Abstract
In 1998, Medicare adopted a per diem Prospective Payment System (PPS) for skilled nursing facility care, which was intended to deter the use of high-cost rehabilitative services. The average per diem decreased under the PPS, but because per diems increased for greater therapy minutes, the ability of the PPS to deter the use of high-intensity services was questionable. In this study, we assess how the PPS affected the volume and intensity of Medicare services. By volume we mean the product of the number of Medicare residents in a facility and the average length-of-stay, by intensity we mean the time per week devoted to rehabilitation therapy. Our results indicate that the number of Medicare residents decreased under PPS, but rehabilitative services and therapy minutes increased while length-of-stay remained relatively constant. Not surprisingly, when subsequent Medicare policy changes increased payment rates, Medicare volume far surpassed the levels seen in the pre-PPS period.
Keywords: Provider reimbursement, Prospective payment, Medicare, Skilled nursing facility
Medicare and other payers are moving toward global or bundled payments to control costs and improve efficiency in health care delivery. Global payments are “prospective,” denoting that revenue is specified (not paid) in advance, and is disconnected, at least in part, from costs incurred. The ultimate bundle is capitation – a per person per year payment – but bundled payment is applied as well to hospital discharges, episodes of specialty care, and other areas.1 Medicare instituted a bundled payment for skilled nursing facilities (SNFs), referred to as the Prospective Payment System (PPS), in 1998 after seeing massive cost increases under the former cost-based reimbursement system. Indeed, over the period 1989 through 1996, Medicare SNF expenditures increased over 300% from $2.8 billion to $11.3 billion (U.S. General Accounting Office, 1997). The purpose of this paper is to describe Medicare’s PPS, evaluate its incentives towards controlling Medicare SNF utilization and expenditures, and investigate the response of SNFs in terms of volume and intensity.
Like the diagnosis-based PPS Medicare uses to pay hospitals, the SNF PPS is not a pure prospective payment system. Indeed, the “prospective” word in the PPS title may belong in quotes, because the SNF payment system is a per diem payment with adjustments for intensity of care. Nonetheless, the SNF PPS has distinct incentives from a cost-based system, which may affect the volume and intensity of care in SNFs. Payment may be one potential mechanism for lowering the high rate of Medicare SNF cost growth. Several previous studies have evaluated the PPS using data from the SNF PPS demonstration, pre-post data around the introduction of PPS, and panel data using non-Medicare patients as a control for unrelated time series variation. This paper combines these different identification strategies by exploiting both participation in the CMS demonstration, pre/post variation around the timing of the rule changes and Medicare payer status. Using both national facility-level data and person-level admission data specific to New York State, we employ both “differences-in-differences” (DD) and “differences-in-differencesin-differences” (DDD) approaches to examine the implications of the adoption of the SNF PPS for Medicare volume and intensity of services. We measure volume by the average number of Medicare residents in a facility and the average length of stay, and intensity by the time per week devoted to rehabilitation therapy. We find that the shift to PPS reduced the average number of Medicare residents in the facility, but increased the intensity of service use. Not surprisingly, when subsequent Medicare policy changes increased payment rates, overall Medicare utilization far surpassed the levels seen in the pre-PPS period.
Background and Literature Review
The nursing home sector has undergone a remarkable transformation over the past two decades. In the 1970s and early 1980s, nursing homes largely provided chronic care services to long-stay residents. The post-acute, rehabilitative side of the nursing home market was negligible, with Medicare, the primary payer for these services, accounting for only 1.7% of total nursing home expenditures in 1980 (National Center for Health Statistics, 2005). With the adoption of Medicare prospective payment for hospital care in 1983, the SNF sector was positioned to accept those discharged “sicker and quicker” from the hospital (U.S. General Accounting Office, 2002). However, the relatively stringent interpretation of SNF coverage and eligibility criteria temporarily held SNF growth in check. When these coverage and eligibility criteria were relaxed in the late 1980s, the SNF sector grew rapidly.
Under a cost-based payment methodology, the SNF expansion occurred along both the extensive and intensive margins. The number of people receiving care in SNFs almost doubled, from 636,000 in 1989 to 1.1 million in 1996 (U.S. General Accounting Office, 1997). Although the average length of a Medicare-covered SNF stay did not change much over that period, the average Medicare payment per day almost tripled from $98 in 1990 to $292 in 1996. Room and board and administrative overhead were subject to limits, but the cost-based rules put few limits on payments for ancillary services and capital-related costs. Ancillary services, such as physical and occupational therapy, were only subject to medical necessity criteria, and relatively little review of their use was done by Medicare. Thus, the cost-based system offered no incentive to provide only clinically necessary services or deliver them efficiently. Former CMS Administrator Bruce Vladeck labeled this financial opportunity for nursing homes as “a hole in Medicare policy through which one could drive a truck” (Lagnado, 2002).
In 1998, Medicare adopted a PPS for nursing home care in order to attempt to curb spending on SNF services (see Table 1 for a summary of Medicare SNF payment changes). Facilities are paid a fixed amount per day, with adjustments for health status and services delivered using the 44 payment categories in the Resource Utilization Group III (RUG-III) system.2 The RUG groups include rehabilitation therapy categories (14 RUGs, 75–80% of admissions), skilled or extensive services (12 RUGs, approximately 20% of admissions) and custodial care services (18 RUGs, <2% of admissions). The PPS was not intended to be budget neutral and the Congressional Budget Office projected savings of $1.2 billion in 1999 from the 1998 total of more than $13 billion (Lewin Group, 2000). However, expenditures actually decreased by over $2 billion (Medicare Payment Advisory Commission, 2003), which led to widespread financial distress and some bankruptcy in the nursing home industry, particularly among hospital-based and chain facilities. About 20 percent of hospital-based nursing facilities had exited the market by 2000 (Dalton & Howard, 2002; Medicare Payment Advisory Commission, 2002).
Table 1.
Summary of Major Changes to the Medicare Skilled Nursing Facility Payment System (1996–2004)
| Timing | Change |
|---|---|
| Start of facility fiscal year on/after July 1, 1998 | Adoption of per diem prospective payment system, which uses Resource Utilization Groups (RUGs) to place residents into payment categories |
| April 1, 2000 | Balanced Budget Refinement Act (BBRA) provided a 20% increase in 12 RUGs dealing with "complex care", and 3 of the rehabilitation RUGs (RHC; RMC; RMB); 4% increase for other RUGs |
| April 1, 2001 | Benefits Improvement and Protection Act (BIPA) provided 16.6% increase for nursing component; removed the 20% BBRA increase for the three rehabilitation RUGs; and, provided a 6.7% increase for all 14 rehabilitation RUGs |
| September 30, 2002 | The 16.6% nursing increase under BIPA expired |
Given concerns about the financial viability of the industry, the Balanced Budget Refinement Act (BBRA) of 1999 increased the federal payment rates by 20 percent in 15 of the groups where rates were thought to be most problematic (the 12 “complex care” RUG groups plus three of the rehabilitation RUG groups) and 4 percent in all other RUG groups, effective in April 2000. The following April, in the Benefits Improvement and Protection Act of 2000 (BIPA), the Congress altered the payment increase mandated by BBRA such that all 14 rehabilitation RUG–III groups, including those previously receiving the 20 percent BBRA increase, would receive an additional 6.7 percent payment increase until CMS announced a refinement to the classification system. BIPA also provided a 16.6% increase for the nursing component of the rate, which expired in September 2002.
