Abstract
Objective
We assessed changes in levels of support for smoke-free bars and restaurants among teens and young adults before and after implementation of a statewide smoke-free law.
Methods
We measured support for smoke-free bars and restaurants among teens and young adults aged 16–24 years living in Minnesota (n=2,785) and five comparison states (n=404), up to 12 months before and up to six months after Minnesota's smoke-free law went into effect in October 2007. We compared changes in support among three subgroups—Minnesota participants who lived with a previous local smoke-free law, Minnesota participants who did not live with a previous local smoke-free law, and participants from the comparison states—before and after Minnesota's statewide smoke-free law went into effect.
Results
Support for smoke-free restaurants and bars among participants in Minnesota and comparison states increased after Minnesota's smoke-free law went into effect. Minnesotans, both those living with and without a previous local smoke-free law, showed similar increases in support for smoke-free restaurants as participants in comparison states. However, Minnesotans living without a previous local law showed larger increases in support for smoke-free bars than both those in comparison states and those living in Minnesota with a previous local smoke-free law.
Conclusions
Our study employed a more robust design than similar studies and focused on the teen and young adult population. Our results will help advocates and policy makers demonstrate how public support for smoke-free laws increases following smoke-free legislation, particularly among those who were not previously living with a local smoke-free law.
Policies that create smoke-free worksites and other public places have been identified as effective measures for reducing environmental tobacco smoke (ETS) exposure1 and smoking rates.2,3 An increasing number of communities and states in the U.S. have enacted laws restricting smoking in public places, including restaurants and bars.4 ETS exposure in restaurant and bar settings is of particular concern because these settings have often been exempt from smoke-free laws in workplaces.5 Efforts to enact smoking restrictions in restaurants, and especially bars, often face strong opposition from the tobacco and hospitality industries;6 however, demonstrating strong public support for these laws can help counter this opposition. As more communities and states enact or consider enacting smoke-free laws in restaurants and bars, measuring levels of public support for these laws will be of increasing importance.
Numerous cross-sectional studies have been conducted to examine public support for smoke-free laws in bars and restaurants among the general adult population. Support varies considerably depending on jurisdiction, year of study, and type of establishment (e.g., restaurant vs. bar). Support for smoke-free laws in bars and restaurants is often greater among older adults, nonsmokers, and adults living in areas with smoke-free laws.7–10
Only a few studies have examined support for smoke-free laws at bars and/or restaurants among young adults specifically, all of which have used a cross-sectional design.11–15 It is particularly important to understand levels of support among the young adult population, not only because some studies have shown their support to be lower than older adults, but also because young adults are often employed in bars and restaurants16 and tend to frequent bars.17 Most previous studies have been limited to college students and only inquired about smoke-free laws on campus.12–15 One study, which used data from the same project as the current study, included a community sample of young adults and found that overall support for smoke-free laws in restaurants was 66% and in bars was 40%. The study also found that, as with the adult population, factors associated with increased support included being a nonsmoker and living with a local smoke-free law.11
Several studies have also assessed the relationship between implementation of smoke-free laws and support for the laws. Two studies conducted in California measured support for smoke-free bars among the general adult population at several time points after a statewide smoke-free law took effect.18,19 Both found that overall support for the law increased over time; however, neither study included a comparison group nor a measure of support prior to the legislation being implemented. In addition, Friis and Safer did not provide a statistical test of change in support across time points.18 The five other longitudinal studies were conducted outside the U.S., including the United Kingdom (UK),20–22 Australia,23 and New Zealand.24 All studies measured support among the general adult population both before and after smoke-free legislation was implemented; however, only the UK studies used comparison groups. All studies concluded that support for a smoke-free law increased after a law was implemented, and the studies that included comparison groups found that support increased more among people living with a law than among those living without a law.
We assessed changes in support for smoke-free laws in restaurants and bars before and after implementation of Minnesota's statewide smoke-free law in all workplaces, including bars and restaurants (effective October 1, 2007). For comparison, we included teens and young adults aged 16–24 years from Minnesota and from several other upper Midwest states that did not have statewide or local smoke-free laws. Additionally, we examined differences and changes in support by sociodemographic and personal characteristics. We hypothesized that (1) public support for both smoke-free bars and restaurants would increase following the Minnesota smoke-free law, mainly for those who lived without local smoke-free legislation; (2) support for smoke-free laws would remain stable across the study period in the comparison states; and (3) those who did not smoke would be more supportive of smoke-free laws, before and after the statewide law was implemented. Our results will help advocates and policy makers demonstrate how public support changes following smoke-free legislation.
