Abstract
Objective
A component of health-care reform in 2010 identified physician assistants (PAs) as needed to help mitigate the expected doctor shortage. We modeled their number to predict rational estimates for workforce planners.
Methods
The number of PAs in active clinical practice in 2010 formed the baseline. We used graduation rates and program expansion to project annual growth; attrition estimates offset these amounts. A simulation model incorporated historical trends, current supply, and graduation amounts. Sensitivity analyses were conducted to systematically adjust parameters in the model to determine the effects of such changes.
Results
As of 2010, there were 74,476 PAs in the active workforce. The mean age was 42 years and 65% were female. There were 154 accredited educational programs; 99% had a graduating class and produced an average of 44 graduates annually (total n=6,776). With a 7% increase in graduate entry rate and a 5% annual attrition rate, the supply of clinically active PAs will grow to 93,099 in 2015, 111,004 in 2020, and 127,821 in 2025. This model holds clinically active PAs in primary care at 34%.
Conclusions
The number of clinically active PAs is projected to increase by almost 72% in 15 years. Attrition rates, especially retirement patterns, are not well understood for PAs, and variation could affect future supply. While the majority of PAs are in the medical specialties and subspecialties fields, new policy steps funding PA education and promoting primary care may add more PAs in primary care than the model predicts.
Physician assistants (PAs) and nurse practitioners (NPs) are considered essential parts of the contemporary U.S. medical workforce.1 As medical providers, PAs have been essential during times of physician shortages and, historically, it was a lack of doctors in underserved areas that first spurred their creation.2 Once again, experts believe that the U.S. faces an insufficient cadre of physicians, with projections indicating that the supply will be unable to keep pace with demand; by 2025, a shortage of 124,000 primary care physicians is anticipated.3,4 Consequently, analysts have suggested that there will be an increased reliance on PAs and NPs.5,6
Models developed to predict the supply of physicians under various scenarios are important for health planners. Because little research has included the supply of PAs and NPs in these projections, accurate numbers of clinically active providers are needed for rational medical workforce planning. Such key data could provide policy makers with needed information to augment physician services in both the specialty and primary care sectors of the medical workforce.
A SHORTAGE OF PHYSICIANS
While the supply of U.S. medical school graduates has increased since the new century, the output of doctors has been modest at best and may not be adequate in the short run.5,6 The aging of the population is expected to increase demand for medical services, particularly in specialties that predominantly serve the elderly (e.g., oncology and rheumatology).7,8 There are indications that the baby-boomer generation (and subsequent generations) will be aggressive in seeking medical care services and will be more likely to seek medical care than previous generations.5 The Association of American Medical Colleges believes that the 30% expansion in medical school enrollment and an increase in graduate medical education positions will not eliminate the projected shortage.9 Additional factors that could affect supply are lifestyle and working hour trends, changes in overall productivity, the flow of international medical graduates, and delivery system adjustments.
A previous attempt to assess the size of the PA workforce overestimated the supply of PAs by 25%.10 This analysis was based on incomplete information and did not utilize more reliable data from the American Academy of Physician Assistants (AAPA) Master File. While the AAPA's Master File is useful, it imputes data of survey nonrespondents to predict supply estimates and does not track retirement.11 Neither of these deterministic studies used projection modeling. We argue that simulation is a preferred approach for health workforce modeling.12 Our objective was to create a more accurate PA workforce projection model to provide analysts with key information needed for policy decision-making.
