Abstract
Objective
To determine whether community-based health workers in a rural region of Ethiopia can provide injectable contraceptives to women with similar levels of safety, effectiveness and acceptability as health extension workers (HEWs).
Methods
This was a prospective non-randomized community intervention trial designed to test the provision of injectable contraceptives by community-based reproductive health agents (CBRHAs). Effectiveness, safety, acceptability and continuation rates were the outcomes of interest. The outcomes observed when injectable contraceptives were administered by HEWs in health posts and when they were administered by CBRHAs were compared by means of χ2 tests for association among categorical variables and t-tests for independent samples to determine differences between group means.
Findings
A total of 1062 women participated in the study. Compared with health post clients, the clients of CBRHAs were, on average, slightly older, less likely to be married and less educated, and they had significantly more living children. Women seeking services from CBRHAs were also significantly more likely to be using injectable contraceptives for the first time; health post clients were more likely to have used them in the past. In addition, clients of CBRHAs were less likely to discontinue using injectable contraceptives over three injection cycles than health post clients.
Conclusion
Receiving injectable contraceptives from CBRHAs proved as safe and acceptable to this sample of Ethiopian women as receiving them in health posts from HEWs. These findings add to the growing body of evidence supporting the development, introduction and scale up of programmes to train community-based health workers such as CBRHAs to safely administer injectable contraceptives.
ملخص
الغرض
تحديد قدرة العاملين الصحيين المجتمعيين في المناطق الريفية في أثيوبيا على تقديم موانع الحمل القابلة للحقن للنساء بنفس مستويات الفعاليّة والأمان والمقبولية للعاملين على امتداد المواقع الصحية.
الطريقة
صُمِمت هذه التجربة الاستباقية للتدخل المجتمعي غير المختارة عشوائياً لاختبار تقديم موانع الحمل القابلة للحقن من قبل الموظفين في الصحة الإنجابية المجتمعية المرتكز. واشتملت النتائج ذات الاهتمام على معدلات الفعالية، والسلامة، والمقبولية، والاستمرار. وقد لوحظت النتائج عند إعطاء موانع الحمل القابلة للحقن من قبل العاملين الصحيين على امتداد المواقع الصحية، وقورنت مع نتائج إعطاء موانع الحمل القابلة للحقن من قبل الموظفين في الصحة الإنجابية المجتمعية المرتكز عن طريق متوسطات اختبار خي المربع χ2 للارتباط بين المتغيرات الفئوية، واختبارات t للعينات المستقلة لتحديد الاختلافات بين متوسطات المجموعة.
النتائج
اشتركت في الدراسة إجمالاً 1062 امرأة. وبالمقارنة مع المتعاملات في المواقع الصحية، كانت المتعاملات مع الموظفين في الصحة الإنجابية المجتمعية المرتكز، في المتوسط، أكبر قليلاً في العمر، وكن على الأرجح من غير المتزوجات، ومن الأقل تعليماً، وكان لديهن على نحو يعتد به عدد أكبر من الأطفال. كما كانت النساء المتلقيات لخدمات الموظفين في الصحة الإنجابية المجتمعية المرتكز على الأرجح أكثر استعمالاً لموانع الحمل القابلة للحقن لأول مرة؛ أما المتعاملات مع المواقع الصحية فقد سبق لهن على الأرجح استعمال موانع الحمل القابلة للحقن. بالإضافة إلى أن عدم الاستمرار في استخدام موانع الحمل القابلة للحقن كان على الأرجح أقل لدى المتعاملات مع الموظفين في الصحة الإنجابية المجتمعية المرتكز طوال ثلاث دورات من الحقن مقارنة بالمتعاملات مع المواقع الصحية.
الاستنتاج
إن تلقي موانع الحمل القابلة للحقن من قبل الموظفين في الصحة الإنجابية المجتمعية المرتكز قد أثبت أنه آمن، ومقبول لهذه العينة من النساء الأثيوبيات مثل تلقيه من العاملين الصحيين على امتداد المواقع الصحية. وتضيف هذه النتائج إلى كم البيّنات المتزايد الذي يدعم إنشاء، وتقديم، وتوسيع نطاق برامج تدريب العاملين الصحيين المجتمعيين مثل الموظفين في الصحة الإنجابية المجتمعية المرتكز على إعطاء موانع الحمل القابلة للحقن.
Résumé
Objectif
Déterminer si le personnel soignant communautaire d’une région rurale d'Éthiopie peut fournir des contraceptifs injectables aux femmes avec des niveaux de sécurité, d'efficacité et d'acceptabilité similaires à ceux des agents de vulgarisation sanitaire (AVS).
Méthodes
Il s'agissait d'un essai d'intervention communautaire prospectif non randomisé, conçu pour tester la fourniture de contraceptifs injectables par les agents communautaires de santé reproductive (ACSR). Les taux d'efficacité, de sécurité, d'acceptabilité et de continuité étaient les résultats recherchés. Les résultats observés lors de l'administration de contraceptifs injectables par les AVS dans les postes sanitaires et lors de leur administration par les ACSR ont été comparés au moyen de tests χ2 pour l'association entre les variables nominales et les tests-t d’échantillons indépendants, afin de déterminer les différences entre les moyennes du groupe.
