Abstract
Objectives
We examined the disparities in health-care coverage between low- and high-income workers in Washington State (WA) to provide support for possible policy decisions for uninsured workers.
Methods
We examined data from the WA Behavioral Risk Factor Surveillance System 2003–2007 and compared workers aged 18–64 years of low income (annual household income <$35,000) and high income (annual household income ≥$35,000) on proportions and sources of health-care coverage. We conducted multivariable logistic regression analyses on factors that were associated with the uninsured.
Results
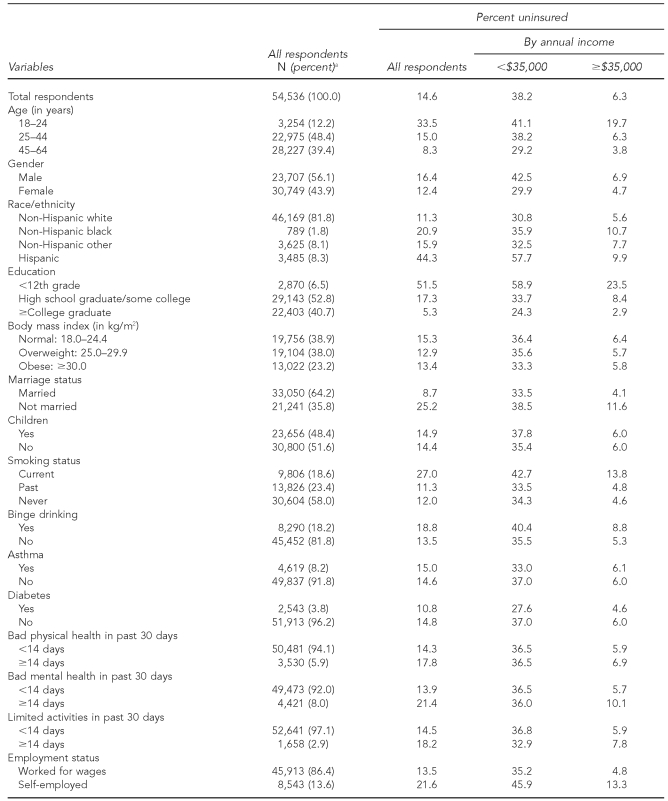
Of the 54,536 survey respondents who were working-age adults in WA, 13,922 (25.5%) were low-income workers. The proportions of uninsured were 38.2% for low-income workers and 6.3% for high-income workers. While employment-based health benefits remained a dominant source of health insurance coverage, they covered only 40.2% of low-income workers relative to 81.5% of high-income workers. Besides income, workers were more likely to be uninsured if they were younger; male; Hispanic; less educated; not married; current smokers; self-employed; or employed in agriculture/forestry/fisheries, construction, and retail. More low-income workers (28.7%) reported cost as an issue in paying for health services than did their high-income counterparts (6.7%).
Conclusion
A persistent gap in health-care coverage exists between low- and high-income workers. The identified characteristics of these workers can be used to implement policies to expand health insurance coverage.
Socioeconomic disparities in health and health care have increased since the 1990s.1–3 In the U.S., while employment-based insurance is the major source of paying for health care,4,5 the increase in health insurance premiums has outpaced workers' earnings and inflation rates. The average cost of health insurance rose 9.6% annually from 2003 to 2007, a rate that was much higher than the overall rate of inflation (2.8%) or the increase in workers' earnings (2.9%) during the same time period (author calculation based on a 2007 report by the Kaiser Family Foundation4). Rising costs impose a greater burden on low-income workers than their higher-income counterparts because low-income workers are less likely to work for a company that offers health insurance coverage.5–9 Without employer-sponsored health insurance, few low-income workers are able to afford private coverage on their own.7,10 Further, most of these low-income workers are ineligible for public health insurance programs.6,10,11 This ineligibility is because in most states, income eligibility is lower for parents than for children and for those adults without dependent children.10
Many factors affect the likelihood of an individual having health insurance and the source of that coverage. Work status and income play a dominant role in determining an individual's likelihood of having health insurance.5,7–9,12 Uninsured workers were found disproportionately in the agriculture, construction, and trade industries,5,8,9,13 and in the farming, operators/fabricators/labors, and services sectors.8,9 Uninsured workers also were more likely to be self-employed,8,14 to work for small firms,5,7–9,13,15,16 and to be employed as part-time or temporary workers.5,14,17,18 Socioeconomic characteristics related to lack of health-care coverage include being male, younger, from a racial/ethnic minority group, less educated, and in a low-wage or low-income job.5,8,12,14,19 Consequently, uninsured workers were less likely to have a usual source of care and receive timely preventive services, and more likely to experience a decline in overall health.7,9,12,20–22
Although national uninsured trends are well documented, published work concurrently considering workers' socioeconomics, industry, and occupation characteristics in Washington State (WA) is lacking. In an effort to expand the current knowledge on uninsured workers in WA and provide support for possible policy decisions, we conducted a multivariate analysis on health-care coverage comparing low-income workers with high-income workers by pooling the five-year WA Behavioral Risk Factor Surveillance System (BRFSS) data. Because most of the uninsured come from working families and have low incomes,4,6,10 we identified characteristics of workers who did not have health-care coverage and examined how low-income workers have fared in health-related outcomes. The analysis presents trends, examines multiple factors that affect health insurance coverage, and discusses policy implications. We hypothesized that even after controlling the multiple factors associated with being uninsured, less health-care coverage and increased health-care costs would impose a greater burden for low-income workers and families.
