Abstract
Schwannoma is the most common neurogenic tumor that is derived from the peripheral nerve sheath. There are no specific serologic markers or characteristic imaging abnormalities associated with schwannoma. Tissue diagnosis and immunohistochemistry are required to diagnose this lesion. We describe a 65-year-old male with a finding of three mass lesions in the superior and middle mediastinum on computed tomography of the chest. The largest lesion measured 4.6 × 5 cm. The patient subsequently underwent endoscopic ultrasonography-guided fine needle aspiration (EUS-FNA) of the lesion and cytology was consistent with spindle cell neoplasm. Immunohistochemical staining of the cytologic specimen was positive for S-100 and negative for pan-cytokeratin, CD34, CD117, calcitonin, smooth muscle actin and desmin. These findings were consistent with schwannoma. This is the second reported case of a mediastinal schwannoma diagnosed by EUS-FNA.
Key words: Endoscopic ultrasonography, Schwannoma, Mediastinal tumor
Introduction
Mediastinal mass is a common clinical problem for which patients are referred to pulmonologists or cardiothoracic surgeons for further evaluation. Depending on the location in the mediastinum, these masses are classified as masses arising from the anterior, mid, or posterior mediastinum. Thymic tumors, Hodgkins and non Hodgkins lymphoma, lipoma, liposarcoma and parathyroid adenoma are some of the commonly found anterior mediastinal tumors [1]. Anterior compartment mediastinal masses are more likely to be malignant when compared to lesions in the other compartments [2]. Masses in the middle mediastinum include thyroid tumors, lymphoma, tracheal tumors, malignant lymph nodes etc. Neurogenic tumors, esophageal tumors, and duplication cysts are usually found in the posterior mediastinum [3].
Schwannomas are the most common benign neurogenic neoplasms in the mediastinum. These tumors originate from Schwann cells, which are the principal neuroglial cells in the nerve sheath of the peripheral nervous system. The prevalence of these tumors is similar in both genders [4, 5]. Schwannomas are either asymptomatic or present with vague symptoms such as chest discomfort, cough and weakness. The lack of specific biochemical assay or tumor markers for these lesions entails the need to obtain tissue from the lesion to make a definitive diagnosis. Endoscopic ultrasonography (EUS) appears to be a useful test for the evaluation of these lesions; however its role in the diagnosis of mediastinal schwannomas has not been extensively evaluated. Fine needle aspiration (FNA) combined with EUS also facilitates tissue sampling to help make a definitive diagnosis of this lesion. Here, we present a case of mediastinal schwannoma diagnosed by ultrasonography-guided fine needle aspiration (EUS-FNA) in a patient presenting for evaluation of mediastinal masses.
Case Report
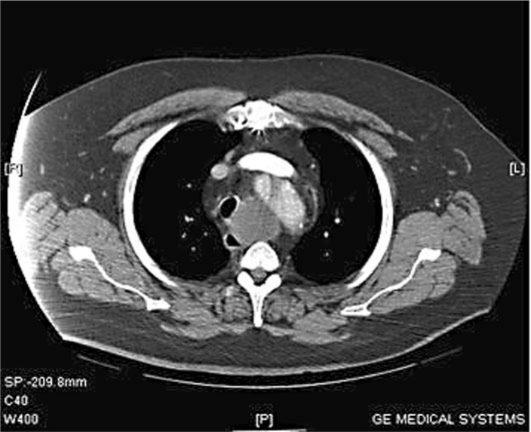
A 65-year-old Caucasian male underwent computed tomography (CT) of the chest for evaluation of dyspnea and intermittent dysphagia and was found to have three mass lesions in the superior and middle mediastinum. The first mass measured 5 × 5 cm and caused tracheal displacement. The second mass measuring 5 × 4 cm was seen in the mid mediastinum medial to the aortic arch, and the third mass measuring 3 × 3 cm was seen just above the left main stem bronchi (fig. 1). No calcifications were identified in the masses and no lymphadenopathy was found in the axillary or subclavian regions. The superior mediastinal portion appeared in continuity with the mass in the mid mediastinum. Physical examination of the heart, lungs, and chest was unremarkable, and no palpable lymphadenopathy was appreciated.
Fig. 1.
CT image of the mediastinal lesions. In this CT, a mass is seen in the mid mediastinum medial to the aortic arch, and another mass is seen just above the left main stem bronchi.
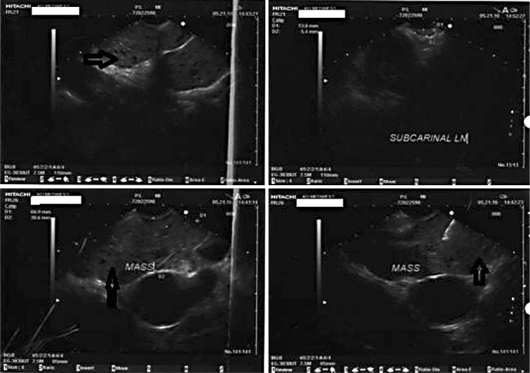
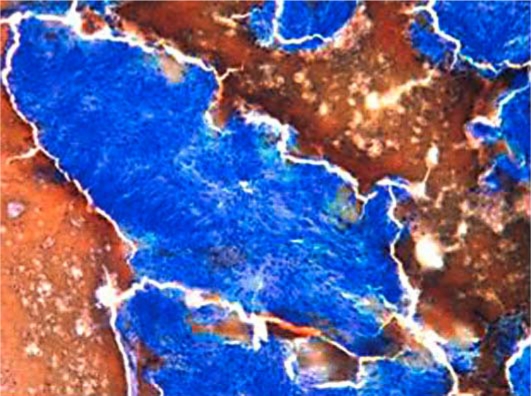
The patient was referred for EUS of this mass lesion which revealed three well-demarcated hypoechoic peritracheal mass lesions. Some anechoic changes were seen within these lesions suggestive of liquification or necrosis of the masses (fig. 2). EUS-FNA of the lesion was performed. Cytologic interpretation showed that the FNA specimen contained a bland proliferation of spindle cells, favoring the diagnosis of a neurogenic neoplasm such as schwannoma. Immunohistochemistry performed on the tumor cells on the cell block was positive for immunohistochemical stain S-100 (fig. 3) and negative for immunohistochemical stains pan-cytokeratin, CD34, CD117, calcitonin, smooth muscle actin and desmin. This immunohistochemical profile was consistent with the diagnosis of schwannoma.
