Abstract
Objectives
We investigated the impact of recruitment bias within the venue-based sampling (VBS) method, which is widely used to estimate disease prevalence and risk factors among groups, such as men who have sex with men (MSM), that congregate at social venues.
Methods
In a 2008 VBS study of 479 MSM in New York City, we calculated venue-specific approach rates (MSM approached/MSM counted) and response rates (MSM interviewed/MSM approached), and then compared crude estimates of HIV risk factors and seroprevalence with estimates weighted to address the lower selection probabilities of MSM who attend social venues infrequently or were recruited at high-volume venues.
Results
Our approach rates were lowest at dance clubs, gay pride events, and public sex strolls, where venue volumes were highest; response rates ranged from 39% at gay pride events to 95% at community-based organizations. Sixty-seven percent of respondents attended MSM-oriented social venues at least weekly, and 21% attended such events once a month or less often in the past year. In estimates adjusted for these variations, the prevalence of several past-year risk factors (e.g., unprotected anal intercourse with casual/exchange partners, ≥5 total partners, group sex encounters, at least weekly binge drinking, and hard-drug use) was significantly lower compared with crude estimates. Adjusted HIV prevalence was lower than unadjusted prevalence (15% vs. 18%), but not significantly.
Conclusions
Not adjusting VBS data for recruitment biases could overestimate HIV risk and prevalence when the selection probability is greater for higher-risk MSM. While further examination of recruitment-adjustment methods for VBS data is needed, presentation of both unadjusted and adjusted estimates is currently indicated.
Venue-based sampling (VBS), also called time-location or time-space sampling, is a study design that is widely used to provide estimates of risk factors and disease outcomes.1 Although it can be used to study any target population that congregates at known venues associated with the population,2 it has been primarily used for behavioral research of groups at risk for human immunodeficiency virus (HIV) or sexually transmitted diseases, such as men who have sex with men (MSM) and drug users.3 Because these populations are often “hidden” from probabilistic sampling (i.e., a population sampling frame cannot be constructed),4 using traditional probability designs may be inefficient or infeasible.5
Several variations of VBS exist, but all introduce elements of randomness in recruitment that improve upon convenience sampling. In the Young Men's Survey of MSM in seven U.S. cities, for example, a universe of MSM-oriented venues was created, venues were randomly selected, and presumed MSM entering a selected venue were non-preferentially approached to participate.6 Sampling efficiency is a chief strength of VBS, as selected recruitment venues contain a high density of the target population. But a corresponding weakness is that the group able to be sampled (e.g., MSM who visit MSM-oriented social venues) may be different from the larger target population (e.g., all sexually active MSM). VBS-based estimates are not generalizable to that larger population when the venue-attending subpopulation exhibits differential characteristics.7 Nonetheless, VBS data are often useful in designing outreach-based HIV prevention programs because the venue-attending subpopulation is inherently accessible.8
Increasing the validity of VBS-based estimates for that subpopulation, however, is a persistent goal. Statistical adjustment of VBS data may be used to correct unequal selection probabilities arising from at least two VBS recruitment biases. First, someone who attends venues frequently is more likely to be sampled than someone who attends venues infrequently. If outcome variables such as partner number or alcohol consumption are also related to attendance frequency, then unweighted data will overestimate population prevalence of these variables. Second, individual selection probability is inversely related to the volume of the target population at each recruitment venue. For example, MSM at low-volume bars have higher selection probabilities than MSM at high-volume gay pride events. Not accounting for these variations may bias estimates if outcome variables are associated with recruitment venue characteristics. Ideally, venue volume would be accounted for a priori in a study design such as probability-proportional-to-size (PPS) sampling, which adjusts second-stage (i.e., participant) selection probability by the size of a first-stage sampling unit.9 But PPS requires precise volume enumeration before recruitment, which is often infeasible for social venues. Post hoc statistical adjustment is an alternative approach. True selection probability will always be unknown in the VBS design because the population sampling frame is undefined, but adjustment for the two aforementioned biases may serve as an appropriate proxy in the absence of that gold standard.
While several studies have compared VBS estimates with those using another study design,10 few VBS-based studies have used statistical adjustment for weighted analyses. Adjustment methods were developed for the Young Men's Survey, but study analyses have only used unweighted data because weighting did not influence HIV prevalence estimates.11 Other VBS studies have presented data weighted to account for differences in venue volume but not attendance frequency.12 To our knowledge, no VBS studies have reported comparisons of unweighted and weighted estimates of the same data. In this study, we examined the impact of adjustment for the two previously mentioned recruitment biases and compared weighted and unweighted prevalence estimates of HIV risk factors and seroprevalence in a VBS-based sample of MSM.