METHODS
WA BRFSS 2003–2007
The BRFSS is an ongoing, nationwide telephone survey conducted at the state level for noninstitutionalized civilian adults aged 18 years and older. The system was established in 1984 by the Centers for Disease Control and Prevention (CDC) in conjunction with state health departments.23 The BRFSS collects information from adults on health behaviors and preventive practices related to several leading causes of death. The BRFSS questionnaire is designed to include a core set of questions used by all states and an additional set of questions sponsored by each state that may be derived from optional modules developed by CDC or other appropriate sources. Since 2003, WA implemented Spanish language in the BRFSS. As a result, the participation of Hispanic people has increased substantially.24
Study population
The study covers workers aged 18–64 years who worked for wages or were self-employed at the time of the survey during 2003–2007. Using the BRFSS core questionnaire, we defined working adults as those who were currently employed for wages or self-employed. Of the 109,912 participants in the WA BRFSS 2003–2007, 57,456 (52.3%) were working adults at the time of the survey. We excluded 2,917 participants who were ≥65 years of age (2.7% of the working population) because this group is eligible for Medicare and can receive health insurance coverage from a number of different sources. In fact, more than 99% of the workers ≥65 years of age reported having health-care coverage in our data. The analyses were conducted for 54,536 working adults aged 18–64 years, which represented an average of 2.5 million WA workers who were either working for wages or self-employed at the time of the survey.
Health-care coverage and characteristics of individual workers
We described health-care coverage of the workers using three questions. The first question concerned whether or not the worker had any kind of health-care coverage, including health insurance, prepared plans such as health maintenance organizations, or government plans such as Medicare. The second question concerned whether the worker could not see a doctor when there was a need because of cost. The third question was about the type of health-care coverage, which applied only to those participants who had health-care coverage. The type of health-care coverage was unique to WA because it was a WA-added question that was available in three of the five survey years (2003, 2005, and 2007; 48.5% of all respondent workers). The sources of health-care coverage included the employer of the participant or someone else's employer, privately bought insurance, or publicly available insurance (e.g., Medicaid, Medicare, the military, the Civilian Health and Medical Program of the Uniformed Services, the Veteran's Administration, or the Indian Health Service).
We obtained workers' demographic characteristics including age, gender, race/ethnicity, educational attainment, income, weight, height, marital status, and whether or not there were children in the household. We calculated body mass index as kilograms per meter squared. We defined low-income workers as those with a household income <$35,000 a year. Lifestyle characteristics included current smoking status and binge drinking, which was defined as consuming five or more drinks on one or more occasions in the past 30 days. Comorbid conditions included asthma or diabetes, as told by a doctor, nurse, or other health professional. We also obtained health status of self-rated unhealthy physical health days, unhealthy mental health days, and activity limitation days because of health conditions during the past 30 days.
We used the self-reported business/industry and job title for industry and occupation coding, respectively. The industry and occupation data were collected as verbatim and were WA-added questions. Eighty-five percent of the verbatim were auto-coded as three-digit industry and occupation groups using the Standardized Occupation and Industry Coding client program.25 The remaining 15% of the verbatim were coded manually by two National Institutes of Occupational Safety and Health-trained researchers as 13 industry and nine occupation groups. We achieved a high level of agreement (Kappa coefficient >0.9) between the two coders on manual coding of industry and occupation subgroups. Industry and occupation were grouped based on the National Center for Health Statistics Instruction Manuals26 and Standardized Occupation and Industry Coding.25 For analysis purposes, industry and occupation were recategorized into nine and six groups, respectively.
