Abstract
Objective
The timely discharge of moderately premature infants has important economic implications. The decision to discharge should occur independent of unit census. We evaluated the impact of unit census on the decision to discharge moderately preterm infants.
Design/Methods
In a prospective multicenter cohort study, we enrolled 850 infants born between 30 and 34 weeks' gestation at 10 NICUs in Massachusetts and California. We divided the daily census from each hospital into quintiles and tested whether discharges were evenly distributed among them. Using logistic regression, we analyzed predictors of discharge within census quintiles associated with a greater- or less-than-expected likelihood of discharge. We then explored parental satisfaction and postdischarge resource consumption in relation to discharge during census periods that were associated with high proportions of discharge.
Results
There was a significant correlation between unit census and likelihood of discharge. When unit census was in the lowest quintile, patients were 20% less likely to be discharged when compared with all of the other quintiles of unit census. In the lowest quintile of unit census, patient/nurse ratio was the only variable associated with discharge. When census was in the highest quintile, patients were 32% more likely to be discharged when compared with all of the other quintiles of unit census. For patients in this quintile, a higher patient/nurse ratio increased the likelihood of discharge. Conversely, infants with prolonged lengths of stay, an increasing Score for Neonatal Acute Physiology II, and minor congenital anomalies were less likely to be discharged. Infants discharged at high unit census did not differ from their peers in terms of parental satisfaction, emergency department visits, home nurse visits, or rehospitalization rates.
Conclusions
Discharges are closely correlated with unit census. Providers incorporate demand and case mix into their discharge decisions.
Keywords: infant, newborn, census, discharge, health services research, workforce
In the year 2000, neonatal intensive care consumed approximately $4.6 billion or 10% of the total health budget allocated to the health care of children.1 Moderately premature infants make up the largest group of infants receiving neonatal intensive care2,3 and, therefore, account for a large part of its direct medical cost. Because of the strong association between cost and length of stay, variability in the decision to discharge has important economic implications.
Theoretically, discharge should be based on the infant's medical condition and the parents' readiness to assume their care taking role at home. However, externalities, such as the unit workload, may contribute to clinical decision-making in relation to discharge. We hypothesized that when NICU workload is high, clinicians might discharge more readily to reduce the strain on personnel. Conversely, when the NICU workload is low, clinicians may be tempted to defer discharge. This creates unnecessary variation in length of stay in the NICU, potentially contributing to increasing health care costs.
Unit census, nurses' workload, doctors' workload, and case mix all contribute to unit workload. These variables interact with each other to influence many work processes in the NICU. Ideally, staffing and work processes are flexible and accommodate fluctuations in workload without affecting the provision of care. Otherwise, periods of high demand may exceed the providers' ability to accommodate workload and compromise quality of care,4 and periods of low demand in NICUs may result in an over-supply of staff in relation to workload.
To understand how NICUs respond to changes in workload, we designed this study to answer the following specific research questions: (1) Are infants being discharged in equal proportions across the entire range of unit census? (2) If not, then what are the characteristics associated with discharge at a given level of unit census? (3) How does discharge timing affect parental satisfaction and postdischarge resource use?
Methods
Sample
The Moderately Premature Infant Project (MPIP) is a multicenter cohort study of infants with a gestational age of 30 weeks to 34 weeks plus 6 days. Details of this study are described elsewhere.5 In brief, between September 2001 and January 2003, 100 infants each were recruited from 3 level II and 7 level III NICUs in Massachusetts and California at their day of discharge. NICU logbooks were used to develop a list of eligible patients at each site, and this list was crosschecked against the hospital birth registry for any missed cases. At 3 high-volume sites, patients were randomly selected using sampling algorithms to assure that the final sample size of 100 was evenly distributed over the enrollment period. In 4 sites, enrollment was slower than expected, and the target size was reduced to 60 to 65 infants so that all of the sites were collecting data through the same period.
Measures
We abstracted data from patient charts and hospitals' administrative records according to a previously validated protocol, the Neonatal Minimum Data Set.6 We derived our dependent variable (unit census at the time of discharge to home) by averaging midnight census of the 2 days before discharge. This served 3 functions. First, we avoided the endogeneity inherent in measuring census after discharge. Second, averaging census over 2 days before discharge clinically captures discharge preparations. Third, smoothing over 2 days may help protect the measure from undue influence by outliers. When information on census at discharge was missing, we imputed its value by carrying forward the last available day.
