Abstract
From ancient times, chemopreventive agents have been used to treat/prevent several diseases, including cancer. They are found to elicit a spectrum of potent responses including anti-inflammatory, anti-oxidant, anti-proliferative, anti-carcinogenic, and anti-angiogenic activity in various cell culture and some animal studies. Research over the past four decades has shown that chemopreventives affect a number of proteins involved in various molecular pathways that regulate inflammatory and carcinogenic responses in a cell. Various enzymes, transcription factors, receptors, and adhesion proteins are also affected by chemopreventives. Although, these natural compounds have shown significant efficacy in cell-culture studies, they elicited limited efficacy in various clinical studies. Their introduction into the clinical setting is hindered largely by their poor solubility, rapid metabolism, or a combination of both, ultimately resulting in poor bioavailability upon oral administration. Therefore, to circumvent these limitations and to ease their transition to clinics, alternate strategies should be explored. Drug delivery systems such as nanoparticles, liposomes, microemulsions, and polymeric implantable devices are emerging as one of the viable alternatives that have been demonstrated to deliver therapeutic concentrations of various potent chemopreventives such as curcumin, ellagic acid, green tea polyphenols, and resveratrol into the systemic circulation. In this review article, we have attempted to provide a comprehensive outlook for these delivery approaches, using curcumin as a model agent, and discussed future strategies to enable the introduction of these highly potent chemopreventives into a physician’s armamentarium.
Keywords: Chemoprevention, Curcumin, Drug Delivery, Bioavailability, Antioxidant
1. Introduction
Currently, clinical and basic research is driven by the aim of curing advanced diseases. This aim is particularly difficult for cancer because of the genetic heterogeneity of the cell types involved. A cancerous lesion usually consists of a family of genetically/phenotypically different cell types that originate over a period of years and when this lesion becomes invasive, cell heterogeneity ultimately complicates the treatment of the disease (1). Therefore, attempts have been made to blunt, if not reverse, this carcinogenic cascade by intervention with agents; an approach coined over 30 years ago by Dr. Michael Sporn as chemoprevention (2). Since a typical carcinogenesis process involves many environmental, dietary, occupational, and epigenetic factors that determine its long latent period, intervention with phytochemicals that have little or no toxicity can provide an alternative strategy for controlling the initiation and progression of this disease. As a result, studies initiated by the National Cancer Institute have led to the screening and identification of thousands of such compounds, of which a few dozen have shown significant preventive/therapeutic potential (1). Although, most of these natural compounds such as curcumin, resveratrol, epigallocatechin gallate (EGCG), and indole-3-carbinol, exhibited potent chemopreventive/anti-tumor activity in cell-culture as well as in some animal studies, they elicited only low activity in various clinical studies (reviewed in ref. 3).
The limited efficacy of several chemopreventives in pre-clinical and clinical studies is attributed largely to their low bioavailability, which results in sub-therapeutic concentrations at the target site. In order to overcome the bioavailability issues, advanced drug delivery systems, designed to provide localized or targeted delivery of these agents, may represent a more viable therapeutic option. Various drug delivery systems such as nanoparticles (4, 5), liposomes (6, 7), microparticles (8, 9), and implants (10) have been demonstrated to significantly enhance the preventive/therapeutic efficacy of many chemopreventives by increasing their bioavailability and targetability. Therefore, we selected curcumin as a model compound to acquaint the readers with various advanced drug delivery strategies that can be successfully used for natural compounds and to help explore other untouched avenues in chemoprevention and therapeutic prevention (inhibition of progression of a disease to advanced malignancies (11)). Although, several drug-delivery systems have been developed to harness various activities of curcumin and other natural compounds, we have restricted our discussion mainly to nanoparticles (NPs), microparticles, liposomes, microemulsions and polymeric implants because of the relatively detailed understanding of these delivery systems and for their potential to enter into various preclinical and clinical studies.
2.0. Curcumin: A potent chemopreventive
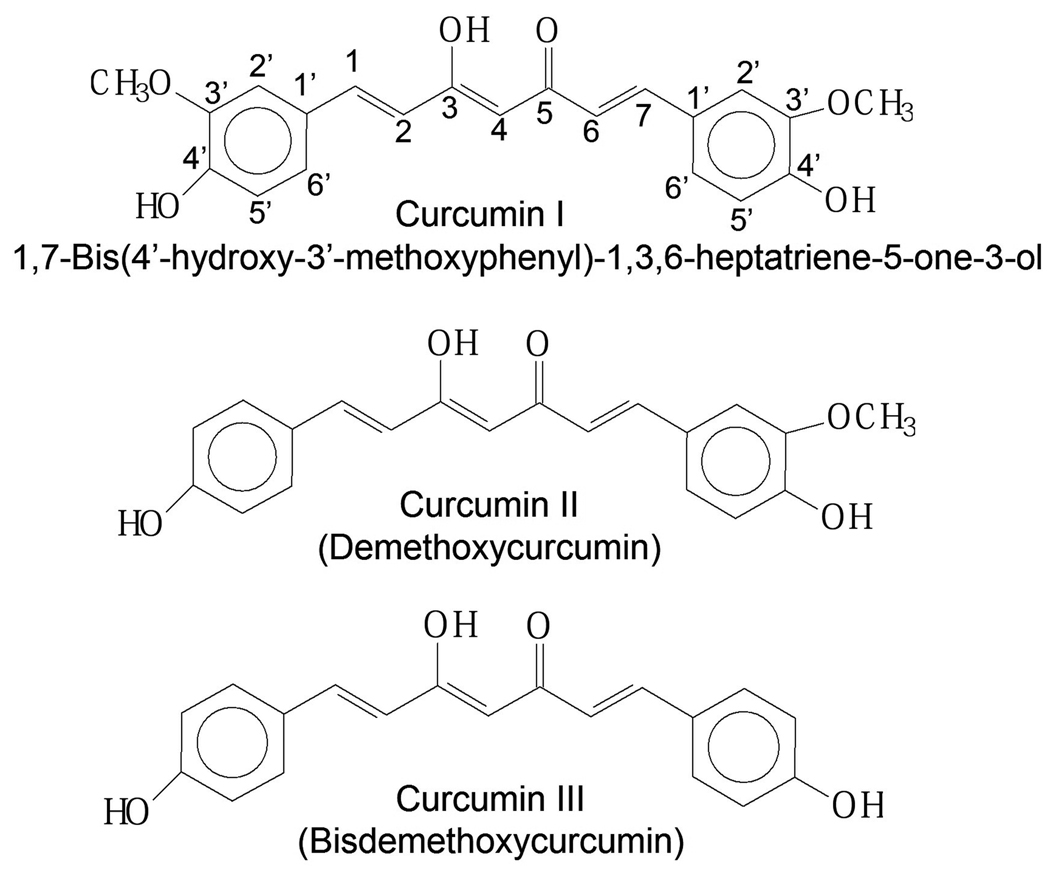
Although, a number of potent chemopreventives have been identified from plant sources, curcumin (a principal bioactive component of Curcuma longa (turmeric)), represents one of the most investigated phytochemicals with over 3,770 hits on using curcumin as the search string on Pubmed with ~1,200 hits in the last 2 years alone. There are 3 major curcuminoids that constitute curcumin: curcumin (curcumin I, 75%), demethoxycurcumin (curcumin II, 20%) and bisdemethoxycurcumin (curcumin III, 5%) (12 and our own analysis) (Fig. 1.). Research over the last two decades has shown curcumin to be a potent antioxidant, anti-inflammatory, anti-proliferative, anti-metastatic, anti-angiogenic, anti-diabetic, hepatoprotective, anti-atherosclerotic, anti-thrombotic, and anti-arthritic agent in cell culture and animal studies (13). Various cell culture studies have shown that it induces apoptosis in oncogenic cells by inhibiting various intracellular transcription factors and secondary messengers such as NF-kB, AP-1, c-Jun, the Jak-STAT pathway and various others (13–15). It exhibits potent anti-inflammatory activity, due to the inhibition of IκB kinase required for the activation of NF-kB, an important transcriptional regulator of inflammatory pathways involved in carcinogenesis and various other pathological conditions (16–18). Curcumin is well known for its potential to inhibit carcinogenesis induced by chemical carcinogens, at both initiation and progression stages under various preclinical studies (19). It is known to inhibit cytochrome P450 (CYP) enzyme mediated bioactivation of environmental carcinogens like benzo[a]pyrene (B[a]P) (20). As a metabolic substrate and an inducer of CYP1A1, curcumin is postulated to act as a competitive inhibitor of B[a]P metabolism, blunting its bioactivation via CYP1A1 (20). Curcumin also increases the levels of other endogenous antioxidants via the Nrf2 pathway to strengthen body’s defenses against reactive oxygen species (ROS) (21).
