraisal, as they are with the predicted model in which the effects of appraisal are mediated by coping (see Appendix: Reviewer’s Comment 3). Nonetheless, the results clearly indicate that both appraisal and coping make distinct contributions to the prediction of somatic symptoms and disability.
Discussion
In this study, pediatric pain patients exhibited patterns of stress appraisal and coping that differed from those of well peers and that were associated with somatic and depressive symptoms as well as functional disability 2 months later. Compared to well children, pain patients had significantly less confidence in their ability either to change or to adjust to stressors assessed during a week of diary interviews. That is, pain patients appraised themselves as having significantly lower levels of both PFCP and EFCP (Folkman & Lazarus, 1980; Smith & Lazarus, 1990). Moreover, consistent with their appraised low level of EFCP, pediatric patients also reported significantly less use of accommodative coping strategies such as accepting the stressor, reframing its significance, or encouraging themselves to keep going.
Correlational analyses across the groups indicated that, in accord with Lazarus and Folkman (1984) (Folkman & Lazarus, 1980; Smith & Lazarus, 1990), children’s appraisals of their PFCP and EFCP were associated with particular types of coping. Higher ratings of PFCP were associated with greater use of active coping, whereas higher ratings of EFCP were associated with greater use of accommodative coping. In contrast, lower ratings of both PFCP and EFCP were associated with greater use of passive coping. Thus, these findings support the hypothesized relations between appraisal and coping as outlined in Fig. 1 and suggest that both types of perceived coping potential may influence children’s response to stress.
Accommodative coping, that is, acceptance and positive reappraisal of stressors, was the most frequent type of coping reported by children in this study. Abdominal pain patients, however, reported significantly less accommodative coping compared to well children. It is possible that failure to accommodate to stress promotes negative affect and physiological arousal that, in turn, exacerbates abdominal pain. Of course, it is equally plausible that abdominal pain interferes with children’s ability to accommodate to daily stressors. Either way, the frequency with which accommodative coping was reported and the group differences highlight the importance of considering this type of response to adverse events in studies of stress and coping in children with chronic abdominal pain. Others have considered specific coping strategies, such as acceptance and positive reappraisal, which fit within our broader construct of accommodative coping (e.g., McCracken, Vowles, & Eccleston, 2004; Park, Cohen, & Murch, 1996; Schiaffino & Revenson, 1992; Sears, Stanton, & Danoff-Burg, 2003; Thomsen et al., 2002) and have found that the use of such strategies generally is associated with positive adaptational outcomes.
Although other studies have examined appraisal and coping with pain by pediatric patients with chronic abdominal pain (Thomsen et al., 2002; Walker et al., 2005), this study is the first to examine appraisal and coping with daily stress in this population. Our findings extend the literature by suggesting that, compared to well children, pediatric pain patients viewed themselves as less able either to change or to adjust to daily stressors. Consistent with their appraised coping ability, pain patients also made less use of accommodative coping strategies than their well peers. The study results showed that both appraisals and coping had significant direct effects on symptoms and disability. These findings underscore the importance of including appraisal in the study of stress adaptation (see also, Park, Armeli, & Tennen, 2004), and suggest that both appraisal and coping may contribute to the frequently observed association between life stress and symptoms in pediatric abdominal pain patients (e.g., Liakopoulou-Kairis et al., 2002; Walker et al., 2001). Thus, appraisal and coping processes may be promising targets for interventions aimed at reducing stress reactivity in patients with chronic abdominal pain.
In addition, these results supported a model in which coping partially mediated the relation between appraisals and symptoms, thereby reflecting relations among stress appraisal, coping efforts, and symptoms that may influence each other in an iterative process over time (Monroe & Kelly, 1995). For example, because pain patients appraise their coping potential as poor, they may not engage with daily stressors in ways that could help them develop new coping skills and greater confidence in their coping ability. Their relatively infrequent use of accommodative coping strategies may have negative consequences that reinforce their perceived poor coping potential and exacerbate their somatic symptoms. It also is possible, however, that the experience of frequent pain episodes and associated impairment may undermine children’s perceptions of their ability to cope with daily stressors. Perceived lack of control over stressors has been linked to anxiety (e.g., Malcarne & Hansdottir, 2001; Weems, Silverman, Rapee, & Pina, 2003) which, in turn, might heighten pain sensitivity through central nervous system processes (Dorn et al., 2003; Drossman, 1996; Zeltzer, Bursch, & Walco, 1997), thereby exacerbating pain and disability.