METHODS
Overview of the cohort study
This study used data from the Minnesota Adolescent Community Cohort Study, which began in 2000. To establish the cohort, Minnesota was divided into 129 group-level units based on geographical and political units (GPUs) thought to reflect local tobacco-control environments. These GPUs were based on the following three criteria: (1) the boundaries of the units adhere to existing geographic and/or political limits, (2) the boundaries of the units reflect patterns of local tobacco program activities, and (3) a sufficient number of teens reside in each unit to meet the sample size requirements. The boundaries included counties, municipalities, school districts, urban neighborhoods, and local planning districts. Of the 129 GPUs, we selected a stratified random sample of 60 GPUs for this study, based on region of the state and distribution of race/ethnicity. Of the 60 GPUs selected, 28 were rural (47%), 21 were suburban (35%), three were small cities (5%), and eight were urban (13%).
We also established a cohort of young people from five other Midwestern states, including South Dakota, North Dakota, Michigan, Kansas, and Missouri. We chose these states based on two main criteria: (1) minimal tobacco prevention activities were expected in these states during the study period, and (2) the states were demographically/geographically similar to Minnesota. We divided the comparison cohort into five GPUs: (1) all of North Dakota (rural/small town), (2) all of South Dakota (rural/small town), (3) Upper Peninsula of Michigan (rural), (4) non-metro Kansas (rural), and (5) Kansas City, Missouri, and Wichita, Kansas (both urban/suburban).
We recruited an equal number of people aged 12–16 years for each year to participate from each GPU and each comparison state. We used a combination of probability and quota sampling methods to assure equal age distribution. Clearwater Research, Inc. (Boise, Idaho) conducted recruitment by telephone using modified random-digit-dial sampling. Our baseline response rate among eligible households was 58.5%. The baseline full cohort sample included young people living in Minnesota (n=3,636), as well as young people living in the comparison states (n=605). At the third round of data collection (2001), an additional sample of 584 12-year-olds was added, for a total sample of 4,825.
Participants were surveyed via telephone every six months from Round 1 (2000) through Round 15 (2008). Interviews took approximately 10–20 minutes to complete. Study participants received $10–$15 for each completed interview depending on age and survey round.
The University of Minnesota Institutional Review Board approved this study, and all participants provided informed consent to participate. Parental permission was obtained to conduct each interview if the participant was younger than 18 years of age.
Current sample and procedures
Participants for this study included teenagers and young adults aged 16–24 years living in Minnesota (n=2,785) and five comparison states (n=404). Participants were surveyed before Minnesota's statewide smoke-free law went into effect (between October 2006 and March 2007; survey Round 13) and once after the law went into effect (between October 2007 and March 2008; survey Round 15). The Minnesota statewide smoke-free law went into effect on October 1, 2007. Participants in the comparison states experienced no statewide or local smoke-free laws during the study period.
Measures
We measured our two main outcome variables, level of support for smoke-free bars and level of support for smoke-free restaurants, in two separate survey items: “In bars and clubs (or restaurants), do you think smoking should be allowed in all areas, some areas, or not at all?” Participants who reported that smoking should not be allowed “at all” were considered supportive of a smoke-free law.
Each model included four demographic and personal characteristics as covariates, including gender, age (<18 years vs. ≥18 years), past 30-day smoking (yes/no), and number of friends who smoke (none vs. ≥1). The sample was divided into three subgroups: (1) those living in Minnesota in an area with a local smoke-free law (in bars and restaurants) before the statewide law went into effect, (2) those living in Minnesota in an area without a local smoke-free law (in bars and restaurants) before the statewide law went into effect, and (3) those living in the comparison group (without statewide or local smoke-free laws). We excluded from analyses those living in areas with local smoke-free laws that had significant exemptions included in their ordinance (e.g., only certain hours when smoking was not allowed) (n=79).
