Spatial analysis lies at the core of methods used to understand public health surveillance data, perhaps most famously employed by John Snow in the identification of the source of a cholera epidemic in 19th century London.1 Geographic distribution of disease is useful information not only because it can help identify the cause of an outbreak and suggest a means of interrupting the spread of disease, but also because understanding how the burden of disease aligns with political and bureaucratic borders assists in policy decisions and judicious allocation of resources. For sexually transmitted diseases, including human immunodeficiency virus (HIV), geographic distribution is especially salient because people tend to have sex with those who live close to them geographically.2
Spatial analysis by geopolitically defined areas (e.g., counties, towns, and cities) of HIV surveillance data is routinely performed and presented by the Centers for Disease Control and Prevention (CDC) and state and local health departments,3,4 and is used to inform HIV prevention, care, and treatment efforts at all levels of government. In New York City (NYC), several geographically focused HIV prevention efforts have been used to maximize the impact of public health resources. In June 2008, NYC launched The Bronx Knows HIV Testing Initiative, the city's largest attempt at municipal scale-up of routine HIV screening to date. The goal of The Bronx Knows is to ensure that every resident of the Bronx aged 13–64 years knows his or her HIV status. The Bronx was selected, in part, on the basis of a high proportional HIV-related mortality ratio compared with that of the other four NYC boroughs.5,6 In addition, condom distribution campaigns have been geographically focused on NYC neighborhoods with the highest HIV prevalence.7 Social marketing campaigns seeking to reach men who have sex with men (MSM) have concentrated a significant portion of their print media placement in bars and clubs in neighborhoods that have long been associated with gay men to maximize visibility among this priority population.
The finest level of geographic detail presented in NYC's HIV public health surveillance reports since the advent of HIV reporting in 2001 has been the United Hospital Fund (UHF) neighborhood, which divides the five boroughs of NYC into 42 areas.8 The populations of UHF neighborhoods range from 30,895 in Lower Manhattan to 477,516 in West Queens,3 and sizes of the populations of people living with HIV range from 131 in Bayside-Little Neck to 5,888 in Chelsea-Clinton.9 Using UHF neighborhood as the smallest unit of geospatial analysis, six to eight neighborhoods in the South and Central Bronx, Central Brooklyn, East and Central Harlem, and Southern Manhattan have been consistently identified as having borne the greatest burden of HIV both in terms of period HIV prevalence and HIV diagnosis rate.3,10,11
Although UHF neighborhood can be descriptive, the density and diversity of NYC's population, and the size and scope of its HIV epidemic, require a finer level of geographic detail to characterize the burden of HIV in NYC at a level comparable to analyses in most other U.S. cities. For example, the most populous UHF neighborhood, West Queens, has a population similar in size to that of Kansas City, Missouri,12 and a people-with-AIDS population that is larger than 26 of the 34 Ryan White Transitional Grant Areas.3,13
In 2008–2009, to provide the analysis necessary for more precise geographic targeting of HIV prevention and outreach efforts in NYC, we performed a geospatial analysis of NYC's HIV epidemic using UHF neighborhoods, but with greater precision and with a much finer level of geographic detail. Specifically, we used the X/Y coordinates of the residential address of people newly diagnosed with HIV and reported to the NYC Department of Health and Mental Hygiene (DOHMH) rather than using residential ZIP code to assign a UHF neighborhood. In addition to informing geographic targeting of prevention activities, we also performed this analysis to detect areas of NYC not previously recognized as having a relatively large burden of HIV disease.
METHODS
Data source
New York State requires named reporting of all diagnoses of HIV and acquired immunodeficiency syndrome (AIDS), all HIV-related illness, all positive western blot (WB) tests for HIV antibody, all viral load (VL) and CD4 values, and all HIV genotypes.14–16 The NYC HIV Registry is a population-based registry that has existed since 1981 and is continuously updated with new, de-duplicated diagnoses and laboratory results. Incoming diagnostic WB and VL reports from providers and laboratories that cannot be matched to an existing registry record initiate a field investigation to confirm through medical record review that the case meets surveillance definitions for HIV and/or AIDS,17 record data elements to be used to establish a date of diagnosis, and collect other data required for surveillance, including residential address.