METHODS
Venue sampling
We based this analysis on data collected in the National HIV Behavioral Surveillance (NHBS) study among MSM in New York City (NYC) during 2008. The methods for first-stage venue sampling and second-stage participant sampling have been described in detail elsewhere.13 Briefly, ethnographers constructed a universe of all MSM-oriented social venues in NYC by reviewing publications, interviewing key informants, and conducting ethnographic research. Potential venues were included in the universe if at least 75% of the population at the venue were adult MSM, as determined through ethnography and brief street interviews. Venues included commercial establishments (e.g., bars and clubs), as well as parks, public sex strolls, hookup spots, high-density street intersections, and house ball events.14 Each venue's peak hours of operation in standardized four-hour time periods were also determined through this process. Venue and time information was entered into randomizing software that selected venues and corresponding time periods for recruitment events. After placing venues-time period blocks onto a monthly recruitment calendar in the order of their selection, the field team conducted 12–15 recruitment events per month for five months.
Participant sampling
Field staff operated in a mobile van outside each venue during each recruitment event. All adult-appearing men who entered the venue were counted. Counted men were sequentially and non-preferentially approached by interviewers to briefly describe the study. Men interested in the study were then screened for eligibility; all eligible men participated. Participants were asked to take a survey administered privately by trained interviewers as well as an HIV test, although they could elect to take the survey only. All recruitment events were standardized to last four hours or to complete 20 eligible interviews, whichever occurred first.
Study eligibility criteria were male gender, adulthood, NYC residence, and English/Spanish comprehension. MSM sexual history was not a criterion, as some men may have been reluctant to disclose this information before informed consent. For this analysis, we removed men with no past-year MSM sexual history and those who self-reported as HIV-positive, as awareness of HIV infection influences risk behavior.15 We obtained informed consent for the study. All study procedures were approved by the Institutional Review Boards of the participating institutions.
Measures
Recruitment venues were classified into seven categories: bars, dance clubs, parks, community-based organizations (CBOs), house ball events, sex strolls/environments, and gay pride or related events. Participants were asked about sociodemographics, HIV risk factors, and encounters with HIV prevention services. In this analysis, we report on race/ethnicity, age, sexual identity, sociodemographics (e.g., birthplace, homelessness, and income level), and past-year MSM behavioral risks (e.g., any unprotected anal intercourse [UAI], UAI with a casual/exchange partner, ≥5 total partners, any partners met through the Internet, group sex encounters, weekly binge drinking, and any hard-drug [non-marijuana] use). Oral fluid was collected and tested for HIV antibodies on OraQuick platforms (OraSure Technologies, Inc., Bethlehem, Pennsylvania). Reactive OraQuick tests were confirmed with OraSure test kits on western blot platforms.
Weighting and analysis
We compared unweighted prevalence estimates with estimates weighted with two individual weights (a response weight and an attendance weight) and a composite weight (the product of the two). We constructed the response weight, similar to previous approaches,12 from the approach and response rates for each recruitment event. We then calculated an approach rate by dividing the number of men approached (MSMa) by the number of men counted entering the venue (MSMc). We calculated a response rate by dividing the number of men interviewed (MSMI) by the number of men approached (MSMa). The overall approximated recruitment probability of a man at any recruitment event was the product of the approach and response rates (MSMI/MSMc). Thus, the response weight (Wr) was the reciprocal of recruitment probability:
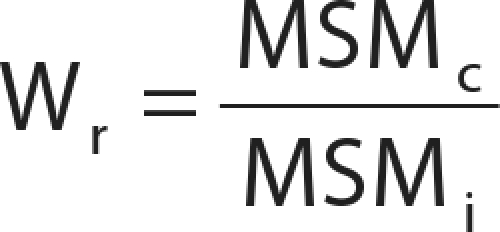 |
We calculated different response weights for HIV infection estimates by replacing the value for MSMI with the number of men who had an HIV test (MSMT), as this was an optional component of the study and the testing rate was lower than the interview rate.