Data analysis
We conducted descriptive analyses on health-care coverage comparing low-income workers with high-income workers as reported in the WA BRFSS data from 2003 to 2007 combined. We compared the proportions of uninsured workers in demographics, lifestyle characteristics, comorbid conditions, health status, and industry/occupation characteristics. We performed these comparisons for all survey respondents, low-income workers, and high-income workers.
We used multivariable logistic regression analyses to evaluate the association between lacking health-care coverage and individual and industry/occupation factors. This analysis was achieved in two steps. First, in an attempt to reduce the number of variables for developing the final models, we performed multivariable logistic regressions adjusted for age and gender only. Specifically, we used health insurance coverage as a dependent variable, and age, gender, and one of the variables of interest as independent variables. This step produced correspondent odds ratios (ORs) and p-values for each of the variables tested besides age and gender. Based on these preliminary estimations, we considered all tested variables with p<0.2 for developing a final model, which controlled all variables simultaneously. The final model kept only those variables that were statistically significant at p<0.05.
We used SAS® SurveyLogistic version 9.227 and applied goodness-of-fit statistics to make sure there was no evidence of lack of fit. When the final model was developed for all survey respondents, we conducted the logistic regression models separately for low- and high-income workers, controlling for the same set of variables.
Because the BRFSS uses a multistage cluster design, based on selection of clusters of telephone numbers, selection of households, and selection of respondents, all of the analyses were conducted using SAS, which took into account differential probabilities of selection and the complex sample design.
RESULTS
Health insurance coverage, sources, and trends
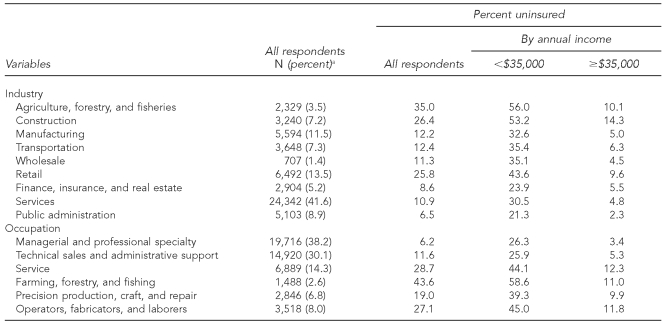
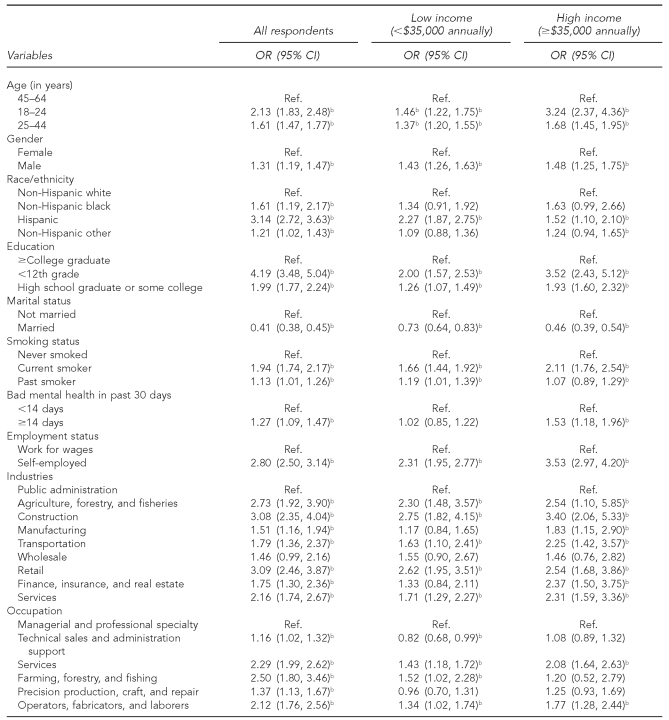
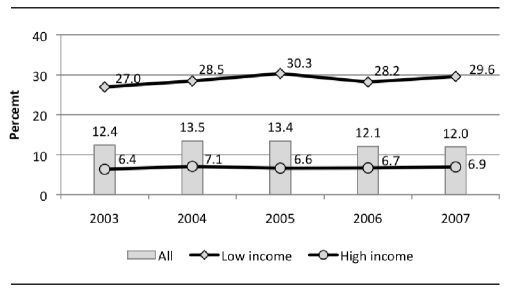
Of the 54,536 survey respondents who were 18–64 years of age and working in WA during 2003–2007, 13,922 (25.5%) were low-income workers with an annual household income <$35,000. The proportion of uninsured was 14.6% for all surveyed workers, 38.2% for low-income workers, and 6.3% for high-income workers (Table 1). Self-reported sources of health insurance among these workers are summarized in Figure 1. The results suggest that health insurance coverage was strongly related to employment, as more than 70% of those having health insurance coverage were provided insurance at the workplace: of those, 81.5% were enrolled in employer-sponsored plans and 18.5% were covered by someone else's insurance (data not shown). While employment-based health benefits remained a dominant source of health coverage, fewer than half (40.2%) of low-income workers in WA received health insurance through their jobs or someone else's employer. This finding is in contrast with 81.5% of high-income workers who received health insurance through their jobs or someone else's employer (Figure 1). During the five survey years examined, uninsured low-income workers ranged from 32.9%–40.3%, while uninsured high-income workers ranged from 5.4%–7.1% (Figure 2). The gap between low- and high-income workers on proportion of uninsured persisted throughout the five years.