METHODS
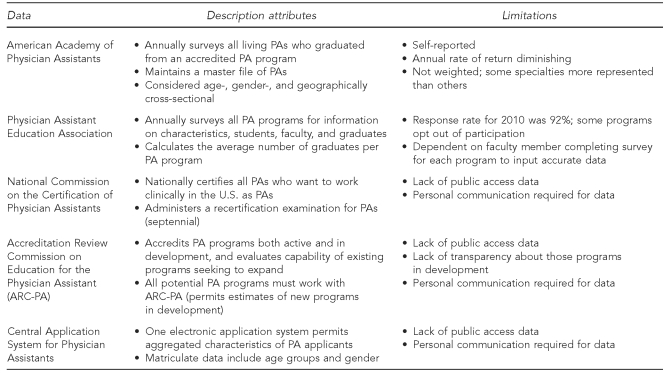
We evaluated available summary data from the four major PA organizations (Figure 1) by developing a spreadsheet and using regression modeling to project annual clinical PA participation and attrition rates. We based key assumptions on available data and expert opinion to produce a final trend analysis using linear regression analysis.
Figure 1.
Physician assistant metadata attributes and limitations used to create a predictive model of clinically active physician assistants by 2025
PA = physician assistant
Data sources
We obtained the number of PAs in active clinical practice from the AAPA Annual Census and Master File, along with the number of PA educational programs and annual graduates from the Physician Assistant Education Association (PAEA). From the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA), we obtained estimates of the number of academic institutions with PA programs in development or on the pathway to accreditation (i.e., “in the pipeline”). We obtained corroborating information on clinically active PAs from the Bureau of Labor Statistics (BLS), the National Commission on the Certification of Physician Assistants (NCCPA), and experts on workforce attrition and retirement in the U.S. labor force. We used BLS career retirement trends and AAMC surveys of older doctors as validation measures of PA clinical attrition.13,14
PA education growth
The 2010 PA graduation cohort formed the basis for projecting the supply. Sources of data for projections came from PAEA and ARC-PA. All U.S. PA programs must obtain provisional accreditation prior to the beginning of the first class and full accreditation before the first class graduates. The mean time from the first day of class to graduation of the first class is approximately 28 months. As of 2010, a total of 154 programs were operational and 152 were accredited (99%) (Personal communication, John McCarty, ARC-PA, January 2011).
Clinically active PAs
We defined clinically active PAs as those possessing a state license or employed in a federal agency (e.g., military or Department of Veterans' Affairs). To be clinically active, a PA must pass the PA National Certification Examination (PANCE), which is administered by the NCCPA. Historically, eventual pass rate of the PANCE is 97% (Personal communication, Janet Lathrop, NCCPA, September 2010). This 3% loss of PAs who never obtain certification—and remain ineligible to be licensed as clinically active—was discounted after graduation and not added to the pool of clinically active PAs. The AAPA annual census data of 2009 was used to estimate the number of clinically active PAs that year.15
Attrition
For the purposes of this model, we defined attrition as any PA leaving a clinical role. This relaxed definition includes loss due to death, illness, retirement, inactive status, changing careers, not qualified, and emigration. We estimated annual attrition based on AAPA census results and estimates for 2010, and then computed attrition based on the age of all PAs departing clinical activity at age 70 years. We calculated a mean annual attrition rate using the 2010 PA survey of active PAs and retiring each individual at age 70 years (to 2025). This population model, with age-specific rates of attrition each year, produced a number (between 4% and 6%) and a mean annual rate of 5%. For validation purposes, we queried PA program managers that maintain longitudinal databases on their alumni, and examined the BLS to estimate retirement of doctors, lawyers, and pharmacists, which revealed similar results.
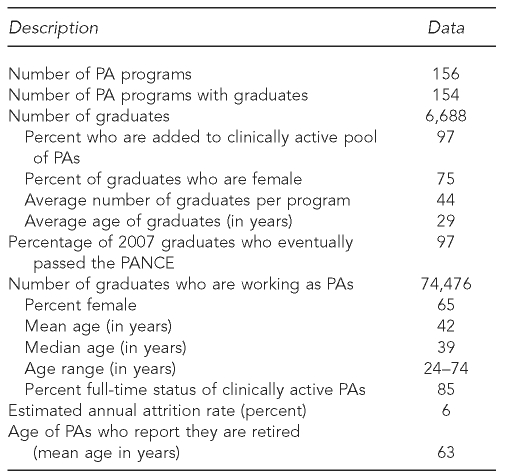
We developed three attrition rates (4%, 5%, and 6%) and projected them during a 15-year span (2010–2025). Factors influencing attrition estimates included the percentage of women entering the PA profession who were 20–45 years of age (average child-rearing years), those who graduated in the 46- to 65-year age group, and the national trend of men and women who continue a career beyond their mid-60s. While we used a simplified annual average, we are aware that the hazard rate of attrition is low in the early years of a career and grows substantially during the latter third of a career, producing the same results as an annual rate of 5%. Sensitivity analyses incorporated the mean age of clinically active PAs, the age of PAs who reported they were retired, and the population profile of clinically active PAs in 2009 projected for all the years (Table).