We defined unit census as our primary determinant of workload but included other markers of this construct, including patient/nurse ratio (PNR) and case mix, in our regression analyses. Based on clinical experience and previous research,7–12 we used the following prenatal, socioeconomic, clinical, and organizational candidate variables as additional potential predictors of discharge: maternal age, multiple gestation, prenatal care, primigravida, antenatal and postnatal steroids, birth weight, gestational age, gender, minor congenital anomalies (including, eg, atrial septal defect, hypospadias, or club foot), Score for Neonatal Acute Physiology II (SNAP II),13 surfactant, mechanical ventilation, central venous line placement, sepsis or bacteremia, any adverse event including need for surgery, intraventricular hemorrhage, necrotizing enterocolitis, inadequate weight gain, discharge weight, use of home oxygen, home oxygen saturation monitoring, home medications, length of stay, PNR averaged over the 48 hours before discharge (akin to our census measure), unit level II or III, state, and weekday versus weekend discharge.
A 3-month postdischarge follow-up telephone survey collected data on annual household income (at or less than $30 000, $30 001–50 000, or more than $50 000), parental return to work, parental education (high school, college, or postgraduate training), race, parental satisfaction, rehospitalizations, emergency department, and home nursing visits. Determination of health care use was based on questions fielded in an evaluation of a demonstration program of perinatal regionalization.14 Satisfaction was ascertained using a 12-item scale, a modified version of an instrument validated previously in 1 of the study settings. This scale had a mean (±SD) of 37.7 (±6.5) and a range of 5 to 45.15
Analysis
We divided each unit's census into quintiles. Discharges should be evenly distributed across all of the quintiles, with 20% occurring in each. We computed a standardized discharge ratio (SDR) by dividing observed and expected discharges (SDR is the number of discharges in census quintile divided by 20% of patients in census quintile). An SDR of 1 indicates that discharges occur at expected proportions.
We calculated the proportion of discharges within each quintile of unit census and used Spearman's ρ (rs) correlation coefficient to assess the trend between census and discharges. A test of binomial proportions applied in each quintile evaluated whether the SDR differed from 1. Bonferroni corrections were used to adjust the results for multiple comparisons.
We used bivariate analyses to test the association of clinical characteristics at the lowest and highest quintiles of unit census. Variables with P values of <.15 were entered into the regression models using a stepwise selection process and retained at P values of <.05. To assess the most important predictors of discharge at the extremes of workload, we used multivariate logistic regression, correcting the SEs of the hospital-level variables for the effect of within-hospital correlation using generalized estimating equations.16
To evaluate the effect of discharge in the highest quintile of census, we used t tests for continuous variables (parental satisfaction) and χ2 tests for categorical variables (home nursing visit, emergency department visit, and rehospitalization). The institutional review boards of participating institutions granted approval for this study.
Results
Summary Statistics
A total of 850 infants were enrolled in the MPIP study, of which 818 had complete census data. As shown in Table 1, median birth weight and gestational age were 1935 g and 33.4 weeks, respectively. Overall illness severity was low, with a median SNAP II score of 5. Theoretically, SNAP II scores can range from 0 to 115. Practically, a score of <9 is considered low, and a score of >20 is considered high. Median census on day of discharge was 14. Postmenstrual age at discharge was just below 36 weeks. About half of our patients were male or white. Minor congenital anomalies and significant bacterial or viral infections were overall relatively uncommon.
TABLE 1. Descriptive Summary of Sample: Maternal and Infant Characteristics.
| Variable | Median (Interquartile Range) |
|---|---|
| Birth weight, g | 1935 (1655–2215) |
| Gestational age, wk | 33.4 (32.1–34.3) |
| SNAP II score | 5 (0–9) |
| Census on day of discharge | 14 (9–37) |
| Length of stay, d | 17 (11–27) |
| Postmenstrual age at discharge, wk | 35.9 (35.3–36.7) |
| PNR averaged over 48 h before discharge | 2.3 (1.9–2.8) |
| Male gender, n (%) | 429 (51) |
| Minor congenital anomaly, n (%) | 19 (2.2) |
| Maternal race, white, n (%) | 405 of 673 (60) |
Total N = 850.