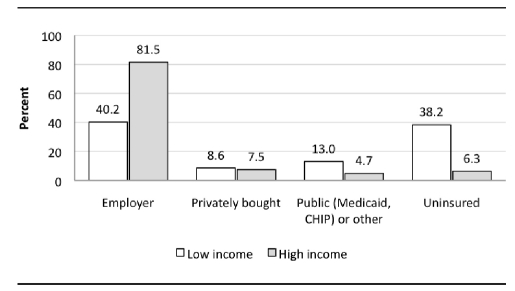
Table 1.
Distribution of individual factors and not having health-care coverage among workers 18–64 years of age: Washington State Behavioral Risk Factor Surveillance System, 2003–2007a
ORs and 95% CIs from multivariable logistic regressions adjusted for all other variables listed. Separate models were performed for all respondents, low-income workers, and high-income workers.
kg/m2 = kilograms per meter squared
Figure 1.
Health insurance sources among workers 18–64 years of age, by household income: Washington State Behavioral Risk Factor Surveillance System, 2003–2007a
a48.5% of respondents (n=26,417) answered this question.
CHIP = Children's Health Insurance Program
Figure 2.
Uninsured workers 18–64 years of age, by income: Washington State Behavioral Risk Factor Surveillance System, 2003–2007
Characteristics of uninsured workers
We examined 17 factors including socioeconomics, lifestyle, comorbidity, and industry/occupation for all respondents and by income in the provision of worker health coverage (Table 1). Young workers aged 18–24 years were more likely to be uninsured than workers of older age groups. Although these young workers represented 12.2% of all workers 18–64 years of age, they comprised 33.5% of the uninsured working population. Male workers were more likely to be uninsured compared with female workers (16.4% vs. 12.4%, respectively). Workers of racial/ethnic minority groups were substantially more likely than non-Hispanic white workers to lack health insurance. Approximately 44.3% of Hispanic workers were uninsured, compared with 20.9% of non-Hispanic black workers and 11.3% of non-Hispanic white workers. Low-income workers were disproportionately represented among the working uninsured.
Industries and occupations varied considerably in percentage of uninsured (Table 1). Ranking the nine major industry and six major occupation categories, low-income workers fared worse than their high-income counterparts in every industry and occupation group compared. For example, by industry, while those in public administration reported the lowest proportion of uninsured for both high- and low-income worker groups, the difference was ninefold: 21.3% for low-income workers and 2.3% for high-income workers.
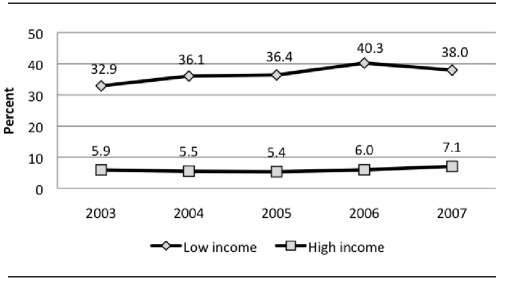
Multivariable logistic regression
Results of multivariable logistic regression indicated that regardless of income, being younger (aged <45 years), male, Hispanic, less than college educated, not married, current or past smokers, with poor mental health that exceeded 14 days during the past 30 days, and self-employed were associated with lack of health insurance (Table 2). Compared with those in public administration, those employed in all industries except for wholesale were more likely to be uninsured. By the same token, compared with workers in managerial and professional specialty occupations, workers in all other occupations were more likely to be uninsured.