Table.
Baseline 2010 data for a physician assistant predictive modela
aEnd-of-year result. Data for 2010 were adjusted for those PAs considered in active clinical practice and used as the basis for all predictions in the model.
PA = physician assistant
PANCE = Physician Assistant National Certification Examination
Age and gender
We determined the age and gender of clinically active PAs using AAPA census data for 2009 and added the 2009 graduation cohort to create a clinically active PA population for 2010.15 The distribution of the age and gender of graduates of an annual cohort was obtained using the Computerized Application System for Physician Assistants (CASPA). In 2007, CASPA identified the summary characteristics of entering PA students, and this was projected for the 2010 graduating cohort age and gender characteristics.2 This age/gender distribution profile was held constant for each annual graduation cohort to 2025.
Primary care
We defined a primary care PA as one who is in active practice in family medicine, general internal medicine, or general pediatrics. The proportion of PAs practicing in primary care (34%) was based on the 2009 AAPA census results.
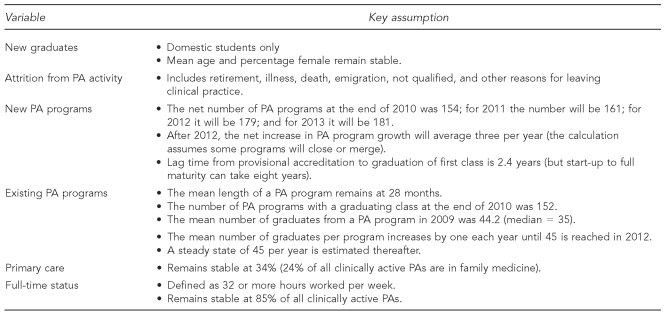
Assumptions
The assumptions used in this analysis are listed in Figure 2. We based these assumptions on data thus described, estimates of new programs, capacity of new programs to grow the class size, and survey data from existing PA programs on their expansion (and constraints).16 Experts, labor economists, program directors, and health workforce analysts reviewed the model for validation of assumptions. We chose the median numbers when given a range and performed sensitivity analyses on vital data points. A key assumption, based on the authors' experience with program development, was that the availability of clinical training sites often determines (and may constrain) growth in the formative years. Beginning in 2011, the mean number of graduates per program was 45 and held steady. The rationale for this average is a balance; new programs with smaller classes offset modest expansion of mature programs.
Figure 2.
Key assumptionsa used to create a simulation model of projected clinically active physician assistants through 2025
aThe assumptions used in the PA predictive model were identified by the variable employed in the sensitivity analysis.
PA = physician assistant
Simulation model technique
The primary aim of this project was to estimate the number of PAs who are in the clinically active segment of the medical workforce each year. The simulation model incorporated current participation numbers, PA education program growth, expansion, and annual production (output) to generate trends. It begins with year 2010 and projects to 2025 by incorporating regression techniques using three attrition scenarios.
Sensitivity analysis
Two approaches to sensitivity analyses explored the influence of uncertainty in the variables and assumptions involved in the estimation.17 First, a series of one-way sensitivity analyses examined the potential impact of the potential changeability of each variable. The range selected for each variable was based on the historical minimum and maximum values. For example, the historical minimum for the number of new PA programs in a given year is zero and the historical maximum is 18. Additional variables addressed in this manner include the number of clinically active PAs, the number of new PA programs per year, the number in a graduating year cohort, and attrition.