We constructed the attendance weight, similar to previous approaches,16 from participants' reported frequency of attending MSM-oriented social venues, as determined through this survey question: “In the past 12 months, how often have you gone to a place where gay men hang out, meet, or socialize? These could include bars, clubs, social organizations, parks, gay businesses, bookstores, or sex clubs.” The response options were once a day, more than once a week, once a week, more than once a month, once a month, or less than once a month. We constructed the attendance weight (Wa) by setting the “once a day” response as the reference weight (value = 1) and then assigning relative values for the other frequency options based on temporal comparisons with that reference. MSM who visited venues once a week, for example, had a relative selection probability of 1/7; thus, their attendance weight was its reciprocal, 7. We used the numerical midpoint for response options between two defined time frames as an approximation. Therefore, Wa for each response option was defined as follows: 1 (once a day), 3.5 (more than once a week), 7 (once a week), 15 (more than once a month), 30 (once a month), and 60 (less than once a month). The composite weight (Wc) simultaneously adjusted for the unequal selection probability created by response and attendance biases. It was the product of the two individual weights:
 |
For prevalence estimation, we calculated unweighted point estimates and 95% confidence intervals (CIs) for all measures, estimates weighted separately with Wr and Wa, and then estimates weighted with Wc. For all weighted analyses, we used procedures for complex survey data in SAS® version 9.117 and R software version 2.12.18 For analyses weighted with Wr and Wc, unique recruitment events were treated as dependent clusters and intracluster correlation was controlled for when calculating standard errors.
To determine statistically significant differences between the unweighted and Wc weighted estimates, we used bootstrap resampling in the Boot Package in R.19 We calculated standard errors of the difference in estimates with 10,000 bootstrap resamples. We considered exponentiated 95% CIs of the difference not crossing 1.0 to be evidence of significant differences between unweighted and Wc weighted estimates (at α=0.05).
RESULTS
Across 59 recruitment events, 568 adult men completed the NHBS interview. Of these, 18 were removed from this analysis because they had no recent MSM sexual history, and 71 were removed because they self-reported as HIV-positive. Of the remaining 479 MSM, 395 (82%) had an HIV test as part of the study.
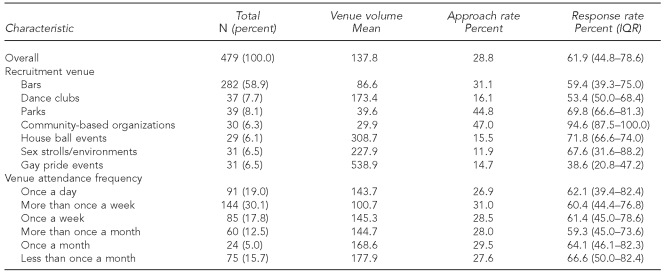
As shown in Table 1, most MSM were recruited from bars (59%), followed by parks (8%), dance clubs (8%), public sex strolls (7%), gay pride events (7%), CBOs (6%), and house ball events (6%). The mean venue volumes ranged from 29.9 enumerated men at CBOs to 538.9 enumerated men at gay pride events, with an overall mean of 137.8. The overall mean approach rate (29%) was inversely related to venue volume: rates were highest at CBOs (47%) and lowest at sex strolls (12%) and gay pride events (15%). The overall mean response rate was 62%, with the lowest rate at gay pride events (39%) and the highest rate at CBOs (95%). Two-thirds of men (67%) attended social venues at least weekly: 19% attended once a day, 30% attended more than once a week, and 18% attended weekly. The remaining 33% attended venues less than weekly, with 13% attending more than once a month, 5% attending once a month, and 16% attending less than once a month. There were small variations in venue volumes (100.7–177.9), approach rates (27%–31%), and response rates (59%–67%) by attendance frequency, suggesting independence of weighting components.
Table 1.