Figure 1.
Structures of the three curcuminoids as components of curcumin.
Despite these advantages, curcumin possess poor water solubility; as a consequence, it exhibits solubility limited bioavailability, which makes it a class II drug in the Biopharmaceutics Classification System (22). Furthermore, due to its rapid intestinal and hepatic metabolism, approximately 60–70% of an oral dose of curcumin gets eliminated in the feces (23). In rats, curcumin administered as an aqueous suspension (2g/kg) provided a maximum plasma concentration of 1 µg/ml within 1 h, and dropped rapidly to undetectable levels within 5 h (24). Studies by Pan et al., showed that after intra-peritoneal administration of 0.1g/kg curcumin to mice, only about 2.25 µg/ml reaches the plasma within 15 min which rapidly drops down to 0.35 µg/ml after 1 h (23). When curcumin was administered by parenteral routes like i.v., ~50% was found to be eliminated in bile within 5 h (25). Even in clinical studies, high doses of orally administered curcumin (8–12 g daily) resulted in very low curcumin concentrations in the plasma (<1 µg/ml), levels that were not high enough to exert any significant pharmacological or therapeutic activity (26). In various clinical studies, only a few patients responded to curcumin despite high doses used (Table I). A very recent clinical study by Carroll et al. (27) reported significant efficacy of curcumin in reducing colorectal aberrant crypt foci (ACF) at 4 g/day dose where 2 g dose was ineffective. No curcumin was detected in the plasma or biopsy samples from patients when analyzed by UFLC-UV (ultra flow liquid chromatography), although significant levels of curcumin conjugates were found. The authors implicated the efficacy may be due to the sulfate and glucuronide conjugates of curcumin, the notion which will require support from pre-clinical studies. If the samples were collected several hours after curcumin intake, it is likely that (free) curcumin was available to the target site at least for initial hours to elicit the efficacy. It is, therefore, quite probable that by the time biopsy tissue and plasma were collected, most of the curcumin might have metabolized giving only the glucuronide and sulfate conjugates in the plasma. It has been found that curcumin undergoes rapid metabolism in the intestine (28) and liver to form various active and inactive metabolic products that are further converted into excretable glucuronide and sulfate conjugates. Curcumin provides easily accessible –OH and -OCH3 sites (Fig. 1) to form conjugates with glucuronides and sulfates by glucuronidases and sulfatases, respectively (29). It has been suggested that this biotransformation of curcumin either occurs in intestine during absorption (30) or in liver (31) coupled with enterohepatic recirculation (32). Studies by Shoba et al (24), showed that co-administration of piperine (20 mg/kg), a potent inhibitor of glucuronidation in the liver and gastro-intestinal tract, significantly increases the curcumin bioavailability by 20 fold in humans. These limitations of low solubility, rapid metabolism and hence low bioavailability has limited the therapeutic success of curcumin in cell culture systems and elicited only limited success in various animal and clinical studies. In last two decades, several novel drug delivery systems such as micelles (33), liposomal vesicles (34), nanoparticles (35–37), nanoemulsions (38), and phospholipid complexes (39) have been designed to enhance the bioavailability of curcumin and to enable use of this compound for therapeutic prevention or risk reduction at the pre-cancer stage, which are discussed below.
Table I.
Examples of some pre-clinical (A) and clinical (B) studies reported with curcumin.
| A: Preclinical Studies | ||||
|---|---|---|---|---|
| Animal | Route | Dose | Findings | Refs. |
| Rats | oral | 1g/kg |
|
(40) |
| Rats | oral | 2% diet |
|
(41) |
| Mice | i/p | 100 mg/kg |
|
(23) |
| Rats | i/v | 40 mg/kg |
|
(42) |
| B: Clinical Studies | |||
|---|---|---|---|
| Route | Dose | Findings | Refs. |
| Oral (n=34*) | 1–4 g/day for 6 months |
|
(43) |
| Oral (n=21*) | 8 g/day until disease progression |
|
(44) |
| Oral (n=25*) | 8000 mg/day for 3 months |
|
(45) |
| Oral (n=12*) | 450–3600 mg/day for 1 wk prior to surgery |
|
(46) |
denotes number of patients in the trial
2.1.1 Nanoparticles
Recently, the development of new drug delivery systems for lipophilic compounds has made tremendous improvements toward enhancing their bioavailability. The advent of nanotechnology has been exploited for the development of various nano-particulate drug delivery systems that can enable formulation and delivery of curcumin (Table II) and other hydrophobic drugs which earlier was a conundrum for the formulation scientists (47). These delivery systems have gained immense popularity in the last decade due to their potential to improve the therapeutic index of the encapsulated drugs either by protecting them from enzymatic degradation (48), by altering their pharmacokinetics (49), by blunting their toxicity (50) or by providing controlled release over extended periods of time (51). According to the National Nanotechnology Initiative (NNI), nanoparticulate (NP)-delivery systems contain encapsulated, dispersed, adsorbed, or conjugated drugs within a particle size range of 1–100 nm (52).
Table II.