A key issue of interest is how these Medicare SNF payment changes affected the volume and intensity of Medicare services. A large literature examines the implications of the shift to Medicare PPS among hospitals (e.g., Kosecoff et al., 1990). However, by comparison, relatively few studies have examined this issue in relation to the SNF PPS. To date, three sets of analyses have considered the implications of the SNF PPS on the volume and intensity of SNF services. First, prior to the national rollout, a CMS demonstration evaluated the implications of the PPS in six states, Kansas, Maine, Mississippi, New York, South Dakota and Texas. The voluntary demonstration compared pre-post outcomes among participating facilities transitioning to PPS versus non-participating facilities still under cost-based reimbursement (Abt Associates, 2002). Under the assumption that non-participating facilities are a good comparison for facilities that volunteered to participate in the demonstration, the evaluation found that Medicare admissions to participating facilities grew less rapidly in nearly every state than did admissions in non-participating facilities. However, admissions to the “upper” rehabilitation RUG-III groups increased particularly rapidly. A potential limitation of the SNF PPS demonstration is that the facilities that chose to enroll in the demonstration may have been different than their non-participating counterparts (e.g., facilities that were well-positioned to benefit from prospective payment).
Medicare payment changes have also been evaluated by a simple pre-post analysis. White (2003) found the average SNF length-of-stay was relatively constant between 1997 (23.8 days) and 2000 (22.9 days). Similarly, he found a decrease in overall Medicare SNF days from 42 million in 1997 to 36.9 million in 2000. In a report to Congress, the General Accounting Office (2002) found that the RUG groups that underwent a 20% payment increase under the BBRA had an 11% increase in the share of Medicare patients, while those other RUG groups unaffected by the rule change generally experienced a decline in Medicare share. A potential limitation with this approach is the lack of a comparison group. That is, it is impossible to know whether some other unobserved factor changed over the period of study.
A final approach to evaluating the SNF PPS has been to compare the intensity of service use across Medicare and private-pay residents over time. The idea here is that private-pay residents serve as a valid comparison group for any unrelated time series variation that may occur over the PPS implementation period. Using data from Michigan and Ohio, Wodchis (2004) found the PPS increased the odds (OR = 1.33) of receiving therapy for Medicare residents relative to their private-pay counterparts, but conditional on the receipt of any therapy, the PPS led Medicare residents to receive 7% less weekly therapy time than those in the reference group. When these two parts of the model were combined, a 4% differential decrease in therapy use across Medicare and private-pay residents was observed. A potential limitation with this approach is that private-pay residents may have been affected by the SNF PPS. For example, research suggests that the SNF PPS impacted the quality of care for long-stay (Medicaid and private-pay) nursing home residents (Konetzka, Norton, & Stearns, 2006).
Conceptual Framework
Our conceptual framework is adapted from the hospital payment literature on incentives and “supply response” which derives the implications of various payment systems for intensity (or sometimes “quality”) of care and for provider volume (Hodgkin & McGuire, 1994; Ma, 1994; McClellan, 1997). The supply response literature assumes that profit is among the arguments of a provider’s objective function. This assumption is reasonable in the SNF industry where roughly two-thirds of nursing homes are for-profit. We are interested in three outcomes: number of discharges, length of stay, and the time per week devoted to rehabilitation therapy which we refer to as “intensity.”3
The SNF PPS is structured around a per diem payment for a particular RUGs classification based on health conditions (e.g., disability, pneumonia, depression, need for assistance with activities of daily living). For the rehabilitation therapy RUGs that constitute roughly 70% of all SNF cases, payments also depend on the total amount of weekly therapy time. Individuals are categorized into “low” (45–149 minutes/week), “medium” (150–324 minutes/week), “high” (325–499 minutes/week), “very high” (500–719 minutes/week) and “ultra high” (720+ minutes/week) rehabilitation categories based on the total amount of physical, occupational and speech therapy, with higher per diems associated with more intensive therapy.
Demand and cost conditions factor into the incentives of a payment system. Suppose the benefits of a stay in a SNF for a representative consumer depend on the length of stay, L, and the intensity of services provided during the stay, e: B(L, e), L, e > 0. We assume that BL(0,e) > 0, BLL < 0, Be > 0, Bee < 0. These assumptions imply that benefits increase initially with L, but at some point longer stay can reduce benefits. Intensity (more services) is always valued positively, though with diminishing marginal benefit. Assume that consumers pay nothing for a stay in a SNF and the demand for the number of SNF “discharges” is N(B(L,e)), with N’ > 0. Let c(e) be the cost per day of providing intensity of services e. c’ > 0. Suppose c can depend continuously on e with well-defined and continuous derivatives.
The SNF payment system is per diem. This per diem is prospective, but is conditioned on e, so the per diem payment is p(e), p’ > 0. Assume also here that p depends continuously on e. We characterize incentives for a typical clinical condition. Profit to a nursing home is:
| (1) |
Letting the nursing home choose L and e, we have the two first-order conditions for profit maximization4:
| (2) |
| (3) |
At this point we can draw some implications for SNF PPS effects.5 Consider (2). The number of discharges N must be positive. For (2) to be satisfied, the LN’BL term must be negative, which implies that BL < 0. In other words, this payment system pushes SNFs to hold patients past the point at which the marginal benefit of an extra day falls to zero. From (3) we can observe that because (p(e) − c(e))(LN’Be) is positive, p’ – c’ must be negative in profit maximization. This will be satisfied easily when p is a step function with ranges of p’ = 0. The first-order effect of increasing payment generosity is to raise (p–c) implying from (3) that e increases and at least Be must fall. Thus, as generosity increases, we expect e to increase. The effect on N and L is ambiguous, although we know they must move in opposite directions because the marginal benefit of L is less than zero in profit maximization (from (2)).
Data
The empirical work utilizes both facility-level data drawn from all U.S. nursing homes for the period 1996 through 2005 and resident-level data drawn from all New York State nursing homes for the period 1998 through 2004. The source of facility-level data, the Online Survey Certification and Reporting (OSCAR) system, contains information from state surveys of all federally certified Medicaid (nursing facilities) and Medicare (skilled nursing care) homes (see Table 2). Collected and maintained by the CMS, the OSCAR data determine compliance with federal regulatory requirements. Every facility is required to have an initial survey to verify compliance. Thereafter, states are required to survey each facility no less often than every 15 months, and the average is about 12 months (Harrington, Swan, Wellin, Clemena, & Carrillo, 1999). OSCAR variables include nursing home ownership, structure and staffing information, the type and scope of regulatory deficiencies, and the availability of various services. A profile of residents in the nursing home on the day of the inspection is provided which includes information on number of residents (by payer category), functional deficits, nursing care needs, and receipt of “high tech” nursing care. We also use facility-level data from the cost reports that all freestanding and hospital-based SNFs must submit each year to CMS. These reports contain information necessary to calculate pre-PPS reimbursement levels and post-PPS reimbursement payment rates by RUG.