Are Infants Being Discharged in Equal Proportions Across the Entire Range of Unit Census?
Figure 1 shows the SDRs across quintiles of unit census at discharge. Measured across all quintiles, unit census and discharges were highly correlated (rs = 0.79; P = .007). Tests within each quintile of unit census revealed that NICUs deviated from expected discharge proportions at both extremes. In the lowest quintile of unit census, patients were less likely to be discharged (SDR: 0.8; range: 0.68–0.94; P = <.01). Conversely, in the highest quintile of unit census, patients were more likely to be discharged (SDR: 1.32; range: 1.17–1.48; P < .001). Only in the middle 3 census quintiles were infants discharged at expected proportions. In summary, an individual's probability of discharge was 20% lower than expected at low census and 32% higher than expected at high census.
FIGURE 1.
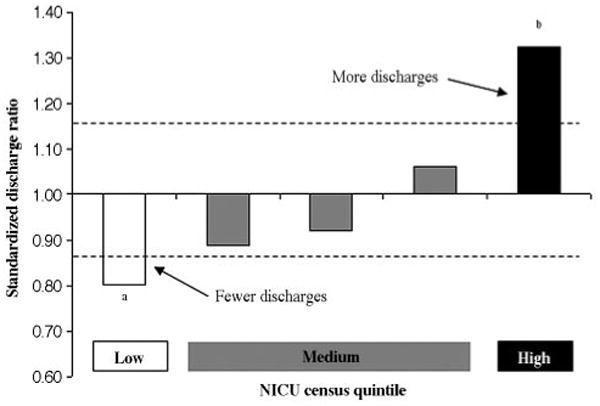
SDR by NICU census level. Dashed lines indicate 95% CI around expected SDR of 1, indicating random variation. aP < .01;b P < .001.
What Are the Characteristics Associated With Discharge at the Extremes of Unit Census?
After establishing that proportions of discharge deviated from expected levels at both extremes of unit census, we identified the characteristics associated with these outcomes using multivariable logistic regression adjusted for clustering at the unit level. As seen in Table 2, the PNR was the only variable associated with discharge in the lowest quintile of unit census. Discharge in the lowest quintile of unit census was more likely at a lower PNR (odds ratio [OR]: 0.04; 95% confidence interval [CI]: 0.01–0.23; P < .001).
TABLE 2. Variable Associated With Discharge at Low Unit Census.
| Model Variables | β | SE | OR | 95% CI | P |
|---|---|---|---|---|---|
| PNR | −3.29 | 0.92 | 0.04 | 0.01–0.23 | <.001 |
Multivariate logistic regression results show the characteristics of infants discharged in the lowest quintile of NICU census. Results were adjusted for clustering at the unit level.
As seen in Table 3, for those patients discharged in the highest quintile of unit census, the higher the PNR, the higher the odds of discharge (OR: 14.2; 95% CI: 2.50–80.5; P = .003). Conversely, infants with prolonged lengths of stay (OR: 0.62; 95% CI: 0.40–0.96; P = .03), an increasing SNAP-II score (OR: 0.99; 95% CI: 0.98–0.99; P = .03), and minor congenital anomalies (OR: 0.43; 95% CI: 0.39–0.63; P < .0001), were less likely to be discharged.
TABLE 3. Variables Associated With Discharge at High Unit Census.
| Model Variables | β | SE | OR | 95% CI | P |
|---|---|---|---|---|---|
| PNR | 2.65 | 0.89 | 14.2 | 2.50–80.5 | .003 |
| Length of stay >90th percentile | −.48 | 0.23 | 0.62 | 0.40–0.96 | .03 |
| SNAP II | −.01 | 0.004 | 0.99 | 0.98–0.99 | .03 |
| Minor congenital anomaly | −.83 | 0.19 | 0.43 | 0.30–0.63 | <.0001 |
Multivariate logistic regression results show the characteristics of infants discharged in the highest quintile of NICU census. Results were adjusted for clustering at the unit level.