Analyses
We computed overall support for smoke-free laws, and support by personal/sociodemographic characteristics and subgroup (i.e., previously living with a local smoke-free law, previously living without a local smoke-free law, and living in a comparison state), before and after the statewide smoke-free law went into effect. We examined changes in support before and after the statewide law, as well as the associations between those changes and each of the four covariates, controlling for the three subgroups (bivariate analyses). Covariates that were significantly associated with changes in support in bivariate analyses (p<0.05) were included in multivariate models. For our multivariate models, we compared changes in support for smoke-free laws across the subgroups, before and after Minnesota's statewide smoke-free law went into effect, adjusting for covariates. We conducted all analyses using SAS® version 9.1, using SAS PROC GLIMMIX for multivariate models.25
RESULTS
Bivariate analyses
Restaurants.
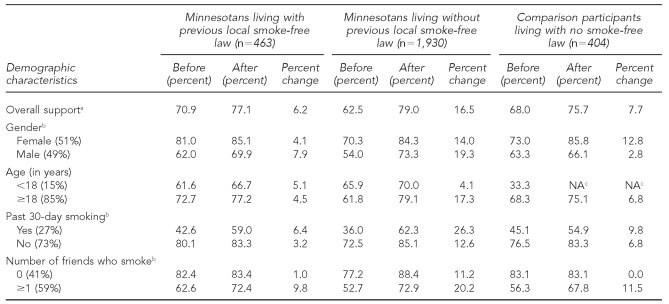
The proportion of participants who supported smoke-free restaurants before and after the statewide law, by subgroup and sociodemographic characteristics, is shown in Table 1. In general, females, older participants, nonsmokers (in the past 30 days), and those who did not have any close friends who smoked were more supportive of smoke-free restaurants, before and after the statewide law went into effect. Results showed that support for smoke-free restaurants among all three study groups increased after Minnesota's statewide smoke-free law was enacted. Minnesota participants living without a prior local law showed a greater increase in support for smoke-free restaurants than those living with a previous law (16.5% vs. 6.2%).
Table 1.
Support for smoke-free laws in restaurants before and after implementation of Minnesota's statewide smoke-free law in October 2007, by subgroup and sociodemographic characteristics
aPercentages in parentheses in first column are from baseline (Round 13) survey (October 2006–March 2007).
bChanges in support were significantly different across the three groups for the specified covariate (p<0.05).
cWe were unable to compute the change in support for those <18 years of age in the comparison group because there were no participants in our sample in this age group at Round 15 (i.e., the data collection period after the Minnesota smoke-free law took effect).
NA = not applicable
Across the three subgroups, three covariates—gender, past 30-day smoking, and number of friends who smoked—were significantly associated with change in support for smoke-free restaurants (females compared with males: degree of freedom [df] = 2, n=2,062, test statistic = 10.78, p<0.0001; past 30-day smokers compared with those who had not smoked in the last 30 days: df=2, n=2,022, test statistic = 20.45, p<0.0001; and participants with at least one close friend who smoked compared with those with no close friends who smoked: df=8, n=2,052, test statistic = 5.96, p<0.0001). Past 30-day smokers (compared with those who had not smoked in the last 30 days) and participants with at least one close friend who smoked (compared with those with no close friends who smoked) showed greater increases in support. The direction of the associations for gender was inconsistent across the three subgroups (data not shown).
Bars/clubs.
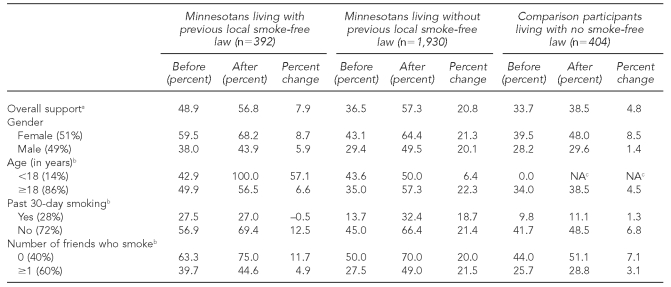
Table 2 details support for smoke-free bars/clubs before and after the statewide smoke-free legislation went into effect by the three subgroups and sociodemographic characteristics. Overall, there was more support for smoke-free restaurants than bars. As with restaurants, support for smoke-free policies in bars increased more for Minnesotans without a prior local law than for those already living with a local smoke-free law (20.8% vs. 7.9%). Across the three subgroups, three covariates—age, past 30-day smoking, and number of friends who smoked—were significantly associated with change in support for smoke-free bars (age ≥18 years compared with age <18 years: df=9, n=1,960, test statistic = 1.96, p=0.04; those who had not smoked in the last 30 days compared with past 30-day smokers: df=2, n=1,934, test statistic = 5.53, p=0.004; and participants with at least one close friend who smoked compared with those with no close friends who smoked: df=8, n=1,966, test statistic = 2.32, p=0.02). Those who had not smoked in the past 30 days showed greater increases in support than those who had smoked in the past 30 days. The direction of the associations for age and number of friends who smoked was inconsistent across the three subgroups.