Table 2.
Odds of not having health-care coverage and associated factors among workers 18–64 years of age: Washington State Behavioral Risk Factor Surveillance System, 2003–2007a
ORs and 95% CIs from multivariable logistic regressions adjusted for all other variables listed. Separate models were performed for all respondents, low-income workers, and high-income workers.
bStatistically significant at p<0.05
OR = odds ratio
CI = confidence interval
Ref. = reference group
Stark differences existed among low- and high-income workers, as the income-stratified analyses revealed different effects of age, race/ethnicity, education, activity limitation, poor mental health, employment status, and industry and occupation. The effects of younger age (18–24 years), less education (<12th grade), and smoking status (current smokers) were more prominent among high-income workers. Low-income workers who were past smokers and high-income workers with poor mental health were more likely to be uninsured. While the effects of industry categories among high-income workers mirrored those of all survey respondents, low-income workers who worked in agriculture/forestry/fisheries, construction, transportation, retail, and services were more likely to be uninsured. Compared with those in the managerial and professional specialty occupation, low-income workers who were in farming/forestry/fishing, services, and operators/fabricators/laborers were more likely to be uninsured, while high-income workers in services and operators/fabricators/laborers were more likely to be uninsured (Table 2).
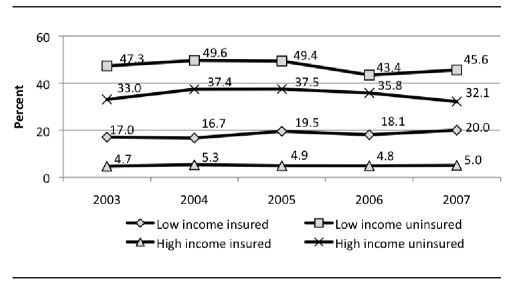
Cost as a barrier to health service access
Workers who could not see a doctor in the last 12 months because of cost were four times as likely to be low-income workers as high-income workers (Figure 3a). More low-income workers reported cost as an issue in paying for health services than their high-income counterparts (28.7% vs. 6.7%). Even for those low-income workers having health-care coverage, about one in five (18%) still considered cost an issue. Further analyses revealed that without health insurance, cost for health care is a burden for both low- and high-income workers. As we considered both income and uninsured status, about one-half of low-income uninsured workers and one-third of high-income uninsured workers reported that they could not see a doctor because of cost, a rate that was higher than that of low-income insured workers (Figure 3b).
Figure 3a.
Workers 18–64 years of age who could not see a doctor because of cost, by income: Washington State Behavioral Risk Factor Surveillance System, 2003–2007
Figure 3b.
Workers 18–64 years of age who could not see a doctor because of cost, by insurance status and income: Washington State Behavioral Risk Factor Surveillance System, 2003–2007
DISCUSSION
This study adds to the published literature on disparities in health insurance coverage by considering workers' demographic, socioeconomic, industry, and occupation characteristics. We used self-reported BRFSS data to describe the nonelderly working uninsured in WA. Our findings were consistent with previous reports that indicated uninsured workers were more likely to be younger; male; Hispanic; less educated; not married; current smokers; self-employed; working in such industries as agriculture/forestry/fisheries, construction, and retail; and employed in occupations such as services and operators/fabricators/laborers.4,5,7–9,13,14,28 The 14.6% overall uninsured workers during 2003–2007 in WA using BRFSS data was similar to the 14.8% reported during 2007–2008 using the Current Population Survey data.29
This study extends the current knowledge of uninsured workers by exploring the disparities between low- and high-income workers. Our data revealed starkly different portraits of low- and high-income uninsured workers. Low-income workers tended to fare worse than high-income workers in health-care coverage, with cost being a major issue in access to health-care services. With household incomes in the lower quartile, low-income workers constituted more than two-thirds of uninsured working adults 18–64 years of age. While employment-based health benefits remained a dominant source of health coverage, the difference between low- and high-income workers in getting employer-sponsored health insurance was significant (40% vs. 80%, respectively).