Résultats
Un total de 1 062 femmes ont participé à l'étude. Par rapport aux patientes des postes sanitaires, les patientes des ACSR étaient, en moyenne, un peu plus âgées, moins susceptibles d'être mariées et moins instruites, et elles avaient beaucoup plus d'enfants en vie. Les femmes s'adressant aux ACSR étaient aussi nettement plus susceptibles d'utiliser des contraceptifs injectables pour la première fois; les patientes des postes sanitaires étaient plus susceptibles de les avoir déjà utilisés dans le passé. En outre, les patientes des ACSR étaient moins susceptibles de cesser d'utiliser les contraceptifs injectables après trois cycles d’injection que les patientes des postes sanitaires.
Conclusion
L'administration de contraceptifs injectables par les ACSR s'est révélée aussi sûre et acceptable pour cet échantillon de femmes éthiopiennes que l'administration dans les postes sanitaires par les AVS. Ces résultats s'ajoutent à la quantité croissante de preuves encourageant le développement, l'introduction et l'augmentation du nombre de programmes de formation d’agents de santé communautaires, comme les ACSR, pour administrer sans danger des contraceptifs injectables.
Resumen
Objetivo
Determinar si los trabajadores sanitarios comunitarios activos en zonas rurales de Etiopía pueden suministrar contraceptivos inyectables a mujeres con niveles de seguridad, eficacia y aceptabilidad similares a los registrados por los trabajadores de extensión de la sanidad (HEW, por sus siglas en inglés).
Métodos
Este fue un ensayo prospectivo, no aleatorizado, de intervención comunitaria y diseñado para probar el suministro de contraceptivos inyectables por parte de agentes sanitarios comunitarios reproductivos (CBRHA, por sus siglas en inglés). Los resultados de interés eran la eficacia, la seguridad, la aceptabilidad y la continuación. Se compararon los resultados observados cuando los HEW administraron los contraceptivos inyectables en centros de salud y cuando los administraron los CBRHA. Esta comparación se realizó mediante pruebas de χ2 para asociar las variables categóricas y mediante pruebas de la t para realizar muestras independientes, con el fin de determinar las diferencias entre los grupos.
Resultados
En el estudio participaron un total de 1062 mujeres. En comparación con las pacientes de los centros de salud, las pacientes de los CBRHA eran ligeramente mayores, presentaban una menor probabilidad de estar casadas, una educación inferior y tenían significativamente más hijos. Las mujeres que solicitaron los servicios de los CBRHA también presentaban una mayor probabilidad de utilizar contraceptivos inyectables por primera vez; las pacientes del centro de salud presentaban una mayor probabilidad de haberlos utilizado en el pasado. Asimismo, las pacientes de los CBRHA presentaban una probabilidad menor de discontinuar el uso de contraceptivos inyectables en ciclos de tres inyecciones, en comparación con las pacientes del centro de salud.
Conclusión
En esta muestra de mujeres etíopes, se probó que recibir contraceptivos inyectables de los CBRHA es tan seguro como recibirlos en los centros de salud de los HEW. Estos resultados se añadieron al conjunto cada vez más amplio de evidencias que apoyan el desarrollo, la introducción y la ampliación de programas de formación de los trabajadores sanitarios comunitarios, como los CBRHA, para administrar contraceptivos inyectables con seguridad.
摘要
目的
旨在确定埃塞俄比亚农村地区社区的卫生工作者能否为妇女提供在安全性、有效性和可接受性上与健康推广人员水平类似的避孕针剂。
方法
这是一项前瞻性非随机性社区干预试验,旨在测试社区的生殖健康代理(CBRHAs)提供的避孕针剂。有效性、安全性、可接受性和续用率是本研究关注的结果。研究主要观察卫生站的健康推广人员和社区的生殖健康代理(CBRHAs)注射避孕针剂的情况,并将两种结果进行χ2 检验以确定各类别变量之间的关联,同时还对独立样本进行t-检验来确定组平均值之间的差异。
结果
总计1062名妇女参加了本项研究。与卫生站服务对象相比,社区的生殖健康代理的服务对象平均略微年长,已婚较少,教育程度较低,并且服务对象的子女存活明显较多。而且社区的生殖健康代理处寻求服务的妇女更可能是第一次使用避孕针剂;而卫生站服务对象则可能已经使用过避孕针剂。此外,与卫生站服务对象相比,社区的生殖健康代理的服务对象不太可能在三个注射周期期间停止使用避孕针剂。
结论
对埃塞俄比亚妇女而言,从社区的生殖健康代理和从卫生站的健康推广人员接收避孕针剂具有一样的安全性和可接受性。这些研究研果提供了更多证据,以支持开发、引进、扩大针对社区卫生工作人员诸如社区的生殖健康代理开展的安全注射避孕针剂的培训项目。
Резюме
Цель
Определить, могут ли общинные медицинские работники обеспечивать женщин инъекционными противозачаточными средствами на том же уровне безопасности, эффективности и приемлемости, что и работники службы санитарного просвещения (ССП).
Методы
Описывается проведенное на уровне общины проспективное нерандомизированное интервенционное испытание, планом которого предусматривалась проверка результатов распространения инъекционных контрацептивов общинными агентами по репродуктивному здоровью (ОАПОРЗ). Результатами, представлявшими интерес, были: эффективность, безопасность и приемлемость данной услуги, а также доля лиц, продолжающих ею пользоваться. Наблюдаемые результаты распространения инъекционных противозачаточных средств работниками ССП, занимающими должности медицинского персонала, и ОАПОРЗ сравнивались со средними значениями χ2-тестов по выявлению корреляции между категориальными переменными и t-тестов для независимых выборок с целью определения различий между средними значениями по группам.