Recruitment venues and venue attendance among men who have sex with men: New York City, 2008 (n=479)
IQR = interquartile range
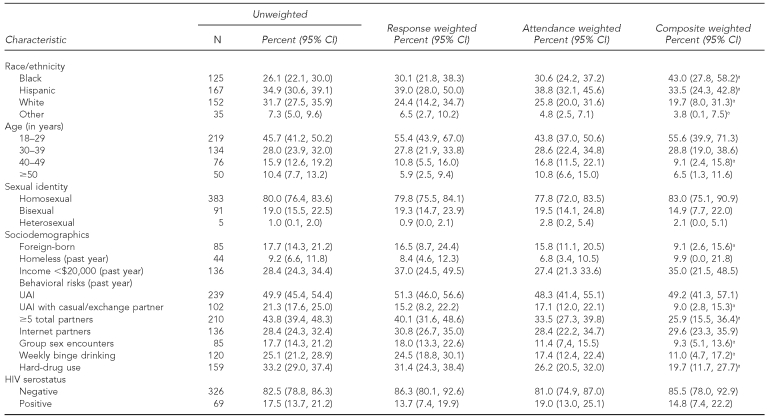
Table 2 presents the unweighted estimates, two individually weighted estimates, and the composite estimates. Using composite weighted estimates, 43% of respondents were black, 34% were Hispanic, 20% were white, and 4% were from another race/ethnicity. All weighted estimates for black MSM were significantly higher than for white MSM and MSM of other races/ethnicities. By age group, 56% were aged 18–29 years, 29% were aged 30–39 years, 9% were aged 40–49 years, and 7% were 50 years of age or older. Estimates for MSM aged 40–49 years were significantly lower in the weighted analysis. By sexual identity, 83% considered themselves homosexual, 15% bisexual, and 2% heterosexual. Nine percent were foreign-born, 10% were homeless, and 35% reported an annual income of <$20,000. Weighted estimates for foreign-born MSM were significantly lower than unweighted estimates.
Table 2.
Comparison of unweighted and weighted HIV prevalence and HIV risk factors for men who have sex with men who self-report HIV-negative: New York City, 2008 (total n=479; HIV tested n=395)
aComposite weighted estimates significantly different from unweighted estimates at α=0.05
HIV = human immunodeficiency virus
CI = confidence interval
UAI = unprotected anal intercourse
Forty-nine percent of respondents had UAI, 9% had UAI with a casual or exchange partner, 26% had ≥5 total partners, 30% had partners they met over the Internet, 9% had group sex encounters, 11% engaged in weekly binge drinking, and 20% used any hard drugs within the past year. Weighted estimates for UAI with a casual/exchange partner, ≥5 total partners, group sex encounters, binge drinking, and hard-drug use were significantly lower than unweighted estimates. The unweighted estimate of undiagnosed HIV infection was 18%. The composite-weighted estimate was lower (15%) than the unweighted estimate, but not significantly.
DISCUSSION
In our study of sexually active MSM in NYC who attended MSM-oriented venues, we found high levels of HIV risk and HIV infection. However, two recruitment biases in the VBS study design, relating to variations in venue volume and attendance frequency, influenced several of these estimates. After adjustment, key risk factors were significantly lower; HIV prevalence was also lower, but not significantly so.
Weighting components
Our composite weighting mechanism reflected two components that may approximate a participant's selection probability at venues where the VBS study was conducted: the recruitment rates at each venue and the reported attendance frequency at all social venues.12,16 The recruitment rate was a product of both approach and response rates. Because the size of the study team did not change according to volume, the approach rate was inversely associated with volume. Accurate counts of unique individuals at venues were necessary to record volume and determine approach rates.13 Varying response rates may have reflected differences in the characteristics of the venues and their attendees, as rates were higher at CBOs and house ball events (where buy-in of HIV research may be stronger)14 and lower at gay pride events (where individuals may not have had adequate time to take a survey).20 This bias can potentially be mitigated through the statistical adjustment we proposed.
The wide variance in attendance frequency, with one quintile visiting MSM-oriented social venues daily and another quintile visiting social venues once a month or less often, also created unequal selection probabilities. Examining these variations is particularly important in VBS designs, as many social venues used in this study design (e.g., bars) influenced or reflected characteristics under study (e.g., binge drinking). Higher attendance frequency at some venues may have increased both behavioral risk and selection probability, which has the effect of overestimating the former.
Influence of bias on prevalence estimates
We found several differences between unweighted and composite-weighted estimates. Unweighted estimates for UAI with a casual/exchange partner, ≥5 total partners, group sex encounters, frequent binge drinking, and hard-drug use were all significantly higher than composite weighted estimates. Differential recruitment rates and venue attendance frequencies were both plausible biases. The highest recruitment rates were at CBOs (45%), parks (31%), and bars (18%), where we also observed higher-than-average levels of risk. This finding may reflect selection bias (e.g., higher-risk MSM at CBOs being more willing to participate in research studies) or differences in venue patron characteristics (e.g., MSM at parks and bars being more likely to meet sexual partners). In contrast, the lowest recruitment rate was at gay pride events, which may reflect a broader, less risky cross-section of MSM. Because the recruitment rate was inversely related to the response weight, men at less risky venues would receive more weight, which is one reason for the lower estimates.