Study population
People included in this analysis were newly diagnosed with HIV infection between January 1, 2007, and December 31, 2007, and reported to NYC DOHMH by September 30, 2008.
Geocoding of residential address
Residential address is one of the standard data elements submitted as part of legally mandated laboratory reporting of HIV in New York State; however, the quality of information for this variable tends to be poor. Beginning February 1, 2007, residential address at diagnosis was confirmed during field investigation through medical record review at the ordering provider's office. Prior to that time, only residential ZIP code was confirmed in this manner. Elements of residential address collected for surveillance purposes are street number, street name, city, state, and ZIP code. In 2007, case patients who were homeless were identified as such and classified as either sheltered homeless or undomiciled homeless if they were not residing in a shelter. Sheltered homeless people were assigned the coordinates and ZIP code of the shelter. The residential street address of undomiciled homeless case patients was left blank.
We performed several rounds of manual data cleaning to remove spelling errors and inconsistent formatting to maximize the proportion of valid NYC addresses that corresponded to a spatial coordinate. Addresses that were missing city and/or state, but had a NYC ZIP code, were assigned to that ZIP code. Addresses with missing ZIP code information were assigned the appropriate ZIP code corresponding to the information available. We resolved internal inconsistencies in address information through additional medical record review or review of the original handwritten form.
We matched all residential addresses with complete information from cases newly diagnosed in 2007 to their corresponding spatial coordinates using Geosupport Desktop Edition version 10.3.18 Case patients with residential addresses in the two ZIP codes that straddle the NYC border and adjoining counties (11001 and 11040) were assumed to reside outside NYC.
We attempted to verify whether geocoded addresses represented actual residential addresses by matching spatial coordinates of case patients’ residences to that of the more than 3,200 NYC providers’ offices, health facilities, and other organizations that have reported HIV cases to NYC DOHMH. This was done to eliminate instances in which the address of the facility of diagnosis was reported to us in place of the residential address. We also identified institutional addresses by using Geosupport's preprogrammed tool for identifying known NYC locations (e.g., City Hall). Addresses that corresponded to one of the 11 correctional facilities on Rikers Island in Queens were identified and excluded from subsequent parts of this analysis. These addresses correspond to patients whose address of origin upon incarceration could not be established during field investigation. Addresses were also excluded if they did not match to a spatial coordinate of a known address included in Geosupport 10.3.
Analysis
We determined HIV diagnosis dates by the earliest date among the following: date of physician diagnosis of HIV, date of first positive HIV WB test, and date of first detectable VL test.
We created a density map of residences of new HIV diagnoses in 2007 in NYC using a one-mile diameter with ArcGIS version 9.3.1 and the Spatial Analyst extension program.19 We removed major nonresidential areas of the city, such as Central Park and Kennedy International Airport, from the dispersion area available for depicting density of newly diagnosed HIV case patients. We visually depicted the magnitude of the geographic density of new diagnoses by dividing the range of values of cases per square mile into deciles and depicting increasing degrees of density with progressively lighter shades of gray on the map.
We compared this numerator-based geospatial representation of 2007 NYC new HIV diagnoses with the standard geographic depiction of NYC surveillance data for the same year, in which HIV diagnosis rates are shown using UHF neighborhood as the most discrete geographic unit. To create the standard map, we used the same data source for the number of new HIV diagnoses in 2007 per UHF neighborhood, and then divided by the appropriate population denominator from the 2000 U.S. Census to calculate the HIV diagnosis rate for each UHF neighborhood. We divided HIV diagnosis rates of UHF neighborhoods into quartiles, and depicted each with a progressively darker shade of gray according to magnitude.
We visually compared the new map with the standard map to detect any previously unrecognized geographic concentrations of new HIV diagnoses in NYC apparent at a macro level. Using the UHF neighborhood borders overlaid on the density map, we listed all the UHF neighborhoods where some portion of the three densest deciles lay (i.e., the lightest shades on the geocoded density map).