Результаты
Всего в исследовании приняли участие 1062 женщины. По сравнению с посетителями медпунктов, клиенты ОАПОРЗ были, в среднем, несколько старше, имели меньшую вероятность нахождения в браке, более низкий уровень образования и значительно больше живых детей. Кроме того, женщины, обращавшиеся к услугам ОАПОРЗ, со значительно более высокой вероятностью пользовались инъекционными контрацептивами впервые, тогда как клиенты медпунктов с большей вероятностью уже использовали их в прошлом. Помимо этого, у клиентов ОАПОРЗ вероятность прекращения пользования инъекционными контрацептивами после трех циклов инъекций была ниже, чем у посетителей медпунктов.
Вывод
Для данной выборки эфиопских женщин получение инъекционных противозачаточных средств у ОАПОРЗ и у работников ССП в медпунктах оказалось одинаково безопасным и приемлемым. Эти результаты дополняют все более растущий объем данных, свидетельствующих в пользу разработки, внедрения и широкого развертывания программ подготовки медработников типа ОАПОРЗ на уровне общин для безопасного распространения инъекционных противозачаточных средств.
Introduction
In many countries, human resources for health are either poorly distributed or in short supply.1–3 To address this critical shortage of health professionals, international health bodies and expert observers have advocated shifting specific health-care tasks from highly-trained medical staff to providers with minimal training, depending on the type of intervention.4–7 This systematic delegation of tasks to less skilled providers, formerly referred to as substitution, is not new.8 However, for such continued and expanded task shifting and sharing to be viable, these services must be delivered just as safely and effectively by less skilled providers as by medical staff.
Numerous factors, among them the availability of staff and commodities, contribute to the quality of the care available at basic health facilities.2,9 While several countries have experimented with shifting the distribution of short-term methods of family planning to community-based distributors or health volunteers,10–12 much unmet need for contraceptives remains.13 Shifting the task of providing longer-acting injectable contraceptives, such as depot medroxyprogesterone acetate (DPMA), to community workers can provide access to these methods to a larger number of women.14,15
Community-based models of DMPA distribution have been successful in several developing country contexts. Most recently, studies conducted in Madagascar, Malawi and Uganda have demonstrated that community health workers who receive proper training in screening, injection technique and counselling can administer DMPA injections to women in rural areas just as safely as clinic-based providers and with comparable rates of acceptability and continuation.11,12,16–18 In numerous settings, DMPA has emerged as the preferred method of contraception primarily because it is effective, can be used privately, has a longer period of action than oral contraceptives or condoms and requires less frequent supply.19 In Ethiopia, DMPA is now the method of choice for over 70% of women using modern methods of contraception, compared with almost no utilization as recently as 1990.20,21 However, women in rural Ethiopia continue to have a low rate of contraceptive use (11%) and a high unmet need (36%).20
Like many developing countries, Ethiopia has a shortage of highly-skilled health-care providers. In 2003, the Government of Ethiopia launched the Health Extension Programme to develop a body of salaried basic-level health-care providers – health extension workers (HEWs) – who could increase the availability and coverage of basic health services for Ethiopia’s large rural population.22,23 While HEWs have been an innovative addition to the Ethiopian health sector, their ability to conduct community outreach varies depending on the time demanded by the wide range of health interventions for which they are responsible. Another group of workers composed of volunteers known as community-based reproductive health agents (CBRHAs) was initially mobilized to provide basic family planning services and referrals, although they have acquired more responsibilities in the community and often support the activities of the HEWs.24 However, CBRHAs are lay health workers and are thus only allowed to distribute oral contraceptives and condoms, for which they can receive a small commission. To date, CBRHAs are not authorized to administer DMPA because it requires an intramuscular injection. As previous research has demonstrated, contraceptive distribution by community health workers such as CBRHAs can increase the use of contraceptives in populations living beyond the reach of health facilities,25,26 as well as eliminate an additional referral from CBRHAs to HEWs before women can begin using their method of choice.
The Ethiopian Ministry of Health’s National Reproductive Health Strategy 2006–2015 states as a goal to “delegate to the lowest service delivery level possible, the provision of all family planning methods, especially long-term and permanent methods, without compromising safety or quality of care”.27 CBRHAs are an integral part of attempts to provide community education and modern contraceptives to women in rural communities. However, most of their outreach activities are supported by nongovernmental organizations and private sector funds and are limited to delivering oral contraceptives and condoms. HEWs can provide these methods, as well as injectable contraceptives, and training is currently under way to also allow them to provide contraceptive implants.28 Additional methods, such as intrauterine devices and sterilization, are provided by clinical officers at health centres or hospitals.
The objective of this study was to determine if, with appropriate training, CBRHAs can administer injectable contraceptives to women in a rural region of Ethiopia with the same effectiveness, safety and acceptability as HEWs.
Setting and intervention
This project took place in Tigray region, Ethiopia, as a collaboration between the Bixby Center at the University of California at Berkeley and the Tigray Regional Health Bureau. Tigray’s sizable rural population (80% of the region’s 4.3 million people),29 among other factors, contributes to the persistence of disparities in the use of family planning methods. Almost a quarter (24%) of the rural women in Tigray report an unmet need for family planning to limit or space their pregnancies and 75% of the women in Tigray who intend to use contraception in the future want to use injectables.20 The use of community-based health workers such as CBRHAs to distribute injectable contraceptives can put DMPA within reach of women who are not currently accessing modern methods of contraception or who are dissatisfied with condoms or oral contraceptive pills.