Polymeric and solid lipid nanoparticle formulations of curcumin.
| Formulation | Method | Particle Size (nm) |
Encapsulation Efficiency (%) |
Advantages | Disadvantages | Refs. |
|---|---|---|---|---|---|---|
| PLGA NPs of curcumin for oral administration. | Solvent Evapration Diffusion | 120–240 (PDI = 0.31) | 77 |
|
37 | |
| PLGA and PEG NPs of curcumin for parenteral administration. | Nano-precipitation | 80–90 | 97.5 |
|
35 | |
| NIPAAM NPs of curcumin containing PEG monoacrylate. | Micellar Aggregation | ~50 | >90 |
|
36 | |
| PLGA NPs of curcumin coated with thiolated chitosan. | Emulsion Solvent Evaporation | 578±67 (pH 7.4) | 28 |
|
|
51 |
| Butylcyanoacrylate NPs of curcumin coated with poloxamer 188. | Anionic Polymerization Solvent Evaporation | 160–240 (PDI ~0.25) | 78 |
|
59 | |
| NIPAAM NPs of curcumin multi layered with PLGA. | Free Radical Polymeriz -ation Double Emulsion Solvent Evaporation | 500–1000 | 49.5 |
|
|
65 |
| Surface modified DMPC SLNs for parenteral administration. | Extrusion through 0.2 µM filter | 187±53 | 97 |
|
|
74 |
Upon oral administration, colloidal particles like nano/micro-particles, are absorbed in their intact form via lympho-epithelial M cells of peyer’s patches. These particles bind to the apical side (towards the lumen) of M cells gets internalized, and are subsequently shuttled to lymphocytes (53). These colloidal carriers transit slowly in the gut which increases the local concentration gradient across the absorptive segments of the intestine, further enhancing the absorption rate (54). NPs as drug delivery vehicles also enables passive targeting in tumors and other inflamed tissues due to increased vascular leakiness that results because of increased production of cytokines and angiogenesis cascades at these sites. In majority of solid tumors, the vascular cut-off pore size ranges between 380–780 nm (55, 56) whereas normal vasculature is impermeable to particles larger than 2–4 nm (57, 58). Such a vast difference in vascular permeability enables the passive targeting of tumor and inflamed tissues by NPs and leads to their accumulation resulting in an enhanced permeation and retention (EPR) effect (55). As a consequence of this passive accumulation at target sites, the concentration of the drug at healthy tissues is correspondingly lower, thereby blunting the intensity of side effects. However, it is noted that for patients with other patho-physiological conditions that are associated with leaky vasculatures, drug delivery by NPs could result in distribution to multiple sites, thereby blunting (to some extent) selectivity for tumor tissues. Such delivery systems are particularly effective in testing and developing new chemical entities including natural compounds like curcumin that possess sub-optimal physicochemical and pharmacokinetic properties to be developed as new drug candidates.
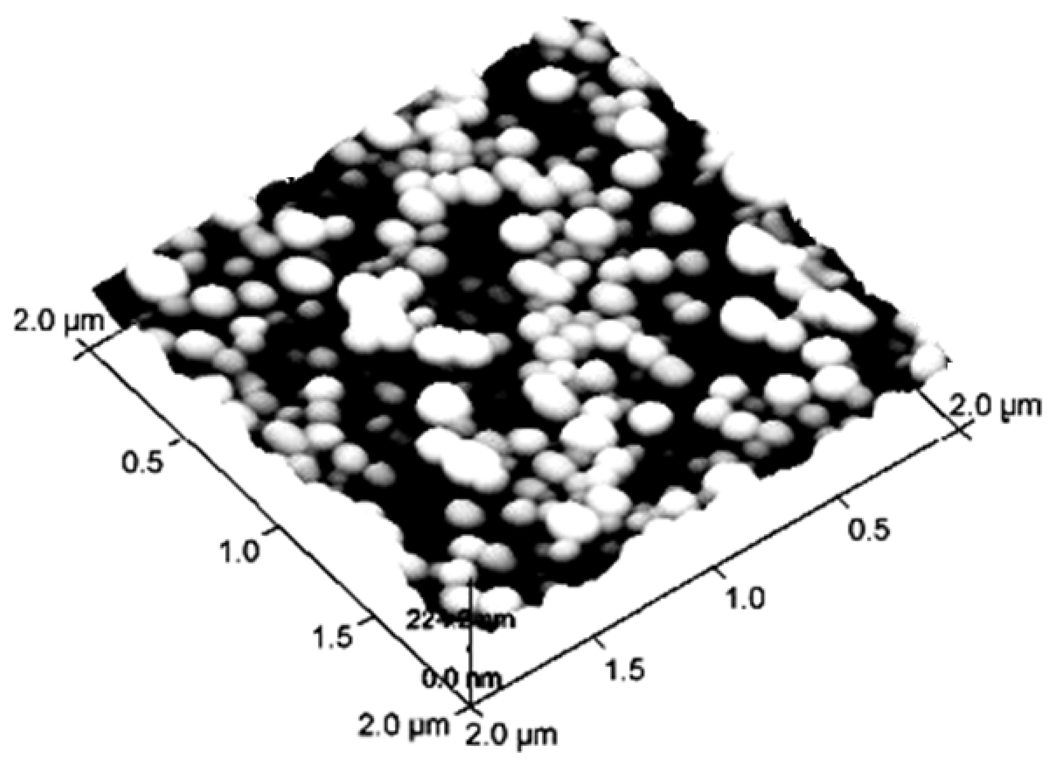
Being lipophilic curcumin partitions/encapsulates into the hydrophobic core of amphiphilic polymers or phospholipids of NPs which not only enhance its bioavailability but also increase its stability by protecting them from the influence of outside environment (51). One of the most investigated method for preparing such NP formulations is emulsion-diffusion-evaporation method which involves solubilizing the drug and/or polymer (Poly(lactic-co-glycolic acid)) in any organic solvent like ethyl acetate, followed by its drop wise addition into an aqueous phase that contains a suitable stabilizer to result into an emulsion. The emulsion can then be homogenized and diluted with a large quantity of water so that solvent diffusion can result in nano-precipitation. This method provides uniformly sized (120–240 nm) spherical NPs of curcumin (Fig. 2), and since solubility of the incorporated drug plays a pivotal role in determining encapsulation efficiency, stabilizers with lower drug solubility were found to be better candidates for achieving high drug encapsulation (37). In vivo studies in rats showed that curcumin NPs increased curcumin bioavailability by 26-fold as compared to oral curcumin suspension and by 9-fold as compared to a curcumin suspension administered in conjunction with piperine (37). Furthermore, similar PLGA NPs, prepared by Anand et al. (35) using F-68 as the solubilizer, were found to possess similar efficacy as free curcumin in killing tumor cells but a higher potency in inhibiting NF-kB activation in cell culture, compared to free curcumin. The authors of this study also claimed superior bioavailability from curcumin NPs; this claim, however, is difficult to assess as curcumin was administered to the mice via i.v. route where bioavailability does not come into play. Nonetheless, an increased half life of the curcumin in plasma was evident (35). Curcumin NPs can also be prepared using other copolymers like N-isopropylacrylamide (NIPAAM), N-vinyl-2-pyrrolidone (VP) and poly(ethyleneglycol) monoacrylate (NIPAAM (VP/PEG A)) (36). These NPs possess very low polydispersity with an average particle size of 50 nm that enables them to freely permeate into different pancreatic cancer cell lines. Although, these curcumin NPs were found to be equally efficacious as free curcumin in cell culture but had an added advantage of their direct injectability into the systemic circulation, thereby bypassing the oral route (36).
