Abstract
Background
Biomechanical research directed at developing customized implant solutions for rib fracture fixation is essential to reduce the complexity and to increase the reliability of rib osteosynthesis. Without a simple and reliable implant solution, surgical stabilization of rib fractures will remain underutilized despite proven benefits for select indications. This article summarizes the research, development, and testing of a specialized and comprehensive implant solution for rib fracture fixation.
Methods
An implant system for rib fracture fixation was developed in three phases: first, research on rib biomechanics was conducted to better define the form and function of ribs. Second, research results were implemented to derive an implant system comprising anatomical plates and intramedullary rib splints. Third, the functionality of anatomic plates and rib splints was evaluated in a series of biomechanical tests.
Results
Geometric analysis of the rib surface yielded a set of anatomical rib plates that traced the rib surface over a distance of 13–15 cm without the need for plate contouring. Structurally, the flexible design of anatomic plates did not increase the native stiffness of ribs while restoring 77% of the native rib strength. Intramedullary rib splints with a rectangular cross-section provided 48% stronger fracture fixation than traditional intramedullary fixation with Kirschner wires.
Conclusion
The anatomic plate set can simplify rib fracture fixation by minimizing the need for plate contouring. Intramedullary fixation with rib splints provides a less-invasive fixation alternative for posterior rib fracture, where access for plating is limited. The combination of anatomic plates and intramedullary splints provides a comprehensive system to manage the wide range of fractures encountered in flail chest injuries.
Keywords: Anatomic plates, Intramedullary splints, Rib fracture, Flail chest
Introduction
Surgical stabilization of rib fractures has been successfully performed for pain management of multiple rib fractures [1], fixation of chronically painful nonunions [2], reduction of overriding ribs [3], and for stabilization of flail chest injuries [4, 5]. Particularly in the case of fail chest stabilization, surgical fixation is of great value, as it can reduce ventilator time [4, 5], pneumonia [4, 5], mortality [4], and medical costs [5] while greatly improving functional outcomes and quality of life compared to nonoperative management [5]. Despite these clinical benefits and over 40 years of clinical experience, rib fracture fixation remains an underutilized procedure [3]. In a 2009 survey, 77% of surgeons supported the need for rib fracture fixation for select indications, but only 26% of surgeons had conducted or assisted in rib fracture fixation [6]. The survey attributed this stark discrepancy in part to the lack of research on optimal fixation techniques.
While a variety of implants for rib fracture fixation have been introduced, biomechanical studies that evaluate and optimize their function are rare at best. In the absence of a validated implant solution, rib fixation remains unnecessarily complex and exhibits persistent complications and limitations. Rib plating with standard plates requires time-consuming and difficult plate contouring [7]. The high stiffness of standard plates has been linked to screw pull-out and persistent discomfort [8–10], requiring hardware removal in 5–15% of patients [10–12]. Furthermore, plating is not well suited for the fixation of posterior fractures, where access is limited [7]. Intramedullary fixation with Kirschner wires has been used for over 40 years and allows the stabilization of posterior fractures in a less invasive manner. However, due to their small circular cross-section, Kirschner wires remain prone to wire migration and cut-out [13–17].
In order to address these complications and limitations, we conducted a series of biomechanical studies to systematically develop an advanced solution for rib fracture fixation, guided by a comprehensive review of the literature that describes the clinical experience on rib fracture fixation over the past 40 years. This review identified essential aspects of rib fracture fixation with plates and intramedullary devices: an advanced plating solution should provide a low-profile fixation construct [7], reduce the need for intraoperative plate contouring [3], allow for spanning and suspension of a flail segment with long plates [18, 19], match the low stiffness of ribs to restore physiologic rib function [9, 20], and it should deliver durable and strong fixation. A comprehensive strategy for rib fracture fixation should furthermore include an IM fixation option for stabilization of posterior fractures that prevents the implant migration and cut-out observed with Kirschner wires.
These design aspects were subsequently integrated into a novel implant system that combines an advanced plating option with an intramedullary (IM) fixation option to deliver a comprehensive solution suitable for the stabilization of simple rib fractures as well as complex flail chest injuries. This manuscript summarizes research pertaining to the three principal phases in the evolution of this novel implant system: (1) basic research on rib biomechanics pertinent to implant design [21]; (2) extrapolation of basic research results into advanced plating and IM solutions; and (3) biomechanical evaluation of advanced plating and IM solutions [22–24]. The results of this research provide surgeons with scientific evidence on the function, features, and performance of this novel implant system for rib fracture fixation.