We compared this list with the UHF neighborhoods with diagnosis rates in the top quartile. We examined more closely UHF neighborhoods containing a dense area of new HIV diagnoses on the density map, but that were not among the UHF neighborhoods with the highest HIV diagnosis rates. We reexamined the density map to determine if high-density areas within its borders extended uninterrupted into a contiguous UHF neighborhood with known high HIV burden, or whether they appeared to represent a previously unrecognized geographic concentration of residences of new HIV case patients.
We further analyzed neighborhoods containing an apparent newly recognized concentration of residences of newly diagnosed HIV case patients to understand neighborhood trends in the annual number of new HIV diagnoses reported, and basic epidemiologic characteristics of case patients diagnosed in these areas. We limited our examination of trends to geographic areas that could be approximated with territories covered by ZIP codes, because residential addresses were not confirmed and geocoded for HIV diagnoses made prior to 2007.
RESULTS
A total of 3,787 case patients were newly diagnosed with HIV between January 1, 2007, and December 31, 2007, and reported to NYC DOHMH by September 30, 2008. Among these new diagnoses, 3,572 (94%) had a NYC ZIP code listed as part of their residential address at the time of diagnosis. Among these cases with NYC addresses, 390 (11%) were excluded from additional analysis, including 239 with a street address that we were not able to geocode, 69 that were missing street number and/or street name, 43 with an institution or correctional facility listed as their residential address, and 39 in which the case patient was homeless at the time of report. The residential addresses of the remaining 3,182 cases with a valid NYC address were matched to their corresponding spatial coordinates.
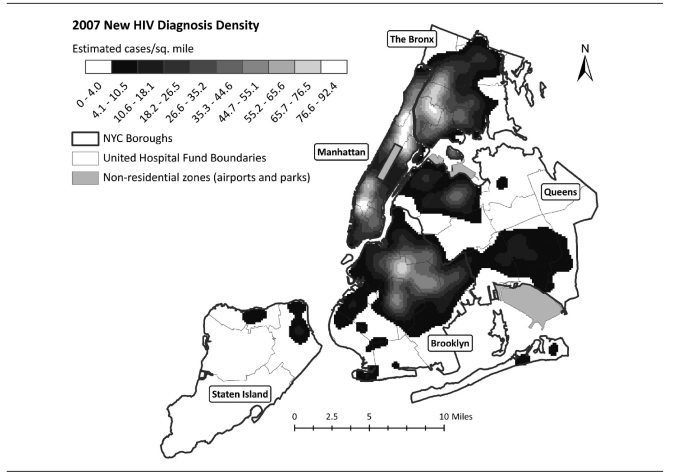
Figure 1 is a density map of newly diagnosed HIV case patients in 2007 in NYC based on the X/Y coordinates of their residential address at the time of diagnosis, with UHF neighborhood borders superimposed. The geographic density (i.e., number of case patient residences per square mile) is divided into deciles according to magnitude, with lighter shades representing areas with more case patient residences per square mile.
Figure 1.
Density surface map of residences of New Yorkers newly diagnosed with HIV infection in 2007a
aEstimated cases per mile can be measured by picking any point on the map and drawing a one-mile radius circle around that point. The legend reflects how many new diagnoses would then fall in that circle.
