Abstract
Objective
To assess levels, trends and gaps between the poorest and the richest in selected health and human development indicators in Bangladesh.
Methods
Data for selected indicators associated with sociodemographic characteristics among ever-married women, contraception use, child vaccination, antenatal care practices and health conditions were extracted from the Bangladesh Demographic and Health Surveys conducted in 1993–94, 1996–1997, 1999–2000, 2004 and 2007. Results for the whole sample and for the poorest and the richest wealth quintiles are presented.
Findings
Positive trends were noted in urbanization, availability of electricity, age at first marriage, use of modern contraception, access to skilled antenatal care, child vaccination, knowledge of human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome and overweight and obesity. In contrast, negative trends were seen in factors such as literacy, infant and child mortality, fertility rate, home delivery and malnutrition and underweight. However, changes in these indicators differed between the poorest and richest quintiles. For instance, only the richest quintile experienced rapid urbanization, whereas illiteracy declined more among the poorest. Noteworthy gaps were found in almost all factors. Rich–poor gaps in urbanization, age at marriage, fertility, condom use, home delivery and overweight increased; in contrast, gaps in education, water and sanitation, use of contraception (except condoms) and child vaccination declined.
Conclusion
Persistent inequities in Bangladesh endanger equitable and sustainable human development in the country. Pro-poor development strategies based on the principles of equity and quality should be implemented to narrow existing gaps and further promote holistic and equitable human development.
ملخص
الغرض
قياس المستويات، والاتجاهات، والثغرة الموجودة بين أفقر الفئات وأغنى الفئات من حيث المؤشرات المنتقاة للتنمية الصحية والبشرية في بنغلاديش.
الطريقة
استُخلِصَت المعطيات الخاصة بمؤشرات منتقاة ترتبط بالسمات الاجتماعية والديموغرافية بين النساء المتزوجات، واستخدام موانع الحمل، وتطعيم الأطفال، وممارسات الرعاية السابقة للولادة، والحالة الصحية، من المسوحات الديموغرافية والصحية لبنغلاديش والتي أجريت في الأعوام 1993-94، 1996-97، 1999-2000، 2004، 2007. واستُعْرِضَت نتائج العينة بأكملها ثم النتائج الخاصة بأفقر شريحة خمسية وأغنى شريحة خمسية.
النتائج
لوحظت اتجاهات إيجابية في المناطق الحضرية، وحيث تتوفر الكهرباء، وحسب العمر عند أول زواج، واستخدام موانع الحمل الحديثة، والقدرة على الوصول إلى الرعاية الماهرة السابقة للولادة، وتطعيم الأطفال، والمعرفة بفيروس العوز المناعي البشري، ومتلازمة عوز المناعة البشرية المكتسبة، وزيادة الوزن والسمنة. وبالمقارنة لوحظت اتجاهات سلبية في عوامل مثل التعليم، ووفيات الرضع والأطفال، ومعدل الخصوبة، والولادة في المنزل، وسوء التغذية، ونقص الوزن. إلا أن التغيرات في هذه المؤشرات اختلفت بين أغنى شريحة خمسية وأفقر شريحة خمسية. فعلى سبيل المثال، شهدت الشريحة الأغنى فقط تمديناً سريعاً، في حين انخفض الجهل أكثر بين الفقراء. وجدير بالملاحظة، اكتشاف ثغرات في جميع تلك العوامل. فهناك ثغرات بين الأغنياء والفقراء في التمدين، وعمر الزواج، والخصوبة، واستخدام العازل الذكري، والولادة في المنزل، وزيادة فرط الوزن؛ وبالنقيض، هناك ثغرات في التعليم، والحصول على الماء والإصحاح، واستخدام موانع الحمل (ما عدا العازل الذكري)، وتدهور تطعيم الأطفال.
الاستنتاج
إن استمرار الإجحاف يهدد التنمية البشرية المستدامة في بنغلاديش. وينبغي تنفيذ استراتيجيات تنموية مناصرة للفقراء استناداً إلى مبادئ العدالة والجودة من أجل تقليل الثغرة القائمة، ولمزيد من تعزيز التنمية البشرية الشاملة والعادلة.
Resumen
Objetivo
Evaluar los niveles, las tendencias y las diferencias entre los más ricos y los más pobres en Bangladesh a través de determinados indicadores de desarrollo humanos y sanitarios.
Métodos
A partir de las Encuestas sobre Salud y Demografía realizadas en Bangladesh en los períodos de 1993–1994, 1996–1997, 1999–2000, 2004 y 2007 se extrajeron los datos para estos indicadores relacionados con las características sociodemográficas entre mujeres solteras, sobre el uso de métodos anticonceptivos, vacunación infantil, condiciones sanitarias y prácticas asistenciales prenatales. Los resultados se presentaron para la totalidad de la muestra y para los quintiles de los más ricos y los más pobres.