Research on rib biomechanics
Design goals for an advanced implant solution were extracted by reviewing over 80 case reports and clinical studies on rib fracture fixation. For plate fixation, the design goal was anatomically shaped plates that match the stiffness of the native rib. Such anatomical plates would support low profile fixation, minimize the need for intraoperative plate contouring, and facilitate the spanning of flail segments with long plates. Plates that match the stiffness of native ribs would furthermore restore physiologic function to decrease the incidence of chest tightness and fixation failure associated with overly stiff plates [7, 9]. For IM fixation, the design goal was an anatomically curved IM device with design features that provide rotational stability and that prevent implant migration or cut-out. In order to meet these design goals, three basic research studies were conducted, characterizing: (1) the rib surface geometry required for an anatomical plate design; (2) the rib cross-sectional geometry required for an IM implant design; and (3) the structural properties of native ribs, which are required to design durable implants that support normal rib function.
Rib surface geometry
The rib surface is twisted and conical, which causes standard plates to diverge from the rib upon bending to the overall rib curvature [21]. To derive an anatomic plate design, the surface geometry of ribs was characterized by three principal parameters: the general rib curvature C G, the unrolled curvature C U, and the longitudinal twist αLT along ribs. To assess these three parameters, the outer surface of ribs 3–9 of eight human cadavers was digitized in 2 mm increments. The general curvature C G of the ribs was calculated from digitized point-triplets for locations ranging from 15 to 85% of the rib length (0% = tubercle, 100% = costochondral junction). The unrolled curvature C U describes the in-plane curvature that a plate must have in order to trace the conical surface of a rib upon bending to its apparent curvature. C U was determined by outlining the rib contour on a template conformed to the rib’s outer surface. Subsequently, this template was unrolled on a flat surface and the curvature C U of the centerline from 15 to 85% of rib length was measured. The longitudinal twist αLT of the rib surface is a geometric feature common to all ribs, whereby the right and left ribs are twisted in opposite directions. This twist αLT was quantified from 15 to 85% of the rib length.
Results of the surface geometry analysis yielded three parameters essential for the anatomic contouring of plates to the rib surface (Fig. 1). The general curvature results described differences in curvature between ribs as well as changes in curvature along ribs, with C G ranging from 3.8 ± 1.5 m−1 at the lateral aspect of rib 7 to 17.3 ± 1.7 m−1 at the anterior portion of rib 3. The unrolled curvature C U decreased gradually from ribs 3–5, and increased gradually with reverse orientation from ribs 6–9, ranging from 1.1 ± 0.8 m−1 in rib 6 to 6.9 ± 0.7 m−1 in rib 3. The longitudinal twist αLT was notably consistent between ribs, ranging from 41° to 45° in ribs 3–7, and from 58° to 60° in ribs 8 and 9. No statistically significant difference in twist between ribs was found (P > 0.05).
Fig. 1.
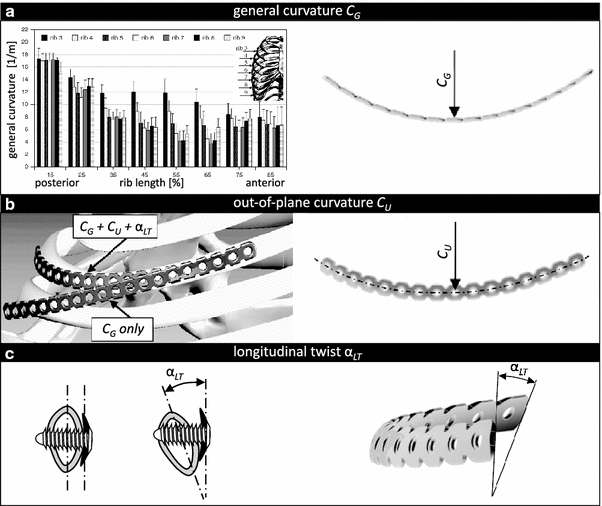
Three principal geometric parameters of ribs required for plate contouring: a the general curvature C G required for out-of-plane plate bending; b the unrolled curvature C U required for in-plane plate bending enables plates to trace the conical rib surface; and c the longitudinal twist αLT is required to ensure that the plate remains parallel to the rib surface
In summary, these results delineated the complex rib surface geometry into three basic parameters for the contouring of rib plates. A systematic approach for contouring a straight plate to the rib requires sequential application of in-plane bending C U, longitudinal twist αLT, and out-of-plane bending C G. Alternatively, these parameters can readily be implemented into an anatomic rib plate design to reduce the time and complexity of intraoperative plate contouring.
Rib cross-section geometry
In a second biomechanical study, the IM canal or ribs was characterized to support the development of an IM implant solution that resists migration and cut-out. The cross-sectional geometry of ribs 3–9 was examined in five fresh frozen human cadavers. Cross-sections of 2 mm thickness were excised at 5, 25, 50, and 75% of rib length, with the 5% cross-section being located posteriorly between the tubercle and angle. Contact radiographs of cross-sectional specimens were analyzed to extract the rib height (h) and width (w), the cortex thickness (t c) at the superior, inferior, inner and outer aspects, and the cross-sectional area of the medullary canal (A M).