Table 2.
Summary statistics: National estimates (N= 17,554 facilities)
| Mean | Std. Dev. | |
|---|---|---|
| Outcomes | ||
| Medicare residents | 12.82 | 17.49 |
| Medicare share | 0.11 | 0.13 |
| Payment Policies | ||
| PPS: All surveys following start of facility FY post 1/1/98 | 0.68 | 0.47 |
| BBRA: All surveys post 4/1/00 | 0.54 | 0.50 |
| BIPA1: All surveys post 4/1/01 | 0.43 | 0.50 |
| BIPA2: All surveys post-10/1/02 | 0.26 | 0.44 |
| Facility-Level Covariates | ||
| Hospital-based facility | 0.55 | 0.23 |
| Chain member facility | 0.56 | 0.50 |
| For-profit owned facility | 0.68 | 0.47 |
| Nonprofit owned facility | 0.26 | 0.44 |
| Government-owned facility | 0.06 | 0.24 |
| Less than 50 beds | 0.04 | 0.19 |
| 50–99 beds | 0.23 | 0.42 |
| 100–149 beds | 0.36 | 0.48 |
| 150–199 beds | 0.19 | 0.39 |
| 200 or more beds | 0.20 | 0.40 |
The source of resident-level data is the Minimum Data Set (MDS), a federally mandated assessment for all nursing home residents that includes approximately 400 data elements, including demographics, diagnoses, treatments and measures of both physical and cognitive function (see Table 3) (Hawes et al., 1995; Morris et al., 1990). The MDS is collected for all new admissions and then (at least) quarterly thereafter. Importantly, the MDS is the instrument used by Medicare to assign individuals into different RUGs for the purposes of payment. In our analyses, we only include the first MDS admission assessment over our period of study. Previous research suggests a high rate of “churning” among SNF patients between the SNF, the community and the hospital (Mor, Intrator, Feng, & Grabowski, 2010). We exclude subsequent SNF admissions (roughly 27% of all admissions) to avoid potential bias due to prior treatment in the SNF.
Table 3.
Summary statistics: New York (N=496,049 individuals)
| Mean | Std. Dev. | |
|---|---|---|
| Outcomes | ||
| Rehabilitation resource utilization groups (RUGs) | 0.75 | 0.43 |
| High rehabilitation RUGS | 0.13 | 0.34 |
| BBRA 20% payment RUGs | 0.16 | 0.37 |
| Therapy minutes | 289.34 | 255.85 |
| Discharge within 20 days | 0.23 | 0.42 |
| Discharge within 90 days | 0.69 | 0.46 |
| Policy periods | ||
| PPS: Demo admissions pre-1/1/99 & all admissions post-1/1/99 | 0.97 | 0.17 |
| BBRA: All admissions post 4/1/00 | 0.74 | 0.44 |
| BIPA1: All admissions post 4/1/01 | 0.60 | 0.49 |
| BIPA2: All assessments post-10/1/02 | 0.37 | 0.48 |
| Payment | ||
| Medicare SNF per diem ($2010) | $375.30 | $79.43 |
| Person-Level Covariates | ||
| Medicare SNF Part A admission | 0.59 | 0.49 |
| Medicaid admission (if no Medicare SNF coverage) | 0.16 | 0.36 |
| Other payer admission (if no Medicare SNF coverage) | 0.27 | 0.44 |
| Age | 78.26 | 11.83 |
| Male | 0.34 | 0.47 |
| White | 0.83 | 0.38 |
| African American | 0.06 | 0.24 |
| Other race | 0.11 | 0.32 |
| Married | 0.28 | 0.45 |
| Less than high school | 0.33 | 0.47 |
| High school | 0.10 | 0.31 |
| Greater than high school | 0.57 | 0.50 |
| Medicare Part B | 0.21 | 0.41 |
| Activity of daily living score (0–28) | 15.10 | 7.13 |
| Fall | 0.24 | 0.43 |
| Fracture | 0.07 | 0.26 |
| Hip fracture | 0.08 | 0.28 |
| Stroke (CVA) | 0.18 | 0.38 |
| Hypertension | 0.59 | 0.49 |
| Cancer | 0.13 | 0.34 |
| Chronic obstructive pulmonary disease | 0.16 | 0.37 |
| Depressed | 0.22 | 0.42 |
| Resists care | 0.10 | 0.30 |
| Facility-Level Covariates | ||
| Hospital-based facility | 0.08 | 0.27 |
| Chain member facility | 0.13 | 0.34 |
| For-profit owned facility | 0.50 | 0.50 |
| Nonprofit owned facility | 0.45 | 0.50 |
| Government-owned facility | 0.06 | 0.23 |
| Number of beds | 262.99 | 158.71 |
Medicare Residents
Regression Specifications
In order to study the effect of the adoption of the PPS on the number of Medicare residents, we estimated the following facility-level model using national data for the period 1996 through March 2000:
| (4) |
where Vnt denotes the number (or share) of Medicare residents in nursing home n at time t, Z is a vector of nursing home factors, ν is a set of year-quarter dummies, λ is a nursing home level fixed effect and ε is a randomly distributed error term. We employ two alternate measures for our dependent variable. First, we use a count of the number of Medicare residents in a facility at a particular survey. Next, we model the dependent variable as the proportion of individuals with Medicare among all of the facility’s residents. Z includes ownership status (for-profit, nonprofit, government), chain membership (yes/no), hospital-based status (yes/no) and the total number of beds. PPS is a dummy variable identifying the adoption of PPS. The PPS was implemented across facilities based on the start of the facility fiscal year on or after July 1, 1998. Thus, a facility with a fiscal year beginning on January 1, 1999 would have a later implementation of the PPS relative to a facility with a fiscal year beginning on July 1, 1998. In spite of some clustering of fiscal year start dates (e.g., 1/1/99), meaningful variation existed among facilities in the timing of the introduction of prospective payment. The mean SNF PPS adoption date was November 25, 2008 and the standard deviation was 86 days. 20% of SNFs had the PPS implemented between July and September 1998, 13% between October and December 1998, 59% between January and March 1999, and 8% between April 1999 and June 1999. Importantly, this dummy variable captures both the change in the “prospectivity” of the system and the change in generosity of payment under PPS.
The identifying assumption here is that the timing of the fiscal year is exogenous to a facility’s decision to admit Medicare residents. A facility had little ability to change its fiscal year start date following the announcement that the PPS would be implemented on this date. Thus, we assert that this modeling strategy implicitly purges the unobserved and potentially confounded cross-sectional heterogeneity by relying on the within-facility variation in the facility’s fiscal year and by using facilities that did not experience a change as a control for unrelated time-series variation.