Resultados
Se observaron tendencias positivas en la urbanización, la disponibilidad de electricidad, la edad del primer matrimonio, el uso de métodos anticonceptivos modernos, el acceso a la asistencia prenatal profesional, la vacunación infantil, el sobrepeso, la obesidad y los conocimientos sobre la infección por el virus de la inmunodeficiencia humana (VIH) y el síndrome de la inmunodeficiencia adquirida. En contraposición, se registraron tendencias negativas en factores como la alfabetización, la mortalidad en bebés y niños, la tasa de fertilidad, el parto domiciliario y la malnutrición, así como el peso insuficiente. No obstante, se observaron diferencias notables en los cambios en estos indicadores entre los quintiles más pobres y los más ricos. Por ejemplo, sólo el quintil más rico experimentó una rápida urbanización, mientras que el analfabetismo descendió más entre los más pobres. En casi todos los factores se observaron diferencias significativas. Las diferencias entre ricos y pobres en cuanto a urbanización, edad al casarse, fertilidad, uso de preservativos, partos domiciliarios y sobrepeso aumentaron. Por el contrario, las diferencias en cuanto a educación, agua y saneamiento, uso de anticonceptivos (exceptuando preservativos) y vacunación infantil disminuyeron.
Conclusión
La persistencia de las desigualdades en Bangladesh pone en peligro el desarrollo humano igualitario y sostenible en este país. Deben ponerse en marcha estrategias de desarrollo a favor de los pobres basadas en los principios de calidad e igualdad, con el fin de reducir las diferencias existentes y promover un desarrollo humano integral e igualitario.
Résumé
Objectif
Evaluer les niveaux, les évolutions et les écarts entre les plus pauvres et les plus riches, pour des indicateurs sanitaires et de développement humain sélectionnés au Bangladesh.
Méthodes
Les données pour les indicateurs sélectionnés, associés aux caractéristiques sociodémographiques des femmes déjà au moins une fois mariées, l'utilisation de la contraception, la vaccination des enfants, les pratiques de soins prénatals et les conditions de santé ont été extraites des enquêtes démographiques et sanitaires bangladaises menées en 1993–94, 1996–1997, 1999–2000, 2004 et 2007. Les résultats de l'ensemble de l'échantillon et des quintiles les plus pauvres et les plus riches sont présentés.
Résultats
Des évolutions positives ont été observées en termes d'urbanisation, d’accès à l'électricité, d'âge lors du premier mariage, d'utilisation de la contraception moderne, d'accès à des soins prénatals qualifiés, de vaccination infantile, de connaissance de l'infection par le virus d'immunodéficience humaine (VIH), du syndrome d'immunodéficience acquise, ainsi que du surpoids et de l'obésité. En revanche, des évolutions négatives ont été observées en termes d'alphabétisation, de mortalité infantile et juvénile, de taux de fécondité, d'accouchement à domicile, de malnutrition et d'insuffisance pondérale. Cependant, l'évolution de ces indicateurs diffère entre les quintiles les plus riches et les plus pauvres. Par exemple, seul le quintile le plus riche a connu une urbanisation rapide, tandis que l'analphabétisme a diminué plus fortement parmi les plus pauvres. Des écarts notables ont été constatés dans presque tous les facteurs. Les écarts entre riches et pauvres en matière d'urbanisation, d'âge au mariage, de fécondité, d'utilisation du préservatif, d'accouchement à domicile et de surcharge pondérale ont augmenté; en revanche, les écarts en termes d'éducation, d'eau et d'assainissement, d'utilisation de la contraception (à l'exception des préservatifs) et de vaccination des enfants ont diminué.
Conclusion
Les inégalités persistantes au Bangladesh mettent en péril le développement humain équitable et durable du pays. Des stratégies de développement en faveur des pauvres, sur la base des principes d'équité et de qualité, devraient être mises en œuvre pour combler les lacunes existantes et promouvoir davantage le développement humain, holistique, et équitable.
Резюме
Цель
Оценить уровни, тенденции и разрыв между беднейшими и богатейшими слоями населения по некоторым показателям состояния здоровья и развития человеческого потенциала в Бангладеш.
Методы
Данные по некоторым показателям, отражающим социально-демографические характеристики женщин, когда-либо состоявших в браке, использование контрацептивов, уровень вакцинации детей, пользование дородовой медико-санитарной помощью, а также медицинские состояния, были взяты из обследований по проблемам демографии и здоровья, проведенных в Бангладеш в 1993–1994, 1996–1997, 1999–2000, 2004 и 2007 годах. Представлены результаты для всей выборки, а также для беднейшей и богатейшей квинтилей.
Результаты
Отмечены положительные тенденции в отношении показателей урбанизации; доступа к электроснабжению; возраста вступления в первый брак; использования современных средств контрацепции; доступа к квалифицированной дородовой помощи; вакцинации детей; знаний о вирусе иммунодефицита человека (ВИЧ) и синдроме приобретенного иммунодефицита (СПИД); избыточного веса и тучности. В противоположность этому, отрицательные тенденции наблюдались в отношении таких факторов, как грамотность, младенческая и детская смертность, уровень фертильности, роды, принятые в домашних условиях, недоедание и пониженная масса тела. Однако изменения по этим показателям были различны в беднейшей и богатейшей квинтилях. Например, стремительная урбанизация наблюдалась только в богатейшей квинтили, а снижение уровня грамотности – большей частью среди беднейшей. Бросающиеся в глаза разрывы были отмечены в отношении почти всех факторов. Разрыв между богатыми и бедными по уровню урбанизации, возрасту вступления в брак, уровню фертильности, использованию презервативов, доле родов, принятых в домашних условиях, и избыточному весу увеличился; в то же время разрыв по уровню образования, охвату системами водоснабжения и канализации, использованию средств контрацепции (кроме презервативов) и уровню вакцинации детей сократился.