We conducted additional analysis, which varied the number of PAs practicing in 2010. We selected a maximum value of 77,672, which was the number of PAs that either held NCCPA certification or had licensure at year's end in 2010. A minimum value of 72,433 represents no growth in the profession from 2009. The maximum value used for average graduating class size was 98, which represents the largest civilian PA education program. The minimum average class size was 35, which was the 2010 median class size.18 Second, we conducted extreme scenario analysis, which sets all variables listed previously, first at the most optimistic values and then at the most pessimistic values to generate the most extreme estimates possible.
RESULTS
Clinically active PAs
There were an estimated 74,476 PAs in the active workforce at the end of 2009 (AAPA 2009) (Table). The mean age was 42 years (median = 39) and 65% were female.
PA programs and graduates
In 2010, there were 154 accredited PA education programs, and 152 (99%) produced a graduating class. In addition, there were 6,688 PA graduates (an average of 44 graduates per program) and 97% were expected to enter the pool of clinically active PAs (based on the percentage of a graduation cohort who ever become nationally certified) (Table). There were 142 programs in 2008 and 154 in 2010. Program growth projections were as follows: seven in 2011, 18 in 2012, two in 2013, and three per year thereafter. For new PA graduates, the mean age in 2010 was 29 years and 75% were female. Two-thirds of females in the 2010 graduation cohort were aged 22–33 years (data not shown).18
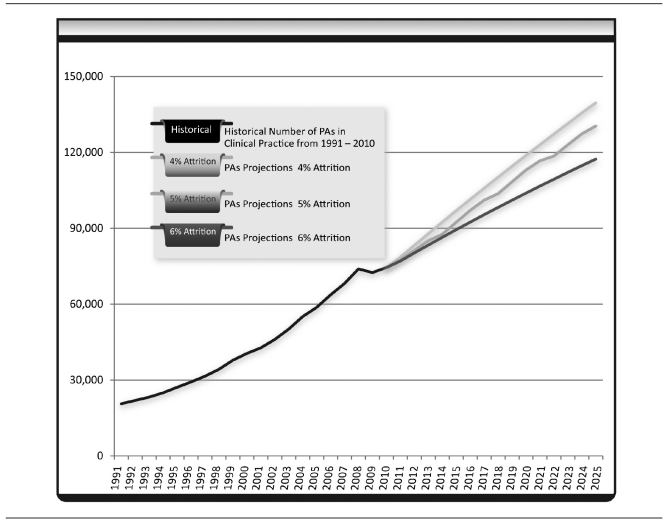
Projecting the PA supply
From our baseline supply, we estimated the number of practicing PAs in 2025 to be 127,821, based on 7% growth and 5% annual attrition. Included input projections were PA program growth and the number of graduates annually. PA program estimates for 2015, 2020, and 2025 were 188, 203, and 218, respectively. Specifically, we modeled the number of PAs per year eligible for clinical practice to be 93,099 in 2015, 111,004 in 2020, and 127,821 in 2025 (Figure 3).
Figure 3.
Physician assistant supply projections, 2010–2025, with three attrition rates
Note: PA supply is projected to year 2025 under three scenarios: 4%, 5%, and 6% attrition. After 2014, the expansion of PA programs reaches a steady state of three per year and the graduation rate averages 45 PAs per program.
PA = physician assistant
Sensitivity analyses
The one-way analyses produced PA estimates in 2025 ranging from 97,801 to 256,421. Extreme scenario analysis provided a range of PA estimates from 90,561 to 353,937.
PA program growth from 1991 to 2011 was fairly steady. Spanning 20 years, the number of PA programs tripled (from 52 to 154). Projected PA program growth (and graduation rates) were constrained in the model due to the long period needed to start a program, graduate the first class, and reach the maximum class size—estimated as an eight-year process (three years to develop and graduate the first class and several years of expansion to reach maximum capacity).