Variations in attendance frequency may also have biased estimates: MSM who attend social venues more frequently are more likely to be sampled, but also may have increased opportunities to engage in sexual risk behaviors, as we found. The lower rates of binge drinking and hard-drug use after adjustment may reflect the association between the frequency of attending bars and the frequency of drinking and using hard drugs.21,22 Moreover, because alcohol and hard-drug use is tied to sexual risk,23,24 the higher levels of sexual risk in unweighted estimates may reflect the higher levels of alcohol and hard-drug use among frequent venue attendees (who are down-weighted). We also found that estimates for low-income MSM were higher (though not significantly) after weighting, which may indicate that higher-income MSM have more monetary opportunities to attend venues. Weighted estimates of HIV prevalence were lower, but not significantly. Although we only examined undiagnosed infections, the time frame of infection was unknown, so the adjustment components may not overlap in time with this outcome.
Comparisons with previous VBS research
Some VBS studies have used response weighting methods to present estimates adjusted for varying recruitment rates.12 Others have developed attendance weighting methods,6 but decided against using them because weighting did not influence HIV prevalence estimates.11,25 It was unstated whether weighting -influenced estimates of other variables, but subsequent methods developed to refine attendance weights showed some effect.16 We replicated that general approach in this study to create attendance weights, but also included the response weight component. To our knowledge, no weighting mechanisms that simultaneously adjust for both response and attendance biases have been explored.
Moreover, despite the widespread use of VBS, few studies have evaluated the effects of VBS recruitment biases inherent in the design. One compared the demographic and risk differences between a VBS study and an online survey of MSM,26 another compared a VBS study and a random-digit-dial telephone survey of MSM,10 and others have examined the potential implications of VBS recruitment among participants of that same telephone survey.7,27 More direct comparisons of unweighted and weighted VBS data, as well as developments on VBS adjustment techniques, are greatly needed to understand the outcomes of this popular study design.
Limitations
The goal of this analysis was to provide a weighting mechanism that adjusts for common recruitment biases in VBS designs and to show the impact of such a mechanism on VBS-collected data. However, this weighting approach did not necessarily increase the validity of the estimates, and the adjusted estimates were not necessarily representative of all sexually active MSM in NYC nor of the subset of MSM who attend MSM-oriented social venues. In any study or evaluation of VBS, it would be very difficult (and probably impossible) to know with certainty each participant's true selection probability—the gold standard—because the underlying sampling frame of eligible men is unknown. We used proxy measures for two components of an individual's selection probability, but the relationship between these proxies and the gold standard could not be estimated in the current study.
A key assumption in the use of these proxy measures is that the measured venue attendance frequency represents the relative selection probabilities of the target population at the specific recruitment venues selected for the study. Ideally, we would know the specific attendance patterns of all participants at all venues during the dates of data collection.6 This knowledge would show nonuniform patterns of attendance clustered in time (e.g., weekends only) or location (e.g., bars only). However, obtaining this information would be nearly impossible because of issues of recall, time constraints during the interview, and the changing characteristics of venues and the participants' attendance at them. For now, further evaluation of this question and its approximation of the gold standard is needed.
Some notable demographic differences in our weighted estimates require further exploration. The higher levels of black MSM after adjustment reflect their lower selection probabilities within the study, but these estimates also are likely not representative of NYC MSM. One limitation of this analytic approach was that the response weighting assumes that men counted at one venue are not counted again at other venues, while the enumeration and corresponding adjustment pertains to the venue visit rather than the venue visitor.13 However, participants could enter the study only once (verified in the eligibility screener and by field team observations), and the response weight was unique for the participant's recruitment event. Further, the size of the MSM population in NYC may have reduced the chances of repeated enumeration of the same men across venues. A related limitation was that the boundaries of some venues are distinct and small (e.g., bars) while the boundaries of others are amorphous and large (e.g., gay pride events). Because of this disparity, the relative venue volume may not have been accurately estimated for the latter type of events.
Finally, the representativeness of these estimates was a function of the comprehensiveness of the venue universe. If some venues were not included on the universe (e.g., exclusive sex parties), then estimates were not representative of MSM who attended only those venues we failed to include.