As of 2009, Tigray had deployed 1200 HEWs to health posts (enough to staff 80% of the targeted positions).30 As a result of investment by the government and by international and local implementing organizations, almost 1500 CBRHAs are currently active in Tigray.30
Four village sites (tabia) in each of two districts (woredas) of the region (Kola Tembien and Tanqua Abergel) were included for participation, for a total of eight intervention sites. Before the start of research activities, investigators contacted community leaders and key community persons and explained the objectives of the study. Since the provision of injectable contraceptives was a new service being offered by CBRHAs, these leaders were instrumental in diffusing information about the project throughout their communities. The study included 30 CBRHAs and 15 HEWs from the target areas. There were approximately four CBRHAs and two HEWs per tabia. While HEWs were already authorized to provide DMPA before the intervention, it was important to standardize the training received by both arms of providers to ensure comparability. A 10-day training addressed topics related to family planning methods, study protocol, screening requirements for the exclusion of participants, injection administration, infection prevention and reporting procedures. CBRHAs and HEWs who successfully completed the classroom training moved on to a two-stage clinic-based practical training in which safe injection technique was emphasized.
The DMPA was supplied specifically for the project and purchased from DKT-Ethiopia, a social marketing organization that markets and distributes a 3-month intramuscular DMPA product in Ethiopia. The product comes in 1-ml vials, each containing 150 mg, which is the standard dose to be administered every three months. For a single administration, a 2-ml syringe with a needle measuring 0.8 × 40 mm was used.
Methods
This was a prospective non-randomized community intervention trial conducted in 2008 and 2009. Women self-selected into different arms of the study based on the type of provider they visited for family planning services. Safety, acceptability, effectiveness and continuation rates were the outcomes of interest. The outcome rates in participants who received DMPA from CBRHAs were compared with the outcome rates in participants who received DMPA from HEWs. We based the sample size of 1000 women on the need to test for non-inferiority of the services provided by CBRHAs. We assumed a continuation rate of 65% after injection among HEW clients and a continuation rate of at least 55% in the CBRHA group (for a maximum difference of 10% between arms) as being equivalent. We also assumed a loss to follow-up of 10%, a design effect of 2.0 and similar recruitment rates among all 8 villages.
All women of reproductive age who approached a participating provider to request a contraceptive method and who wished to use DMPA were recruited for the study. Participation was voluntary. After obtaining consent, the CBRHA or HEW screened each participant to see if she was eligible for contraceptive use based on current WHO recommendations. Consistent with their usual practice, both types of providers referred clients who were medically ineligible to the nearest health facility. No compensation was given to participants, but during the study DMPA was given free of charge. Both types of providers explained to the participants that in the private sector DMPA can normally be purchased for a nominal fee.
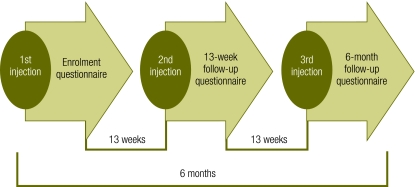
We used three survey instruments over the course of the project: an enrolment questionnaire, a 13-week follow-up questionnaire and a 6-month follow-up questionnaire. Fig. 1 shows the timing of the injections and the interview schedule for the three consecutive injections.
Fig. 1.
Timeline of enrolment and follow-up
The data collected included sociodemographic characteristics, satisfaction with DMPA as a method, satisfaction with the provider, quality of the service provided, knowledge and experience of side-effects, reasons for discontinuing the injections, willingness to pay for injectables and preferred point of care for DMPA administration.
For the data analysis we used SPSS version 15.0 (SPSS Inc., Chicago, United States of America). Differences in responses between the two client groups were assessed with χ2 tests for association among categorical variables and t-tests for independent samples to determine differences between group means. Statistical significance was set at P < 0.05.
Ethical approval was obtained from the Committee for the Protection of Human Subjects at the University of California at Berkeley and from the Tigray Regional Health Bureau in Ethiopia. This intervention was registered with ClinicalTrials.gov with the identifier NCT01288274.
Results
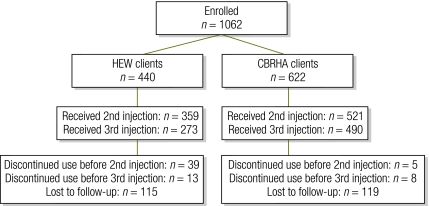
A total of 1062 women participated in this study, including 662 who were receiving services from CBRHAs. Fig. 2 shows the number who enrolled, who continued the injections and who were lost to follow-up.
Fig. 2.
Enrolment, continuations and loss to follow up
CBRHA, community-based reproductive health agent; HEW, health extension worker.
Table 1 shows the characteristics of CBRHA and HEW clients. CBRHA clients were, on average, slightly older, less likely to be married and less educated than HEW clients, and they had significantly more living children. In addition, women seeking services from CBRHAs were significantly more likely to be using DMPA for the first time.
Table 1. Background characteristics of clients of health extension workers (HEWs) and community-based reproductive health agents (CBRHAs), by provider type, Ethiopia, 2008–2009.
| Sample characteristics | HEW clients | CBRHA clients |
|---|---|---|
| (n = 440) | (n = 622) | |
| Mean age (years) | 28.4 | 30.0* |
| Married (%) | 92.4 | 88.0* |
| Mean age at first marriage (years) | 15.5 | 16.1* |
| Mean age at first pregnancy (years) | 17.9 | 18.3* |
| Mean no. of living children | 3.6 | 4.0* |
| No education (%) | 78.1 | 89.4* |
| Using DMPA for first time (%) | 45.9 | 58.4* |
DMPA, depot medroxyprogesterone acetate; * P < 0.05.