A strength of this study was the use of a daily diary to assess children’s appraisals and coping with real life stressors relatively close in time to their actual occurrence. Although clearly an improvement over methods that rely on retrospective recall of events that might have happened days or weeks earlier, however, an even stronger methodology might be the use of an ecological momentary assessment approach (e.g., Barrett & Barrett, 2001; Christensen, Barrett, Bliss-Moreau, Lebo, & Kaschub, 2003) which can measure cognitions and events at a given moment in time.
Prior work has linked passive coping with pain to negative health outcomes in pediatric abdominal pain patients (Thomsen et al., 2002; Walker et al., 1997, 2005). This study suggests that passive coping with life stress also is associated with symptoms and disability in these patients. Thus, behavioral interventions might aim to teach alternative responses to stress such as the accomodative strategies that were reported significantly more frequently by well children than by pain patients in this study. Our findings also suggest that interventions for stress management should evaluate perceived stress severity and personal coping potential as they are linked both to the nature of coping and to symptoms and disability. To the extent that perceived stress severity is high and coping potential is low, patients may choose passive coping strategies over alternative strategies taught in intervention programs.
Acknowledgments
This research was supported by a grant to the investigators from the National Institute on Child Health and Development (R01 HD23264), the NIDDK-supported Vanderbilt Digestive Disease Research Center (5P30 DK058404), and a core grant (HD15052) to the John F. Kennedy Center, Vanderbilt University. Garber was supported in part by an Independent Scientist Award from NIMH (K02 MH66249). The authors thank the staff of the Pediatric Gastroenterology, Hepatology and Nutrition Clinic at Vanderbilt University for assistance with patient recruitment and medical evaluations.
Appendix: Reviewer’s Comment
A reviewer of a previous version of this article questioned whether the responses to the Likert-type scales used to assess coping yielded true interval data, and, thus, whether the parametric statistical techniques used in this article were appropriate. The issue raised by the reviewer is applicable to virtually all of the measures used in this study as well as virtually all Likert-type measures that are prominently used in a broad range of social science research. At present, there is widespread consensus in the field that Likert-type scales, although clearly ordinal, seldom meet strict criteria for yielding true interval-level data. However, there is also a clear consensus that parametric statistical techniques are robust to this assumption violation and that the common use of parametric techniques to analyze such data is well justified (e.g., Jaccard & Wan, 1996; Zumbo and Zimmerman, 1993). For instance, in their review of this topic, Jaccard and Wan (1996) conclude: “for many statistical tests, rather severe departures (from intervalness) do not seem to affect type I and type II errors dramatically” (p. 4).
A reviewer of a previous version of this article questioned whether it was appropriate to treat the two appraisal variables as “repeated measures” because they represented two different variables measured at the same time, rather than the same variable measured on multiple occasions. Although, strictly speaking, the appraisal variables are not “repeated measures,” the within-subjects comparison produced by this analysis is meaningful and appropriate to examine both because the two appraisal variables represent different facets of a broader construct (appraisals of coping potential) and because these variables were measured on the same scale to facilitate their direct comparison. As reported in the results of this analysis, the within-subjects comparison asks whether children appraised their PFCP and EFCP at similar or different levels in response to the reported stressors. This same logic also applies to the “repeated measures”/within-subjects analysis subsequently reported for the coping variables.
A reviewer suggested that we might supplement the reported regression analyses with Sobel’s (1982) test, to explicitly examine whether the indirect effects of the antecendent (appraisal) variables on the outcomes, carried by the mediator (coping), were statistically significant. Although this is a reasonable suggestion, we did not pursue it for two reasons. First, given that both the antecedent and mediator variables are represented in these analyses by sets of variables, rather than single variables, it is not immediately obvious how to apply Sobel’s test to these analyses. Second, whatever the results of these tests, they would not alter the overall conclusion that the evidence in support of the hypothesized mediational model yielded by our analyses is equivocal.