HIV = human immunodeficiency virus
Sq. = square
NYC = New York City
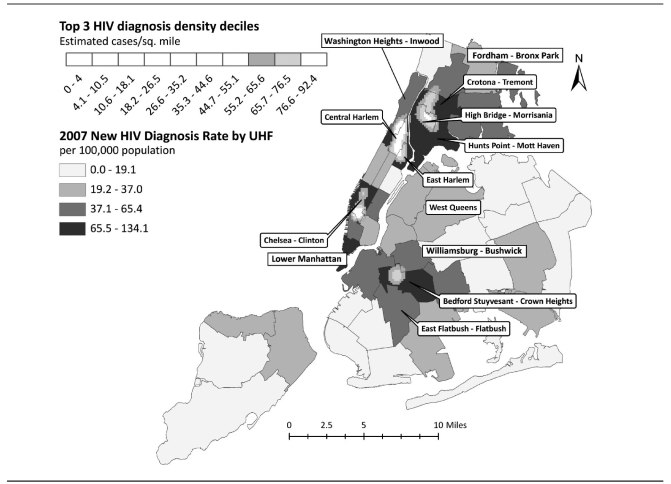
Figure 2 shows the densest areas (top three deciles) of 2007 HIV case patients’ residences overlaid on the standard map of HIV diagnosis rate per 100,000 population by UHF neighborhood in 2007. It also highlights the eight UHF neighborhoods in the upper quartile of HIV diagnosis rates per 100,000 population in 2007. Four continuous high-density geographic areas that cross UHF neighborhood borders are visible. The northernmost high-density area is mostly within the Bronx UHF neighborhoods of High Bridge-Morrisania and Crotona-Tremont, but reaches into Hunts Point-Mott Haven and Fordham-Bronx Park. Just south of this high-density area is another area that spreads across three northern Manhattan UHF neighborhoods: East Harlem, Central Harlem-Morningside Heights, and Washington Heights-Inwood. A third high-density area is located almost entirely within the Southern Manhattan UHF neighborhood of Chelsea-Clinton, with slight overlap into three bordering UHF neighborhoods. The southernmost high-density area is in Brooklyn, within the UHF neighborhood of Bedford Stuyvesant-Crown Heights, with a small portion extending into Williamsburg-Bushwick.
Figure 2.
New York City HIV diagnosis rates per 100,000 population in 2007 by United Hospital Fund neighborhood, superimposed with density surface map of residences of New Yorkers newly diagnosed with HIV infection in 2007 (top three deciles only)a
aEstimated cases per mile can be measured by picking any point on the map and drawing a one-mile radius circle around that point. The legend reflects how many new diagnoses would then fall in that circle.
HIV = human immunodeficiency virus
Sq. = square
NYC = New York City
UHF = United Hospital Fund
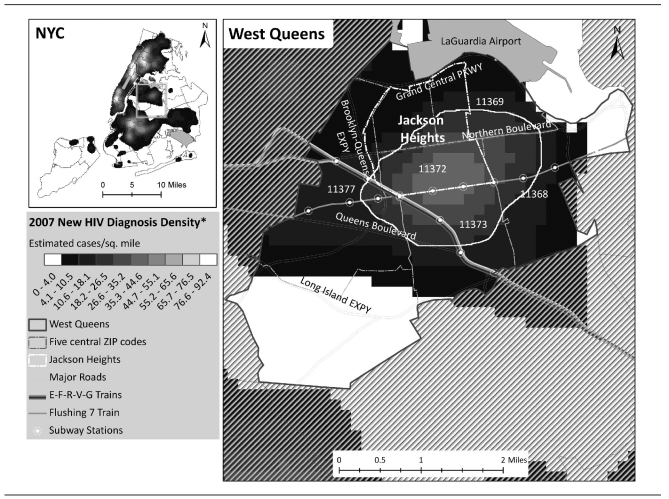
No previously unrecognized UHF neighborhoods were identified that wholly contained a collection of new HIV diagnoses that met our criteria for high density. However, we did observe a relatively dense area in the middle of the UHF neighborhood of West Queens (Figure 3) that is visually notable because of the contrast it strikes with the surrounding area. Although nowhere does its density reach the top three deciles and, thus, meet our criteria for high density, its structure appears similar to the four major geographic foci described previously (identifiable on Figure 2 as the four areas in which the top three deciles of the density map are overlaid), including a less dense “rim” surrounding an increasingly dense “core.”
Figure 3.
Density surface map of residences of New Yorkers newly diagnosed with HIV infection in 2007, with West Queens neighborhood detail mapa
aThe roughly circular area outlined in gray is a previously unrecognized geographically clustered group of residences of newly diagnosed HIV case patients who share similar demographic characteristics and reported HIV transmission risk. This epidemiologically significant concentration of case patient residences was not apparent in standard geographic representations of New York City's HIV epidemic, which are based on HIV diagnosis rate by United Hospital Fund neighborhood.