The subsequent payment changes under the BBRA and BIPA were implemented on a national basis. As such, we next consider a model that replaces the time dummies in equation 4 with a time trend (t):
| (5) |
where BBRA (April 2000), BIPA (April 2001) and BIPA2 (October 2002) represent national Medicare payment changes. Specifically, BBRA and BIPA changes increased payment generosity in high rehabilitation RUGs categories and the BIPA2 change repealed some of the payment increases. Thus, BBRA and BIPA are associated with increased payment generosity and BIPA2 is associated with a decrease in payment generosity. Importantly, all of these payment dummies are coded as “zero” for the pre-period and then “one” after the date of implementation. Thus, the coefficient estimates can be interpreted as the effects relative to the preceding period (PPS relative to pre-PPS, BBRA relative to PPS, etc.). This model was estimated using OSCAR data from 1996 through the end of 2004.
For the Medicare share measure, we use the logit transformation so the dependent variable is of the form where Pi represents the proportion of Medicare residents of nursing home i. Because the logit transformation assigns no value when the percent is equal to either zero or one, zero values were recoded as .0001 and values of one were recoded as .9999.6 In the facility-level regressions, observations are weighted according to the number of residents in nursing home i at time t. Because we have multiple observations from each facility, standard errors are clustered at the level of the facility.
Results
We first present national facility-level regressions examining the effect of the Medicare policy changes on the admission of Medicare SNF patients. The first two columns of Table 4 examine Medicare utilization (count of Medicare residents), while the latter two examine Medicare share (Medicare residents/total residents). For both outcomes, we estimate both a model with year fixed effects encompassing the pre- and post-PPS periods, and because the latter policy changes were implemented nationally, a model with a time trend including all periods. For these models, we constructed our policy dummy variables such that the interpretation is the effect relative to the immediately prior period.7
Table 4.
Medicare Payment Changes and the Number of Medicare Patients
| Medicare Utilization | Medicare Share | |||
|---|---|---|---|---|
| 1996–March 2000 | 1996–2004 | 1996–March 2000 | 1996–2004 | |
| PPS | −0.986** (0.298) | −1.94** (0.233) | −0.097** (0.029) [−0.087] | −0.219** (0.014) [−0.195] |
| BBRA | --- | 0.297 (0.202) | --- | −0.049** (0.013) [−0.044] |
| BIPA1 | --- | 1.13 (0.713) | --- | 0.082** (0.014) [0.073] |
| BIPA2 | --- | 0.542 (0.622) | --- | 0.127** (0.013) [0.113] |
| Year fixed effects | Y | Y | ||
| Time Trend | Y | Y | ||
| N | 58,880 | 128,480 | 58,880 | 128,480 |
Notes: Each model includes facility covariates from Table 3, season fixed effects and facility fixed effects. Standard errors are presented in parentheses; percentage effects (relative to baseline means) are presented in brackets.
Statistically significant at the 5-percent level
Statistically significant at the 1-percent level
From the fixed effects model, the average SNF served nearly one (0.986) fewer Medicare residents following the adoption of PPS. Similarly, the facility share of Medicare residents decreased 8.7% in the post-PPS period. From the time trend model, the Medicare utilization model suggests, once again, that PPS was associated with nearly two (1.94) fewer Medicare patients relative to the pre-PPS period. The subsequent rate enhancements under BBRA and BIPA, coupled with the repeal of the BBRA, were all associated with more Medicare patients, but none of these results are statistically significant. The results from the Medicare share model indicate a decrease of nearly 20% following the adoption of PPS, a decrease of 4% following the implementation of the BRRA, an increase of 7% following BIPA1 and an increase of 12.7% following BIPA2. Taken together, the results imply that the adoption of PPS led to a short-term decline in the number of Medicare residents served, but the subsequent policy rate enhancements roughly offset this decline.
Medicare Intensity and Length-of-Stay
Regression Specifications
In order to examine the effect of the Medicare payment changes on the intensity of service use and length-of-stay, we next estimate the following model encompassing the pre- and post-PPS periods:
| (6) |
where Y denotes the services received by individual i in facility n at time t, X is a vector of individual controls, Z is a vector of facility controls (same as above), ν is a set of year dummies, λ is a nursing home level fixed effect and ε is a randomly distributed error term. Unlike the models above, this individual-level model is estimated using data from New York State only. Importantly, New York was one of the PPS demonstration states. The first phase of the PPS demonstration began in 1995, and by Phase III in 1997, 428 (or 74.5%) of facilities in the state were paid using the PPS as part of the demonstration. The non-participating CMS demonstration facilities transitioned to the PPS on January 1, 1999. Thus, using data from January 1998 through March 2000, we initially estimate a DD model that compares the pre-post PPS difference in service use among Medicare admissions in facilities not participating in the demonstration against the difference in facilities participating in the demonstration. We obtained payer status on each admission MDS assessment based on whether the individual was covered by a Medicare per diem.
As initially specified, the PPS dummy in equation 6 encompasses the response to both the marginal and average payment changes under PPS. That is, the PPS dummy variable captures both the change in the “prospectivity” of the system and the change in generosity of payment under PPS. In an effort to decompose these two changes, we re-estimated equation 6 with the inclusion of a variable measuring the average facility payment by SNF. Thus, this rate variable captures changes in the generosity of payment, while the PPS dummy captures changes in the prospectivity of payment. The full details regarding the construction of the payment rate measure (as well as further sensitivity analysis results mentioned in the text) are available in an unpublished appendix available upon request.
As a brief overview, we used data from three sources to construct these payment rates. First, we used SNF cost reports to calculate the level of reimbursement for each facility pre-PPS, and to ascertain the extent to which payment rates by RUG were based in part on historical facility costs post-PPS. Second, we used regulations published in the Federal Register from various years to calculate the national RUG payment rates, another important component of SNF reimbursement post-PPS. Finally, we used MDS data to construct day counts by RUG in the pre-PPS period. We used these day counts to hold each facility’s case mix constant at its pre-PPS level, so that the facility-level payment rates we calculated were not influenced at all by any changes in case mix due to the SNF PPS rules.
We have several different measures of service use (Y) at the patient-level. In terms of service intensity, we apply a binary indicator as to whether the individual qualifies for a rehabilitation (45+ minutes of therapy) or high-rehabilitation (500+ minutes of therapy) visit. Second, conditional on receipt of therapy, we measure the number of minutes of therapy received over the past 7 days. For individuals surveyed before their seventh day in the facility, we use their average minutes per day to construct a 7-day total. For individuals discharged prior to day 7 with a survey from an earlier day, we adjust their therapy minutes based on the total number of days in the facility (e.g., for an individual surveyed at day 3 and then discharged on day 5, we multiply their reported therapy minutes by 5/3).
We created two binary length-of-stay measures based on discharge within 20 days and discharge within 90 days. We should note that results are robust to employing other cutoffs (5, 14 or 30 days) and also using a continuous measure of length-of-stay.