Figure 2.
Atomic force microscopy (AFM) image of curcumin-loaded PLGA nanoparticles prepared by emulsion-diffusion-evaporation method (From shaikh et al., reproduced with permission) (37).
Another method to prepare curcumin NPs is by anionic polymerization-solvent-evaporation method (59). This method involves drop-wise addition of a butylcyanoacrylate monomer solution into a constantly stirred acidic ethanol solution containing a suitable surfactant and sodium sulfate. At the critical micelle concentration (CMC), surfactant molecules aggregate together to form a swollen micellar structure containing multiple monomer units. Polymerization of monomer units occurs inside these micelles, forming primary polymer particles that grow in size to form NPs. Curcumin or any other chemopreventive can be added during or after the addition of monomer solution to achieve efficient encapsulation during the growth phase. This method provides uniform NPs (PDI of 0.23–0.27) of 160–240 nm, with particle size directly related to monomer concentration and inversely related to surfactant concentration (59). Furthermore, it also results in the formation of a highly porous structure with a very high surface area that can be loaded with hydrophobic drugs like curcumin (60). These NPs were found to provide higher drug release under in vitro conditions at acidic pH compared to physiological pH, demonstrating their ability to efficiently deliver their cargo inside the cells after degradation by lysosomes, where conditions are more acidic (59).
The other advantage of using polymeric NPs is their amenability to alterations of surface properties. Different functional groups like thiols can be covalently or non-covalently conjugated with the polymeric chains to increase or decrease the mean residence time of the nanoparticles in the gastrointestinal mucosa. Grabovac et al. prepared such PLGA NPs modified at the surface with thiolated chitosan (51). Thiolated chitosans owing to their –SH groups interact with mucus to form disulphide linkages conferring them with highly muco-adhesive properties and hence an increased residence time (61). Furthermore, due to various inter- and intra-molecular disulfide bonds between chitosan molecules, a tight 3D structure results providing a controlled release (61). Other mechanisms like reversible opening of tight junctions and inhibition of efflux P-gp pumps have also been demonstrated to be associated with these thiolated chitosans (62). Although thiolation increases the mean residence time of the coated NPs on the mucosa, it also increases the particle size with decreased encapsulation efficiency of drugs as compared to unmodified NPs (51). The size of curcumin NPs was found to increase from 284–420 nm to 817–960 nm on chitosan coating with half the entrapment efficiency limiting the drug-loading capacity of the thiolated NPs (51).
Another variant of modified NPs is formulation of multi layered polyionic/polymeric shells encapsulating NPs containing drugs. These polyelectrolyte shells are formed as layers over the surfaces of NPs to alter their cell uptake, to attach tumor targeting agents, to increase stability, and/or to control their loading/release characteristics (63). These layered NPs have been demonstrated using gelatin as the polymer and can be prepared by a two step desolvation method followed by formation of layered poly-ionic shells (64). First, the gelatin NPs are prepared by precipitating gelatin from an acidified solution by slowly adding acetone and then cross linking gelatin with glutaraldehyde. Then, an aqueous solution of these NPs can be coated with polyionic shells by the sequential addition of polyanions (polystyrene sulfonate, poly-L-glutamic acid or dextran sulphate) and polycations (polyallylamine HCl, poly-L-lysine, or protamine sulphate) at pH 6. Since gelatin is positively charged at acidic pH, a polyanionic layer forms first followed by a polycation layer. Once prepared, these NPs can be further added to curcumin solution to adsorb curcumin at their surface via hydrophobic interactions that develop between curcumin’s phenol groups and gelatin’s amino acids like proline (63).
Such multi-layered NPs can also be modified for the targeted delivery of chemopreventives. In such nanostructures, polymeric layers with the entrapped chemopreventives encapsulate a magnetic iron core that acts as a targeting system (65). Efficacy of such multi-layered NPs of curcumin was demonstrated by Koppolu et al, (65) using poly (NIPAAM) and PLGA as polymers. In this approach, NIPAAM undergoes free radical polymerization onto the magnetic core via covalent coupling with a silane reagent. The resultant NPs can then be coated with PLGA using a double emulsion solvent evaporation method, yielding NPs of 500–1000 nm size that can be used to deliver both hydrophilic and hydrophobic chemopreventive compounds simultaneously. The hydrophilic compounds can be loaded into the poly (NIPAAM) layer, and the hydrophobic drugs can be loaded into outer PLGA layer (65). However, attachment of multiple poly (NIPAAM) particles at the surface of PLGA particles as well as encapsulation of multiple poly (NIPAAM) particles in the PLGA layer (as opposed to the encapsulation of a single particle) raises some concerns regarding control and the success of the formulation method.
Targeted delivery of chemopreventives can also be achieved by conjugation of NPs or drugs with ligands like folic acid that can recognize some specific surface attributes of target cell types. Different cancer types often over-express some specific epitopes or receptors (66) and bio-conjugation of chemopreventives to ligands having high specificity for these unique surface receptors can help in achieving their targeted delivery to any cancer type. Salmaso et al. (67) demonstrated targeted delivery of curcumin by attaching folic acid (as a ligand) to the polymeric carrier. Presence of folic acid enabled these NPs to undergo clathrin independent endocytosis into cells that specifically over express folic acid receptors. This formulation involved conjugation of PEG, covalently linked to folic acid on one end with isocyanate group of hexamethylene which is further linked to a cyclodextrin curcumin complex on the other end. Hexamethylene is used as a linker to decrease the steric hindrance of bulky PEG chains with cyclodextrin curcumin complex where cyclodextrin was used to bind curcumin into its cavity and to enhance its solubility. These conjugated complexes of curcumin were found to be i) 3,200 times more soluble, ii) ~12 times more stable, iii) 2 times more specific, and iv) 45 times less degradable at pH 7.2 (the degradation rate constant decreased from 321×10−4 min−1 to 7×10−4 min−1) compared to curcumin alone (67). However, an insufficient cell uptake led to limited beneficial effects of this bio-conjugate and further biological investigations are required to demonstrate efficient drug release from the conjugates into the tumor cells.