HIV = human immunodeficiency virus
NYC = New York City
Sq. = square
The geographic area depicted in the detail map in Figure 3 is approximately 2.5 square miles, and located mostly in the neighborhood of Jackson Heights. Using the 2000 U.S. Census population totals for the 38 census tracts that are the closest geographic match to this area as the numerator,20 the mean population density of this area is 83,400 people per square mile; it is more densely populated than Manhattan (66,900 people per square mile), NYC overall (26,400 people per square mile),21 and the U.S. as a whole (80 people per square mile).22 Six major subway lines intersect in this area, which is bounded by four major highways. This Jackson Heights concentration of HIV case patient residences lies mostly within the area covered by ZIP code 11372, but portions lie in the ZIP code areas 11368, 11369, 11373, and 11377. Overall, Jackson Heights residents are 62% Hispanic23 and 63% foreign-born;24 this percentage is far higher than the proportion of New Yorkers overall who are Hispanic (28%)25 or foreign-born (39%).26
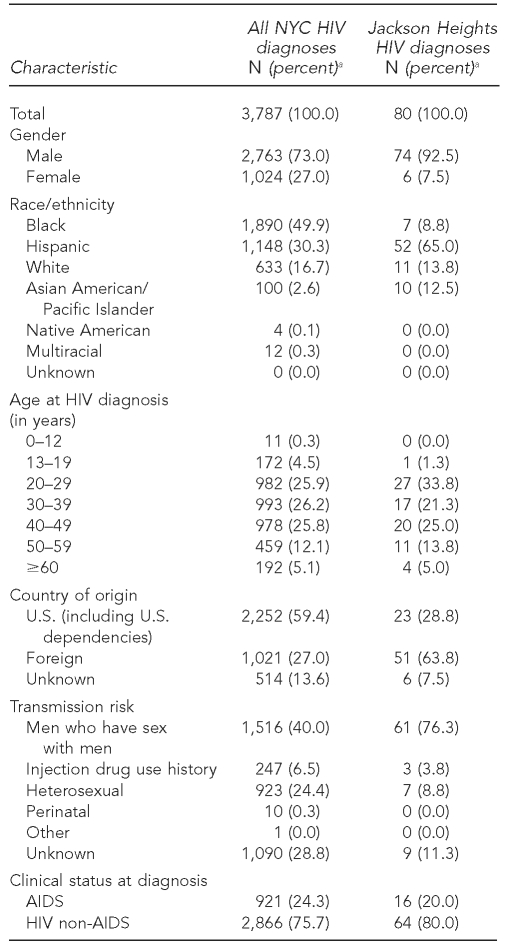
There were 80 newly diagnosed HIV case patients residing in the Jackson Heights area of interest depicted in Figure 3 at the time of their diagnosis in 2007. Seventy-four (93%) case patients were male, 52 (65%) were Hispanic, 51 (64%) were foreign-born, and 28 (35%) were younger than 30 years of age at the time of diagnosis (Table). Of the 74 male case patients, 61 (76%) reported a history of sex with a man. A diagnosis of AIDS was made at the same time as the new HIV diagnosis in 16 (20%) of the case patients. Compared with 2007 new HIV diagnoses citywide, people newly diagnosed and residing in this area of Queens were more likely to be male, Hispanic, <30 years of age, and foreign-born. A greater proportion of the newly diagnosed men residing in this area of Queens reported sex with men compared with newly diagnosed men citywide (82% vs. 55%)
Table.
Characteristics of HIV case patients newly diagnosed in 2007 in New York City: citywide and in the Jackson Heights area of interest
aPercentages do not always total 100 due to rounding.