Table 2.
Support for smoke-free laws in bars/clubs before and after implementation of Minnesota's statewide smoke-free law in October 2007, by subgroup and sociodemographic characteristics
aPercentages in parentheses in first column are from baseline (Round 13) survey (October 2006–March 2007).
bChanges in support were significantly different across the three groups for the specified covariate (p<0.05).
cWe were unable to compute the change in support for those <18 years of age in the comparison group because there were no participants in our sample in this age group at Round 15 (i.e., the data collection period after the Minnesota smoke-free law took effect).
NA = not applicable
Multivariate analyses
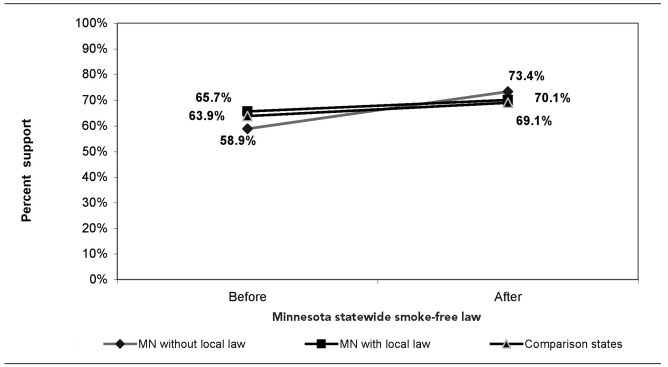
Figures 1 and 2 show the results of our multivariate analyses—the proportion of participants who supported smoke-free restaurants and bars, respectively, before and after Minnesota's statewide smoke-free law went into effect, and after controlling for the socio-demographic variables significant in bivariate analyses. For restaurants, changes in support did not differ for either of the Minnesota groups as compared with the comparison group, meaning that both those living with and without a previous local smoke-free law showed a similar increase in support for smoke-free restaurants as the comparison group.
Figure 1.
Percentage supporting smoke-free restaurants before and after implementation of the Minnesota statewide smoke-free law in October 2007: three subgroups, multivariate modelsa
aAdjusted for gender, past 30-day smoking, and number of close friends who smoked. Minnesotans with a local smoke-free law did not differ significantly from comparison states without a local smoke-free law (p50.80). Minnesotans without a local smoke-free law did not differ significantly from comparison states without a local smoke-free law (p=0.054). Minnesotans without a local smoke-free law did differ significantly from Minnesotans with a local smoke-free law (p=0.021).
MN = Minnesota
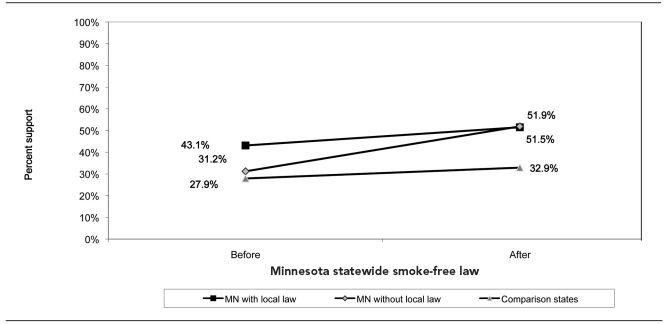
Figure 2.
Percentage supporting smoke-free bars/clubs before and after implementation of the Minnesota statewide smoke-free law in October 2007: three subgroups, multivariate modelsa
aAdjusted for gender, past 30-day smoking, and number of close friends who smoked. Minnesotans with a local smoke-free law did not differ significantly from comparison states without a local smoke-free law (p=0.80). Minnesotans without a local smoke-free law did not differ significantly from comparison states without a local smoke-free law (p=0.054). Minnesotans without a local smoke-free law did differ significantly from Minnesotans with a local smoke-free law (p=0.021).
MN = Minnesota
However, for bars/clubs, those living without a previous local smoke-free law showed larger changes in support compared with both the comparison group (F[2, 1,658] = 10.91, p<0.0001) and those living with a local law (F[2, 1,644] = 5.59, p=0.004). The change in support among Minnesotans living with a previous local smoke-free law did not differ from the change in support in the comparison group.