Вывод
Сохраняющееся в Бангладеш неравенство представляет собой угрозу для справедливого и устойчивого развития человеческого потенциала в этой стране. Для сокращения существующих разрывов и дальнейшего содействия комплексному, социально-справедливому развитию человека необходимо внедрять стратегии развития в интересах бедных слоев населения, базирующиеся на принципах справедливости и качества.
摘要
目的
旨在评估孟加拉国最贫困人群和最富有人群之间在选定的健康和人类发展指标方面的水平、趋势和差异。
方法
已婚妇女中避孕措施运用、儿童预防接种、产前保健和健康状况等与社会人口特点相关指标的数据从1993-1994,1996-1997,1999-2000,2004和2007年进行的孟加拉国人口和健康调查中提取。基于提取的数据给出整个样本的以及最贫困和最富有人群财富五分位组的结果。
结果
在都市化、电力可用性、初婚年龄、现代避孕措施运用、获得熟练产前保健、儿童预防接种以及对艾滋病毒感染(HIV)、获得性免疫缺陷综合征、超重和肥胖的了解方面发现积极趋势。与此相反,在读写能力、婴幼儿死亡率、生育率、在家分娩、营养不良和重量不足等方面则发现消极趋势。然而,最贫困和最富有人群五分位组中该指标的变化并不相同。例如,仅最富有的五分位组经历了快速的都市化,而文盲比例主要在最贫困的人群中出现下降。几乎在所有的因素方面均能发现显著差距。贫富之间在都市化、初婚年龄、生育、安全
套使用、在家分娩和超重方面的差距增加;与此相反,贫富之间在教育、水和卫生、避孕措施运用(除安全套外)和儿童预防接种方面的差距减小。
结论
孟加拉国持续的不平等现象危及孟加拉国公平的可持续的人类发展。应该实施基于公平和质量原则的扶贫发展策略从而缩小现存差距并进一步促进整体的平等的人类发展。
Introduction
Bangladesh is one of the most densely populated and disaster-prone countries in the world. The country’s low-lying deltaic topography, frequent natural disasters and low financial and adaptive capacity undermine the national economy and greatly impact on human lives.1,2 In spite of this, Bangladesh has made impressive progress in health and human development since its emergence as an independent nation in 1971.3–5 Human rights are recognized as fundamental in the constitution and health and education are prioritized. Moreover, Bangladesh has ratified most international treaties and declarations, including the Alma-Ata Declaration, the International Conference on Population and Development and the United Nations’ Millennium Development Goals (MDGs).6 Health services have received special attention since the Alma-Ata conference in 1978.7
Over the last three decades Bangladesh has made strides in many areas. For example, mortality in children under 5 years of age has declined sharply – from 140 to 65 per 1000 live births between the 1970s and 2007 – and life expectancy at birth increased from 45 years in 1972 to 64 in 2007. The rate of absolute poverty has declined from 59% in 1991–92 to 40% in 2007.5 The maternal mortality ratio dropped from 724 per 100 000 live births in 1990 to 338 in 2008.8 Bangladesh has already achieved MDG 34 and is on track to achieving MDGs 1, 2 and 4 by 2015.4,5 Such developments have been achieved as a result of several key factors, including a strong commitment by the government to promote and protect civil and political rights; a growing network of health-care providers from the local to the national level;6 an increasing national effort to reduce gross inequities;3 the timely implementation of public health interventions; and rising and steady economic growth supported by good economic and social strategies.5 The human development index in Bangladesh has also improved substantially over the years. By 2003 Bangladesh had moved from a low- to a medium-level human development index country.9
Despite much progress, social inequalities persist. In Bangladesh wealth and power are highly concentrated and the poorer and more disadvantaged segments of the population reap few of the benefits of development, yet relevant public policies to redress the situation are rarely implemented. Poverty is higher in rural areas than in urban areas,5 the health system caters to the rich, urban elite4,6 and the poor have less access to health care than the rich.10 As in the rest of southern Asia, widespread gender discrimination contributes to disparities in health, sex-specific abortions, the neglect of female children and poor access to health care, especially for girls and women.11,12 Although absolute poverty has declined in all of southern Asia, including Bangladesh, the gap between the rich and poor within and between countries has widened in recent years.13,14 Consequently, significant inequity between the rich and poor remains in access to health-care services and their utilization.7,14–18 Although Bangladesh is likely to achieve several of the health-related MDGs at the national or aggregate level, the critical question is whether it can substantially narrow the internal gaps between the rich and poor.