NYC = New York City
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
We examined HIV disease trends in the five-ZIP-code area that roughly approximates the location of the Jackson Heights collection of HIV diagnoses to understand whether or not this geographic concentration of HIV burden is a new or longstanding phenomenon. In 2007, 145 new HIV diagnoses were made among residents of ZIP codes 11372, 11368, 11369, 11373, and 11377, similar to the number (n=144) reported in 2003 among residents of these same five ZIP codes. The lowest total reported during 2003–2007 from this five-ZIP-code area was in 2005 (n=118). The demographic composition of case patients was stable during this time; each year, more than three-quarters of case patients were male, more than 60% were Hispanic, and at least half were foreign-born. The proportion of newly diagnosed men residing in this area who reported a history of sex with another man as their HIV transmission risk increased between 2003 and 2007, from 58% to 77% (data not shown).
DISCUSSION
Rates are the standard epidemiologic measure for comparing burden of disease among geographic areas; however, rates can obscure small but significant concentrations of disease burden, particularly when the geographic area is densely populated and diverse, such as many areas of NYC. We used geocoded residential address data from new HIV diagnoses in NYC's HIV surveillance registry to measure the geographic distribution of HIV burden in NYC at a finer level of detail, compared it with standard maps based on HIV diagnosis rates, and found one previously unrecognized geographically clustered group of residences of newly diagnosed HIV case patients who shared very similar demographic characteristics and reported HIV transmission risk. This epidemiologically significant concentration of case patient residences was not apparent in standard geographic representations of NYC's HIV epidemic, which are based on HIV diagnosis rate by UHF neighborhood, despite the fact that it appears to be a longstanding feature of the geography of HIV in NYC, based on our retrospective analysis of neighborhood data using the corresponding ZIP code-based area.
These Jackson Heights case patients reflect, in one geographic focus, many important trends in the HIV epidemic in NYC and nationwide: an increasing proportion of foreign-born case patients;27 an increasing proportion of men and MSM among those newly diagnosed;28,29 and, more specifically, increasing numbers of new diagnoses among young, foreign-born Hispanic males.30
The identification of this geographic collection and the characteristics that make it distinct from NYC as a whole has been useful for local HIV prevention efforts. Based in part on these data, NYC DOHMH began funding new HIV risk-reduction interventions that focus on Latino MSM in Queens, with an emphasis on Jackson Heights. In 2009, more than 10,000 peer-delivered, risk-reduction messaging contacts were made among MSM in Queens through an evidence-based, community-level intervention called MPowerment (Unpublished data, NYC DOHMH, Bureau of HIV Prevention Program, Research, Evaluation and Monitoring Unit, 2009). Prevention programming in this area has been tailored to meet the needs of a diverse population, including non-English speakers and recent immigrants, and varying cultural approaches to male-male sexual activity.
In 2010, a field-based HIV prevention specialist was transferred to Queens from another unit in NYC DOHMH and assigned to strengthening partnerships between clinical and community-based organizations there, especially those involved in condom distribution, HIV testing, and peer-delivered risk-reduction outreach and education in Jackson Heights. Plans for 2011 include expanding the use of a social network strategy among Latino MSM in Jackson Heights to increase HIV testing and linkage to HIV primary care and support services; dissemination of social marketing messaging, delivered in Spanish and focusing on Latino MSM; and delivery of syringe services for injection drug users.
Limitations
Although we found an important new collection of newly diagnosed HIV case patients through density mapping, it is important to remain aware of the limitations of epidemiologic analysis that does not take a population denominator into account. We estimated the population denominator of the 2.5-square-mile area of Jackson Heights to be approximately 250,000, which, if used to determine a diagnosis rate, would be lower than the HIV diagnosis rate in NYC overall.3 We did not attempt to use statistical techniques to quantify the strength of spatial autocorrelation such as Moran's I, so we could not define this collection of new HIV diagnoses as a true geographic cluster. Our primary goal in this analysis was to inform planning of local prevention activities, and we found that we were able to provide valuable information for prevention planning by simply creating this higher-resolution map and comparing it with our standard map.
We do not know how many of the Jackson Heights diagnoses represented recent infections. The proportion of Jackson Heights patients given concurrent HIV and AIDS diagnoses was lower than the proportion citywide, which suggests that they were diagnosed relatively early in the course of their infection. Nonetheless, it is possible that some Jackson Heights patients were infected with HIV years before moving to this neighborhood.