Income was strongly associated with the progression of both functional limitations and chronic conditions2 and was more important than family type as a determinant of health-care coverage.8 Glied et al. reported a widened gap in health care between low- and high-wage workers during 1996–2003 using data from the Medical Expenditure Panel Survey.3 We used household income, which was reported as stronger than workers' wages, to measure health insurance coverage because a low-wage worker can be covered by a high-wage worker in the same household.8 In our data, while age, gender, race/ethnicity, education, and marital status together created a demographic profile of a typical WA uninsured working adult, household income was the strongest factor associated with insurance status. The results of this study also suggest that the financial burden rose concurrently with lack of health insurance coverage, regardless of household income.
The trend in health insurance coverage among workers was mostly determined by employer-sponsored coverage, which, in turn, was largely affected by changes in the economy. Our data on trends in health insurance coverage during 2003–2007 among WA low-income workers paralleled the data reported for nonelderly uninsured adults (including workers) during the same time period,5,12 with a steady increase during 2003–2006 (from 33% to 40%) and a slight dip (38%) in 2007 (Figure 2). For high-income workers, the uninsured proportions were much lower (5%–7%) during the same time period (Figure 2).
The cost and extent of health insurance coverage was also related to the nature of employment and firm size.5,7–9,13,15,16 Uninsured workers were more likely to be self-employed, as these workers often must obtain their own health insurance coverage and, therefore, pay higher premiums than those paid for by group plans.8,14 In our data, among the self-employed, high-income workers were 3.5 times as likely to be uninsured as those working for wages. Low-wage workers were 2.3 times as likely to be uninsured as those who worked for wages. Uninsured workers were more likely to hold temporary or part-time positions that may have limited their eligibility for employer-sponsored coverage.14 Our data lacked information on industry and occupation for those who were out of work for less than one year. The results from our analyses, therefore, likely underestimated the magnitude of the uninsured, because the loss of employment and income is often compounded by the loss of health insurance.29
Lack of health insurance increases the likelihood of unmet health-care needs. More than one-third of Americans who do not have health insurance reported having problems paying medical bills during the past year.30,31 This number was comparable to that for high-income workers in our data. Our study indicated that a much higher proportion of low-income workers than high-income workers had trouble paying for health services (47.1%). Our data also suggested that even those with health coverage were struggling to cope with soaring medical costs. For employed workers who were <200% of the federal poverty level, only one in four received health coverage through Medicaid or other public programs.6,11 Workers who had no health insurance were less likely to receive preventive services, get routine checkups, and use the latest generation of medical technologies.7,9,12,20–22,32
Strengths and limitations
Our study had several important strengths. First, our samples were relatively representative of the general working-for-wages or self-employed population in WA. Second, BRFSS information has been validated and used to track changes in behavior and measure progress toward achieving national, state, and local public health objectives. The five-year survey data allowed us to examine the patterns of change over time in health-care coverage for all survey participants in WA, while adjusting for socioeconomic and employment characteristics, which would help explain variation across categories or over time. The large sample size of the pooled five-year data ensured more stable estimates and enabled further analyses of the subgroups of low- and high-income workers.
Third, our data captured a more representative Hispanic racial/ethnic minority group. This is important because Hispanic people constitute the fastest-growing and largest racial/ethnic minority group in the U.S., and the socioeconomic inequality in health care between Hispanic and non-Hispanic people is well-known.9,33,34 WA started adding Spanish-language questions in the BRFSS in 2003, which resulted in a 60% increase of Spanish-speaking participants.24 With the implementation of Spanish language in the WA BRFSS, self-reported uninsured Hispanic respondents rose from 13%–29% during 1997–2002 to 42%–47% during 2003–2008.35 Fourth, the industry and occupation data were unique to WA, and these data were not available in BRFSS from other states. Considering workers' industry and occupation simultaneously with other related individual factors provided additional value in evaluating the multiple factors associated with lack of health insurance coverage among workers.
Our study also had several limitations. One limitation of our data was that they lacked income adjustment for the five survey years. The data for household income in the BRFSS was collected at eight fixed levels, with the lower quartile being close to <$35,000. Because of the fixed income categories, we could not factor in inflation for each survey year. Further, because we used the same cut point for low-income workers, our data indicated a steady decline in proportions of low-income workers in each survey year: 26% for 2003–2005, 23% for 2006, and 19% for 2007.