The opposing influence of PNRs on discharge at low and high unit census may be explained by the correlation between this variable and unit census. Among the 10 NICUs, the correlation between unit census and PNR at the time of discharge was very strong in 6 NICUs (rs > 0.7; range: 0.72–0.94), moderate in 2 NICUs (rs = 0.44 and 0.56), and weak in only 2 units (rs = 0.14 and 0.19). The association of these 2 variables with discharge, therefore, indicates that as census rises, the PNR rises. Therefore, discharge at low census is likely to be associated with a low PNR and discharge at high census with a high PNR.
How Does Discharge Timing Affect Parental Satisfaction and Postdischarge Resource Use?
The response rate to the 3-month follow-up survey was 80% (676 of 850). There was no statistical difference in parental satisfaction scores, postdischarge nurse visits, emergency department visits, or rehospitalizations between infants who were discharged when unit census was high compared with their peers (Table 4).
TABLE 4. Postdischarge Resource Use.
| Variable | Discharge Highest Quintile | Discharge Other Quintiles | P |
|---|---|---|---|
| PSS, mean (SD) | 37.4 (6.4) | 37.9 (6.4) | .41 |
| Home nursing visit, % | 48.4 | 48.7 | .93 |
| Emergency department visit, % | 14.3 | 18.9 | .17 |
| Rehospitalization, % | 10.4 | 11.9 | .61 |
Parental satisfaction and resource use between infants discharged in the highest census quintile versus all others. Parental satisfaction score (PSS) is a continuous variable. Home nursing visit, emergency department visit, and rehospitalization are categorical variables. Adjustment for case mix in logistic regression did not alter results.
Discussion
This is the first study to relate discharges of moderately premature infants to unit census. We demonstrated that in the highest quintile of unit census, infants were more likely to be discharged, and in the lowest quintile of unit census, infants were less likely to be discharged. Our findings indicate that discharges depend not only on clinical status but also on unit workload, suggesting that admissions to and discharges from NICUs fluctuate to create periods of both spare and reduced capacity. These fluctuations influence provider behavior such that when unit workload is high, patients with a low clinical risk profile are tagged for discharge. When unit workload is low, on the other hand, the bar for discharge seemed to rise for all of the infants.
In the highest quintile of unit census, patients were discharged more readily. Infants with prolonged lengths of stay, minor congenital anomalies, and a higher SNAP II were less likely to be discharged in this environment, representing appropriate provider selection for underlying clinical risk. The association of increased discharges with higher PNRs suggests that strains on staff influenced clinical decision-making. This is disconcerting, because there may have been trade-offs in quality of care.4,17
We were unable to demonstrate a negative influence on either parental satisfaction or subsequent use of medical resources. However, given the low illness severity of the study population, these measures may not have been sensitive enough to signal a quality problem.
In the lowest quintile of NICU census, infants were less likely to be discharged. The PNR was the only variable associated with discharge in this environment. Our results indicate that as the PNR rose, patients were less likely to be discharged, the opposite of the trend observed at high NICU census levels. We suggest the following explanation for this finding. PNR and census strongly covaried in many NICUs. Thus, as the PNR increased, patients were less likely to be in the lowest quintile of census. Overall, the interpretation of this particular finding is speculative and should not be over-emphasized.
A variety of factors may contribute to our findings, including variability in medical care and organizational and staffing factors. Variability in neonatal intensive care practices is well documented in the literature.7,11,18–23 Furthermore, providers have been shown to use different criteria for determining discharge readiness.9,24 The findings of this study suggest that these criteria are not consistently applied to all patients but rather depend on unit workload.
Our study confirms and expands previous research that highlights the important influence of unit workload and staffing factors on mortality4,10,25–31 and morbidity.32–37 Tarnow-Mordi et al11 examined the impact of unit workload (as measured by occupancy rates and nurse staffing) on mortality in adult ICUs and found that the adjusted mortality was more than double for patients exposed to high unit workload. The United Kingdom Neonatal Staffing Study Group reported that infants admitted at full NICU capacity were 50% more likely to die.28 Studies by Gould et al10 and Touch et al12 assessed the influence of the weekend effect on mortality and discharge timing, respectively. Whereas findings of the former suggest comparable mortality rates across days, Touch et al12 showed an uneven distribution of discharges across days of the week, suggesting the potential for organizational intervention and cost savings.