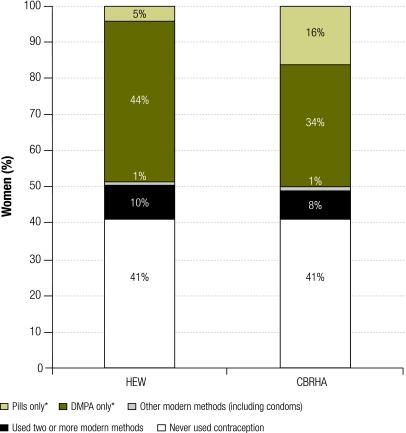
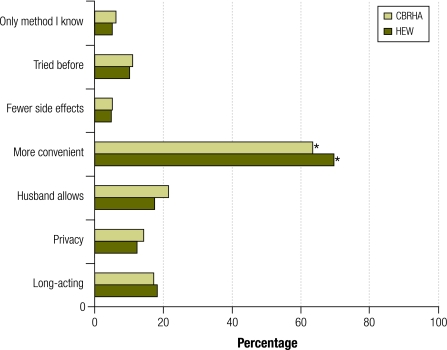
Rates of previous use of modern contraception were similar between the two groups; 41% of the women in both groups reported that they had never used a modern contraceptive method before this project (Fig. 3). However, CBRHA clients were significantly less likely to have used DMPA in the past than HEW clients (34% versus 44%, respectively). At enrolment, providers asked women to cite their main reasons for choosing DMPA. Significantly more HEW clients mentioned convenience, although the majority of CBRHA clients also gave this response (Fig. 4). In this sample, the husband’s permission, period of action and privacy were less influential in women’s choice to use DMPA.
Fig. 3.
Previous use of contraception among study population, by provider type, Ethiopia, 2008–2009
CBRHA, community-based reproductive health agent; DMPA, depot medroxyprogesterone acetate; HEW, health extension worker; * P < 0.01.
Inconsistencies arise in some values due to rounding.
Fig. 4.
Client reasons for choosing depot medroxyprogesterone acetate, by provider type, Ethiopia, 2008–2009
CBRHA, community-based reproductive health agent; HEW, health extension worker; *P < 0.05.
HEW clients were more likely to discontinue using DMPA over the course of the project, particularly between the 13th week and the 6th month (Table 2). While approximately 80% of clients of both types of providers received their second injection, the number who did so among CBRHA clients was slightly but significantly higher. By the time the 13-week follow-up questionnaire was administered, 9% of HEW clients had discontinued the injections, compared with only 1% of CBRHA clients. Similarly, a larger proportion of CBRHA clients than HEW clients received the third injection (79% versus 62%, respectively). Discontinuation rates after the 13-week follow-up questionnaire continued to be higher among HEW clients, as 4% failed to receive the third injection compared with 2% of CBRHA clients. One pregnancy was reported in the 6-month follow-up questionnaire, although the woman in question had discontinued DMPA after her second injection. Women gave “trying to get pregnant” as the most common reason for discontinuing the injections, and the majority of women who discontinued DMPA in favour of another method reported having switched to implants (data not shown).
Table 2. Proportion of women who did and did not receive a second or third injection of depot medroxyprogesterone acetate, by provider type, Ethiopia, 2008–2009.
| Continuation | 2nd injection |
3rd injection |
|||||
|---|---|---|---|---|---|---|---|
| HEW clients |
CBRHA clients |
P | HEW clients |
CBRHA clients |
P | ||
| (n = 440) | (n = 622) | (n = 440) | (n = 622) | ||||
| Received injection (%) | 81.6 | 83.7 | < 0.01 | 62.3 | 78.8 | < 0.01 | |
| Discontinued injections (%) | 8.9 | 0.8 | < 0.01 | 3.6 | 1.5 | 0.03 | |
CBRHA, community-based reproductive health agent; HEW, health extension worker.
Proportions do not add up to 100 due to loss to follow up.
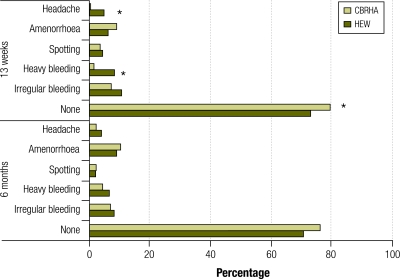
Women receiving injections from CBRHAs were less likely to report side-effects resulting from the DMPA after their second injection (Fig. 5). However, by the 6-month interview, differences in reported side-effects between CBRHA and HEW clients were no longer noted. Reactions at the injection site were very few. The only significant difference was reported at the 13-week follow-up, when more CBRHA clients than HEW clients reported induration at the injection site (2.1% versus 0.5%, respectively). This difference had disappeared by the third follow-up, at which point less than 1.5% of the women reported any problems (data not shown).
Fig. 5.
Reported side-effects following second and third injections of depot medroxyprogesterone acetate, Ethiopia, 2008–2009
CBRHA, community-based reproductive health agent; HEW, health extension worker; *P < 0.05.