Health inequities are ubiquitous;7,15,17 they exist in both developed and developing societies.17,18 Most development advocates, planners and practitioners view them as unacceptable, unfair7,11,19 and rooted in broader social injustice.15,20 Such inequities pose critical challenges across countries and cultures15 and are becoming an important social concern.7 Inequities and poverty systematically exacerbate the disadvantaged position of the poor with respect to health and health care utilization,19,20 undermine population health, and seriously hinder equitable, sustainable development.13,14 Therefore, reducing health inequities should be an integral part of the ongoing fight against poverty and ill health21 and a core goal of contemporary development paradigms.16 Unless the needs of the poorest segments of the population are effectively addressed, equity in health and overall socioeconomic development will be difficult to achieve.14
All of the above-mentioned points draw attention to the fact that in Bangladesh the overall development process has favoured the rich and powerful and has generated gross inequity across socioeconomic groups. The main objective of this study was to quantify existing inequity across a set of selected health and human development indicators. These pertain to socioeconomic and demographic characteristics, fertility control measures, antenatal care practices, childhood vaccination coverage, the prevalence of common childhood diseases, the prevalence of underweight and overweight and knowledge about acquired immunodeficiency syndrome (AIDS). The study focused on women of reproductive age belonging to the poorest and the richest population quintiles. The gap between these two wealth quintiles was calculated for each survey by subtracting the value of the poorest quintile from that of the richest quintile. Changes over time were also calculated by subtracting the value obtained from the first survey (depending on data availability) from the value obtained from the last survey (not shown). The focus was on women because multiple layers of gender-based discrimination and inequality have rendered them more vulnerable than men to poverty-linked health outcomes. Women are over-represented among the world’s poor and are grossly deprived of the benefits of economic, political and social gains.11,13 Unless development indicators are disaggregated by population subgroups and carefully analysed, improvements in national averages may conceal persisting or worsening inequalities within a society.16 This study is intended to help better understand and address the needs of the poorest groups and develop effective strategies to reduce existing gaps and accelerate progress towards greater equality and social justice in Bangladesh.
Methods
The study is based on five data sets of the Bangladesh Demographic and Health Surveys (DHS) carried out in 1993–94, 1996–97, 1999–2000, 2004 and 2007. These surveys were conducted by the National Institute of Population Research and Training with financial and technical support from the United States Agency for International Development (USAID). The study design, informed consent form and methods of data collection were described in detail in the country-specific reports.22 All DHS are nationally representative and apply a common methodology across countries.23 More than 170 countries routinely conduct such surveys under the DHS programme with financial and technical support from USAID.22 All the analyses were performed for women selected through multistage stratified cluster sampling. The sample sizes varied from 9127 in 1996–1997 to 11 440 in 2004. For the first three surveys, relevant data on women were merged with the file containing the DHS wealth index (WI) variable. Increases in the sample from urban areas (15.2% in 1993–1994 and 37.8% in 2007) have gradually improved the representativeness of the samples because Bangladesh has experienced rapid urbanization. Similarly, decreases in the sample from the poorest quintile along with increases in the sample from the highest quintile have improved representativeness because of the socioeconomic development that Bangladesh has experienced. We report the non-response rate for each survey only for the total sample considered eligible for interview.
The DHS WI is an asset-based index that reflects the relative socioeconomic status of the household19,23,24 and is widely used in low- and middle-income countries to quantify inequalities and to control the confounding effect of socioeconomic variables.23 Variables that have been used to calculate the WI included ownership of durable assets (e.g. car, refrigerator, television), housing characteristics (e.g. materials of the floor, roof, walls) and access to services (e.g. availability of electricity and drinking water source). This index is constructed using the principal component analysis procedure of the SPSS factor analysis (SPSS Inc., Chicago, United States of America).24–26 In this procedure, the indicator variables are first standardized, the factor loadings are then calculated and, finally, the indicator values are multiplied by the loadings and summed up to produce the household’s index value. Only the first factor (first principal component) is used to represent the WI.24,25
Selected factors
In this study we considered a group of indicators reflecting socioeconomic status (e.g. education, access to improved sanitation), demographic conditions (e.g. age at marriage, total number of children ever born) and fertility control behaviour (e.g. history and type of contraceptive use). Other selected factors pertain to the antenatal care received during the last childbirth (e.g. at least one antenatal care visit, delivery at home), vaccination coverage of the last child (e.g. measles vaccine, bacille Calmette-Guérin [BCG], first dose of diphtheria–pertussis–tetanus [DPT1] vaccine), important symptoms/diseases of the last child (e.g. diarrhoea, cough) and other health-related conditions of the women (e.g. underweight, overweight). Socioeconomic and demographic characteristics, fertility control behaviour and practices and some health-related conditions were based on the entire sample, whereas other variables were based on subsamples. Infant mortality and other information such as vaccination coverage, prevalence of tuberculosis, access to safe drinking water and improved sanitation facilities were obtained from published sources.22,27
Results
In this section we report on selected macro-level indicators obtained from national reports22 and official United Nations data27. The prevalence of underweight among children under 5 years of age declined from 67.4% in 1992 to 41% in 2007. The infant mortality rate declined by 40%: from 87 per l000 live births in 1989–93 to 52 in 2002–2006. Measles vaccination coverage among infants (i.e. children aged 12 months or less) increased from 55.0% in 1989–1993 to 77.2% in 2002–2006 – a rise of more than 40% within a decade. The proportion of births attended by skilled health personnel increased from 8% in 1996–97 to 18% in 2007. The prevalence of tuberculosis decreased from 638.6 per 100 000 population in 1990 to 386.8 in 2007. However, access to safe drinking water (adjusted for arsenic contamination) improved only marginally – from 78% in 1990 to 80% in 2006. On the other hand, the availability and use of improved sanitation facilities rose from 26% in 1990 to 36% in 2006. Most of these health- and development-related indicators are also used to assess progress towards attaining the MDGs endorsed by Bangladesh.