CONCLUSIONS
When evaluating the validity of VBS-based estimates, it is important to remember that there is often no probability-based study design for estimating behavioral risks and disease outcomes for high-risk populations.1 Although some probabilistic methods have been used to estimate HIV prevalence and risk among MSM,28 they are often limited in their depth and efficiency, and may not capture members of the target population that are hidden from probabilistic sampling.5 VBS estimates, even the weighted estimates provided in this study, do not necessarily apply to MSM who never attend MSM-oriented social venues. However, the venue-attending subpopulation is inherently accessible for targeted HIV prevention activities (e.g., condom distribution and HIV counseling and testing) located at these venues. In fact, unweighted estimates could better reflect the characteristics of these targeted MSM, as outreach programs may share the same recruitment biases as our VBS studies.
VBS and other quasi-probability study designs, including respondent-driven sampling,29 that are used to sample hidden populations feature elements of randomness that increase external validity compared with convenience sampling. But there are persistent biases within these methods that necessitate statistical adjustment. Our goal was to examine a method for adjustment and to demonstrate its influence on estimates of HIV risk and seroprevalence in a VBS sample of MSM. We found that not adjusting VBS data for inherent recruitment biases could overestimate HIV risk factors and prevalence, as the selection probability may be greater for higher-risk MSM. Further methodological research on adjusting VBS data is needed, in part to investigate the accuracy and relevance of the response and attendance weights. In the interim, recruitment statistics (venue types, attendance frequency, and recruitment rates) should be reported in all VBS studies to evaluate any VBS-related bias.
Footnotes
This research was funded by a cooperative agreement between the New York City Department of Health and Mental Hygiene (NYC DOHMH) and the Centers for Disease Control and Prevention (CDC) (grant #U62/CCU223595-03-1). The authors acknowledge Elizabeth DiNenno, Amy Drake, Amy Lansky, and Isa Miles of CDC for their contributions to the National HIV Behavioral Surveillance (NHBS) study design; Colin Shepard and James Sarn of the NYC DOHMH for reviewing previous drafts of this article; Charles Cleland of New York University for statistical guidance; and the NYC NHBS field staff for all their efforts.
REFERENCES
- 1.Muhib FB, Lin LS, Stueve A, Miller RL, Ford WL, Johnson WD, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–22. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitchell MK, Gregersen PK, Johnson S, Parsons R, Vlahov D. The New York Cancer Project: rationale, organization, design, and baseline characteristics. J Urban Health. 2004;81:301–10. doi: 10.1093/jurban/jth116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothenberg R, Dan My Hoang T, Muth SQ, Crosby R. The Atlanta Urban Adolescent Network Study: a network view of STD prevalence. Sex Transm Dis. 2007;34:525–31. doi: 10.1097/01.olq.0000258132.06764.a1. [DOI] [PubMed] [Google Scholar]
- 4.Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–72. doi: 10.1097/01.aids.0000172879.20628.e1. [DOI] [PubMed] [Google Scholar]
- 5.Lansky A, MacKellar D, Gallagher KM, Lin LS, Sullivan PS, Onorato IM. Evaluation of the new National HIV Behavioral Surveillance System (NHBS) is imperative. Sex Transm Dis. 2006;33:272–3. doi: 10.1097/01.olq.0000215745.61542.d4. [DOI] [PubMed] [Google Scholar]
- 6.MacKellar D, Valleroy L, Karon J, Lemp G, Janssen R. The Young Men's Survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep. 1996;111(Suppl 1):138–44. [PMC free article] [PubMed] [Google Scholar]
- 7.Xia Q, Tholandi M, Osmond DH, Pollack LM, Zhou W, Ruiz JD, et al. The effect of venue sampling on estimates of HIV prevalence and sexual risk behaviors in men who have sex with men. Sex Transm Dis. 2006;33:545–50. doi: 10.1097/01.olq.0000219866.84137.82. [DOI] [PubMed] [Google Scholar]
- 8.Ellen JM, Fichtenberg CM. Venue-based sampling in STD research: generalizeable to and independent of whom? Sex Transm Dis. 2007;34:532–3. doi: 10.1097/OLQ.0b013e318125660c. [DOI] [PubMed] [Google Scholar]