2.1.2 Solid Lipid Nanoparticles
Solid lipid nanoparticles (SLNs) have also shown significant potential for the delivery of lipophilic compounds like curcumin (68). SLNs were first introduced in mid 1990s as novel drug delivery systems (69) capable of protecting the labile drugs from light/pH/heat mediated degradation, controlled release and excellent biocompatibility/toleratability (70). These are spherical lipid NPs with a high specific surface area that can be easily modified to i) attain a favorable zeta potential, ii) pseudo zero-order kinetics, iii) rapid internalization by cancer cells and iv) impart stealth properties to lessen uptake by the reticulo-endothelial system (RES). These properties make them highly versatile drug delivery systems for a variety of compounds with different physicochemical and pharmacological properties (68). Their lipophilic character enables them to cross the blood brain barrier (BBB), providing a viable alternative vehicle for the delivery of less lipophilic drugs that cannot cross the BBB (47). Furthermore, biological origin of lipid component of these SLNs renders them less toxic as compared to polymeric NPs (71). This drug delivery carrier not only protects the entrapped drug from photochemical or pH mediated degradation but also enables drug targeting and easy large scale production (72, 73). Such characteristics make SLNs as suitable drug delivery carriers for curcumin and other chemopreventives like resveratrol, and β-carotene which owing to their lipid solubility gets localized in the bilayer membrane of lipid vesicles/NPs and results in enhanced bioavailability. Initially, hot homogenization and warm microemulsion techniques were used for the preparation of SLNs but later other advanced techniques like high pressure homogenization, solvent emulsification evaporation/diffusion, high speed stirring, double emulsion method and ultrasonication were introduced (47).
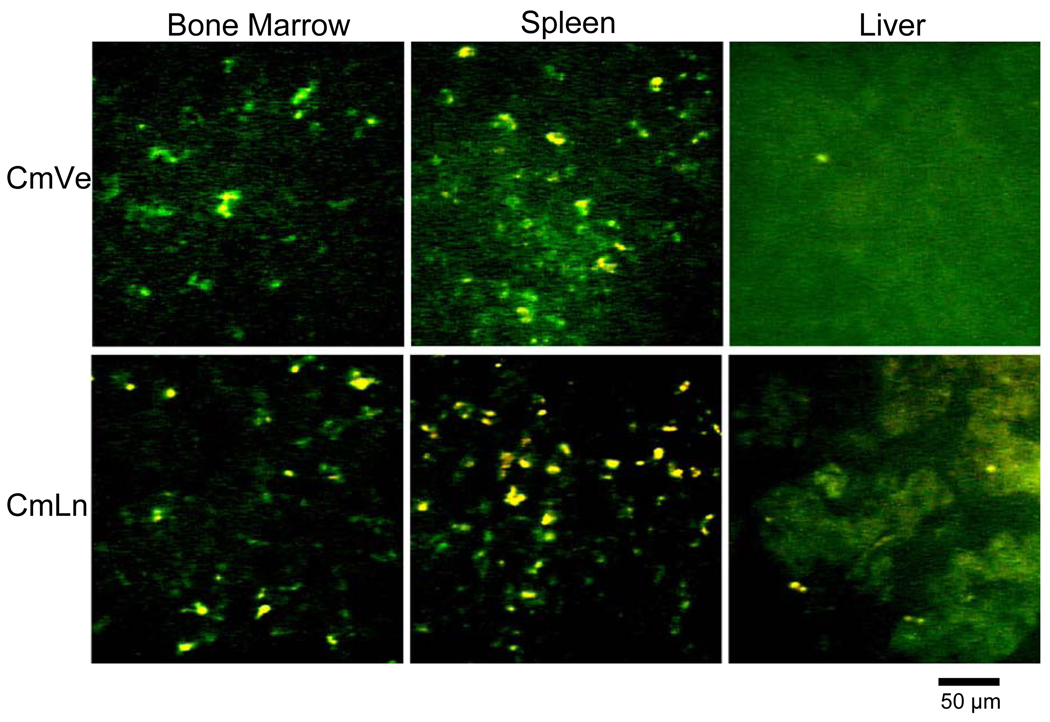
Curcumin SLNs can be formulated using dimyristoyl phophatidylcholine (DMPC) via extrusion through a 0.2 µm filter (74). These vesicles were surface modified by L-glutamic acid, N-(3-carboxy-1-oxopropyl)-1, 5-dihexadecyl ester, and PEG to increase their uptake by macrophages. Since, macrophages produce ROS that leads to oxidative damage and inflammatory responses, curcumin delivery to these macrophages can result in its maximal anti-inflammatory action. Sou et al. (74), has reported localization of curcumin SLNs in macrophage rich sites such as bone marrow, spleen, and liver even at 6 h after the injection, demonstrating their preferential uptake by macrophages and their considerable ROS scavenging potential equivalent to 160 to 1,050 SOD units when analyzed by a hypoxanthine and xanthine oxidase system (74). Although an initial decrease in white blood cells, red blood cells and platelets was observed with these vesicular NPs, the levels of these blood components recovered within 3 h demonstrated absence of any acute toxic response of body towards these delivery vehicles. The potential of this system to deliver curcumin to different tissues was further demonstrated by the presence of yellow fluorescence of curcumin in tissue samples of animals, as detected by confocal microscopy (Fig. 3) (74). One concern with this approach, however, involves an increase in curcumin release from these vesicles at room temperature (20–30°C), suggesting a possible problem with the retention of entrapped curcumin during long storage.
Figure 3.
Confocal scanning images of bone marrow, spleen and liver tissues of rats after 6 h of intravenous administration of curcumin vesicles (CmVe) and curcumin lipid nanospheres (CmLn). Yellow flourescence shows the presence of curcumin in the tissues (From Sou et al., reproduced with permission) (74).
2.2. Liposomes
Liposomes are the spherical bilayer vesicles with an aqueous interior formed by the self association behavior of amphiphilic phospholipids with cholesterol molecules. This self associating behavior of phospholipids originates from their tendency to shield their hydrophobic groups from aqueous environment while interacting with the aqueous phase with their hydrophilic groups. Depending upon their bilayer structure and size, liposomes can be categorized as multilamellar, large unilamellar, or small unilamellar. Alternatively, depending upon the driving force for drug release, they can be classified as conventional liposomes, pH sensitive liposomes, cationic liposomes, immuno-liposomes and long circulating liposomes (reviewed in ref (47). These lipid based particulate carriers can significantly enhance the solubility of poorly water soluble chemopreventives. Different drugs based upon their lipophilic character can distribute either in the phospholipid bilayer, in the interior aqueous phase, or at the bilayer water interface. The lipophilic nature of many chemopreventives including curcumin (Table III), resveratrol (7, 75), oryzanol (76), and N-acetyl cysteine (77), make them suitable candidates for liposomal drug delivery where lipophilic core of these liposomes provide an optimum environment for drug entrapment (78).
Table III.