The following sections present all results based on an extensive analysis of relevant data extracted from the DHS surveys. Some figures illustrate the results very clearly. The findings suggest that some of the gains attained by Bangladesh in health and development over the past 30 years may be undermining other gains. For instance, rapid and unplanned urbanization leading to the growth of slums could endanger the progress attained in access to safe drinking water and sanitation facilities. Similarly, the low rate of condom use may lead to an increased prevalence of HIV/AIDS and other sexually-transmitted infections.
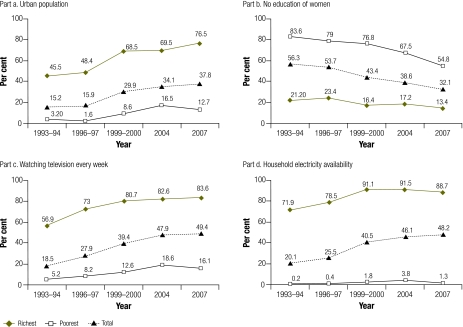
Socioeconomic factors
In the richest quintile, the percentage of women living in urban areas increased rapidly, from 45.5% in 1993–94 to 76.5% in 2007. In contrast, the poorest quintile experienced only sporadic urbanization. Moreover, the gap in urbanization between the poorest and richest quintiles also increased (Fig. 1, part a). Illiteracy rates declined among all women, but those in the poorest quintile experienced a more rapid decline than those in the richest quintile (Fig. 1, part b). Gaps in television watching increased slightly during 1996–2007 (Fig. 1, part c). The percentage of households with electricity also increased, but primarily in the richest quintile (Fig. 1, part d).
Fig. 1.
Socioeconomic indicators: levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
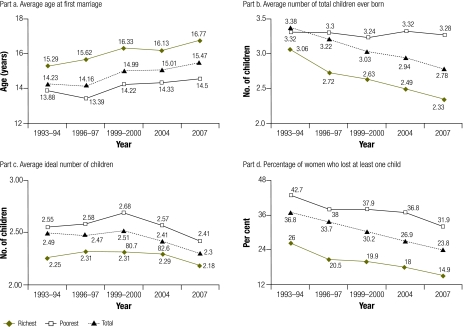
Demographic factors
Most of the demographic variables analysed showed improvement in both the poorest and the richest quintiles, although noteworthy gaps continue to exist. For some variables such as age at first marriage (Fig. 2, part a) and total number of children ever born (Fig. 2, part b), positive changes occurred at a faster pace in the richest quintile than in the poorest one. Very little change was observed in the poorest quintile in the total number of children ever born and the number of living children. Gaps widened in age at first marriage, age at first birth, total number of children ever born and number of living children. The gaps in other variables remained almost unchanged.
Fig. 2.
Demographic indicators: levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
Fertility-control practices
Some results related to fertility control practices are displayed in Fig. 3. The study found gradual improvement and narrowing gaps between the richest and the poorest women in the use of any contraceptive method ever (Fig. 3, part a) and in the use of a modern method at the time the survey was conducted (Fig. 3, part b). Condom use increased faster in the richest quintile than in the poorest one (not shown) and therefore the gap between the two groups gradually widened (Fig. 3, part c). An increasing gap was also seen in considering condoms the preferred future method of contraception (not shown). Among the modern contraceptive methods, the pill was found to be more popular than condoms or sterilization (not shown). However, women in the poorest quintile shifted to using the pill faster than women in the richest quintile (not shown). Although sterilization was more popular among the poorest women, its frequency among them seems to have decreased sharply in recent years (Fig. 3, part d).
Fig. 3.
Contraception-related indicators: levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
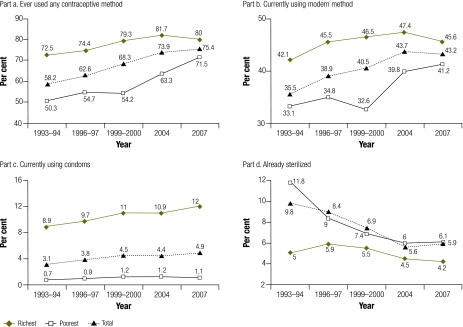
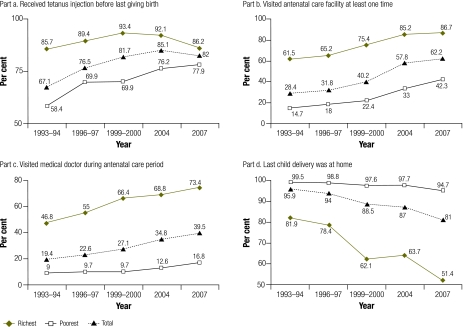
Antenatal-care practices
The gap between the richest and the poorest quintiles decreased for one of the six antenatal care indicators: receipt of tetanus immunization before the last birth (Fig. 4, part a). The gaps remained almost unchanged for having made at least one visit to antenatal care (Fig. 4, part b) but increased for three indicators: a visit to a physician (Fig. 4, part c), a visit to a nurse or midwife (not shown) and delivery at home (Fig. 4, part d). A visit to a family welfare visitor during the antenatal period showed an increase among the richest quintile but no discernible trend was seen among the poorest quintile (not shown). Gaps widened mainly because change occurred faster in the richest quintile than in the poorest quintile.