Primary care
The number of PAs in primary care in 2010 was estimated at 23,830. Based on the prediction model of 34% of PAs in primary care, the number would grow to 43,459 in 15 years. If the percentage of PAs in primary care was at its historical maximum of 49%, the number of PAs in primary care would be 62,632 (range: 30,791–173,429 based on extreme scenario analysis) by 2025. These projections can potentially provide between 6% and 121% of the providers required to fill the projected primary care physician shortage. The most likely estimate is that 16% of PAs will fill primary care provider ranks in 2025.
DISCUSSION
The predictive model suggests that the overall supply of PAs is likely to increase by 72% to 127,821 PAs by 2025. With one-third of PA programs inaugurated since 2000, and two-thirds inaugurated since 1991, growth is likely to continue, although not at the same trajectory.
The decline in the percentage of PAs identifying primary care in the AAPA census has shown a slow and steady downward trend of 1%–2% per year since the turn of the century, and a plateau was not predictable in our model. This subject is murky for a number of reasons. PA census respondents separately identified occupational medicine, geriatric medicine, corrections medicine, hospital medicine, public health, and women's health; such roles are primary care in nature but did not meet our definition. At the same time, military PAs use a wide range of skills and roles beyond primary care; however, without their own category, they often select family medicine or general internal medicine on the census form. Finally, while the percentage of primary care PAs may be declining in census statistics, the annual cadre of PAs producing primary care is growing, and a statistical counterbalance may be in effect.
Annual attrition estimates were projected at 4%, 5%, and 6% for the model to provide a range of those departing clinical activity. These attrition assumptions are bolstered by BLS observations for various professionals such as doctors and lawyers at various times in their careers and are offset by a rising percentage of seniors working past 65 years of age.19 If the mean age of a PA at graduation is 29 years, then an average 35-year career as a PA seemed reasonable to our advisors. The PA profession is a relatively young one in age composition (with the mean age at graduation likely to remain around 30 years for the next decade), thus providing an annual production that exceeds attrition. The first two decades of the profession comprised older males with at least one career behind them. Currently, a larger cadre of younger females with no prior career is replacing a smaller, older generation. Furthermore, the age distribution curve of PAs in the 2009 census is more skewed to the right than a bell shape. Finally, our conservative attrition rate of 5% is tempered by the observation that the average age of all PAs who reported being retired is 63 years, which is considered relatively young.15
Retention is the obverse side of attrition, and 82% of people who graduated from a PA program were estimated to be clinically active in 2009.15 Accurate attrition and retention rates for PAs are challenging to estimate as no experiential data are available and because individuals may leave the workforce for a few years and then return, a pattern that is not easily captured. Turning to other studies, a plurality (42%) of PA faculty was uncertain about retiring prior to age 62 years if given the option.20 The annual attrition of PAs in the Veterans Administration (the largest employer of PAs) is 9%, with some PAs departing the Veterans Health Administration with a federal pension but reentering in the private sector.21 We obtained a similar attrition rate of 9% from the Department of Defense, indicating PAs completing 20- to 30-year careers (Personal communication, William Tozier, U.S. Army, March 2010). These high attrition and retirement rates are mentioned as the only reliable data at the time of this study and do not reflect the general population. Death and disability are also absent from PA statistics.