The results of this study described for the first time differences in IM canal size and shape between ribs and along ribs (Fig. 2a). The cross-sectional area of the ribs was nearly constant along the ribs. However, the size of the intramedullary canal increased by 38% from posterior to anterior. The results furthermore described the cortex thickness, which was 37.5% greater at the inner cortex (1.1 ± 0.5 mm) than at the outer cortex (0.8 ± 0.4 mm, P < 0.01). In combination, these results provide guidance for the design and scaling of intramedullary implants for rib fracture fixation.
Fig. 2.
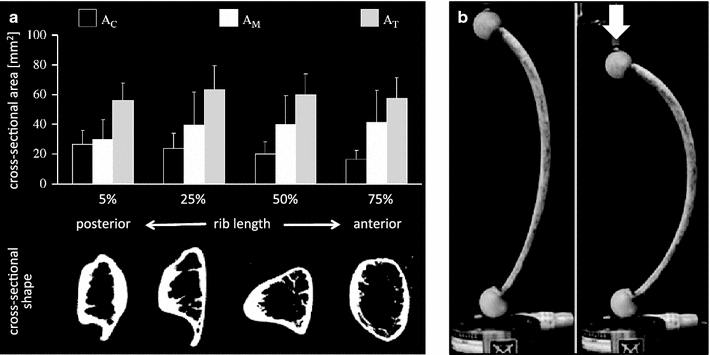
a Changes in cross-sectional area and shape of the intramedullary canal along the rib diaphysis; b ribs have a unique ability to tolerate large amounts of flexion. The same rib is shown unloaded and axially loaded
Structural properties of ribs
In a third biomechanical study, the stiffness and strength of native ribs was determined. Characterizing the structural function of the intact rib is crucial to designing implants of the appropriate stiffness, since stiffer implants may not provide better fixation. Particularly for rib fracture fixation, the use of overly stiff implants has been linked to screw pull-out, fixation failure, persistent discomfort and chest tightness [7, 9, 25, 26].
The stiffnesses and strengths of 20 human ribs 4–9 were assessed. To replicate quasi-physiological loading in a material test system, polymer spheres of diameter 25 mm were applied to both ends of each rib specimen, simulating anatomic constraints at the costrovertebral and sternocostal articulations. The actuator of the test system applied axial loads that induced two-point bending of the rib, representative of the principal loading mode in vivo [27–29].
The average stiffness of ribs was 10.2 ± 6.2 N/mm, and varied by over one order in magnitude, ranging from 1.5 to 20.1 N/mm. The ribs tolerated a large amount of flexion before fracturing (Fig. 2b), and fractured at a bending moment of 3.0 ± 1.8 N m (range 0.6–6.4 N m). The low stiffness of ribs, combined with their unique ability to undergo large amounts of flexion, emphasizes the need for an implant design that supports the physiological flexion of ribs and prevents the fixation failure seen with implants that are considerably stiffer than ribs.
Implant design
The results of the biomechanical analysis of ribs were used to derive an implant system for rib fracture fixation comprising anatomical plates and intramedullary implants (Fig. 3). The flexibility provided by combining a plating and IM solution was deemed essential to accommodate the range of fracture patterns and fracture locations encountered in flail chest injuries.
Fig. 3.
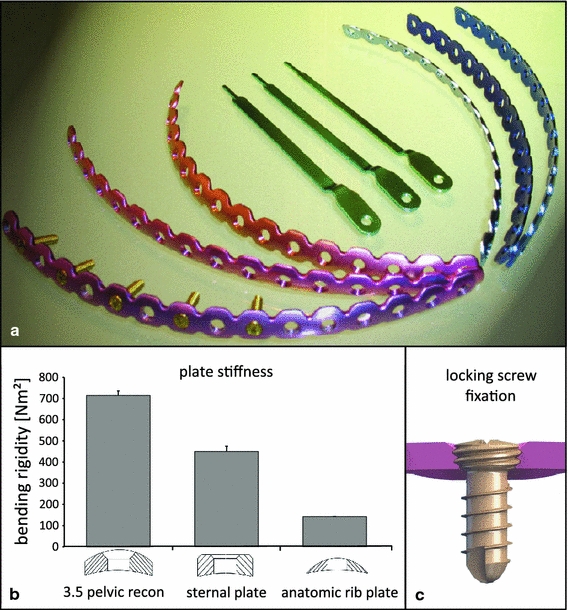
a Implant system for rib fracture fixation comprising a set of three left and three right anatomical plates and intramedullary rib splints in three sizes; b anatomic rib plates are over three times less stiff than titanium sternal locking plates (Synthes CMF), and over five times less stiff than stainless steel 3.5 mm reconstruction plates; c locking screws have a threaded head that engages in threaded plate holes to improve fixation strength
Anatomical plating solution
Based on the results of the rib surface analysis, an anatomic plate set was derived that accounts for the three principal parameters defining the rib surface: the general curvature, the in-plane curvature, and the twist. An analysis of these parameters revealed similarities between ribs that were exploited to reduce their complex surface geometry into a set of six anatomic plates that would accommodate the plating of right and left ribs 3–9. The six plates varied in in-plane curvature and twist while having the same general curvature. The plate set was manufactured with a general curvature of 5.1 m−1. This general curvature can be readily increased by out-of-plane bending the flexible plates to accommodate the increased curvature of posterior rib segments. To account for the conical rib surface, the anatomic plate set comprised plates with varying in-plane curvatures of up to 5 m−1. To accommodate for the longitudinal twist of the rib surface, the three left plates of the plate set were designed with a clockwise twist of 1.5°/cm, and the right plates were designed with a counterclockwise twist of the same magnitude.