Fig. 4.
Antenatal care indicators (related to most recent birth): levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
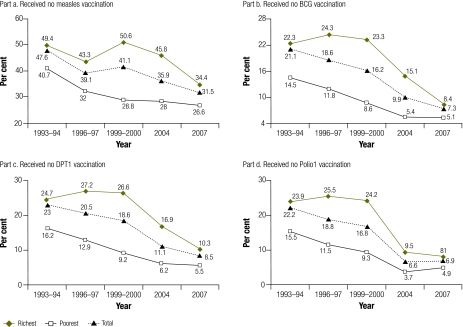
Child vaccination-related factors
Factors related to child vaccination (Fig. 5 part a, part b, part c and part d) registered a steady improvement. Although the poorest quintile had lower coverage than the richest, change occurred relatively faster in the poorest quintile, and the gaps gradually narrowed as a result. The sole exception was measles vaccination, since both the rich and poor seem to avoid immunizing their children against measles, perhaps because in Bangladesh the incidence of measles has declined over the last three decades. The complacency that has set in surrounding measles vaccination needs to be addressed by the health-care system.
Fig. 5.
Child vaccination indicators (for last child): levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
BCG, bacille Calmette-Guérin; DPT1, diphtheria-pertussis-tetanus first dose.
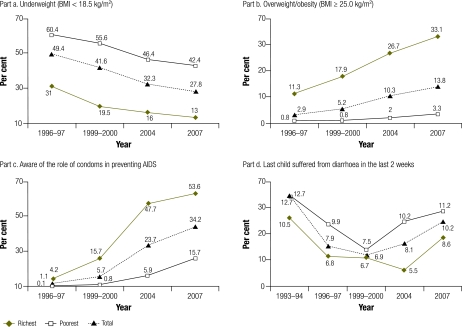
Other health-related factors
Other indicators are presented in Fig. 6. In both the richest and the poorest quintiles the prevalence of underweight, defined as a body mass index (BMI, or weight in kg divided by height in m2) < 18.5, decreased slowly, although the gap was still large and change took place a little faster in the poorest quintile (Fig. 6, part a). In contrast, the prevalence of overweight increased sharply in the richest quintile (Fig. 6, part b). Knowledge about AIDS prevention improved overall, but at a relatively faster rate in the richest quintile (Fig. 6, part c). The prevalence of children having common conditions such as diarrhoea (Fig. 6, part d) was notably higher in the poorest than in the richest quintile. Increasing gaps were observed for factors such as overweight and knowledge of the role of condoms in preventing HIV infection.
Fig. 6.
Other health-related indicators: levels, trends and gaps between ever-married women in the poorest and richest quintiles, Bangladesh, 1993–2007
AIDS, acquired immunodeficiency syndrome; BMI, body mass index.
Discussion
The study demonstrated huge disparities between the poorest and the richest quintiles. Other studies have also reported huge socioeconomic and health-related disparities in developing countries.17–19,28 Of 49 factors considered, 16 show increasing inequity, whereas 22 show a decrease in the rich-poor gap. Inequity has remained almost unchanged over the years in 11 areas. Inequity has declined in areas such as literacy among women and their partners, improved sanitation, current use of modern contraceptive methods and child vaccination. The decrease in inequity may reflect the fact that change occurred faster in the poorest than in the richest quintile, given that the poor had much lower levels of sanitation, electricity, antenatal care and vaccination coverage and much higher rates of illiteracy. Increasing gaps were identified in areas such as urbanization, access to television and electricity, respondents’ age at first birth and subsequent fertility-related behaviour, access to skilled antenatal care, condom use, overweight and knowledge of the role of condoms in preventing HIV infection. According to the present study, progress in these areas occurred much more slowly in the poorest than in the richest quintile, and the poor are at a greater disadvantage than the rest of the population. Some of our findings are also in line with those of other studies.29,30 Although one usually expects everyone in the richest population quintile to live in a house with electricity, this is not the case in Bangladesh because not all regions of the country have electricity infrastructure, especially in rural areas.