DISCUSSION
Similar to other studies, we observed an increase in support for smoke-free restaurants and bars after Minnesota's statewide smoke-free law was implemented, both for those living with and without a previous local smoke-free law. However, when compared with states in which a smoke-free law was not enacted, only those teens and young adults living without a previous local smoke-free law showed a significant increase in support for smoke-free legislation, and only for bars, not restaurants. Thus, those previously living with a local smoke-free law showed a similar increase in support for smoke-free bars and restaurants as those in the comparison group.
This greater change in support among teens and young adults not living with a previous local smoke-free law explains a change in norms that occurs after such a policy change, helping to answer the question, “Does public support increase because of a policy, or does public support drive a policy change?” Our analyses suggest that policy change drives changes in support, but changes in support may also lead to policy change.
In addition to increased support seen among teens and young adults in Minnesota after the statewide smoke-free law was enacted, our data also showed some evidence of a secular trend in increased support for smoke-free policies in the absence of any law, as seen in the comparison group (although this increase was only seen for smoke-free restaurants, not bars/clubs). This finding may be explained by attitudes among participants in the comparison group being affected somewhat by smoke-free laws being implemented throughout the nation and the world, even though they may not be directly affected by a smoke-free law in their community or state.
We also found some differences by sociodemographic and personal characteristics, including different support for both smoke-free restaurants and bars based on past 30-day smoking and number of friends who smoked across the three subgroups. For example, among past 30-day smokers not experiencing a previous local smoke-free law, overall support was lower than among nonsmokers, but there was a fairly substantial increase in support among smokers. However, overall patterns of changes in support were inconsistent across subgroups and for bars and restaurants, making it difficult to draw any clear conclusions.
Limitations
One limitation of this study was that two of our covar-iates (past 30-day smoking and number of friends who smoked) were self-reported behaviors that may have been susceptible to reporting bias. An additional limitation was that we were not able to include in our analyses other potential covariates (e.g., other tobacco-control efforts or media influences) related to support for smoke-free policies.
CONCLUSIONS
This study significantly contributes to the research literature and provides support for advocacy actions toward comprehensive smoke-free policies. Our study employed a more robust design than most previous studies, particularly compared with other U.S. studies. We measured support both before and after implementation of a smoke-free law, and we included a comparison group. In addition, we focused on the teen and young adult population, a particularly important age group, given that they are often employed in bars and restaurants16 and young adults tend to frequent bars.17
This study was also the first longitudinal study of support for smoke-free bars and restaurants in the U.S. conducted outside of California.18,19 Our results will help advocates and policy makers to demonstrate how public support for a smoke-free law increases following comprehensive smoke-free legislation, particularly among those who were not previously living with a local smoke-free law.
Acknowledgments
The authors thank Rose Hilk for her assistance with data management, Amanda Rian for formatting the article, Clearwater Research, Inc. for its careful implementation of the telephone survey procedures, and the Health Survey Research Center for its assistance with tracking participants.
Footnotes
This research was funded by the National Cancer Institute (NCI) (R01 CA86191; Jean Forster, Principal Investigator) and ClearWay Minnesota (RC-2007-0018; Jean Forster and Debra Bernat, Coprincipal Investigators). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of NCI or ClearWay Minnesota.
REFERENCES
- 1.Department of Health and Human Services (US) The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta: HHS; 2006. [PubMed] [Google Scholar]
- 2.Hahn EJ, Rayens MK, Butler KM, Zhang M, Durbin E, Steinke D. Smoke-free laws and adult smoking prevalence. Prev Med. 2008;47:206–9. doi: 10.1016/j.ypmed.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Siegel M, Albers AB, Cheng DM, Biener L, Rigotti NA. Effect of local restaurant smoking regulations on progression to established smoking among youths. Tob Control. 2005;14:300–6. doi: 10.1136/tc.2005.012302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Americans for Nonsmokers' Rights. Smokefree lists, maps, and data. [cited 2010 Sep 30]. Available from: URL: http://www.no-smoke.org/goingsmokefree.php?id=519.