Liposomal formulations of curcumin for parenteral administration.
| Formulation | Method | Particle Size (nm) |
Encapsulation Efficiency (%) |
Advantages | Refs. |
|---|---|---|---|---|---|
| DMPC:DMPG:Cholesterol (7:1:8) liposomes of curcumin for parenteral administration. | Vortexing of SMLs | N. R. | N. R. |
|
80 |
| Pegylated DMPC, Cholesterol, DMPG liposomes of curcumin for parenteral administration. | Extrusion through 0.22 µm filter | N. R. | N. R. |
|
79 |
| DMPC:DMPG (9:1) liposomes of curcumin for parenteral administration. | Extrusion through 0.22 µm filter | N. R. | N. R. |
|
81 |
| DMPC liposomes coated with PSA specific antobodies. | Sonication of SUVs | 100–150 | N. R. |
|
34 |
N. R.: Not Reported
A liposomal system for the targeted delivery (by coating with prostate membrane antigen specific (PSA) antibodies) of curcumin was also reported to study its partitioning potential (34). It has been observed that DMPC based liposomes possess greater encapsulation efficiency with a more desirable particle size of 100–150 nm as compared to liposomes prepared with dipalmitoyl phosphatidylcholine (DPPC) and egg phosphatidylcholine (PC). Furthermore, DMPC liposomes were found to inhibit (70–80%) cellular proliferation of the human prostate LNCaP and C4-2B cancer cells at 5–10 µM concentration as compared to free curcumin that required 10-fold higher doses to elicit similar inhibition. Both in vitro and in vivo studies have shown that liposomal curcumin is much more effective than free curcumin at equimolar concentrations emphasizing that liposomal delivery of curcumin can enhance their uptake and hence bioavailability/activity into the cells (34). A liposomal formulation of curcumin using dimyristoyl-sn-glycero-3-phosphocholine was also tested for its effects on the modulation of signaling pathways involving proliferation, apoptosis and angiogenesis of human pancreatic carcinoma cells (79). When administered at 40 mg/kg (3 times/wk), this liposomal formulation suppressed the growth of BXPC3 and MiaPaCa2 tumors in a xenograft murine model suggesting in vivo efficacy of these liposomes (79).
Chemopreventives as liposomal formulations can also be delivered trans-cutaneously through hair follicles (83) providing a reservoir for locally applied substances and to enable topical administration. Jung et al. (83) investigated the penetration depth of a novel class of amphoteric liposomes having iso-electric point at slightly acidic pH to measure the efficiency of trans-follicular delivery of curcumin. They found that these liposomes can penetrate ~35 to 69% of the follicle length depending upon the charge on the liposomes, demonstrating their ability for topical delivery of lipophilic chemopreventives for both therapeutic as well as chemopreventive purposes. However, rapid elimination of these liposomal vesicles by active opsonization is known to limit their overall efficacy which can be avoided by modifying the liposomal surface with polymers such as PEG to confer stealth properties to them. Similar liposomal delivery systems are also reported for active curcumin metabolites like tetrahydrocurcumin (THC). Government Pharmaceutical Organization of Thailand developed a tetrahydrocurcumin cream formulation using phospholipid-derived THC liposomes (84). Dermatological tests for irritation, carried out by Wattanakrai et al. (84) on human female volunteers, demonstrated that these liposomes not only were safe but also possessed a significantly lower irritation potential compared to the reference material. Furthermore, a corneometer analysis of the skin above antecubital fossae revealed a higher moisturizing effect, which further showed that topical delivery of liposomal curcumin can be used in various skin ailments. However, some of the major problems of this delivery system include stability, poor batch to batch reproducibility, sterilization difficulties, and low drug loading (85).
2.3. Microemulsions/Microencapsulation
Microemulsions are one of the most widely-used drug delivery systems capable of providing high drug entrapment efficiency with long term stability of hydrophobic molecules (82). These thermodynamically stable, optically isotropic, transparent formulations are characterized by a dynamic microstructure that results spontaneously by mixing lipophilic and hydrophilic excipients in presence of suitable surfactants (86). This microstructure results in high drug solubilization capacity along with free and fast drug diffusion (87) that coupled with lipophilic nature endow them with a high potential for delivering lipophilic compounds like curcumin not only across lipophilic cell membranes but also through skin. Studies by Teichmann et al. (87), demonstrated that curcumin can easily be delivered through the stratum corneum and into the complete follicular infundibula via o/w (oil in water) micro-emulsions. These micro-emulsions can be further formulated into hydrogel patches of chitosan or chitosan starch blends to protect the drug from the detrimental effects of pH, light and/or oxygen mediated degradation (88). Once these agents are micro-emulsified and entrapped into a hydrogel like matrix, their stability increases significantly and controlled release at a desirable site can be obtained. Studies have shown that even after 2 months of storage at room temperature mean hydrodynamic diameter of the oily internal phase increases slightly, demonstrating the high stability and efficiency of such hydrogels (88). In addition, the external aqueous phase of these emulsions provides hydration to the stratum corneum and moisturizes the skin (88). Drug release from micro-emulsified droplets can be further augmented by using external energy sources such as ultrasonic waves. It has been observed that on application of external energy these droplets undergo a structural reorganization that results in the phase separation of oil droplets from the aqueous vehicle releasing the compound (82). Similarly, a microemsulsion cream formulation of curcumin SLNs was also described by Tiyaboonchai et al. (89). An entrapment efficiency of 35–70% was demonstrated for curcumin in SLNs with a diffusion mediated controlled release pattern. In addition, the formulation was found to increase the photo stability of curcumin where after 6 months of storage, with no significant change in the viscosity or color of the formulation (89). Although this approach seems promising in enhancing the delivery of potent therapeutics, its usefulness for chemopreventives has not been established in animal and human clinical studies.
Aziz et al. (90) prepared microcapsules of curcumin with gelatin using ethanol/acetone as coacervating agents to separate the two phases that result in precipitation of the drug in spherical microcapsules. They prepared curcumin dispersion in the gelatin solution followed by its addition to ethanol. A Formaldehyde solution (37% v/v) was then added to provide rigidity to gelatin coating. It was reported that micro-encapsulation yield, drug loading and entrapment efficiency all were significantly affected by the solubility of curcumin in the coacervating solvents. They were higher when acetone was used to dissolve curcumin as compared to ethanol in which curcumin tend to disperse at high concentrations used for loading into micro-emulsions. Furthermore, the microcapsules prepared by using acetone were found to possess better flowability and high stability with retention of their spherical shape (90). A similar injectable microparticulate formulation of curcumin using PLGA polymer was prepared and used in breast cancer chemoprevention study (91). These microparticles were found to provide sustained blood and tissue levels for around 1 month by a single subcutaneous injection with tissue levels 10–30 fold higher in brain and lung as compared to that in plasma suggesting their potential to sustain drug levels on subcutaneous administration (Table IV).
Table IV.
Microparticle/microemulsion formulations of curcumin.
| Formulation | Method | Particle Size |
Encapsulation Efficiency (%) |
Advantages | Refs. |
|---|---|---|---|---|---|
| Curcumin macrocapsules prepared with gelatin. | Coacervation Method | 80–90 µm | 75.5 |
|
90 |
| PLGA microparticles of curcumin for parenteral administration. | Emulsion Solvent Evaporation | 22±9 µm | 75 |
|
91 |
| Curcumin microemulsion (o/w) formulated into a hydrogel matrix for topical application. | Surfactant mediated Microemulsification | 45–50 nm | N. R. |
|
88 |
| Microemulsified curcumin loaded SLNs for topical appication. | Microemulsification | 450 nm (PDI 0.4) | 70 |
|
89 |
N. R.: Not Reported
2.4. Implantable Drug Delivery Systems
Over the past few decades, polymeric implantable drug delivery systems have exhibited tremendous potential for systemic delivery of various therapeutic agents, including carmustine and leuprolide at a controlled rate (92, 93). These implants with homogenous entrapment of drugs in a polymeric matrix achieve sustained localized delivery coupled with complete bioavailability into systemic circulation by slowly releasing the encapsulated drug at the site of implantation (94). Furthermore, due to their slow release kinetics, implants can provide drug release ranging from months to years which improves the patient compliance, especially for poorly bioavailable and rapidly metabolized compounds like curcumin (95).