Some variables that influence supply and have predictable values were incorporated into this model. Specifically, we included the average number of graduates per program; 3% who never obtained certification; an aging, predominantly male cadre; and the median age of graduates who are young and female. Growth factors included an increase in the number of universities developing PA programs and class expansion in some older programs. We think these are reasonable assumptions, as graduate programs such as PA education are financially advantageous for institutions, and most of the new programs in the pipeline are private institutions. Furthermore, PA programs are sponsored by less than 5% of U.S. institutions of higher education and less than 50% of academic health centers, suggesting that there is room for new program installation. Constraints on PA program expansion include faculty shortages and an inadequate number of clinical training sites, as PA programs compete with allopathic and osteopathic medical schools and NP programs for student placement.15,16 Another factor is debt obligation, which appears to have a dampening effect on enrollment, at least in proprietary institutions. The opportunity cost of a PA education in a private university exceeds $100,000 and is likely to grow, which could stifle applicant trends.2
The effect of age and gender on the U.S. labor force is still playing out and could not be estimated with the current data. Based on applicants entering PA education, the mean age of graduates has leveled off at 30 years, and the female PA composition will plateau at 66%. Observations in developed countries suggest that a gender shift is not unique to the U.S., and women are beginning to dominate in a number of historically male domains.22 Women entering the PA profession are younger and more likely to take time off for family development.23
Retention in the PA workforce is expected to remain at the current level for a number of reasons. PA career satisfaction is generally considered high, and a national poll found that most practicing PAs would select this career again.24 PAs appear to respond to market forces, and at least half change to another specialty during the span of a career, which may contribute to their satisfaction.25 The ability to change specialties suggests that mobility and adaptability could be vocational characteristics that contribute to retention. Furthermore, procedural-based specialties coupled with physician shortages tend to attract PAs. This finding may be due to high salaries associated with labor-intensive specialties.26,27 Finally, traditional retirement patterns are changing and seniors are using bridging strategies to remain at least partially involved in their career into their 70s, a trend that may be rising but is difficult to calculate.28
Policy implications
The supply and rate of growth of PAs in the U.S. medical workforce has significant policy implications given the reliance that is placed on them to supplement the predicted shortage of physicians.5 The projected growth will result in 72% more PAs by 2025, but will likely only provide 16% of the providers needed to address the projected primary care physician shortage, unless additional policies are instituted to increase the number of PA graduates and/or incentivize PAs to practice in primary care.6
Instituting policies that encourage the -development of new PA training programs holds potential for addressing some of the primary care physician -shortage. Expanding the number of graduates per program appears to be the change with the greatest likelihood of increasing the number of PAs by 2025. This increase could be accomplished through policies that provide funding for clinical preceptor sites, thereby addressing the biggest limitation in PA program expansion.
There is also the potential for PAs to make increased contributions to primary care delivery through policy initiatives. For example, §5501(a) of the Patient Protection and Affordable Care Act provides for an incentive payment for PAs for whom primary care services accounted for a majority of their service provision.29
Limitations
As with any modeling exercise, the projections depend on the variables, parameters, and estimates used. For example, there was no information on the retirement pattern of nonfederal PAs. Thus, the rate of attrition calculated may be subject to some margin of error. Additionally, there are no details about role delineation and what percentage of PAs has daily patient contact. These limitations spotlight the need for better data that a longitudinal cohort analysis could bring. Qualitative analysis of career satisfaction, job mobility, and retirement goals could provide needed insight into occupational stability.
Also, while the predictions have the appearance of accuracy, there are too many variables to achieve such precision over long periods of time in modeling. Furthermore, forecasts are vulnerable in the adequacy of model documentation, the frequency of model maintenance, the existence of evaluative information on model validity, and the quality of model data. Triangulating census data with state licensure data would provide some confidence in the numbers, although even this methodology has problems of uniformity.30 Adherence to the intent of the National Provider Identifier would improve annual estimates of care by different providers.
Strengths
This study also had several strengths. One strength of this study was that we drew on a suite of refined and reliable databases that complement one another. High participation rates in the annual PAEA surveys and NCCPA data incorporated in this study also contributed to the confidence of the numbers. The release of confidential program development data from ARC-PA added substantial value to the predictive model. Finally, previously unknown annual noncertification rates from the NCCPA permitted refinement of projections.