In order to reproduce the flexibility of native ribs, low-profile plates were designed from elastic titanium. This plate design aimed to match the stiffness of osteoporotic ribs rather than strong ribs. Plate fixation in osteoporotic bone poses the greatest challenge, whereby overly stiff plates cause increased stress at the screw–bone interface and subsequent fixation failure by screw pull-out. Bending tests of prototype rib plates demonstrated that they were over three times less stiff than titanium sternal locking plates (Synthes CMF), and over five times less stiff than stainless steel 3.5 mm reconstruction plates (Fig. 3b). For durable fixation in osteoporotic bone, the plates were designed with threaded screw holes that accommodate locking screws with threaded screw heads (Fig. 3c). Upon insertion into the rib, these locking screws securely engage into the threaded plate holes and resist pull-out.
Intramedullary splint solution
Based on the results of the rib cross-sectional analysis, rib splints for intramedullary fixation of rib fractures were developed (Fig. 4a). The final rib splint design has a thickness of 1 mm and a rectangular cross-section to provide rotational stability and increased cut-out resistance. The rib splint is designed in widths of 3, 4, and 5 mm to accommodate the size range of the IM canal obtained in the cross-sectional rib analysis. The rib splint has a 75 mm long intramedullary segment to stabilize a single fracture. The intramedullary segment has an out-of-plane curvature of 200 mm to minimize residual stress after implant insertion. The splint front section is tapered to reduce the insertion force (Fig. 4b). The splint tip is sloped to guide the splint along the medullary canal without penetrating the lateral cortex (Fig. 4c). Rib splints have a small extramedullary segment that aids insertion and allows fixation with a single locking screw to prevent implant migration (Fig. 4d). Splints are designed for insertion through a lateral entry portal, applied at a distance of 30 mm from the fracture. A custom insertion tool was developed that rigidly connects to the extramedullary splint segment, allowing for the controlled insertion of the rib splint by tapping onto the insertion tool with a mallet (Fig. 4e).
Fig. 4.
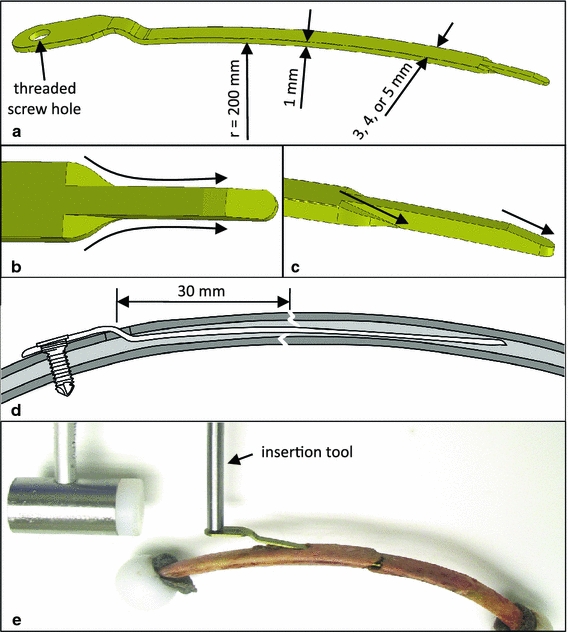
a The rib splints have an intramedullary shaft with a rectangular cross-section to provide rotational stability and cut-out resistance, while maintaining flexible fixation; b, c the tapered and sloped splint tip facilitates insertion and guides the splint along the intramedullary canal; d the rib splints are inserted through an entry portal at a distance of 30 mm from the fracture, and are secured with a locking screw to prevent splint migration; e the splints are inserted with a custom tool that can be rigidly connected to the splint
Implant evaluation
Prototypes of the implant system were manufactured and biomechanically tested in human cadaveric ribs. Anatomic plates were evaluated in regard to their fit to the rib, and the stiffness, durability and strength of the plate fixation constructs were assessed [23]. IM splints were evaluated in direct comparison to the traditional approach of IM fixation with Kirschner wires.
Evaluation of anatomic plates
First, the longitudinal fit of the anatomic plate set was assessed in 109 human ribs by measuring the plate length l P over which plates traced the rib surface in the absence of manual plate contouring (Fig. 5a). To assess the benefits of anatomic plates over standard plates, the same measurement was obtained for standard plates that were bent to the general curvature of the ribs but that had no in-plane curvature or twist. The results demonstrated that the anatomic plates could trace the surface of ribs 3–9 over a plating length l P ranging from 12.5 to 14.7 cm without the need for contouring. Compared to standard plates, the anatomic plates significantly increased the plating length l P by 79% for rib 3, by 67% for rib 4, and by 65% for rib 9.