A number of patient-level covariates X were available from the MDS. In order to capture the need for services, an Activities of Daily Living (ADL) score was created from each resident admission assessment. The ADL score is based on the individual’s need for help with bathing, bed mobility, dressing, eating, toileting, transferring and walking. For each of these seven areas, the individual is scored as a zero (independent), one (supervised), two (limited assistance), three (extensive assistance) or four (total dependence). Thus, the total ADL score ranges between zero and twenty-eight. We also included indicators for a fall, hip fracture, other fracture, stroke, hypertension, cancer, chronic obstruction pulmonary disease, depression and whether the individual resists care. Finally, we also included a number of demographic variables including age at admission, gender, race (African American, white, other), education (less than high school, high school, greater than high school), and current marital status. We also control for whether the individual had coverage under Medicare Part B.8
The identifying assumption in the DD model above is that Medicare admissions in non-participating facilities serve as a valid comparison group for Medicare admissions in participating facilities. Because the demonstration was voluntary, the type of facility selecting into the demonstration may be different from other facilities. Thus, we next present results based on a regression model that explicitly relies on admissions among non-Medicare residents to provide possibly better controls for unobserved facility and time-specific nursing home admission shocks.
More specifically, this second specification takes the following basic form:
| (7) |
The term, mi, represents fixed effects for each payer group. This unrestrictive model includes a full set of interactions between the payer, quarter and facility fixed-effects. Identification in this DDD framework relies effectively on comparing the change in the gap in service use between Medicare and non-Medicare admissions in facilities that did and did not adopt the PPS.9 The interactions between the Medicare policy variable, PPSnt, and the Medicare fixed effects, mi, are set to zero for the non-Medicare residents for whom these payment policies were presumably irrelevant. Non-Medicare residents encompass all Medicaid and other (private-pay, Veteran’s Administration, etc.) admissions. Thus, contemporaneous admissions among the non-Medicare cohort serve as controls for facility-quarter unobserved factors. It should be noted that this DDD approach assumes that Medicare and non-Medicare admissions share the same “shocks” in a given facility and quarter. For example, it could be the case that Medicare payment changes “spill over” to the non-Medicare population, suggesting that the non-Medicare population is not a valid comparison group. The DD approach, which instead used as controls the within-facility admission shocks among Medicare admissions in other SNFs, may actually be preferable. Because we have little basis for distinguishing these approaches ex ante, these models are probably best viewed as complementary approaches for exploring the validity of this study’s key results. Similar to the DD approach above, we initially estimate the overall PPS effect (model includes only the PPS*Medicare interaction term) before decomposing the marginal and average effects under the PPS (model includes both the PPS*Medicare and payment*Medicare interaction terms).
Given that the demonstration period only applied to the PPS period, we can evaluate the latter Medicare payment changes by comparing the effects on service use across Medicare and non-Medicare residents. Thus, we estimate the following model:
| (8) |
where the key coefficients of interest are the interaction terms between Medicare (m) and the national policy changes under the PPS, BBRA, BIPA and BIPA2. Identification in this DD framework relies on comparing the pre-post change in the use of services between Medicare and non-Medicare admissions. Non-Medicare patients, who are presumably unaffected by the Medicare policy changes, serve as a control for unrelated time-series variation. Given that the analysis is extended to the latter policy changes, we also include an additional outcome measuring the RUGs payment categories associated with a 20% increase under the BBRA. Similar to the DD and DDD models above, we initially estimate the overall effect of the national policy changes (model includes only the policy*Medicare interaction terms in equation 8) before decomposing the marginal and average effects under the policy changes (model includes both policy*Medicare and payment*Medicare interaction terms).
For the binary individual-level outcomes (e.g., receipt of high rehabilitation services), least squares models estimations of linear probability regression models are presented. Although this approach does not recognize the binary nature of the quality measures, it facilitates the tractable estimation of these models, which are based on a large number of observations and an expansive set of regression controls. Using a sub-sample of the data however, the linear probability estimates were robust to those obtained using a conditional logit model. For the minutes of therapy time outcome, we estimate models using least squares using the natural logarithm of the measure. Importantly, the results from this model were robust to those obtained using a negative binomial count model. Once again, standard errors are clustered at the level of the facility.
Results
The main evaluation results from the DD models for Medicare intensity and length-of-stay are reported in Table 5. These person-level models condition on Medicare status among New York State nursing home residents, and examine the pre-post difference in outcomes for residents in facilities adopting PPS on January 1, 1999 compared to the difference for residents in CMS demonstration facilities with PPS over the same period. The results in the upper panel are based on a model with an overall PPS dummy, while the results in the lower panel decompose the prospectivity and level of payment. As expected, the results in the upper panel suggest that the adoption of PPS was associated with a 3.7 percentage point (or 4.9% of the dependent variable mean) increase in admissions within the 14 rehabilitation RUGs payment categories and an 8.8 percentage point (or 61.5%) increase in the six “high” rehabilitation RUGs. Therapy minutes increased 14.1% following the adoption of PPS. Given that nursing homes were paid a per-diem rate, the lack of a statistically meaningful effect of the PPS on discharge within 20 or 90 days is unsurprising.
Table 5.
Effects of the Medicare Prospective Payment System (PPS) Demonstration on the Intensity of Medicare Services and Length-of-Stay: New York State, January 1998–March 2000.
| Rehabilitation | High Rehabilitation |
Ln(Minutes) | Discharge within 20 days |
Discharge within 90 days |
|
|---|---|---|---|---|---|
| Medicare Admissions | |||||
| PPS | 0.037* (0.016) | 0.080** (0.028) | 0.141** (0.046) | 0.024 (0.017) | 0.029 (0.016) |
| N | 76,094 | 76,094 | 67,262 | 76,265 | 76,265 |
| PPS | 0.036* (0.016) | 0.063* (0.024) | 0.121** (0.045) | 0.023 (0.018) | 0.028 (0.017) |
| Per diem (10s of $2010) | 0.0006 (0.0017) | 0.010** (0.004) | 0.012** (0.004) | 0.0007 (0.0012) | 0.0006 (0.0017) |
| N | 76,094 | 76,094 | 67,262 | 76,265 | 76,265 |
Notes: Each model includes person and facility covariates from Table 3, quarter fixed effects and facility fixed effects. Standard errors are presented in parentheses.
Statistically significant at the 5-percent level
Statistically significant at the 1-percent level
When we decompose the level and prospectivity of payment under the PPS (bottom panel of Table 5), the size of the estimates on the PPS dummy (modeling prospectivity) are roughly four-fifths as large as the upper panel for the high rehabilitation and therapy minutes outcomes. These results suggest that both the level and prospectivity of payment explain the change of intensity observed under the PPS. In 2010 dollars, a $10 increase in Medicare SNF payment under the PPS led to a 1.0 percentage point (or 7.7%) increase in the six “high” rehabilitation RUGs and a 1.2% increase in therapy minutes.