CONCLUSIONS
Health workforce analysts rely on PAs and NPs to augment medical services in the coming years as the impact of a physician shortage becomes apparent. Because the doctor-to-population ratio is likely to decrease over time despite modest domestic medical school growth, the anticipated graduation rate, and current policies constraining international medical graduate immigration, we believe that the demand for PAs will continue to be strong. Workforce modeling to estimate with reasonable accuracy the projected numbers of health-care providers is vital information for policy makers. Similar efforts to model the physician and NP components of the workforce may require more centralization of data.5
Because estimates are just that, some caution is suggested in taking comfort from the present and future contributions of PAs in the medical workforce. Barring major changes, it appears that the annual output will increase from 2010 to 2025, but attrition will modulate this gain. Because analysts believe that PAs will be a necessary component of the medical workforce, and will be needed to help mitigate the expected physician shortage, policy steps enacted in 2010 to fund and promote an increased annual supply of PAs appear justified.
Footnotes
This research was made possible through the generous time and information supplied by Christal Ramos (American Academy of Physician Assistants), Mei Liang (Physician Assistant Education Association), John McCarty (Accreditation Review Commission for the Physician Assistant), Janet Lathrop (National Commission on the Certification of Physician Assistants), Demi Woodmansee (Department of Veterans Affairs), and William Tozier (U.S. Army). The authors thank the Bureau of Labor Statistics for the helpful analysts who offered important information; the many reviewers of the model we used and their valuable opinions that helped shape our assumptions, particularly Perri Morgan (Duke University), who tested many of the assumptions in this model; and Namrata Sen (The Lewin Group), who refined the predictive model and attrition rates.
Christine Everett received financial support from the Agency for Healthcare Research and Quality National Research Service Award (T32 HS00083), Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UL1RR025011), and the Health Innovation Program.
REFERENCES
- 1.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29:799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 2.Hooker RS, Cawley JF, Asprey DP. Physician assistants: policy and practice. 3rd ed. Philadelphia: F.A. Davis; 2010. [Google Scholar]
- 3.Dill MJ, Salsberg ES Center for Workforce Studies. The complexities of physician supply and demand: projections through 2025. Washington: Association of American Medical Colleges; 2008. [Google Scholar]
- 4.Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Health Aff (Millwood) 2008;27:w232–41. doi: 10.1377/hlthaff.27.3.w232. [DOI] [PubMed] [Google Scholar]
- 5.Sargen M, Hooker RS, Cooper RA. Gaps in the supply of physicians, advance practice nurses, and physician assistants. J Am Coll Surg. 2011:212. doi: 10.1016/j.jamcollsurg.2011.03.005. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Mullan F. Workforce issues in health care reform: assessing the present and preparing for the future: hearings before the Senate Committee on Finance; 111th Cong, 1st Sess.2009. [Google Scholar]
- 7.Deal CL, Hooker R, Harrington T, Birnbaum N, Hogan P, Bouchery E, et al. The United States rheumatology workforce: supply and demand, 2005–2025. Arthritis Rheum. 2007;56:722–9. doi: 10.1002/art.22437. [DOI] [PubMed] [Google Scholar]
- 8.Ross AC, Polansky MN, Parker PA, Palmer JL. Understanding the role of physician assistants in oncology. J Oncol Pract. 2010;6:26–30. doi: 10.1200/JOP.091062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center for Workforce Studies. Recent studies and reports on physician shortages in the U.S. Washington: Association of American Medical Colleges; 2010. [Google Scholar]
- 10.He XZ, Cyran E, Salling M. National trends in the United States of America physician assistant workforce from 1980 to 2007. Hum Resour Health. 2009;7:86. doi: 10.1186/1478-4491-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Academy of Physician Assistants. Projected number of people eligible to practice as PAs and the number in clinical practice in 2007 through 2020. [cited 2010 Dec 31]. Available from: URL: http://www.aapa.org/images/stories/supplyprojectionsto2020.pdf.
- 12.Sokolowski JA, Banks CM, editors. Principles of modeling and simulation: a multidisciplinary approach. Hoboken (NJ): John Wiley – Sons, Inc; 2009. [Google Scholar]
- 13.Purcell PJ. Older workers: employment and retirement trends. Monthly Labor Review October 2000:19-30. [cited 2011 May 2]. Also available from: URL: http://www.bls.gov/opub/mlr/2000/10/art3full.pdf.