As shown in Table 3, the women in both study arms were highly satisfied with DMPA as a method and with their provider. CBRHAs provided care similar in quality to the care provided by HEWs. The only differences reported were that CBRHAs were less likely than HEWs to give written appointment reminders and significantly more likely to offer condoms in addition to DMPA. Differences between the two groups were noted in the type of knowledge about potential side-effects that the women retained. By the 6-month follow-up survey, CBRHA clients could recall significantly more of the side-effects that the CBRHAs had explained to them during DMPA consultations. At the 13-week follow-up survey HEW clients could name significantly more of the adverse events for which they were told to visit a health centre, although the difference had almost disappeared by the 6-month follow-up survey.
Table 3. Care received by surveyed women due to injection of depot medroxyprogesterone acetate (DMPA) from health extension workers (HEWs) and by community-based reproductive health agents (CBRHAs), Ethiopia, 2008–2009.
| Characteristic | 13 week questionnaire |
6 month questionnaire |
|||||
|---|---|---|---|---|---|---|---|
| HEW clients (%) |
CBRHA clients (%) |
P |
HEW clients (%) |
CBRHA clients (%) |
P |
||
| (n = 398) | (n = 526) | (n = 286) | (n = 498) | ||||
| Satisfaction | |||||||
| With DMPA | 98.4 | 99.2 | 0.26 | 100.0 | 98.8 | 0.06 | |
| With provider | 97.6 | 95.6 | 0.10 | 97.6 | 96.2 | 0.29 | |
| Provider services | |||||||
| Gave written appointment reminder | 98.9 | 92.8 | < 0.01 | 100.0 | 96.4 | < 0.01 | |
| Explained potential side-effects | 98.1 | 98.8 | 0.40 | 98.9 | 98.1 | 0.41 | |
| Discussed STI/HIV/AIDS | 95.9 | 95.1 | 0.58 | 98.9 | 97.6 | 0.20 | |
| Explained that DMPA does not protect against HIV | 97.5 | 97.1 | 0.68 | 98.9 | 99.4 | 0.47 | |
| Offered condoms in addition | 58.3 | 75.8 | < 0.01 | 72.7 | 80.4 | 0.01 | |
| Naming of side-effects from DMPA | |||||||
| Irregular bleeding | 35.9 | 34.9 | 0.75 | 31.5 | 43.2 | < 0.01 | |
| Heavy bleeding | 31.7 | 19.9 | < 0.01 | 33.9 | 31.2 | 0.43 | |
| Spotting | 10.3 | 12.3 | 0.36 | 12.2 | 15.3 | 0.24 | |
| Amenorrhoea | 18.2 | 38.7 | < 0.01 | 20.3 | 41.5 | < 0.01 | |
| Headache | 16.4 | 10.3 | < 0.01 | 16.8 | 10.8 | 0.02 | |
| Weight gain | 4.5 | 11.7 | < 0.01 | 9.4 | 21.4 | < 0.01 | |
| Weight loss | 1.3 | 1.0 | 0.61 | 0.7 | 2.0 | 0.15 | |
| Irritability | 3.4 | 8.8 | < 0.01 | 1.7 | 6.9 | < 0.01 | |
| Hair loss | 5.8 | 11.5 | < 0.01 | 10.1 | 19.1 | < 0.01 | |
| Naming of side-effects requiring visit to health centre | |||||||
| Severe headache | 38.5 | 31.1 | 0.03 | 28.1 | 30.5 | 0.47 | |
| Very heavy bleeding | 61.3 | 53.3 | 0.02 | 66.3 | 57.5 | 0.02 | |
| Pregnancy | 21.4 | 16.4 | 0.07 | 31.2 | 32.8 | 0.66 | |
| Chest pain | 4.3 | 5.8 | 0.32 | 2.1 | 1.6 | 0.65 | |
AIDS, acquired immunodeficiency syndrome; HIV, human immunodeficiency virus; STI, sexually-transmitted infection.
In both follow-up surveys CBRHA clients were overwhelmingly in favour of receiving their injections at home or in the home of the CBRHA (Table 4). A key finding was that after they received their third injection, 52% of the HEW clients expressed the desire to be given their injections at home. In this sample the preference for receiving injections at home may have been related to the fact that almost half of the women in both study arms reported having difficulty in getting to a health facility for family planning.
Table 4. Contraceptive methods discussed by provider with surveyed women due to receive injection of depot medroxyprogesterone acetate (DMPA) and preferred point of service, by provider type, Ethiopia, 2008–2009 .
| Characteristic | 13 week questionnaire |
6 month questionnaire |
|||||
|---|---|---|---|---|---|---|---|
| HEW clients (%) |
CBRHA clients (%) |
P | HEW clients (%) |
CBRHA clients (%) |
P | ||
| (n = 398) | (n = 526) | (n = 286) | (n = 498) | ||||
| Other family planning methods discussed | |||||||
| Condoms | 25.9 | 26.8 | 0.76 | 25.4 | 34.1 | 0.01 | |
| OCP | 85.6 | 82.8 | 0.27 | 73.6 | 78.3 | 0.14 | |
| Implants | 51.1 | 42.5 | 0.01 | 64.8 | 54.1 | < 0.01 | |
| IUD | 7.0 | 10.6 | 0.06 | 10.6 | 8.9 | 0.44 | |
| Sterilization | 3.7 | 7.9 | 0.01 | 7.4 | 14.9 | < 0.01 | |
| Preferred point of service | |||||||
| Health post | 48.8 | 2.9 | < 0.01 | 43.4 | 2.4 | < 0.01 | |
| Client’s home | 47.4 | 85.7 | < 0.01 | 51.6 | 84.2 | < 0.01 | |
| CBRHA’s home | 3.8 | 11.4 | < 0.01 | 5.0 | 13.4 | < 0.01 | |
| Difficulty getting to clinic for family planning | 44.4 | 48.6 | 0.22 | 44.3 | 48.5 | 0.26 | |
CBRHA, community-based reproductive health agent; HEW, health extension workers; IUD, intrauterine device; OCP, oral contraceptive pill.