Fig. 5.
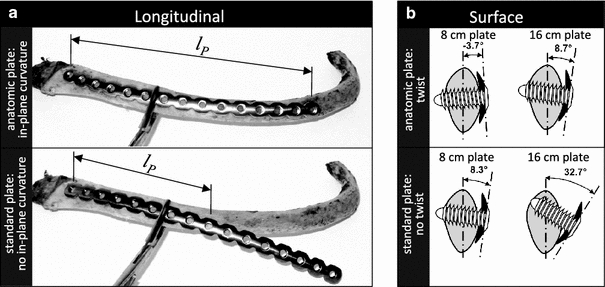
a Anatomic plates with in-plane curvature can trace the conical rib surface over a longer plate distance l P than plates without in-plane curvature, which thus tend to diverge from the rib surface; b the improved congruency provided by the anatomic plate twist compared with a standard plate without twist is depicted to scale for 8 and 16 cm long plates
In addition to the longitudinal fit, the surface fit of the anatomic plates was assessed. The congruency between the rib surface and the plate surface was measured by comparing the anatomic twists of 8 and 16 cm long rib segments with the twists of 8 and 16 cm long sections of the anatomic plates. An 8 cm long plate is suitable for spanning a single fracture, while the 16 cm plate is suitable for spanning multiple fractures of a flail segment. This analysis demonstrated that the surface of ribs 3–9 twisted on average by 8 ± 13° over an 8 cm segment, and by 33 ± 11° over a 16 cm segment. The anatomic plates approximated the twist of the rib surface within 3.7° on average for an 8 cm long plate, and within 8.7° on average for a 16 cm long plate (Fig. 5b).
These findings demonstrate that a small set of anatomic rib plates can minimize the need for intraoperative plate contouring by providing an increased plating length l P over which plates trace the rib surface, and by approximating the twist of the rib surface. Anatomic rib plates can therefore reduce the time and complexity of rib fracture fixation, and facilitate the spanning of flail segments with long plates. Furthermore, the inherent congruency between anatomic plates and ribs is essential to achieving low-profile fixation constructs and will contribute to durable fixation with screws that can reliably be inserted along the rib midline.
The mechanical function of anatomic plate constructs was characterized by assessing construct stiffness, durability, strength, and failure modes in 20 human cadaveric ribs (donor age: 69 ± 19 years). Rib segments were prepared for loading in the form of the two-point bending representative of the principal physiological loading mode, as previously described for stiffness assessment in native ribs (Fig. 6). Specimens were subjected to a sequence of four tests to determine the strength of intact ribs, the stiffness of plate constructs, the durability of plate constructs under exaggerated dynamic loading, and the residual strength and failure mode of constructs after dynamic loading. First, the ribs were loaded to failure to determine the strength of the intact ribs and to induce a clinically realistic fracture pattern. Second, fractures were stabilized with 7-hole anatomic plates, using three bicortical locking screws on each side of the fracture while retaining one empty screw hole over the fracture. The stiffness of plate constructs was assessed equivalent to the stiffness assessment of native ribs. Third, the plate constructs were dynamically loaded for 360,000 cycles to simulate a respiratory loading history until fracture stabilization by callus formation can be expected [26, 30]. Dynamic loading was applied with an exaggerated respiratory loading magnitude of 200 N mm, representing five times the bending moment measured in vivo on human ribs during physiologic respiration [26, 28]. Fourth, rib fixation constructs were quasi-statically loaded to failure to determine their residual strength and to analyze the failure mode.
Fig. 6.
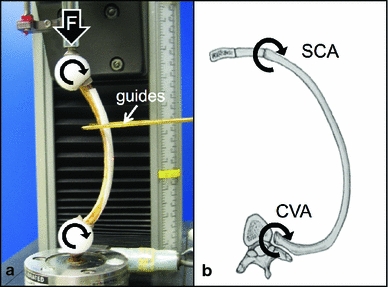
a Test setup used to evaluate the stiffness, durability and strength of fixation constructs under axial loading controlled by a material test system; b polymer spheres simulate physiologic constraints at the costrovertebral and sternocostal articulations
The results demonstrated that the stiffness of the plate constructs (7 ± 4 N/mm) remained on average below the stiffness of native ribs (10 ± 6 N/mm). The finding that the plates did not increase the stiffness of the ribs held true for the weakest rib tested (1.5 N/mm rib stiffness, 1.3 N/mm construct stiffness) as well as for the strongest rib tested (20 N/mm rib stiffness, 11 N/mm construct stiffness). All plating constructs survived exaggerated dynamic loading without encountering screw loosening or fixation failure. Subsequent loading to failure yielded a residual strength for plate constructs of 2.30 ± 1.17 N m, demonstrating that plating restored 77% of the strength of native ribs (2.97 ± 1.80 N m). This residual construct strength was 58 times greater than physiologic loads during normal respiration. Eighteen of the 20 constructs failed by rib fracture adjacent to the plate end, and two constructs failed by plate bending over the fracture.