Another potential limitation of our analysis was the lack of durability of residential address as a measure of where HIV case patients live, given the likelihood that a young, urban, foreign-born population will change residences frequently.
CONCLUSION
Identification of the Jackson Heights concentration of HIV disease burden underscores the importance of geospatial analyses with finer resolution than has customarily been available, particularly in densely populated areas. Other large cities and densely populated areas using these same methods may find similar geographic concentrations of HIV diagnoses among groups distinct from the wider HIV-infected population. NYC plans to incorporate density mapping of new HIV diagnoses into its panel of routine analyses of HIV surveillance data.
Acknowledgments
The authors thank Monica Sweeney, Kent Sepkowitz, Chris Goranson, Ellen Wiewel, David Hanna, and the Bureau of HIV Epidemiology and Field Services public health advisers. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
Footnotes
This analysis was supported in part by Centers for Disease Control and Prevention (CDC) cooperative agreements #5U62PS001026-03 and #5U38HM000414.
REFERENCES
- 1.Snow J. On the mode of communication of cholera. 2nd ed. London: John Churchill; 1855. [Google Scholar]
- 2.Rothenberg R, Muth SQ, Malone S, Potterat JJ, Woodhouse DE. Social and geographic distance in HIV risk. Sex Transm Dis. 2005;32:506–12. doi: 10.1097/01.olq.0000161191.12026.ca. [DOI] [PubMed] [Google Scholar]
- 3.New York City Department of Health and Mental Hygiene. HIV Epidemiology and Field Services semiannual report, vol. 4 no. 2. New York: NYC DOHMH; 2009. [cited 2011 May 9]. Also available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/dires-2009-report-semi2.pdf. [Google Scholar]
- 4.Centers for Disease Control and Prevention (US) HIV surveillance report, 2008: rates of diagnoses of HIV infection, 2008—37 states and 5 U.S. dependent areas. [cited 2011 May 9]. Available from: URL: http://www.cdc.gov/hiv/topics/surveillance/resources/slides/2008report_tables/slides/HASR_19.pdf.
- 5.New York City Department of Health and Mental Hygiene, Bureau of Vital Statistics. Summary of vital statistics 2007: the city of New York. [cited 2011 May 9]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/vs/2007sum.pdf.
- 6.New York City Department of Health and Mental Hygiene. Health department launches Bronx-wide HIV testing initiative [press release]; 2008 Jun 26. [cited 2011 May 10]. Available from: URL: http://www.nyc.gov/html/doh/html/pr2008/pr045-08.shtml.
- 7.Renaud TC, Bocour A, Irvine MK, Bernstein KT, Begier EM, Sepkowitz KA, et al. The free condom initiative: promoting condom availability and use in New York City. Public Health Rep. 2009;124:481–9. doi: 10.1177/003335490912400404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New York City Department of Health and Mental Hygiene. New York City United Hospital Fund neighborhoods and NYC ZIP code areas. 2006. [cited 2011 May 10]. Available from: URL: http://home2.nyc.gov/html/doh/downloads/pdf/survey/uhf_map_100604.pdf.
- 9.HIV Epidemiology and Field Services Program. New York City HIV/AIDS annual surveillance statistics 2008. New York: New York City Department of Health and Mental Hygiene; 2009. [cited 2011 May 10]. Also available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2008_tables_all.pdf. [Google Scholar]
- 10.New York City Department of Health and Mental Hygiene HIV Epidemiology and Field Services semiannual report vol 3 no. 2. New York: NYC DOHMH; 2008. [cited 2011 May 10]. Also available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/dires-2008-report-semi2.pdf. [Google Scholar]
- 11.New York City Department of Health and Mental Hygiene. HIV Epidemiology and Field Services semiannual report vol. 2 no. 2. New York: NYC DOHMH; 2007. [cited 2011 May 10]. Also available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/dires-2007-report-semi2.pdf. [Google Scholar]
- 12.Census Bureau (US) Population estimates: incorporated places and minor civil divisions—places over 100,000: 2000 to 2008. [cited 2011 May 10]. Available from: URL: http://www.census.gov/popest/cities/SUB-EST2008.html.