The next model we examined was the DDD specification. Once again, the identification strategy relies on comparing the change in the gap in service use between Medicare and non-Medicare admissions in facilities that did and did not adopt the PPS. Similar to the DD specification, the results suggest the adoption of the PPS significantly increased assignment of Medicare patients to the rehabilitation categories (see Table 6). Specifically, when we model the overall effect of the PPS, the policy change led to a 4.8 percentage point (or 6.4%) increase in the rehabilitation RUGs and a 3.9 percentage point (or 30%) increase in the high rehabilitation RUGs. Similarly, therapy minutes increased 8.7% following PPS. Finally, we found no statistically meaningful effects of PPS on discharge within 20 or 90 days.
Table 6.
Effects of Medicare Prospective Payment System (PPS) on the Intensity of Medicare Services and Length-of-Stay, Differences-in-Differences-in-Differences Specifications
| Rehabilitation | High Rehabilitation |
Ln(Minutes) | Discharge within 20 days |
Discharge within 90 days |
|
|---|---|---|---|---|---|
| PPS*Medicare | 0.048* (0.021) | 0.039** (0.013) | 0.087** (0.030) | −0.001 (0.013) | 0.016 (0.018) |
| N | 129,989 | 129,989 | 103,357 | 130,292 | 130,292 |
| PPS*Medicare | 0.045 (0.022) | 0.026* (0.012) | 0.069* (0.029) | −0.005 (0.013) | 0.010 (0.019) |
| Per diem*Medicare | 0.0015 (0.0023) | 0.006** (0.001) | 0.008** (0.003) | 0.0017 (0.0014) | 0.0029 (0.0021) |
| N | 129,989 | 129,989 | 103,357 | 130,292 | 130,292 |
Notes: The average Medicare per diem is expressed in denominations of ten using 2010 dollars. Each model includes person and facility covariates from Table 3, quarter-by-Medicare fixed effects, facility-by-quarter fixed effects and facility-by-Medicare fixed effects. Standard errors are presented in parentheses.
Statistically significant at the 5-percent level
Statistically significant at the 1-percent level
When we decomposed the PPS into changes in the level and prospectivity of payment under the DDD framework (see bottom panel of Table 6), we found that the level of payment was important towards explaining the changes in rehabilitation care and therapy minutes. The DDD model suggests a $10 increase in Medicare SNF payment under the PPS led to a 0.6 percentage point (or 4.6%) increase in the six “high” rehabilitation RUGs and a 0.7% increase in therapy minutes.
The final model examines all the various payment changes over the study period via an interaction term between payer type and the various policy changes. In this specification, we find strong support for increased assignment to rehabilitation payment RUGs for Medicare relative to non-Medicare residents (see Table 7). Specifically, the adoption of PPS increased the assignment of Medicare admissions to the rehabilitation RUGs by 3.5 percentage points and to the high rehabilitation RUGs by 6.1 percentage points relative to non-Medicare admissions. Similarly, the provision of weekly therapy minutes increased 9.6% for Medicare residents under PPS. In terms of other significant results, Medicare admissions to the high rehabilitation RUGs decreased by 3.2 percentage points under the BBRA, but increased by 1.7 percentage points in the BIPA2 period. Similarly, Medicare admissions to the rehabilitation RUGs declined 2.2 percentage points under BIPA2. We generally did not find statistically meaningful differences in terms of discharge within 20 or 90 days across Medicare and non-Medicare residents. The exceptions were a 1.5 percentage point decline in discharge for Medicare admissions within 90 days under BBRA and a 1.5 percentage point increase in 20-day discharges under BIPA. In sum, the takeaway point from these models is that PPS led to an increase in the intensity of services, but little change in length-of-stay. Some small changes were observed in subsequent periods, but they did not offset the large changes following the adoption of PPS.
Table 7.
The Effects of Medicare Payment Changes on the Intensity of Medicare Services and the Length-of-Stay
| Rehabilitation RUGs |
High Rehabilitation RUGs |
BBRA “20%” Payment RUGs |
Ln(Minutes) | Discharge within 20 days |
Discharge within 90 days |
|
|---|---|---|---|---|---|---|
| PPS*Medicare | 0.035* (0.017) | 0.061** (0.022) | −0.031** (0.012) | 0.096** (0.036) | 0.014 (0.012) | 0.011 (0.015) |
| BBRA*Medicare | 0.004 (0.009) | −0.032** (0.010) | −0.008 (0.007) | −0.005 (0.015) | −0.0016 (0.0049) | −0.015* (0.006) |
| BIPA1*Medicare | −0.004 (0.008) | 0.009 (0.006) | −0.001 (0.006) | 0.018 (0.012) | 0.015** (0.006) | 0.006 (0.005) |
| BIPA2*Medicare | 0.022** (0.007) | 0.017** (0.007) | 0.016** (0.005) | −0.003 (0.014) | 0.003 (0.005) | −0.004 (0.005) |
| N | 495,745 | 495,745 | 496,049 | 406,309 | 496,049 | 496,049 |
| Per diem*Medicare | −0.0078** (0.0010) | 0.0023** (0.0008) | 0.0045** (0.0007) | −0.0022 (0.0016) | −0.0016** (0.0004) | −0.0038** (0.0005) |
| PPS*Medicare | 0.056** (0.016) | 0.055* (0.022) | −0.042** (0.011) | 0.101** (0.036) | 0.018 (0.012) | 0.021 (0.015) |
| BBRA*Medicare | 0.005 (0.008) | −0.032** (0.009) | −0.009 (0.006) | −0.0052 (0.0153) | −0.0014 (0.0050) | −0.014* (0.006) |
| BIPA1*Medicare | 0.011 (0.008) | 0.0051 (0.0058) | −0.009 (0.006) | 0.022 (0.011) | 0.018** (0.006) | 0.013* (0.005) |
| BIPA2*Medicare | −0.044** (0.007) | 0.024** (0.007) | 0.029** (0.005) | −0.0095 (0.0137) | −0.002 (0.006) | −0.015** (0.005) |
| N | 495,745 | 495,745 | 496,049 | 406,309 | 496,049 | 496,049 |
Notes: The average Medicare per diem is expressed in denominations of ten using 2010 dollars. Each model includes person and facility covariates from Table 3, Medicare fixed effects, quarter fixed effects, and facility fixed effects. Standard errors are presented in parentheses.
Statistically significant at the 5-percent level
Statistically significant at the 1-percent level
When we decomposed the level and prospectivity of the payment changes (see bottom panel of Table 7), the results suggested that the generosity of payment had a statistically meaningful effect on nearly all the outcomes. A $10 increase in Medicare SNF payment was associated with a 0.8 percentage point decline in the assignment of Medicare admissions to the rehabilitation RUGs, but a 0.2 percentage point increase in the high rehabilitation RUGs and a 0.5 percentage increase in the BBRA “20% ” payment RUGs. A $10 increase in payment also decreased discharges at 20 days by 0.2 percentage points and discharges at 90 days by 0.4 percentage points. The estimates of the payment*Medicare interaction terms were qualitatively similar to those described above in the overall model.