- 14.Kirch DG, Salsberg E. The physician workforce challenge: response of the academic community. Ann Surg. 2007;246:535–40. doi: 10.1097/SLA.0b013e3181571a39. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Physician Assistants. Alexandria (VA): American Academy of Physician Assistants; 2010. [cited 2011 May 2]. 2009 national physician assistant census report. Also available from: URL: http://www.aapa.org/images/stories/Data_2009/National_Final_with_Graphics.pdf. [Google Scholar]
- 16.Glicken AD, Lane S. Results of the PAEA 2006 survey of PA program expansion plans. J Physician Assist Educ. 2007;18:48–53. [Google Scholar]
- 17.Briggs A, Sculpher M. Sensitivity analysis in economic evaluation: a review of published studies. Health Econ. 1995;4:355–71. doi: 10.1002/hec.4730040502. [DOI] [PubMed] [Google Scholar]
- 18.Liang M. Physician Assistant Education Association. The 25th annual survey of physician assistant educational programs in the United States, 2008–2009. Alexandria (VA): Physician Assistant Education Association; 2010. [Google Scholar]
- 19.Bureau of Labor Statistics (US). Fastest growing occupations. 2008. [cited 2011 May 2]. Available from: URL: http://www.bls.gov/emp/ep_table_103.htm.
- 20.Jones PE, Repka M, Draper D, Orcutt V. Physician assistant faculty retirement intentions. J Physician Assist Educ. 2006;17:17–21. [Google Scholar]
- 21.Woodmanssee DJ, Hooker RS. Physician assistants working in the Department of Veterans Affairs. JAAPA. 2010;23:41–4. doi: 10.1097/01720610-201011000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Schofield DJ, Fletcher SL, Callander EJ. Aging medical workforce in Australia—where will the medical educators come from? Hum Resour Health. 2009;7:82. doi: 10.1186/1478-4491-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coplan B, Essary A, Virden T, Cawley JF, Stoehr J. Gender differences in salary among physician assistants. Women's Health Issues. In press. [DOI] [PubMed]
- 24.Marvelle K, Kraditor K. Do PAs in clinical practice find their work satisfying? JAAPA. 1999;12:43–4. 47, 50. [PubMed] [Google Scholar]
- 25.Hooker RS, Cawley JF, Leinweber W. Career flexibility of physician assistants and the potential for more primary care. Health Aff (Millwood) 2010;29:880–6. doi: 10.1377/hlthaff.2009.0884. [DOI] [PubMed] [Google Scholar]
- 26.Morgan PA, Hooker RS. Choice of specialties among physician assistants in the U.S. Health Aff (Millwood) 2010;29:887–92. doi: 10.1377/hlthaff.2008.0835. [DOI] [PubMed] [Google Scholar]
- 27.Jones PE, Cawley JF. Workweek restrictions and specialty-trained physician assistants: potential opportunities. J Surg Educ. 2009;66:152–7. doi: 10.1016/j.jsurg.2009.03.033. [DOI] [PubMed] [Google Scholar]
- 28.Cahill KE, Giandrea MD, Quinn JF. Washington: Department of Labor, Bureau of Labor Statistics (US); 2005. Are traditional retirements a thing of the past? New evidence on retirement patterns and bridge jobs. [Google Scholar]
- 29.Steinbrook R. Easing the shortage in adult primary care—is it all about money? N Engl J Med. 2009;360:2696–9. doi: 10.1056/NEJMp0903460. [DOI] [PubMed] [Google Scholar]
- 30.Morgan P, Strand de Oliveira J, Short NM. Physician assistants and nurse practitioners: a missing component in state workforce assessments. J Interprof Care. 2010:24. doi: 10.3109/13561820.2010.501917. epub ahead of print. [DOI] [PubMed] [Google Scholar]