- 13.Centers for Disease Control and Prevention (US) HIV/AIDS data through December 2006 provided for the Ryan White HIV/AIDS Treatment Modernization Act of 2006, for fiscal year 2008. [cited 2011 May 10];HIV/AIDS Surveill Supp Rep. 2009 14:11–2. Also available from: URL: http://www.cdc.gov/hiv/surveillance/resources/reports/2009supp_vol14no1/index.htm. [Google Scholar]
- 14.New York State Law, Title III, Art. 21, Public Health Law §§2130-2139.
- 15.New York State Law, Art 27-F, Public Health Law §§ 2780-2787. [cited 2011 May 10]. Also available from: URL: http://public.leginfo.state.ny.us/LAWSSEAF.cgi?QUERYTYPE=LAWS*&QUERYDATA=@SLPBH0A27-F*&LIST=LAW*&BROWSER=EXPLORER*&TOKEN=16763516*&TARGET=VIEW.
- 16. New York State Code of Administrative Rules and Regulations, 10 NYCRR 63.4 (2010)
- 17.Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep. 2008;57(RR-10):1–12. [PubMed] [Google Scholar]
- 18.Department of City Planning of the City of New York. Geosupport Desktop Edition: Version 10.3, Release 07C. New York: Department of City Planning of the City of New York; 2009. [Google Scholar]
- 19.ESRI. ArcGIS and the Spatial Analyst extension program: Version 9.3.1. Redlands (CA): ESRI; 2009. [Google Scholar]
- 20.Census Bureau (US) Census 2000, summary file 1; GCT-PH1 population, housing units, area, and density—Queens County, New York—census tract. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 21.Census Bureau (US) New York: 2000 population and housing unit counts—2000 census of population and housing. Washington: Census Bureau, Department of Commerce, Economics and Statistics Administration (US); 2003. [cited 2011 May 10]. Also available from: URL: http://www.census.gov/prod/cen2000/phc-3-34.pdf.
- 22.Census Bureau (US) Census 2000, summary file 1: GCT-PH1 population, housing units, area, and density 2000—United States and Puerto Rico. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 23.Census Bureau (US) 2006–2008 American Community Survey: demographic and housing estimates: PUMA5 04102, New York, NY. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 24.Census Bureau (US) 2006–2008 American Community Survey: selected social characteristics in the United States: PUMA5 04102, New York. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 25.Census Bureau (US) 2006–2008 American Community Survey: demographic and housing estimates: 2006–2008, New York, NY. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 26.Census Bureau (US) 2006–2008 American Community Survey: selected social characteristics in the United States: New York, NY. [cited 2010 Sep 16]. Available from: URL: http://factfinder.census.gov.
- 27.Wiewel E, Nasrallah H, Hanna D, Shepard C, Torian L, Begier E. HIV diagnosis and care initiation among foreign-born persons in New York City, 2001–2007. Abstract presented at the 16th Conference on Retroviruses and Opportunistic Infections; 2009 Feb 8–11; Montreal. [Google Scholar]
- 28.Trends in HIV/AIDS diagnoses among men who have sex with men—33 states, 2001–2006. MMWR Morb Mortal Wkly Rep. 2008;57(25):681–6. [PubMed] [Google Scholar]
- 29.New York City Department of Health and Mental Hygiene. HIV Epidemiology and Field Services semiannual report vol. 4 no. 1. New York: NYC DOHMH; 2009. [cited 2011 May 10]. Also available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/dires-2009-report-semi1.pdf. [Google Scholar]
- 30.Espinoza L, Hall HI, Selik RM, Hu X. Characteristics of HIV infection among Hispanics, United States 2003–2006. J Acquir Immune Defic Syndr. 2008;49:94–101. doi: 10.1097/QAI.0b013e3181820129. [DOI] [PubMed] [Google Scholar]