Mechanical testing results demonstrated that flexible rib plates did not increase the native stiffness of ribs, regardless of whether the fractures were stabilized in osteoporotic or strong ribs. By combining flexible plating with locking screw fixation, the anatomic rib plates effectively prevented screw loosening and pull-out while restoring 77% of the native rib strength.
Evaluation of IM splints
The mechanical function of the rib splint constructs was characterized analogously to that of the anatomic plate constructs by assessing construct stiffness, durability, strength, and failure modes in 22 paired ribs [24]. Paired testing was performed to allow for a direct comparison in mechanical function between rib splint constructs and conventional Kirschner-wire constructs for IM stabilization of rib fractures. Fractures in right ribs were stabilized with 80 mm long Kirschner wires of 1.5 mm diameter that were inserted through an entry portal at a distance of 30 mm from the fracture (Fig. 7a). Fractures in left ribs were stabilized with 4 mm wide rib splints (Fig. 7b).
Fig. 7.
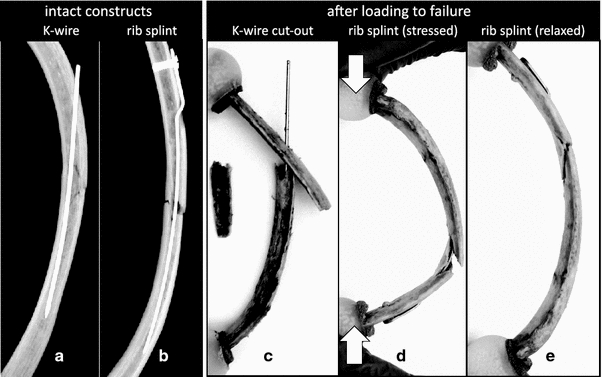
Rib fractures stabilized with a 1.5 mm Kirschner wire and b rib splint; c catastrophic failure of Kirschner-wire construct by cutting through the medial cortex, causing loss of reduction, instability, and protrusion of the wire from the rib; d failure of the rib splint construct by fracture along the superior and inferior cortices, shown in the stressed position; e after load removal, splint constructs recovered elastically and retained functional reduction and fixation, suggesting that this failure mode would remain clinically asymptomatic
There was no significant difference in stiffness between the rib splint constructs (2.0 ± 1.0 N/mm) and the Kirschner-wire constructs (2.5 N/mm, P > 0.05). All constructs sustained dynamic loading without failure. After dynamic loading, the residual strength of the rib splint constructs remained 48% greater than that of the Kirschner-wire constructs, and was 26 times greater than the bending loads under physiologic respiration [28]. Five of the 11 Kirschner-wire constructs failed catastrophically by cutting through the medial cortex, leading to complete loss of stability and wire migration through the lateral cortex (Fig. 7c). In contrast, no splint construct failed catastrophically and all of the splint constructs retained functional reduction and fixation (Fig. 7d, e).
In summary, rib splints provided superior strength and prevented the complications of implant migration and cut-out seen with Kirschner wires.
Discussion
This line of research described the anatomic foundation, design features, and biomechanical evaluation of a novel implant system for the stabilization of rib fractures. By combining anatomic plates and intramedullary splints, this system provides a comprehensive solution that accommodates the large variety of fracture patterns and fracture locations encountered in complex flail chest injuries. Most recently, this system has been further refined and has been made available for clinical use by Synthes CMF (MatrixRIB, Synthes, West Chester, PA, USA). The system represents a conservative solution based on established techniques which were systematically enhanced to support the unique requirements for rib fracture fixation while preventing the complications reported for the traditional techniques. Plate osteosynthesis and intramedullary fixation historically represent the two most common techniques for rib fracture stabilization.
Compared to traditional plating, the anatomic plate set reduces the challenge of intraoperative plate contouring, provides flexible stabilization, and employs locking screws to enhance fixation in osteoporotic ribs. It therefore not only reduces the time and complexity of the operative procedure but also provides durable, low-profile fixation with a decreased need for implant removal. Anatomic plates also support the use of long plates to allow the bridging of comminuted fractures, the spanning of multiple fractures, and the suspension of fail segments [18, 19].
The results of the plate fit evaluation demonstrated that the anatomic plate set largely eliminates the need for intraoperative plate contouring by providing the appropriate in-plane curvature and longitudinal twist. Locking plates provide improved fixation strength by rigidly connecting locking screws to the plate and rib, while conventional plating constructs rely on plate compression onto the rib surface to achieve stable fixation [31]. By eliminating the need for plate compression to the bone surface, locking plates support biological fixation while preserving periosteal perfusion [32, 33]. Locking plates provide stable fixation even if the plate is not perfectly contoured to the rib surface. However, to avoid the unintended elevation of locking plates over the rib surface, the plates should be approximated to the rib surface before the head of the locking screw engages into the plate.