Discussion
Our findings reflect the extent to which community health workers such as CBRHAs can provide access to injectable contraceptives at the community level. The findings are consistent with results from studies in which community health workers have safely and effectively administered DMPA in Madagascar, Malawi and Uganda.10–12 In this study in Tigray, CBRHAs provided DMPA to more first-time users of the method, which underscores the role of these community health workers in expanding access to family planning methods other than condoms and the pill. Clients of CBRHAs were also less likely to discontinue the injections after three cycles, perhaps because having CBHRAs come to their “doorstep” makes it unnecessary for women to visit health posts and facilitates their adherence to the DMPA injection schedule. Overall, differences in the reported quality of service provision were very few. Both groups of women were able to recall the side-effects of DMPA and the problems requiring medical attention. The fact that a slightly larger number of CBRHA clients reported induration at the site of the first injections raises the need to periodically monitor CBRHAs and offer them refresher training to ensure that they continue to practice proper injection technique. Overall, CBRHAs delivered DMPA to women very safely and with high acceptability, with very few problems at the injection site.
Women cited convenience, husband’s consent and the product’s length of action as the key reasons for using DMPA. Though privacy was cited less frequently, community-based interventions allow women quick and confidential access to methods such as DMPA. The nature of the method and its delivery mechanism are appealing to women who may not want to openly use one of the short-term contraceptive methods more commonly available.
As expected, the overwhelming majority of women who chose CBRHAs as their providers reported wanting to receive DMPA injections at home, yet at both follow-up surveys around half of HEW clients said that they would choose this option as well if they could. Unfortunately, we did not gather in-depth qualitative information from women about why they chose to receive DMPA from CBRHAs rather than HEWs. However, almost half of the women in the sample reported difficulty in getting to a facility for family planning purposes and since CBRHAs administered DMPA injections competently and to the satisfaction of their clients, the provision of injectable contraceptives in women’s households by CBRHAs can satisfy women’s preferences in terms of location and improve their adherence to the injection schedule.
In 2009, a WHO technical consultation reviewed evidence on the community-based provision of injectable contraceptives from 16 projects (including the present study) in nine countries.31 The conclusions were that with adequate support and skills training, community health workers can administer injectable contraceptives as safely and effectively as facility-based providers, and that continuation and satisfaction rates are high when the providers are community health workers. Including these workers in a distribution model for family planning can increase the contraceptive options available and their accessibility, especially in populations with limited access to facilities and to a variety of methods.
As a result of the demonstration projects mentioned above, Uganda has moved forward with a national policy to allow community health workers to provide injectable contraceptives and several countries, including Afghanistan, Madagascar and Malawi, are taking steps in that direction. However, such a change in policy depends on governments’ ability to identify a source of funding for the training and monitoring of the workers. In Uganda, for example, changing policy has taken approximately five years, despite research showing that community health workers were highly capable of providing DMPA.11 As the Health Extension Programme has been scaled up in Ethiopia, the Ministry of Health is currently considering CBRHAs as merely health promotion agents. However, HEWs have not been able to consistently provide as much community outreach as expected given that most of their time is spent providing clinical care, so the role of CBRHAs may be reviewed in the future.
The demand for injectable contraceptives in Ethiopia has been amply documented and both the results of this study and the technical review of the evidence highlight the need for plans to introduce, sustain, and scale up the administration of DMPA by CBRHAs in Ethiopia. Admittedly, training large numbers of these workers can impose a heavy financial burden on health systems with few resources. Innovative public–private partnership models could be one solution. A combination of social marketing and community-based distribution methods could help defray some of the costs of training and monitoring, generate income for community health workers and increase women’s access to modern contraceptive methods.
Acknowledgements
The authors thank the Tigray Regional Health Bureau, especially Gebre Ab Barnabas and the late Araya Kahsu Abraha; Martine Holston and Deborah Karasek; project trainers; woreda heads; project coordinators and supervisors, and participating HEWs and CBRHAs. They also thank all the women who have participated in this study.
Funding:
This project was a collaboration between the Bixby Center for Population, Health and Sustainability; the Tigray Health Bureau, Ethiopia, and Venture Strategies for Health and Development. It received financial support from the Brush Foundation, and during its last stages, it benefited from the support of Venture Strategies Innovations.
Competing interests:
None declared.