There are 2 type of implantable drug delivery systems; reservoir type and matrix type. In reservoir type implants, drug core is coated by a semi permeable polymeric membrane which controls the rate of drug release and is dependent upon the rate of water influx into the system (96). But the reservoir type implants are often discouraged due to their probability of dose dumping. Matrix type implants on the other hand contain uniformly distributed drug into the polymeric matrix (96). Depending upon the polymer degradation characteristics they can be surface erosion type (degrade only at the surface) or bulk erosion type (slow uniform degradation in the bulk of the implant) (93). Matrix type implants are devoid of any dose dumping phenomenon and provide desirable biphasic drug release mediated by diffusion. This biphasic release consists of a burst release followed by a slow controlled release. Initial burst release delivers the drug for distribution to a large volume, to rapidly reach the therapeutic concentration and a slow, controlled release maintains the therapeutic concentrations for prolonged periods of time (97).
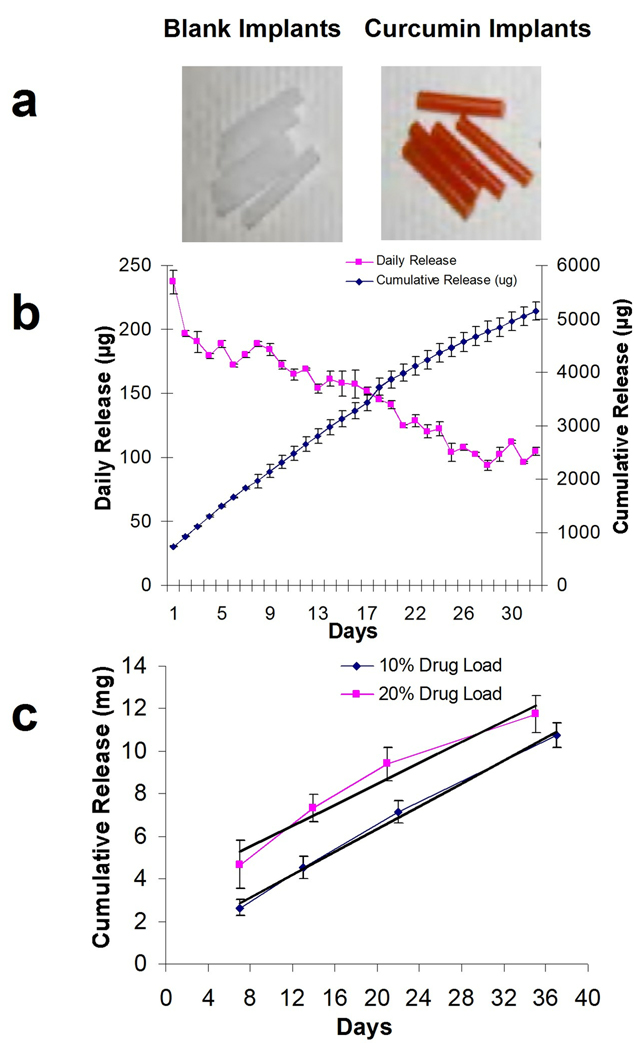
Recently, we developed poly(ε-caprolactone) (PCL) implants using solvent evaporation coupled with melt extrusion technique for many natural compounds, including curcumin (98). Implants were prepared by dissolving PCL together with F68 (PCL:F68, 9:1) in dichloromethane (DCM) and drug in ethanol and mixing the two solutions with stirring to prepare a homogenous solution. The solvents were then evaporated on a water bath maintained at 65 °C for 1–2 h. The semi solid residue was then concentrated overnight under vacuum to ensure complete removal of the solvents. The dried polymeric material was melted and extruded at 70°C into silastic tubing (internal diameter 3.4 mm) attached to a syringe and then cut into desired lengths (Fig. 4a). These implants were optimized under in vitro conditions for drug release kinetics by incubating them in PBS supplemented with (10% v/v) BCS (to simulate extracellular fluid conditions) and by changing the media daily to measure the drug released. In vitro release studies showed a biphasic release pattern for curcumin where an initial burst release was observed for the first week from surface bound drug followed by a diffusion controlled release from inner layers of polymeric matrix (Fig. 4b) (10). Measurement of residual curcumin in the implants (2-cm implant; 200 mg; 10 or 20% drug load) recovered from Sprague Dawley rats at the time of euthanasia showed ~1.8–2 fold higher cumulative drug release over a period of 5 weeks compared to in vitro release but with similar release kinetics (Fig 4c) (10). These implants (2 cm, 200 mg, 10% drug load) released ~2.64 mg (13.2 %) of curcumin in the first week with an average daily release of ~370 µg/day which dropped slowly to around 240 µg/day after 35 days of implantation (10). Other studies conducted in this laboratory showed that these implants are stable and can release up to ~0.2 mg curcumin per week even after 42 weeks of implantation (98).
Figure 4.
(a) shows photographs of blank implants and of curcumin implants. (b) In Vitro release of curcumin from a 2-cm implant (3.4 mm diameter; 200 mg) with 10% curcumin load (n=3). (c) In vivo release of curcumin from a 2-cm implant formulated either with 10% or 20% curcumin load (n=3). Implants were grafted subcutaneously at the back of Sprague-Dawley rats and were recovered at the time of euthanasia at indicated times to measure the residual curcumin content. Cumulative release was calculated by subtracting residual amount at each interval from initial amount of drug present in implants (reproduced with permission from data published by Bansal et al.) (10).
This polymeric implant delivery system not only provided high local concentrations of curcumin but also enabled systemic delivery of curcumin and other phytochemicals such as green tea polyphenols, punicalagins, and diindolylmethane to various other organs of the body (98). These implants were found to deliver significantly higher levels of curcumin in the plasma, liver and brain tissues compared to the oral delivery of curcumin (unpublished data). Analysis of liver tissue from Sprague Dawley rats implanted with two 2-cm curcumin implants (200 mg implant with 10% drug load) showed presence of 60 ± 20 ng/g of curcumin after 4 days of implantation which dropped to 8–15 ng/g after 7 days and stayed almost constant over a period of 5 weeks (10). Furthermore, curcumin delivered via the implant route was found to inhibit benzo[a]pyrene induced tissue DNA adducts, demonstrating the biological efficacy of systemic delivery of these chemopreventives at substantially reduced (25 to 50 fold) doses compared to the traditional oral route (99). In summary, this novel, continuous release (“24/7”) implant delivery concept has been found to 1) be applicable for many commonly used chemopreventive agents of varied lipophilicities; 2) circumvent bioavailability issues for many of these agents compared to their administration by the traditional oral route; and 3) enable minor components of plant origin to be tested in vivo for their chemopreventive/chemotherapeutic potential, which otherwise remain uninvestigated due to the high quantities required for oral delivery.