NICUs will experience staffing constraints for the foreseeable future.36,38 It is, therefore, important to optimize work processes so that providers can manage high workload. Naylor et al39 demonstrated that advanced-practice nurse-centered discharge planning and home care intervention for at-risk hospitalized elders can reduce readmissions and decrease health care costs. Data on the reduction of length of stay using case managers are mixed, but seem promising in resource-intensive environments, such as NICUs.40–44 In a recent study, we reported on the differences of gestational age at discharge for moderately premature infants who received their care at the Kaiser Permanente Medical Care Program in Northern California versus those cared for in Massachusetts and the United Kingdom. Infants in the California cohort experienced an 18% shorter length of stay, implying room for improvement in the discharge process.45
Our findings have to be interpreted within the frame-work of the study design.5 Given the low illness severity of the study population, power to detect clinical predictors of discharge or effects on postdischarge resource consumption may have been insufficient.
The primary results of this study are strengthened by their face validity. We know from clinical experience that when unit workload is low, there is less incentive to discharge, and when unit census is high, there is pressure to decompress and make room for new admissions. We hypothesize that improvements in operations management, including clear discharge guidelines, case management, primary nursing, and improved communication procedures for patient handoffs, may improve overall workflow and efficiency of patient discharge. Future research should aim to reproduce these findings in different settings, as well as evaluate the safety and cost-effectiveness of changes in discharge processes, including their effect on postdischarge resource use.
Acknowledgments
This project was supported by Agency for Healthcare Research and Quality grants T32 HS 000063 (to Dr Profit) and R01 HS 10131 (to Dr Richardson).
We thank Dr Laura Petersen, Director of the Baylor College of Medicine's Division of Health Policy and Quality, at the Houston Center for Quality of Care and Utilization Studies, for reviewing the article. We also acknowledge our patients, their parents, the medical staff at participating NICUs, and the entire MPIP research team. Finally, Dr Profit thanks his mentors at the Harvard Pediatric Health Services Research Fellowship: Drs Tracy Lieu, Sharon Muret-Wagstaff, Donald Goldmann, James Perrin, and Jonathan Finkelstein.
Abbreviations
- MPIP
Moderately Premature Infant Project
- PNR
patient/nurse ratio
- SNAP II
Score for Neonatal Acute Physiology II
- SDR
standardized discharge ratio
- OR
odds ratio
- CI
confidence interval
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Owens PL, Thompson J, Elixhauser A, Ryan K. Care of Children and Adolescents in US Hospitals. Rockville, MD: Agency for Healthcare Research and Quality; 2003. [Google Scholar]
- 2.Zupancic JA, Richardson DK. Characterization of the triage process in neonatal intensive care. Pediatrics. 1998;102:1432–1436. doi: 10.1542/peds.102.6.1432. [DOI] [PubMed] [Google Scholar]
- 3.Kramer MS, Demissie K, Yang H, et al. The contribution of mild and moderate preterm birth to infant mortality. JAMA. 2000;284:843–849. doi: 10.1001/jama.284.7.843. [DOI] [PubMed] [Google Scholar]
- 4.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 5.Escobar GJ, McCormick MC, Zupancic JAF, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91:F238–F244. doi: 10.1136/adc.2005.087031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Escobar GJ, Fischer A, Kremers R, Usatin MS, Macedo AM, Gardner MN. Rapid retrieval of neonatal outcomes data: the Kaiser Permanente Neonatal Minimum Data Set. Qual Manag Health Care. 1997;5:19–33. [PubMed] [Google Scholar]