Discussion
The SNF PPS was adopted with the objective of limiting Medicare spending growth, especially among those high rehabilitation patients. Using multiple identification strategies, our analyses suggest that the SNF PPS led to a short-term decrease in the number of Medicare SNF patients, but an increase in the intensity of Medicare patients admitted to SNFs. We found little effect of the SNF PPS on length-of-stay. When we decomposed the level and prospectivity of the payment changes under the PPS, we generally found that both were important towards explaining the change in intensity under the PPS. These results highlight the importance of the level of Medicare payment and the effective degree of marginal cost sharing in a bundled or prospective system for the volume and intensity of SNF services. When subsequent Medicare policy changes (BBRA and BIPA) increased the generosity of SNF payment, the number of SNF patients returned to pre-PPS levels. When taken together, our volume and intensity results suggest that SNF PPS did little to curb the rate of growth of SNF expenditures.
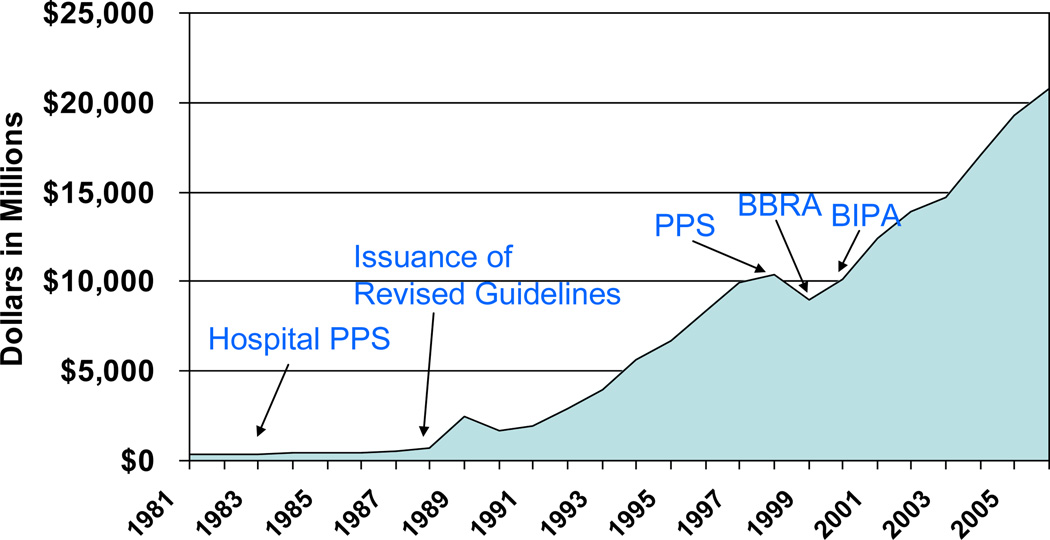
This conclusion is confirmed when we examine the trend in overall Medicare SNF expenditures over the period 1981 through 2006 (see Figure 1). As noted in the introduction, Medicare SNF expenditures were relatively stable until 1989, when CMS issued revised guidelines for SNFs. These changes, coupled with the earlier shift to a PPS system for hospitals, led to a large increase in Medicare expenditures during the early and mid 1990s. As shown in the figure, the adoption of the PPS was associated with a short-term decrease in expenditures, but beginning around the time of the BBRA, expenditures begin to increase again at roughly the same pace as pre-PPS expenditures. Indeed, after accounting for inflation, the unadjusted Medicare payment per SNF day had returned to the pre-PPS level by 2001 (Center for Medicare & Medicaid Services, 2010). Obviously, the one-time decrease in expenditures under the PPS shifted costs on to a lower trajectory, saving billions of dollars over the last decade. However, other than the one-time cost decline, the PPS did little to bend the cost curve downwards.
Figure 1.
Medicare SNF Expenditures, 1981–2006
Although the PPS is termed a “prospective” system, this term is misleading in several respects. First, the PPS is not episode-based, and SNFs receive a payment for each day of care set to cover costs on average. Thus, although our conceptual framework suggested we would observe longer length-of-stay, we observed—similar to previous research (White 2003)—little change in length-of-stay following the PPS. Second, facilities are paid higher per diem rates for providing additional rehabilitative therapy care. Not surprisingly, similar to earlier research (Wodchis 2004), we observed an increase in the provision of therapy minutes following the PPS. We also found—similar to earlier studies (Abt Associates 2002; Wodchis 2003)—increased assignment to the high rehabilitation categories with the largest per diem payment rates.
Economic research has suggested that the preferred reimbursement system is a “mixed” system that balances the cost-saving incentives under a prospective system with the quality incentives under a cost-based system (Ellis & McGuire, 1986, 1990; Newhouse, 1986). Thus, any attempt to rebalance SNF payment towards a more prospective system would have implications for quality of care. Indeed, research has shown that the initial shift to the SNF PPS did lower SNF quality of care (Konetzka, Yi, Norton, & Kilpatrick, 2004). Nevertheless, if CMS sought a real prospective payment system, several potential approaches are available. In the evaluation of the PPS SNF demonstration, Abt Associates (2002) suggested that the “variability of length of stay – and thereby episode cost – is too great to practically implement an episode-based prospective pricing mechanism” (page 2). However, there might be some ability to construct episodes of SNF care for particular conditions such as chronic obstructive pulmonary disease (COPD), hip fracture or stroke. Indeed, the Medicare Payment Advisory Commission (2008) has recently considered taking the episode concept to an even higher level by bundling payment for SNF and other post-acute services around a base hospitalization for particular conditions (e.g., COPD). Episode-based payment, whether at the SNF level or bundled with other services, could dramatically alter the incentives around both the use and intensity of Medicare SNF services.
In sum, the SNF PPS did little to achieve its goal of slowing the rate of SNF cost growth. However, the initial decrease in the level of payment was associated with a one-time decrease in the number of Medicare patients. Length of stay remained relatively unchanged under PPS and intensity of services increased. Not surprisingly, when subsequent Medicare policy changes increased payment generosity, the number of Medicare patients returned to—and eventually surpassed—the pre-PPS levels. Today, the rate of growth in SNF expenditures is similar to the pre-PPS period.
Acknowledgments
We gratefully acknowledge funding from the National Institute on Aging (R01 AG030079).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Any fixed fee can be thought of as a bundled payment. Even a fee for an office visit “bundles” payment for the inputs used in that visit, such as time of the doctor, office staff, supplies, etc.
The SNF PPS was phased in over 4 years with the start date corresponding to each facility’s own fiscal year start date on or after July 1, 1998. In the first year, facilities were paid based on 25 percent of the new federal rate and 75 percent of the old facility-specific rate based on 1995 costs (adjusted for inflation). The federal portion of the rate increased by 25 percentage points each year until the new federal rate was completely phased in after 4 years. Subsequent refinements to the SNF PPS gave facilities the option to switch to 100 percent of the federal rate more quickly.
In the supply response literature, the provider chooses intensity, interpreted in a hospital context as length of stay (Ellis & McGuire, 1996; Meltzer, Chung, & Basu, 2002), and in the physician literature as minutes per visit (Glied & Zivin, 2002). For a recent review of supply response literature, see Newhouse (2002).