Rib splints represent an enhanced version of the traditional approach of intramedullary rib fixation with Kirschner wires. The biomechanical evaluation of the rib splint constructs demonstrated that the design features of the rib splint reliably prevented the implant migration and cut-out seen with Kirschner wires, while delivering improved construct strength. Therefore, rib splints are an attractive intramedullary alternative for the less-invasive stabilization of rib fractures, especially in the case of posterior rib fractures, where access for plating is limited. Unlike anatomic rib plates, rib splints are not designed to span multiple or severely comminuted fractures. While rib splints enable a less-invasive approach compared to plate fixation, sufficient access is required to ensure that rib splints can be inserted tangential to the rib surface.
Both anatomic plate and rib splint implants are designed for flexible fixation in order to provide durable stabilization, to restore rib function, and to promote fracture healing by callus formation. Elastic implants with low stiffness can minimize peak stresses at the bone–implant interface, making them particularly suitable for fracture fixation in osteoporotic bone [20]. Specific for rib fixation, Labitzke et al. [9] emphasized that stiff implants can restrict respiratory motion and are prone to fixation failure due to stress concentrations. Unlike implants that are primarily designed for load bearing, they stated that the principal function of rib implants is to restore chest wall integrity by maintaining fracture apposition without restricting respiratory kinematics, which requires elastic fixation constructs. In regard to fracture healing, flexible fixation enables interfragmentary motion, which in turn promotes callus formation and bony union [32]. Conversely, rigid fixation can suppress healing and can lead to bone resorption [34].
The mechanical evaluation of anatomic plate and rib splint constructs has several limitations. Implants were only tested in one loading mode, representing the principal loading of ribs in vivo [28]. Testing was limited to the fixation of single transverse or oblique fractures, and did not account for severely comminuted fractures. Furthermore, constructs were tested in isolation without accounting for secondary stabilization provided by adjacent ribs and the surrounding soft-tissue envelope. To overcome the limitations inherent to any biomechanical study, a prospective clinical study will be essential to further evaluate the performance of MatrixRIB implants in vivo.
In conclusion, research on rib biomechanics afforded a detailed understanding of the form and function of ribs, which served as the foundation for the design of a specialized system for rib fracture fixation. The resulting system combines a set of anatomic plates and intramedullary splints to accommodate the range of fractures seen in complex flail chest injuries. By resolving the principal limitations and complications encountered with traditional plating and IM fixation techniques, this comprehensive system for rib fracture fixation will simplify the surgical procedure, provide more reliable stabilization, and will likely be better tolerated by patients.
Acknowledgments
Conflict of interest
One or more of the authors receive consulting/royalty payments from Synthes CMF related to technology discussed.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Cacchione RN, Richardson JD, Seligson D. Painful nonunion of multiple rib fractures managed by operative stabilization. J Trauma. 2000;48(2):319–321. doi: 10.1097/00005373-200002000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Ng AB, Giannoudis PV, Bismil Q, Hinsche AF, Smith RM. Operative stabilisation of painful non-united multiple rib fractures. Injury. 2001;32(8):637–639. doi: 10.1016/S0020-1383(01)00017-1. [DOI] [PubMed] [Google Scholar]
- 3.Richardson JD, Franklin GA, Heffley S, Seligson D. Operative fixation of chest wall fractures: an underused procedure? Am Surg. 2007;73(6):591–596. [PubMed] [Google Scholar]
- 4.Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4(6):583–587. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727–732. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Mayberry JC, Ham LB, Schipper PH, Ellis TJ, Mullins RJ. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma. 2009;66(3):875–879. doi: 10.1097/TA.0b013e318190c3d3. [DOI] [PubMed] [Google Scholar]
- 7.Engel C, Krieg JC, Madey SM, Long WB, Bottlang M. Operative chest wall fixation with osteosynthesis plates. J Trauma. 2005;58(1):181–186. doi: 10.1097/01.TA.0000063612.25756.60. [DOI] [PubMed] [Google Scholar]
- 8.Friedrich B, Redeker H, Kljucar S. The unstable thoracic wall: possibilities for treatment. Helv Chir Acta. 1991;58(1–2):77–82. [PubMed] [Google Scholar]