Another limitation was that we did not have data on firm size. Small firms are less likely than large firms to offer employer-sponsored health coverage.5,8,13,15,16 Research in labor economics has demonstrated a strong positive relationship between employer size and -wages.36 Using data from the Current Population Survey, Acs and Nichols reported that 47.8% of low-wage workers with incomes <200% of the federal poverty level worked in small firms with fewer than 25 employees.6 Because low-wage workers in large firms are less likely to be covered by their employers than high-wage workers in small firms,8 it is necessary to consider both firm size and wages to explain the differences in characteristics between uninsured low- and high-income workers. However, our data used household income and measured health-care coverage through workplaces. Therefore, we speculate that firm size would have less effect on the uninsured than workers' wages.
CONCLUSION
We found a persistent gap in health insurance coverage between low- and high-income WA workers. Most of the uninsured were low-income workers. To attenuate inequalities in health-care coverage will require a multifaceted approach involving a combination of both regulatory policies and employer participation. Although a majority of Americans are insured through their workplace, rising health-care costs and the recent economic recession have affected employers' ability to offer health insurance coverage. Thus, policies that encourage employers to sponsor or expand eligibility to health insurance are needed. Such policies could include subsidizing employers and enacting requirements for employers to offer affordable health insurance to workers. Faced with higher premiums and greater out-of-pocket costs, it would be more difficult for employees, especially low-income employees, to purchase employer-based health coverage. Policies that target the reduction of income inequality through tax reform and expand public health insurance, such as Medicaid for low-income adults, could help eliminate disparities in health insurance coverage. Additionally, policies that demand accountability from health-care providers and health plans alike to reduce health-care costs are sorely needed.
Acknowledgments
The authors thank Dr. David Bonauto and Dr. Katrina Simmons for assistance in obtaining the data from the Washington State Department of Health.
Footnotes
This research was supported in part by the U.S. National Institute for Occupational Safety and Health and the Washington State Department of Labor and Industries. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
REFERENCES
- 1.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986 [published erratum appears in N Engl J Med 1993;329:1139] N Engl J Med. 1993;329:103–9. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 2.Herd P, Goesling B, House JS. Socioeconomic position and health: the differential effects of education versus income on the onset versus progression of health problems. J Health Soc Behav. 2007;48:223–38. doi: 10.1177/002214650704800302. [DOI] [PubMed] [Google Scholar]
- 3.Glied S, Mahato B. The widening health care gap between high- and low-wage workers. Washington: The Commonwealth Fund; 2008. May, [PubMed] [Google Scholar]
- 4.Claxton G, Gabel J, DiJulio B, Pickreign J, Whitmore H, Finder B, et al. Health benefits in 2007: premium increases fall to an eight-year low, while offer rates and enrollment remain stable. Health Aff (Millwood) 2007;26:1407–16. doi: 10.1377/hlthaff.26.5.1407. [DOI] [PubMed] [Google Scholar]
- 5.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2009 Current Population Survey. Washington: Employee Benefit Research Institute; 2009. [PubMed] [Google Scholar]
- 6.Acs G, Nichols A. Low-income workers and their employers: characteristics and challenges. Washington: Urban Institute; 2007. [Google Scholar]
- 7.Glied S, Mahato B. Who pays for health care when workers are uninsured? Washington: The Commonwealth Fund; 2008. May, [PubMed] [Google Scholar]
- 8.Greenman E, Garrett B, Nichols L. Workers without health insurance: who are they and how can policy reach them? Washington: Urban Institute; 2001. [Google Scholar]
- 9.Patton B, Duerksen S, Baxamusa M. The working uninsured: an analysis of worker health coverage among California industries. San Diego: Center on Policy Initiatives; 2007. Jul, [Google Scholar]
- 10.Kaiser Commission on Medicaid and the Uninsured. The uninsured: a primer. Key facts about Americans without health insurance. Washington: Kaiser Family Foundation Publications; 2006. [Google Scholar]