- 7.Brodie SB, Sands KE, Gray JE, et al. Occurrence of nosocomial bloodstream infections in six neonatal intensive care units. Pediatr Infect Dis J. 2000;19:56–65. doi: 10.1097/00006454-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK. Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol. 2001;21:272–278. doi: 10.1038/sj.jp.7210563. [DOI] [PubMed] [Google Scholar]
- 9.Eichenwald EC, Blackwell M, Lloyd JS, Tran T, Wilker RE, Richardson DK. Inter-neonatal intensive care unit variation in discharge timing: influence of apnea and feeding management. Pediatrics. 2001;108:928–933. doi: 10.1542/peds.108.4.928. [DOI] [PubMed] [Google Scholar]
- 10.Gould JB, Qin C, Marks AR, Chavez G. Neonatal mortality in weekend vs weekday births. JAMA. 2003;289:2958–2962. doi: 10.1001/jama.289.22.2958. [DOI] [PubMed] [Google Scholar]
- 11.Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356:185–189. doi: 10.1016/s0140-6736(00)02478-8. [DOI] [PubMed] [Google Scholar]
- 12.Touch SM, Greenspan JS, Kornhauser MS, O'Connor JP, Nash DB, Spitzer AR. The timing of neonatal discharge: an example of unwarranted variation? Pediatrics. 2001;107:73–77. doi: 10.1542/peds.107.1.73. [DOI] [PubMed] [Google Scholar]
- 13.Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100. doi: 10.1067/mpd.2001.109608. [DOI] [PubMed] [Google Scholar]
- 14.Gray JE, Safran C, Davis RB, et al. Baby CareLink: using the internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000;106:1318–1324. doi: 10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- 15.McCormick MC, Shapiro S, Starfield BH. The regionalization of perinatal services. Summary of the evaluation of a national demonstration program. JAMA. 1985;253:799–804. [PubMed] [Google Scholar]
- 16.Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review. Health Technol Assess. 1999;3:33–46. [PubMed] [Google Scholar]
- 17.Numata Y, Schulzer M, van der WR, et al. Nurse staffing levels and hospital mortality in critical care settings: literature review and meta-analysis. J Adv Nurs. 2006;55:435–448. doi: 10.1111/j.1365-2648.2006.03941.x. [DOI] [PubMed] [Google Scholar]
- 18.Horbar JD, Badger GJ, Lewit EM, Rogowski J, Shiono PH. Hospital and patient characteristics associated with variation in 28-day mortality rates for very low birth weight infants. Vermont Oxford Network. Pediatrics. 1997;99:149–156. doi: 10.1542/peds.99.2.149. [DOI] [PubMed] [Google Scholar]
- 19.Ringer SA, Richardson DK, Sacher RA, Keszler M, Churchill WH. Variations in transfusion practice in neonatal intensive care. Pediatrics. 1998;101:194–200. doi: 10.1542/peds.101.2.194. [DOI] [PubMed] [Google Scholar]
- 20.Richardson DK, Shah BL, Frantz ID, 3, Bednarek F, Rubin LP, McCormick MC. Perinatal risk and severity of illness in newborns at 6 neonatal intensive care units. Am J Public Health. 1999;89:511–516. doi: 10.2105/ajph.89.4.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walsh-Sukys MC, Tyson JE, Wright LL, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics. 2000;105:14–20. doi: 10.1542/peds.105.1.14. [DOI] [PubMed] [Google Scholar]
- 22.Olsen IE, Richardson DK, Schmid CH, Ausman LM, Dwyer JT. Intersite differences in weight growth velocity of extremely premature infants. Pediatrics. 2002;110:1125–1132. doi: 10.1542/peds.110.6.1125. [DOI] [PubMed] [Google Scholar]
- 23.Zupancic JA, Richardson DK, O'Brien BJ, Eichenwald EC, Weinstein MC. Cost-effectiveness analysis of predischarge monitoring for apnea of prematurity. Pediatrics. 2003;111:146–152. doi: 10.1542/peds.111.1.146. [DOI] [PubMed] [Google Scholar]
- 24.Eichenwald EC, Escobar GJ, Zupancic JA, Greene JD, McCormick MC, Richardson DK. Inter-NICU variation in discharge timing of moderately premature infants: earlier discharge does not affect outcome. Pediatr Res. 2004;55:372A. [Google Scholar]
- 25.Tarnow-Mordi W, Parry G. The CRIB score. Lancet. 1993;342:1365. doi: 10.1016/0140-6736(93)92276-y. [DOI] [PubMed] [Google Scholar]