References
- American Academy of Pediatrics and North American Society for Pediatric Gastroenterology, & Hepatology, and Nutrition, Subcommittee on Chronic Abdominal Pain. Technical report: chronic abdominal pain in children. Pediatrics. 2005;115:370–385. [Google Scholar]
- Apley J. The Child with Abdominal Pains. London: Blackwell; 1975. [Google Scholar]
- Apley J, Naish N. Recurrent abdominal pains: A field survey of 1000 school children. Archives of Diseases in Childhood. 1958;33:165–170. doi: 10.1136/adc.33.168.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Barrett DJ. An introduction to computerized experience sampling in psychology. Social Science Computer Review. 2001;19:175–185. [Google Scholar]
- Boyle JT. Recurrent abdominal pain: An update. Pediatrics in Review. 1997;18:310–321. doi: 10.1542/pir.18-9-310. [DOI] [PubMed] [Google Scholar]
- Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987;31:53–63. doi: 10.1016/0304-3959(87)90006-6. [DOI] [PubMed] [Google Scholar]
- Campo J, Comer D, Jansen-McWilliams L, Gardner W, Kelleher K. Recurrent pain, emotional distress, and health service use in childhood. Journal of Pediatrics. 2002;141:76–83. doi: 10.1067/mpd.2002.125491. [DOI] [PubMed] [Google Scholar]
- Campo J, DiLorenzo C, Chiappetta L, Bridge D, Colborn J, Gartner C, Jr, et al. Adult outcomes of pediatric recurrent abdominal pain: Do they just “grow out of it?”. Pediatrics. 2001;108(1):E1. doi: 10.1542/peds.108.1.e1. [DOI] [PubMed] [Google Scholar]
- Christensen TC, Barrett LF, Bliss-Moreau E, Lebo K, Kaschub C. A practical guide to experience-sampling procedures. Journal of Happiness Studies. 2003;4:53–78. [Google Scholar]
- Claar RL, Walker LS. Functional assessment of pediatric pain patients: Psychometric properties of the functional disability inventory. Pain. 2006;121:77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn LD, Campo JC, Thato S, Dahl RE, Lewin D, Chandra R, et al. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:66–75. doi: 10.1097/00004583-200301000-00012. [DOI] [PubMed] [Google Scholar]
- Drossman DA. Gastrointestinal illness and the biopsychosocial model. Journal of Clinical Gastroenterology. 1996;22:252–254. doi: 10.1097/00004836-199606000-00002. [DOI] [PubMed] [Google Scholar]
- Folkman S. Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology. 1984;46:839–852. doi: 10.1037//0022-3514.46.4.839. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus A. An analysis of coping in a middle-aged community sample. Journal of Health and Social behavior. 1980;21:219–239. [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Wan CK. LISREL Approaches to Interaction Effects in Multiple Regression. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- Kovacs M. The children’s depression inventory. Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kristjansdottir G. Prevalence of pain combinations and overall pain: A study of headache, stomach pain, and back pain among school-children. Scandinavian Journal of Social Medicine. 1997;25:58–63. doi: 10.1177/140349489702500112. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Emotion and Adaptation. New York: Oxford University Press; 1991. [Google Scholar]
- Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- Liakopoulou-Kairis M, Alifieraki D, Protagora D, Korpa T, Kondyli K, Dimosthenous E, et al. Recurrent abdominal pain and headache: Psychopathology, life events, and family functioning. European Child and Adolescent Psychiatry. 2002;11:115–122. doi: 10.1007/s00787-002-0276-0. [DOI] [PubMed] [Google Scholar]
- Malcarne VL, Hansdottir I. Vulnerability to anxiety disorders in childhood and adolescence. In: Price JM, Ingram RE, editors. Vulnerability to psychopathology: risk across the lifespan. New York: Guilford Press; 2001. pp. 271–303. [Google Scholar]
- McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: Component analysis and a revised assessment method. Pain. 2004;107:159–166. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Kelley JM. Measurement of Stress Appraisal. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: a guide for health and social scientists. New York: Oxford; 1995. [Google Scholar]