Fig. 2.
EUS images of the mediastinal lesion. The arrow points to the hypoechoic mass lesion that was seen in the mediastinum during the EUS procedure. The fourth image in the series shows the FNA needle obtaining a specimen from the lesion.
Fig. 3.
Immunohistochemistry staining of lesional cells with S-100 that was supportive of the diagnosis of schwannoma. The cells did not stain for pan-cytokeratin, CD34, CD117, calcitonin, smooth muscle actin and desmin (not shown). This pattern fit in with the immunohistochemical pattern of schwannoma.
Since the patient had symptoms associated with the schwannoma, he underwent thoracotomy and resection of the lesion. The histopathology result from the resected specimen was also interpreted as schwannoma, confirming the findings of EUS-FNA cytology. No complications were reported from the EUS-FNA procedure or from the surgical resection of the lesion.
Discussion
This case report demonstrates that EUS-FNA can be used as an effective and noninvasive modality for the diagnosis of a mediastinal schwannoma. Transthoracic imaging studies such as CT, magnetic resonance imaging, and positron emission tomography can define the exact location of the lesions and may narrow the differential diagnosis; however histological diagnosis is invariably required to establish the diagnosis of schwannoma. The diagnostic modalities available to obtain tissue for diagnosis in this clinical scenario include mediastinoscopy, CT-guided biopsy, video-assisted thoracotomy, EUS-FNA, and endobronchial ultrasound FNA. Among these, EUS-FNA is the least invasive test. In addition, the availability of Doppler ultrasonography during EUS-FNA also helps to minimize injury to the surrounding vascular structures during FNA of mediastinal lesions.
Although mediastinal schwannoma is not that uncommon, this is only the second case report demonstrating the diagnosis of this lesion by EUS-FNA [6], suggesting that EUS is not often performed for this indication. By opting to undergo EUS-FNA as the diagnostic modality to obtain tissue from the mediastinal lesion, the patient avoided the complications associated with other more invasive procedures such as mediastinoscopy. In addition, EUS has the additional advantage of being an outpatient procedure. However, EUS is not a preferred technique to investigate the anterior mediastinum as the presence of air in the trachea decreases the resolution and quality of imaging.
There might be a concern for using EUS in this scenario as the amount of tissue obtained by FNA may not be adequate for cytologic interpretation, however most programs like ours have a bedside cytopathologist available who will guide endosonographers to perform enough FNA passes so that an adequate specimen is obtained to make a conclusive diagnosis. Immunostains can also be performed on the aspirate that further help to differentiate schwannoma from other mediastinal tumors. The specimens obtained by EUS-FNA are also not subject to artifacts from crush or cautery injury that are usually seen with samples obtained by other modalities like mediastinoscopy. The later phenomenon can make pathological interpretation difficult.
In conclusion, EUS-FNA should be offered to patients as a viable diagnostic modality for all accessible mediastinal lesions, including schwannoma. Potential complications from other invasive procedures can be avoided by opting to perform EUS for this indication. Studies comparing the efficacy and safety of EUS-FNA with other procedures for this indication such as CT-guided biopsy, mediastinoscopy or video-assisted thoracoscopic surgery are awaited.
Disclosure Statement
The authors have no financial disclosure to make.
References
- 1.Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part I: Tumors of the anterior mediastinum. Chest. 1997;112:511–522. doi: 10.1378/chest.112.2.511. [DOI] [PubMed] [Google Scholar]
- 2.Davis RD, Jr, Oldham HN, Jr, Sabiston DC., Jr Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44:229–237. doi: 10.1016/s0003-4975(10)62059-0. [DOI] [PubMed] [Google Scholar]
- 3.Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part II. Tumors of the middle and posterior mediastinum. Chest. 1997;112:1344–1357. doi: 10.1378/chest.112.5.1344. [DOI] [PubMed] [Google Scholar]
- 4.Marchevsky AM. Mediastinal tumors of peripheral nervous system origin. Semin Diagn Pathol. 1999;16:65–78. [PubMed] [Google Scholar]
- 5.Moran CA, Suster S. Primary mediastinal choriocarcinomas: a clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1997;21:1007–1012. doi: 10.1097/00000478-199709000-00004. [DOI] [PubMed] [Google Scholar]
- 6.McGrath KM, Ballo MS, Jowell PS. Schwannoma of the mediastinum diagnosed by EUS-guided fine needle aspiration. Gastrointest Endosc. 2001;53:362–365. doi: 10.1016/s0016-5107(01)70419-1. [DOI] [PubMed] [Google Scholar]