- 26.Heller G, Misselwitz B, Schmidt S. Early neonatal mortality, asphyxia related deaths, and timing of low risk births in Hesse, Germany, 1990–8: observational study. BMJ. 2000;321:274–275. doi: 10.1136/bmj.321.7256.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 28.Tucker J. Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet. 2002;359:99–107. doi: 10.1016/s0140-6736(02)07366-x. [DOI] [PubMed] [Google Scholar]
- 29.Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollack MM, Koch MA. Association of outcomes with organizational characteristics of neonatal intensive care units. Crit Care Med. 2003;31:1620–1629. doi: 10.1097/01.CCM.0000063302.76602.86. [DOI] [PubMed] [Google Scholar]
- 31.Arias Y, Taylor DS, Marcin JP. Association between evening admissions and higher mortality rates in the pediatric intensive care unit. Pediatrics. 2004;113:530–534. doi: 10.1542/peds.113.6.e530. [DOI] [PubMed] [Google Scholar]
- 32.Pronovost PJ, Dang D, Dorman T, Lipsett PA, Garrett E, Jenckes M, et al. Intensive care unit nurse staffing and the risk for complications after abdominal aortic surgery. Eff Clin Pract. 2001;4:199–206. [PubMed] [Google Scholar]
- 33.Dimick JB, Pronovost PJ, Heitmiller RF, Lipsett PA. Intensive care unit physician staffing is associated with decreased length of stay, hospital cost, and complications after esophageal resection. Crit Care Med. 2001;29:753–758. doi: 10.1097/00003246-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Amaravadi RK, Dimick JB, Pronovost PJ, Lipsett PA. ICU nurse-to-patient ratio is associated with complications and resource use after esophagectomy. Intensive Care Med. 2000;26:1857–1862. doi: 10.1007/s001340000720. [DOI] [PubMed] [Google Scholar]
- 35.Ruttimann UE, Pollack MM. Variability in duration of stay in pediatric intensive care units: a multi-institutional study. J Pediatr. 1996;128:35–44. doi: 10.1016/s0022-3476(96)70425-0. [DOI] [PubMed] [Google Scholar]
- 36.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 37.Higgins TL, McGee WT, Steingrub JS, Rapoport J, Lemeshow S, Teres D. Early indicators of prolonged intensive care unit stay: impact of illness severity, physician staffing, and pre-intensive care unit length of stay. Crit Care Med. 2003;31:45–51. doi: 10.1097/00003246-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Ulrich CM, Wallen G, Grady C, et al. The nursing shortage and the quality of care. N Engl J Med. 2002;347:1118–1119. doi: 10.1056/NEJM200210033471419. [DOI] [PubMed] [Google Scholar]
- 39.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 40.Thompson DG, Maringer M. Using case management to improve care delivery in the NICU. MCN Am J Matern Child Nurs. 1995;20:257–260. [PubMed] [Google Scholar]
- 41.Spinner SS, Girifalco RB, Gibson E, Stavis RL, Greenspan JS, Spitzer AR. Earlier discharge of infants from neonatal intensive care units: a pilot. Clin Pediatr (Phila) 1998;37:353–357. doi: 10.1177/000992289803700604. [DOI] [PubMed] [Google Scholar]
- 42.McGettigan BA, Zebrowitz J. Triumph and tragedy: using physicians to impact length of stay, part I. Lippincotts Case Manag. 2004;9:163–165. doi: 10.1097/00129234-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 43.McGettigan BA, Zebrowitz J. Triumph and tragedy: implementing a physician-focused program to impact length of stay, part II. Lippincotts Case Manag. 2004;9:213–215. doi: 10.1097/00129234-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 44.White KR, Bazzoli GJ, Roggenkamp SD, Gu T. Does case management matter as a hospital cost-control strategy? Health Care Manage Rev. 2005;30:32–43. doi: 10.1097/00004010-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Profit J, Zupancic JAF, McCormick MC, et al. Moderately premature infants at Kaiser Permanente Medical Care Program in California are discharged home earlier than their peers in Massachusetts and the United Kingdom. Arch Dis Child Fetal Neonatal Ed. 2006;91:F245–F250. doi: 10.1136/adc.2005.075093. [DOI] [PMC free article] [PubMed] [Google Scholar]