References
- 1.Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, et al. Human resources for health: overcoming the crisis. Lancet. 2004;364:1984–90. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 2.Naicker S, Plange-Rhule J, Tutt RC, Eastwood JB. Shortage of healthcare workers in developing countries-Africa. Ethn Dis. 2009;19:S1-60–4. [PubMed] [Google Scholar]
- 3.Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M, Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health. 2011;9:1. doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The world health report 2006: working together for health Geneva: World Health Organization; 2006. [Google Scholar]
- 5.Lehmann U, Van Damme W, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa? Hum Resour Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Task shifting: rational redistribution of tasks among health workforce teams. Global recommendations and guidelines Geneva: World Health Organization; 2008. [Google Scholar]
- 7.Culwell KR, Vekemans M, de Silva U, Hurwitz M, Crane BB. Critical gaps in universal access to reproductive health: contraception and prevention of unsafe abortion. Int J Gynaecol Obstet. 2010;110(Suppl):S13–6. doi: 10.1016/j.ijgo.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Dovlo D. Using mid-level cadres as substitutes for internationally mobile health professionals in Africa. A desk review. Hum Resour Health. 2004;2:7. doi: 10.1186/1478-4491-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stephenson R, Beke A, Tshibangu D. Community and health facility influences on contraceptive method choice in the Eastern Cape, South Africa. Int Fam Plan Perspect. 2008;34:62–70. doi: 10.1363/3406208. [DOI] [PubMed] [Google Scholar]
- 10.Katz K, Ngalande RC, Jackson E, Kachale F, Mhango C. Evaluation of community-based distribution of DMPA by health surveillance assistants in Malawi United States Agency for International Development & Malawi Ministry of Health & Family Health International; 2010. [Google Scholar]
- 11.Stanback J, Mbonye AK, Bekiita M. Contraceptive injections by community health workers in Uganda: a nonrandomized community trial. Bull World Health Organ. 2007;85:768–73. doi: 10.2471/BLT.07.040162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatzell-Hoke T, Wheeler S, Blumenthal P, Rasamihajamanana E, Razafindravony B. Safety, feasibility, and acceptability of community-based distribution (CBD) of depot medroxy progesterone acetate (DMPA) in Madagascar Research Triangle Park: Family Health International & Madagascar Ministère de la Santé & and United States Agency for International Development; 2008. [Google Scholar]
- 13.White JS, Speizer IS. Can family planning outreach bridge the urban-rural divide in Zambia? BMC Health Serv Res. 2007;7:143. doi: 10.1186/1472-6963-7-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malarcher S, Meirik O, Lebetkin E, Shah I, Spieler J, Stanback J. Provision of DMPA by community health workers: what the evidence shows. Contraception. 2010 doi: 10.1016/j.contraception.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Prata N, Vahidnia F, Potts M, Dries-Daffner I. Revisiting community-based distribution programs: are they still needed? Contraception. 2005;72:402–7. doi: 10.1016/j.contraception.2005.06.059. [DOI] [PubMed] [Google Scholar]
- 16.Family Health International Madagascar tests the CBD of DMPA: initial success spurs plans for expansion. Fam Health Res. 2007;1:2. [Google Scholar]
- 17.Richardson F, Chirwa M, Fahnestock M, Bishop M, Emmart P, McHenry B. Community-based distribution of injectable contraceptives in Malawi Washington: Futures Group International; 2009. [Google Scholar]
- 18.Hamblin K, Msefula M. Malawi: distribution of DMPA at the community level – lessons learned Arlington: United States Agency for International Development; 2009. [Google Scholar]
- 19.Lande R, Richey C. Expanding services for injectables (Population Reports, Series K, Injectables and Implants, No. 6). Baltimore: John Hopkins Bloomberg School of Public Health; 2006. Available from: http://www.populationreports.org/k6/ [accessed 13 April 2011]. [Google Scholar]
- 20.Ethiopia Demographic and Health Survey 2005 Calverton: Central Statistical Agency of Ethiopia and Macro International; 2006.
- 21.National Family and Fertility Survey 1990. Addis Ababa: Central Statistical Agency of Ethiopia; 1990.
- 22.Sebastian MS, Lemma H. Efficiency of the health extension programme in Tigray, Ethiopia: a data envelopment analysis. BMC Int Health Hum Rights. 2010;10:16. doi: 10.1186/1472-698X-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koblinsky M, Tain F, Gaym A, Karim A, Carnell M, Tesfaye S. Responding to the maternal health care challenge: the Ethiopian Health Extension Program. Ethiop J Health Dev. 2010;24:105–9. [Google Scholar]
- 24.Giday T, Asnake M, Wilder J. Ethiopia's Health Extension Program: Pathfinder International's support 2003-2007 Watertown: Pathfinder International; 2008.
- 25.Curtis C, Huber D, Moss-Knight T. Postabortion family planning: addressing the cycle of repeat unintended pregnancy and abortion. Int Perspect Sex Reprod Health. 2010;36:44–8. doi: 10.1363/3604410. [DOI] [PubMed] [Google Scholar]
- 26.Jahanfar S, Ghodsy Z, Shahpoorian F, Jamshidi R. Community-based distribution and contraception usage in Iran. J Fam Plann Reprod Health Care. 2005;31:194–7. doi: 10.1783/1471189054483960. [DOI] [PubMed] [Google Scholar]
- 27.National Reproductive Health Strategy 2006-2015 Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health; 2006.
- 28.Asnake M, Tilahun Y. Scaling up community-based service delivery of Implanon: the integrated family health program's experience training health extension workers Watertown: Pathfinder International, Integrated Family Health Program; 2010. [Google Scholar]
- 29.Summary and statistical report of the 2007 Population and Housing Census of Ethiopia Addis Ababa: Central Statistical Agency of Ethiopia; 2008.
- 30.Tigray Health Bureau profile of 2001 EFY (2009 GC) Mekelle: Tigray Regional Health Bureau; 2009.
- 31.Stanback J, Spieler J, Shah I, Finger WR, Expanding Access to Injectable Contraceptives Technical Consultation Participants Community-based health workers can safely and effectively administer injectable contraceptives: conclusions from a technical consultation. Contraception. 2010;81:181–4. doi: 10.1016/j.contraception.2009.10.006. [DOI] [PubMed] [Google Scholar]