Reducing poverty and health inequalities is crucial for overall sustainable socioeconomic development.31,32 Several actions or interventions have been proposed to minimize the gaps between the rich and poor.6,18,31 Policy-makers and planners must implement measures to provide everyone with equal access to health-care facilities and other ancillary services.6 Three broad strategic approaches built on the principles of equity and quality could minimize and gradually eliminate health gaps between the poor and rich: (i) focusing on the most disadvantaged groups through specific interventions; (ii) setting realistic targets to improve the health of the poorest groups; and (iii) forcefully addressing the social determinants of health inequities. Concerted efforts are needed to give voice to the voiceless. Public health services should be made accessible to all people in accordance with their needs and must not be influenced by their ability to pay or by profit-seeking. High-quality public health services must be available and accessible to all people, irrespective of their socioeconomic status.31
According to a World Bank report, Bangladesh could make greater progress and achieve more sustainable and equitable development if it: (i) improved accountability and the transparency of public services, (ii) removed key barriers to sustainable growth (e.g. institutional inadequacy, lack of urban governance, lack of tenurial rights of slum dwellers, deteriorating environmental conditions in urban slums, limited access to safe drinking water and good sanitation), and (iii) built on and strengthened its already successful urban programmes (e.g. female secondary scholarship). At the same time, public–private partnerships should be fostered and expanded.5 Recipient and donor governments should take an integrated approach to the entire health system and prioritize primary health care and the strengthening of the system’s institutional and technical capacity.32 National health policy must also focus on developing and strengthening the health system. Strategies to effectively address the barriers to achieving and sustaining equity within and outside the health system should be implemented. Policy-makers, planners, service providers and health service managers should be made more aware of the magnitude of existing inequities, the trends currently observed and the most affected subgroups.18 Moreover, development and private sector partners should explore every opportunity to make legislation flexible enough to allow greater access to low-cost medicines and other treatments in developing countries.32
Policy implications
Despite progress over the years, gross inequities in health and socioeconomic development continue to persist. Bridging the gaps between the rich and poor must consequently be the central goal of all development strategies. As our findings show, to minimize these gaps health programmes and interventions will need to focus on the poorest and most vulnerable subpopulations. These are so often marginalized and socially excluded from health, welfare and environmental protection.21 Programme statistics based on national averages are misleading because they often conceal gross inequities within and between different segments of the population and between regions and districts. Since population averages do not capture social disparities, they often result in an under- or an overestimation of certain health outcomes in some groups (e.g. among the poorest segments, communicable disease outcomes are often overestimated, whereas non-communicable disease outcomes are underestimated). Our findings also illustrate the complexities of designing and effectively implementing interventions to tackle inequity. Policies and programmes implemented to improve the socioeconomic conditions of poor and marginalized populations will reduce their burden of communicable diseases, but their burden of non-communicable diseases will probably continue to increase as a result of the demographic and epidemiological transitions.29
Strengths and limitations of the study
One strength of the study is the in-depth analysis of data from large and representative data sets covering a long period. Another strength is the use of many development indicators to illustrate long-term trends and critically examine socioeconomic and health-related inequities between the rich and poor in a developing country.
Among the study’s most important limitations is the use of the wealth index,24–26 which does not take into account household size or composition or fluctuations in the price of assets. Its appropriateness varies depending on the population subgroup (e.g. rural versus urban) and on geographical region.25 It only reflects long-term household wealth and fails to include short-run financial shocks or interruptions. Despite these limitations, the wealth index is a useful and pragmatic tool that can help overcome research survey weaknesses such as recall bias and seasonality.26
Conclusion
Many of the indicators used in this study to reflect sustainable and equitable health and development show marked differences between Bangladeshi women belonging to the poorest and the richest quintiles. Policy-makers and planners must therefore use segregated data to formulate better policies and programmes for promoting and protecting equitable health and development. To reduce disparities between the rich and poor, efforts should focus on promoting equitable access to health and to the benefits of social development. Progress towards achieving national and international health goals will only be accelerated by mainstreaming equity in health policies and programmes.18 In short, Bangladesh needs concerted, integrated and holistic efforts based on the fundamental principle of equity to bridge the gaps between the rich and the poor and usher in an era of more progressive, equitable and sustainable socioeconomic development.
Acknowledgements
We thank Erich Wehmeyer for his help with improving the English in the manuscript.
Competing interests:
None declared.
References
- 1.Streatfield PK, Karar ZA. Population challenges for Bangladesh in the coming decades. J Health Popul Nutr. 2008;26:261–72. [PMC free article] [PubMed] [Google Scholar]
- 2.Shahid S. Probable impacts of climate change on public health in Bangladesh. Asia Pac J Public Health. 2010;22:310–9. doi: 10.1177/1010539509335499. [DOI] [PubMed] [Google Scholar]
- 3.Chowdhury AMR. Rethinking interventions for women’s health. Lancet. 2007;370:1292–3. doi: 10.1016/S0140-6736(07)61554-2. [DOI] [PubMed] [Google Scholar]
- 4.Government of the People’s Republic of Bangladesh. Millennium Development Goals: mid-term Bangladesh progress report Dhaka: Planning Commission; 2007. Available from: http://www.undp.org.bd/mdgs/MDG_Mid-term_Progress_Report2007.pdf [accessed 15 April 2011].
- 5.To the MDGs and beyond: accountability and institutional innovation in Bangladesh (Bangladesh Development Series Paper No. 14). Dhaka: The World Bank; 2007. Available from: http://siteresources.worldbank.org/BANGLADESHEXTN/Resources/295759-1171499457708/complete.pdf [accessed 17 May 2011].