- 9.Labitzke R. Early thoracotomy and chest wall stabilization with elastic rib clamps (author’s transl) Zentralbl Chir. 1981;106(20):1351–1359. [PubMed] [Google Scholar]
- 10.Lardinois D, Krueger T, Dusmet M, Ghisletta N, Gugger M, Ris HB. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20(3):496–501. doi: 10.1016/S1010-7940(01)00818-1. [DOI] [PubMed] [Google Scholar]
- 11.Paris F, Tarazona V, Blasco E, Canto A, Casillas M, Pastor J, Paris M, Montero R. Surgical stabilization of traumatic flail chest. Thorax. 1975;30(5):521–527. doi: 10.1136/thx.30.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Schmit-Neuerburg KP. Operative chest wall stabilization in flail chest—outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187(2):130–138. doi: 10.1016/S1072-7515(98)00142-2. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110(6):1676–1680. doi: 10.1016/S0022-5223(95)70030-7. [DOI] [PubMed] [Google Scholar]
- 14.Albrecht F, Brug E. Stabilization of the flail chest with tension band wires of ribs and sternum (author’s transl) Zentralbl Chir. 1979;104(12):770–776. [PubMed] [Google Scholar]
- 15.Menard A, Testart J, Philippe JM, Grise P. Treatment of flail chest with Judet’s struts. J Thorac Cardiovasc Surg. 1983;86(2):300–305. [PubMed] [Google Scholar]
- 16.Moore BP. Operative stabilization of nonpenetrating chest injuries. J Thorac Cardiovasc Surg. 1975;70(4):619–630. [PubMed] [Google Scholar]
- 17.Shah TJ. On internal fixation for flail chest. J Thorac Cardiovasc Surg. 1996;12(3):849–850. doi: 10.1016/S0022-5223(96)70080-6. [DOI] [PubMed] [Google Scholar]
- 18.Haasler GB. Open fixation of flail chest after blunt trauma. Ann Thorac Surg. 1990;49(6):993–995. doi: 10.1016/0003-4975(90)90886-B. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez-Lloret J, Letang E, Mateu M, Callejas MA, Catalan M, Canalis E, Mestres CA. Indications and surgical treatment of the traumatic flail chest syndrome. An original technique. Thorac Cardiovasc Surg. 1982;30(5):294–297. doi: 10.1055/s-2007-1022410. [DOI] [PubMed] [Google Scholar]
- 20.Lill H, Hepp P, Korner J, Kassi JP, Verheyden AP, Josten C, Duda GN. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003;123(2–3):74–81. doi: 10.1007/s00402-002-0465-9. [DOI] [PubMed] [Google Scholar]
- 21.Mohr M, Abrams E, Engel C, Long WB, Bottlang M. Geometry of human ribs pertinent to orthopedic chest-wall reconstruction. J Biomech. 2007;40(6):1310–1317. doi: 10.1016/j.jbiomech.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 22.Bottlang M, Helzel I, Long W, Fitzpatrick D, Madey S. Less-invasive stabilization of rib fractures by intramedullary fixation: a biomechanical evaluation. J Trauma. 2010;68(5):1218–1224. doi: 10.1097/TA.0b013e3181bb9df1. [DOI] [PubMed] [Google Scholar]
- 23.Bottlang M, Helzel I, Long WB, Madey S. Anatomically contoured plates for fixation of rib fractures. J Trauma. 2010;68(3):611–615. doi: 10.1097/TA.0b013e3181a5b260. [DOI] [PubMed] [Google Scholar]
- 24.Helzel I, Long W, Fitzpatrick D, Madey S, Bottlang M. Evaluation of intramedullary rib splints for less-invasive stabilisation of rib fractures. Injury. 2009;40(10):1104–1110. doi: 10.1016/j.injury.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Mouton W, Lardinois D, Furrer M, Regli B, Ris HB. Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg. 1997;45(5):242–244. doi: 10.1055/s-2007-1013735. [DOI] [PubMed] [Google Scholar]
- 26.Reber PU, Kniemeyer HW, Ris HB. Reconstruction plates for internal fixation of flail chest. Ann Thorac Surg. 1998;66(6):2158. [PubMed] [Google Scholar]
- 27.Granik G, Stein I. Human ribs: static testing as a promising medical application. J Biomech. 1973;6(3):237–240. doi: 10.1016/0021-9290(73)90045-6. [DOI] [PubMed] [Google Scholar]
- 28.Rehm KE. Die Osteosynthese der Thoraxwandinstabilitaeten. Hefte zur Unfallheilkunde 1986;175.
- 29.Sales JR, Ellis TJ, Gillard J, Liu Q, Chen JC, Ham B, Mayberry JC. Biomechanical testing of a novel, minimally invasive rib fracture plating system. J Trauma. 2008;64(5):1270–1274. doi: 10.1097/TA.0b013e31804a7fd5. [DOI] [PubMed] [Google Scholar]
- 30.Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–1046. doi: 10.1097/00005373-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Fitzpatrick DC, Doornink J, Madey SM, Bottlang M. Relative stability of conventional and locked plating fixation in a model of the osteoporotic femoral diaphysis. Clin Biomech (Bristol, Avon) 2009;24(2):203–209. doi: 10.1016/j.clinbiomech.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg. 2002;84(8):1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 33.Tan SL, Balogh ZJ. Indications and limitations of locked plating. Injury. 2009;40(7):683–691. doi: 10.1016/j.injury.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci. 2006;11(2):118–126. doi: 10.1007/s00776-005-0984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