- 11.McAndrew C. Unemployed and uninsured in America. New York: Families USA; 2009. Feb, [Google Scholar]
- 12.Claxton G, DiJulio B, Whitmore H, Pickreign J, McHugh M, Finder B, et al. Job-based health insurance: costs climb at a moderate pace. Health Aff (Millwood) 2009;28:w1002–12. doi: 10.1377/hlthaff.28.6.w1002. [DOI] [PubMed] [Google Scholar]
- 13.Nichols LM, Blumberg LJ, Acs GP, Uccello CE, Marsteller JA. Small employers: their diversity and health insurance. Washington: Urban Institute; 1997. Jun, [Google Scholar]
- 14.Office of Health Care Access. Who are the uninsured? Characteristics of uninsured workers in Connecticut. Hartford (CT): Office of Health Care Access; 2003. Jan, [Google Scholar]
- 15.Cooper PF, Schone BS. More offers, fewer takers for employment-based health insurance: 1987 and 1996. Health Aff (Millwood) 1997;16:142–9. doi: 10.1377/hlthaff.16.6.142. [DOI] [PubMed] [Google Scholar]
- 16.Schoen C, Collins SR, Kriss JL, Doty MM. How many are underinsured? Trends among U.S. adults, 2003 and 2007. Health Aff (Millwood) 2008;27:w298–309. doi: 10.1377/hlthaff.27.4.w298. [DOI] [PubMed] [Google Scholar]
- 17.Farber HS, Levy H. Recent trends in employer-sponsored health insurance coverage: are bad jobs getting worse? J Health Econ. 2000;19:93–119. doi: 10.1016/s0167-6296(99)00027-2. [DOI] [PubMed] [Google Scholar]
- 18.Thorpe KE, Florence CS. Why are workers uninsured? Employer-sponsored health insurance in 1997. Health Aff (Millwood) 1999;18:213–8. doi: 10.1377/hlthaff.18.2.213. [DOI] [PubMed] [Google Scholar]
- 19.Kaye HS. Stuck at the bottom rung: occupational characteristics of workers with disabilities. J Occup Rehabil. 2009;19:115–28. doi: 10.1007/s10926-009-9175-2. [DOI] [PubMed] [Google Scholar]
- 20.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 21.Hadley J. Sicker and poorer—the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 Suppl):3s–75s. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- 22.Hoffman C, Paradise J. Health insurance and access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–60. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 23.Remington PL, Smith MY, Williamson DF, Anda RF, Gentry EM, Hogelin GC. Design, characteristics, and usefulness of state-based behavioral risk factor surveillance: 1981–87. Public Health Rep. 1988;103:366–75. [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (US), Office of Surveillance, Epidemiology, and Laboratory Services. Behavioral Risk Factor Surveillance System annual survey data: 2003. Atlanta: CDC; 2004. [Google Scholar]
- 25.National Institute for Occupational Safety and Health (US). Standardized occupation and industry coding: version 1.5. Morgantown (WV): NIOSH; 2001. [Google Scholar]
- 26.Department of Health and Human Services, Public Health Service (US). National Center for Health Statistics instruction manuals parts 19A and 19B. Hyattsville (MD): National Center for Health Statistics (US); 1999. [Google Scholar]
- 27.SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc.; 2009. [Google Scholar]
- 28.Department of Health and Human Services, Agency for Healthcare Research and Quality (US). Estimates for U.S. civilian noninstitutionalized workers ages 16–64. Rockville (MD): AHRQ; 1998. Dec, Highlights #7: uninsured workers—demographic characteristics, 1996. [Google Scholar]
- 29.Rowland D, Garfield R. Health insurance for unemployed workers. Medscape Gen Med. 2002;4(1) [PubMed] [Google Scholar]
- 30.Robert Wood Johnson Foundation. At the brink: trends in America's uninsured. Princeton (NJ): Robert Wood Johnson Foundation; 2009. Mar, [Google Scholar]
- 31.Blendon RJ, Benson JM, Weldon KJ. Health priorities survey: the medical system and the uninsured. Princeton (NJ): Harvard School of Public Health, Robert Wood Johnson Foundation; 2009. Aug, [Google Scholar]
- 32.Hoffman C, Schwartz K. Trends in access to care among working-age adults, 1997–2006. Washington: Kaiser Commission on Medicaid and the Uninsured; 2008. [Google Scholar]
- 33.Livingston G. Hispanics, health insurance and health care access. Washington: Pew Hispanic Center; 2009. Sep, [Google Scholar]
- 34.Pleis JR, Lethbridge-Cejku M. Vital Health Stat 10. 235. 2007. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (US), Office of Surveillance, Epidemiology, and Laboratory Services. Behavioral Risk Factor Surveillance System annual survey data: 2008. Atlanta: CDC; 2009. [Google Scholar]
- 36.Oi WY, Idson TL. Firm size and wages. In: Ashenfelter O, Card D, editors. Handbook of labor economics, volume 3A. Amsterdam: Elsevier Science B.V.; 1999. pp. p. 2165–214. [Google Scholar]