The term (p(e) − c(e)) drops out of (2) if (2) holds with equality. L drops out of (3).
Conditions (2) and (3) are not set up to conduct comparative static analysis on payment system variables as is done in some hospital payment papers, such as Hodgkin and McGuire (1994). Level of payment here is how generous p is in relation to cost, and prospectiveness is negatively related to the degree p is tied to e. We explored parameterizing these features but the additional complexity was not rewarded with additional insights. Key predictions remain indeterminant without strong assumptions on the demand and cost functions.
Results were robust to using .001 and .999 or .00001 and .99999 in recoding the zero and one values.
We present the key policy parameters in the table. Full regression results are available upon request from the authors.
For Medicare beneficiaries not covered under the Part A SNF benefit, a limited amount of rehabilitation services are available under the Part B benefit. Specifically, Part B payments for rehabilitation services are determined by a schedule with an annual benefit limit.
This identification strategy has been used in other policy contexts including evaluations of the labor market effects of mandated maternity benefits (Gruber, 1994).
REFERENCES
- Abt Associates. Evaluation of the Nursing Home Casemix and Quality Demonstration. Baltimote, MD: Final Report to Centers for Medicare and Medicaid Services, HCFA; 2002. Contract No. 500-94-0061. [Google Scholar]
- Center for Medicare & Medicaid Services. Medicare & Medicaid Statistical Supplement. 2010 Retrieved. from https://www.cms.gov/MedicareMedicaidStatSupp/LT/itemdetail.asp?filterType=dual,keyword&filterValue=2010&filterByDID=0&sortByDID=1&sortOrder=ascending&itemID=CMS1241877&intNumPerPage=10.
- Dalton K, Howard HA. Market entry and exit in long-term care: 1985–2000. Health Care Financing Review. 2002;24(2):17–32. [PMC free article] [PubMed] [Google Scholar]
- Ellis RP, McGuire TG. Provider behavior under prospective reimbursement. Cost sharing and supply. Journal of Health Economics. 1986;5(2):129–151. doi: 10.1016/0167-6296(86)90002-0. [DOI] [PubMed] [Google Scholar]
- Ellis RP, McGuire TG. Optimal payment systems for health services. Journal of Health Economics. 1990;9(4):375–396. doi: 10.1016/0167-6296(90)90001-j. [DOI] [PubMed] [Google Scholar]
- Ellis RP, McGuire TG. Hospital response to prospective payment: moral hazard, selection, and practice-style effects. Journal of Health Economics. 1996;15(3):257–277. doi: 10.1016/0167-6296(96)00002-1. [DOI] [PubMed] [Google Scholar]
- Glied S, Zivin JG. How do doctors behave when some (but not all) of their patients are in managed care? Journal of Health Economics. 2002;21(2):337–353. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Gruber J. The incidence of mandated maternity benefits. American Economic Review. 1994;84(3):622–641. [PubMed] [Google Scholar]
- Harrington C, Swan JH, Wellin V, Clemena W, Carrillo HM. San Francisco: Department of Social & Behavioral Sciences, University of California; 1999. 1998 State Data Book on Long Term Care Program and Market Characteristics. [Google Scholar]
- Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, Nonemaker S. Reliability estimates for the Minimum Data Set for nursing home resident assessment and care screening (MDS) Gerontologist. 1995;35(2):172–178. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- Hodgkin D, McGuire TG. Payment levels and hospital response to prospective payment. Journal of Health Economics. 1994;13(1):1–29. doi: 10.1016/0167-6296(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Norton EC, Stearns SC. Medicare payment changes and nursing home quality: effects on long-stay residents. Int J Health Care Finance Econ. 2006;6(3):173–189. doi: 10.1007/s10754-006-9000-9. [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Yi D, Norton EC, Kilpatrick KE. Effects of Medicare payment changes on nursing home staffing and deficiencies. Health Services Research. 2004;39(3):463–488. doi: 10.1111/j.1475-6773.2004.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosecoff J, Kahn KL, Rogers WH, Reinisch EJ, Sherwood MJ, Rubenstein LV, et al. Prospective payment system and impairment at discharge. The 'quicker-and-sicker' story revisited. Journal of the American Medical Association. 1990;264(15):1980–1983. [PubMed] [Google Scholar]
- Lagnado L. Nursing Home Empire Collapsed When CEO Mined Medicare Cash. Wall Street Journal. 2002 May 24; 2002. [Google Scholar]
- Lewin Group. Briefing Chartbook on the Effect of Balanced Budget Act of 1997 and the Balanced Budget Act of 1999 on Medicare Payment to Skilled Nursing Facilities. [Retrieved April 5, 2006];2000 from http://www.ascp.com/public/ga/2000/pdfs/SNFBBACH.PDF. [Google Scholar]
- Ma CA. Health Care Payment Systems: Costs and Quality Incentives. Journal of Economics and Management Strategy. 1994;3(1):93–112. [Google Scholar]
- McClellan M. Hospital Reimbursement Incentives: An Empirical Analysis. Journal of Economics and Management Strategy. 1997;6(1):91–128. [Google Scholar]
- Medicare Payment Advisory Commission. Report to Congress. Washington, DC: Medicare Payment Advisory Commission; 2002. [Google Scholar]
- Medicare Payment Advisory Commission. A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Commission; 2003. [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2008. [Google Scholar]
- Meltzer D, Chung J, Basu A. Does competition under Medicare Prospective Payment selectively reduce expenditures on high-cost patients? Rand Journal of Economics. 2002;33(3):447–468. [PubMed] [Google Scholar]
- Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Affairs (Millwood) 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2005. Hyattsville, MD: 2005. [PubMed] [Google Scholar]
- Newhouse JP. Rate adjusters for Medicare under capitation. Health Care Financing Review. 1986;7 Annual Supplement:45–55. [PMC free article] [PubMed] [Google Scholar]
- Newhouse JP. Pricing the priceless: A health care conundrum. Cambridge and London: MIT Pres; 2002. [Google Scholar]
- U.S. General Accounting Office. Medicare Post-Acute Care: Home Health and Skilled Nursing Facility Cost Growth and Proposals for Prospective Payment. Washington, DC: 1997. GAO/T-HEHS-97-90. [Google Scholar]
- U.S. General Accounting Office. Skilled Nursing Facilities: Providers Have Responded to Medicare Payment System by Changing Practices. Washington, DC: 2002. GAO-02-841. [Google Scholar]
- White C. Rehabilitation therapy in skilled nursing facilities: effects of Medicare's new prospective payment system. Health Affairs (Millwood) 2003;22(3):214–223. doi: 10.1377/hlthaff.22.3.214. [DOI] [PubMed] [Google Scholar]
- Wodchis WP. Physical rehabilitation following medicare prospective payment for skilled nursing facilities. Health Services Research. 2004;39(5):1299–1318. doi: 10.1111/j.1475-6773.2004.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]