- Oster J. Recurrent abdominal pain, headache, and limb pains in children and adolescents. Pediatris. 1972;50:429–436. [PubMed] [Google Scholar]
- Park CL, Armeli S, Tennen H. Appraisal-coping goodness of fit: A daily internet study. Personality and Social Psychology Bulletin. 2004;30:558–569. doi: 10.1177/0146167203262855. [DOI] [PubMed] [Google Scholar]
- Park CL, Cohen LH, Murch RL. Assessment and prediction of stress-related growth. Journal of Personality. 1996;64:71–105. doi: 10.1111/j.1467-6494.1996.tb00815.x. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, MacKinnon D, Ayers TS, Roosa MW. Developing linkages between theory and intervention in stress and coping processes. In: Wolchik SA, Sandler IN, editors. Handbook of children’s coping: Linking theory and intervention. New York: Plenum Press; 1997. pp. 3–40. [Google Scholar]
- Schiaffino KM, Revenson TA. The role of perceived self-efficacy, perceived control, and causal attributions in adaptation to rheumatoid arthritis: Distinguishing mediator from moderator effects. Personality and Social Psychology Bulletin. 1992;16:709–718. [Google Scholar]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22:487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Smith CA, Lazarus RS. Emotion and Adaptation. In: Pervin LA, editor. Handbook of personality: theory and research. New York: Guilford; 1990. pp. 609–637. [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. Vol. 1982. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Thomsen AH, Compas BE, Colletti RB, Stanger C, Boyer MC, Konik BS. Parent reports of coping and stress responses in children with recurrent abdominal pain. Journal of Pediatric Psychology. 2002;27:215–226. doi: 10.1093/jpepsy/27.3.215. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J. Manual for the children’s somatization inventory. Nashville, TN: Department of Pediatrics, Vanderbilt University Medical Center; 2003. [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. Journal of Abnormal Child Psychology. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: A prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. Journal of Consulting and Clinical Psychology. 1994;6:1213–1221. doi: 10.1037//0022-006x.62.6.1213. [DOI] [PubMed] [Google Scholar]
- Walker LS, Greene JW. Negative life events and symptom resolution in pediatric abdominal pain patients. Journal of Pediatric Psychology. 1991;16:341–360. doi: 10.1093/jpepsy/16.3.341. [DOI] [PubMed] [Google Scholar]
- Walker LS, Guite JW, Duke M, Barnard JA, Greene JW. Recurrent abdominal pain: A potential precursor of irritable bowel syndrome in adolescents and young adults. Journal of Pediatrics. 1998;132:1010–1015. doi: 10.1016/s0022-3476(98)70400-7. [DOI] [PubMed] [Google Scholar]
- Walker LS, Lipani TA, Greene JW, Caines K, Stutts J, Polk DB, et al. Recurrent abdominal pain: Subtypes based on the Rome II criteria for pediatric functional gastrointestinal disorders. Journal of Pediatric Gastroenterology and Nutrition. 2004;38:187–191. doi: 10.1097/00005176-200402000-00016. [DOI] [PubMed] [Google Scholar]
- Walker LS, Smith CA, Garber J, Claar RL. Testing a model of pain appraisal and coping in children with recurrent abdominal pain. Health Psychology. 2005;24(4):364–374. doi: 10.1037/0278-6133.24.4.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the pain response inventory for children. Psychological Assessment. 1997;9:392–405. [Google Scholar]
- Walker LS, Smith CA, Garber J, Van Slyke DA, Claar R. The relation of daily stressors to somatic and emotional symptoms in children with recurrent abdominal pain. Journal of Consulting and Clinical Psychology. 2001;69:85–91. [PMC free article] [PubMed] [Google Scholar]
- Weems CF, Silverman WK, Rapee RM, Pina AA. The role of control in childhood anxiety disorders. Cognitive Therapy and Research. 2003;27:557–568. [Google Scholar]
- Zeltzer L, Bursch B, Walco G. Pain responsiveness and chronic pain: A psychobiological perspective. Developmental and Behavioral Pediatrics. 1997;18:413–422. doi: 10.1097/00004703-199712000-00008. [DOI] [PubMed] [Google Scholar]
- Zumbo BD, Zimmerman DW. Is the slection of statistical methods governed by level of measurement? Canadian Psychology. 1993;34:390–399. [Google Scholar]