- 9.McNaghten AD, Wolfe MI, Onorato I, Nakashima AK, Valdiserri RO, Mokotoff E, et al. Improving the representativeness of behavioral and clinical surveillance for persons with HIV in the United States: the rationale for developing a population-based approach. PLoS One. 2007;2:e550. doi: 10.1371/journal.pone.0000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwarcz S, Spindler H, Scheer S, Valleroy L, Lansky A. Assessing representativeness of sampling methods for reaching men who have sex with men: a direct comparison of results obtained from convenience and probability samples. AIDS Behav. 2007;11:596–602. doi: 10.1007/s10461-007-9232-9. [DOI] [PubMed] [Google Scholar]
- 11.Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. Young Men's Survey Study Group. JAMA. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- 12.Ferreira LO, de Oliveira ES, Raymond HF, Chen SY, McFarland W. Use of time-location sampling for systematic behavioral surveillance of truck drivers in Brazil. AIDS Behav. 2008;12(4 Suppl):S32–8. doi: 10.1007/s10461-008-9386-0. [DOI] [PubMed] [Google Scholar]
- 13.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murrill CS, Liu KL, Guilin V, Colon ER, Dean L, Buckley LA, et al. HIV prevalence and associated risk behaviors in New York City's house ball community. Am J Public Health. 2008;98:1074–80. doi: 10.2105/AJPH.2006.108936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 16.Karon JM. Proceedings of the ASA Section on Survey Research Methods . 2005. The analysis of time-location sampling study data; pp. 3180–6. [Google Scholar]
- 17.SAS Institute, Inc. SAS®: Version 9.1. Cary (NC): SAS Institute, Inc.; 2007. [Google Scholar]
- 18.R Development Core Team. R: Version 2.12. Vienna (Austria): R Foundation for Statistical Computing; 2011. [Google Scholar]
- 19.Canty A, Ripley B. boot: Bootstrap R (S-Plus) Functions. R: Version 1.2-43. Vienna (Austria): R Foundation for Statistical Computing; 2010. [Google Scholar]
- 20.Rapid HIV testing among racial/ethnic minority men at gay pride events– nine U.S. cities, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(24):602–4. [PubMed] [Google Scholar]
- 21.Clapp JD, Reed MB, Min JW, Shillington AM, Croff JM, Holmes MR, et al. Blood alcohol concentrations among bar patrons: a multi-level study of drinking behavior [published erratum appears in Drug Alcohol Depend 2009;104:272-3] Drug Alcohol Depend. 2009;102:41–8. doi: 10.1016/j.drugalcdep.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curran PJ, Harford TC, Muthen BO. The relation between heavy alcohol use and bar patronage: a latent growth model. J Stud Alcohol. 1996;57:410–8. doi: 10.15288/jsa.1996.57.410. [DOI] [PubMed] [Google Scholar]
- 23.Morojele NK, Kachieng'a MA, Mokoko E, Nkoko MA, Parry CD, Nkowane AM, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med. 2006;62:217–27. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 24.Farley T, Olson C, Frazer MS, Kerker B. Alcohol use and risky sex in New York City. NYC Vital Signs. 2008;7:1–4. [Google Scholar]
- 25.Sifakis F, Hylton JB, Flynn C, Solomon L, Mackellar DA, Valleroy LA, et al. Racial disparities in HIV incidence among young men who have sex with men: the Baltimore Young Men's Survey. J Acquir Immune Defic Syndr. 2007;46:343–8. doi: 10.1097/QAI.0b013e31815724cc. [DOI] [PubMed] [Google Scholar]
- 26.Raymond HF, Rebchook G, Curotto A, Vaudrey J, Amsden M, Levine D, et al. Comparing Internet-based and venue-based methods to sample MSM in the San Francisco Bay area. AIDS Behav. 2010;14:218–24. doi: 10.1007/s10461-009-9521-6. [DOI] [PubMed] [Google Scholar]
- 27.Pollack LM, Osmond DH, Paul JP, Catania JA. Evaluation of the Centers for Disease Control and Prevention's HIV behavioral surveillance of men who have sex with men: sampling issues. Sex Transm Dis. 2005;32:581–9. doi: 10.1097/01.olq.0000175419.02839.d6. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen TQ, Gwynn RC, Kellerman SE, Begier E, Garg RK, Pfeiffer MR, et al. Population prevalence of reported and unreported HIV and related behaviors among the household adult population in New York City, 2004. AIDS. 2008;22:281–7. doi: 10.1097/QAD.0b013e3282f2ef58. [DOI] [PubMed] [Google Scholar]
- 29.Heckathorn DD. Extensions of respondent-driven sampling: analyzing continuous variables and controlling for differential recruitment. Sociol Methodol. 2007;37:151–207. [Google Scholar]