- 5.Siegel M, Skeer M. The descriptive epidemiology of local restaurant smoking regulations in Massachusetts: an analysis of the protection of restaurant customers and workers. Tob Control. 2003;12:221–6. doi: 10.1136/tc.12.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dearlove JV, Bialous SA, Glantz SA. Tobacco industry manipulation of the hospitality industry to maintain smoking in public places. Tob Control. 2002;11:94–104. doi: 10.1136/tc.11.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borland R, Yong HH, Siahpush M, Hyland A, Campbell S, Hastings G, et al. Support for and reported compliance with smoke-free restaurants and bars by smokers in four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):ii34–41. doi: 10.1136/tc.2004.008748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rayens MK, Hahn EJ, Langley RE, Zhang M. Public support for smoke-free laws in rural communities. Am J Prev Med. 2008;34:519–22. doi: 10.1016/j.amepre.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Torabi MR, Seo DC. Sociodemographic correlates of public perceptions regarding a smoking ban in bars and restaurants. J Drug Educ. 2004;34:335–50. doi: 10.2190/RLYV-LV71-YCAG-78C2. [DOI] [PubMed] [Google Scholar]
- 10.Tzelepis F, Walsh RA, Paul CL. Community attitudes towards environmental tobacco smoke in licensed premises: follow-up study after the Sharp case. Aust N Z J Public Health. 2003;27:539–42. doi: 10.1111/j.1467-842x.2003.tb00830.x. [DOI] [PubMed] [Google Scholar]
- 11.Bernat DH, Klein EG, Fabian LEA, Forster JL. Young adult support for clean indoor air laws in restaurants and bars. J Adolesc Health. 2009;45:102–4. doi: 10.1016/j.jadohealth.2008.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammond D, Costello MJ, Fong GT, Topham J. Exposure to tobacco marketing and support for tobacco control policies. Am J Health Behav. 2006;30:700–9. doi: 10.5555/ajhb.2006.30.6.700. [DOI] [PubMed] [Google Scholar]
- 13.Lazuras L, Eiser JR, Rodafinos A. Predicting smokers' non-compliance with smoking restrictions in public places. Tob Control. 2009;18:127–31. doi: 10.1136/tc.2008.025841. [DOI] [PubMed] [Google Scholar]
- 14.Loukas A, Garcia MR, Gottlieb NH. Texas college students' opinions of no-smoking policies, secondhand smoke, and smoking in public places. J Am Coll Health. 2006;55:27–32. doi: 10.3200/JACH.55.1.27-32. [DOI] [PubMed] [Google Scholar]
- 15.Rigotti NA, Regan S, Moran SE, Wechsler H. Students' opinion of tobacco control policies recommended for US colleges: a national survey. Tob Control. 2003;12:251–6. doi: 10.1136/tc.12.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leibert A. Teen summer employment outlook for 2009. St. Paul (MN): Minnesota Department of Employment and Economic Development; 2009. [Google Scholar]
- 17.Biener L, Albers AB. Young adults: vulnerable new targets of tobacco marketing. Am J Public Health. 2004;94:326–30. doi: 10.2105/ajph.94.2.326. [published erratum appears in Am J Public Health 2004;94:697] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friis RH, Safer AM. Analysis of responses of Long Beach, California, residents to the smoke-free bars law. Public Health. 2005;119:1116–21. doi: 10.1016/j.puhe.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Tang H, Cowling DW, Lloyd JC, Rogers T, Koumjian KL, Stevens CM, et al. Changes of attitudes and patronage behaviors in response to a smoke-free bar law. Am J Public Health. 2003;93:611–7. doi: 10.2105/ajph.93.4.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown A, Moodie C, Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine Tob Res. 2009;11:924–32. doi: 10.1093/ntr/ntp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeill A, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control. 2006;15(Suppl 3):ii51–8. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hyland A, Hassan LM, Higbee C, Boudreau C, Fong GT, Borland R, et al. The impact of smoke-free legislation in Scotland: results from the Scottish ITC: Scotland/UK longitudinal surveys. Eur J Public Health. 2009;19:198–205. doi: 10.1093/eurpub/ckn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller C, Wakefield M, Kriven S, Hyland A. Evaluation of smoke-free dining in South Australia: support and compliance among the community and restaurateurs. Aust N Z J Public Health. 2002;26:38–44. doi: 10.1111/j.1467-842x.2002.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 24.Thomson G, Wilson N. One year of smoke-free bars and restaurants in New Zealand: impacts and responses. BMC Public Health. 2006;6:64. doi: 10.1186/1471-2458-6-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.SAS Institute, Inc. SAS®: Version 9.1. Cary (NC): SAS Institute, Inc.; 2004. [Google Scholar]