- 6.Rahman RM. Human rights, health and the state in Bangladesh. BMC Int Health Hum Rights. 2006;6:4. doi: 10.1186/1472-698X-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Razzaque A, Streatfield PK, Gwatkin DR. Does health intervention improve socioeconomic inequalities of neonatal, infant and child mortality? Evidence from Matlab, Bangladesh. Int J Equity Health. 2007;6:4. doi: 10.1186/1475-9276-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 9.Human development reports [Internet]. New York: United Nations Development Programme, Human Development Report Office; 2010. Available from: http://hdr.undp.org/en/reports/global/hdr2010/ [accessed 15 May 2011].
- 10.Chowdhury ME, Ronsmans C, Killewo J, Anwar I, Gausia K, Das-Gupta S, et al. Equity in use of home-based or facility-based skilled obstetric care in rural Bangladesh: an observational study. Lancet. 2006;367:327–32. doi: 10.1016/S0140-6736(06)68070-7. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed SM, Adams AM, Chowdhury M, Bhuiya A. Gender, socioeconomic development and health-seeking behaviour in Bangladesh. Soc Sci Med. 2000;51:361–71. doi: 10.1016/S0277-9536(99)00461-X. [DOI] [PubMed] [Google Scholar]
- 12.Fikree FF, Pasha O. Role of gender in health disparity: the South Asian context. BMJ. 2004;328:823–6. doi: 10.1136/bmj.328.7443.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sicchia SR, Maclean H. Globalization, poverty and women’s health: mapping the connections. Can J Public Health. 2006;97:69–71. doi: 10.1007/BF03405219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karim F, Tripura A, Gani MS, Chowdhury AMR. Poverty status and health equity: evidence from rural Bangladesh. Public Health. 2006;120:193–205. doi: 10.1016/j.puhe.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 16.Bhuiya A, Hanifi SMA, Urni F, Mahmood SS. Three methods to monitor utilization of healthcare services by the poor. Int J Equity Health. 2009;8:29. doi: 10.1186/1475-9276-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Victora CG, Matijasevich A, Silveira MF, Santos IS, Barros AJD, Barros FC. Socio-economic and ethnic group inequities in antenatal care quality in the public and private sector in Brazil. Health Policy Plan. 2010;25:253–61. doi: 10.1093/heapol/czp065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG, Countdown 2008 Equity Analysis Group Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 Countdown countries. Lancet. 2008;371:1259–67. doi: 10.1016/S0140-6736(08)60560-7. [DOI] [PubMed] [Google Scholar]
- 19.Janković J, Simić S, Marinković J. Inequalities that hurt: demographic, socio-economic and health status inequalities in the utilization of health services in Serbia. Eur J Public Health. 2010;20:389–96. doi: 10.1093/eurpub/ckp189. [DOI] [PubMed] [Google Scholar]
- 20.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 21.Jancloes M. The poorest first: WHO’s activities to help the people in greatest need. World Health Forum. 1998;19:182–7. [PubMed] [Google Scholar]
- 22.Demographic and Health Surveys [Internet]. Calverton: Macro International. Available from: http://www.measuredhs.com/ [accessed 17 May 2011].
- 23.Howe LD, Hargreaves JR, Gabrysch S, Huttly SRA. Is the wealth index a proxy for consumption expenditure? A systematic review. J Epidemiol Community Health. 2009;63:871–7. doi: 10.1136/jech.2009.088021. [DOI] [PubMed] [Google Scholar]
- 24.Rutstein SO, Johnson K. The DHS wealth index (DHS Comparative Reports No. 6). Calverton: ORC Macro; 2004. Available from: http://www.childinfo.org/files/DHS_Wealth_Index_(DHS_Comparative_Reports).pdf [accessed 15 May 2011].
- 25.Howe LD, Hargreaves JR, Huttly SRA. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerg Themes Epidemiol. 2008;5:3. doi: 10.1186/1742-7622-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 27.Millennium Development Goals indicators. Bangladesh [Internet]. New York: United Nations Statistics Division. Available from: http://mdgs.un.org/unsd/mdg/Data.aspx [accessed 15 May 2011].
- 28.Mohanty SK, Pathak PK. Rich-poor gap in utilization of reproductive and child health services in India, 1992–2005. J Biosoc Sci. 2009;41:381–98. doi: 10.1017/S002193200800309X. [DOI] [PubMed] [Google Scholar]
- 29.Gwatkin DR, Guillot M. The burden of disease among the global poor: current situation, future trends, and implications for strategy Washington: The World Bank; 2000. Available from: http://www.dhsantementale.net/cd/biblio/pdf/SM-DH_124.pdf [accessed 15 May 2011].
- 30.Gwatkin DR. How much would poor people gain from faster progress towards the Millennium Development Goals for health? Lancet. 2005;365:813–7. doi: 10.1016/S0140-6736(05)17992-6. [DOI] [PubMed] [Google Scholar]
- 31.Farrell C, McAvoy H, Wilde J; Combat Poverty Agency. Tackling health inequalities - an all-Ireland approach to social determinants Dublin: Combat Poverty Agency; 2008. Available from: http://www.publichealth.ie/files/file/Tackling%20health%20inequalities.pdf [accessed 15 May 2011]. [Google Scholar]
- 32.Implementing the Millennium Development Goals: health inequality and the role of global health partnerships New York: United Nations; 2009. Available from: http://www.unicef.org/health/files/MDG_and_Health_Inequalities_UN_2009.pdf [accessed 15 May 2011].