3. Bioavailability issues for other chemopreventives
Although in this review we have focused on oral bioavailability issues for curcumin and the advanced delivery systems that can enhance its bioavailability, the oral bioavailabilty problem has also been encountered for many naturally occurring chemopreventives, e.g., EGCG, resveratrol and ellagic acid, and the delivery systems described for curcumin can be readily adopted for these and other compounds. The natural compounds like EGCG, ellagic acid, resveratrol that showed efficacy in cell culture studies elicited limited activity in several animal studies. These compounds possess poor biopharmaceutical properties with low oral bioavailability, limited either by poor aqueous solubility and/or permeability for absorption into the systemic circulation. As a result, the advanced drug delivery systems like nanoparticles (ellagic acid (5), resveratrol (100), EGCG (4) and quercetin (101)), liposomes (resveratrol (7), EGCG (6), quercetin (102), β carotene (103)), microparticles (quercetin (8), EGCG (9) and resveratrol (104)) and polymeric implants (EGCG, resveratrol, punicalagans, di-indoylmethane, withaferin A, tanshinone II, etc.) (our unpublished data) have been developed to circumvent their bioavailability issues.
Conclusions
Since ancient times, plant-derived compounds that are known to possess a plethora of activities have been used in the treatment and prevention of many ailments, including cancer. However, even after half a century of research, none of the naturally occurring compounds (including the most investigated ones such as curcumin and EGCG) have managed to find a place in the physician’s armamentarium for prophylactic treatments. The main reasons for their limited success in the clinical setting are their poor bioavailability, rapid rate of metabolism, or both. The quest to utilize traditional natural compounds for their chemotherapeutic and chemopreventive potential in the clinical setting has motivated drug delivery scientists to devise advanced drug-delivery systems such as nanoparticles, liposomes, microemulsions, and implants. Although research on most of these delivery systems has demonstrated the potential for enhanced bioavailability, two important aspects would need attention: 1) the occurrence of rapid drug metabolism (e.g. for curcumin), which may be mitigated by the application of combination therapies such as with enzyme inhibitors like piperine; and 2) the need for frequent parenteral dosing, in order to maintain effective therapeutic concentrations in the blood. It is now clear that further development of naturally occurring compounds with chemopreventive/chemotherapeutic potential will be dictated by the development of formulations that can bypass their poor oral bioavailability along with eliminating hepatic first pass metabolism while not compromising with patient acceptability.
Acknowledgments
Financial Support
This work was supported by USPHS grants CA-118114, CA-125152, Kentucky Lung Cancer Research Program and the Agnes Brown Duggan Endowment. R.C.G. holds the Agnes Brown Duggan Chair in Oncological Research.
Abbreviations
- AFM
Atomic force microscopy
- BBB
blood brain barrier
- BCS
bovine calf serum
- B[a]P
benzo[a]pyrene
- CMC
critical micelle concentration
- DMPC
dimyristoyl phophatidylcholine
- DPPC
dipalmitoyl phosphatidylcholine
- EGCG
epigallo catechin gallate
- EPR
enhanced permeation and retention
- NIPAAM
N-isopropylacrylamide
- NNI
National Nanotechnology Initiative
- NPs
nanoparticles
- PC
phosphatidylcholine
- PCL
poly(ε-caprolactone)
- PLGA
poly(lactic-co-glycolic acid
- PEG
polyethylene glycol
- RES
reticulo-endothelial system
- ROS
reactive oxygen species
- SLNs
Solid lipid nanoparticles
- THC
tetrahydrocurcumin
- VP
N-vinyl-2-pyrrolidone
References
- 1.Sporn MB, Suh N. Chemoprevention of cancer. Carcinogenesis. 2000;21:525–530. doi: 10.1093/carcin/21.3.525. [DOI] [PubMed] [Google Scholar]
- 2.Sporn MB. Approaches to prevention of epithelial cancer during the preneoplastic period. Cancer Res. 1976;36:2699–2702. [PubMed] [Google Scholar]
- 3.Shureiqi I, Reddy P, Brenner DE. Chemoprevention: general perspective. Crit Rev Oncol Hematol. 2000;33:157–167. doi: 10.1016/s1040-8428(99)00072-4. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqui IA, Adhami VM, Bharali DJ, Hafeez BB, Asim M, Khwaja SI, et al. Introducing nanochemoprevention as a novel approach for cancer control: proof of principle with green tea polyphenol epigallocatechin-3-gallate. Cancer Res. 2009;69:1712–1716. doi: 10.1158/0008-5472.CAN-08-3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sonaje K, Italia JL, Sharma G, Bhardwaj V, Tikoo K, Kumar MN. Development of biodegradable nanoparticles for oral delivery of ellagic acid and evaluation of their antioxidant efficacy against cyclosporine A-induced nephrotoxicity in rats. Pharm Res. 2007;24:899–908. doi: 10.1007/s11095-006-9207-y. [DOI] [PubMed] [Google Scholar]
- 6.Fang JY, Hung CF, Hwang TL, Huang YL. Physicochemical characteristics and in vivo deposition of liposome-encapsulated tea catechins by topical and intratumor administrations. J Drug Target. 2005;13:19–27. doi: 10.1080/10611860400015977. [DOI] [PubMed] [Google Scholar]
- 7.Narayanan NK, Nargi D, Randolph C, Narayanan BA. Liposome encapsulation of curcumin and resveratrol in combination reduces prostate cancer incidence in PTEN knockout mice. Int J Cancer. 2009;125:1–8. doi: 10.1002/ijc.24336. [DOI] [PubMed] [Google Scholar]
- 8.Scalia S, Mezzena M. Incorporation of quercetin in lipid microparticles: effect on photo- and chemical-stability. J Pharm Biomed Anal. 2009;49:90–94. doi: 10.1016/j.jpba.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Shutava TG, Balkundi SS, Lvov YM. (−)−Epigallocatechin gallate/gelatin layer-by-layer assembled films and microcapsules. J Colloid Interface Sci. 2009;330:276–283. doi: 10.1016/j.jcis.2008.10.082. [DOI] [PubMed] [Google Scholar]
- 10.Bansal SS, Vadhanam MV, Gupta RC. Development and In Vitro-In Vivo Evaluation of Polymeric Implants for Continuous Systemic Delivery of Curcumin. Pharm Res. 2011 doi: 10.1007/s11095-011-0375-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Meyskens FL, Jr, McLaren CE. Chemoprevention, risk reduction, therapeutic prevention, or preventive therapy? J Natl Cancer Inst. 2010;102:1815–1817. doi: 10.1093/jnci/djq466. [DOI] [PubMed] [Google Scholar]
- 12.Aggarwal BB, Sung B. Pharmacological basis for the role of curcumin in chronic diseases: an age-old spice with modern targets. Trends Pharmacol Sci. 2009;30:85–94. doi: 10.1016/j.tips.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Anand P, Thomas SG, Kunnumakkara AB, Sundaram C, Harikumar KB, Sung B, et al. Biological activities of curcumin and its analogues (Congeners) made by man and Mother Nature. Biochem Pharmacol. 2008;76:1590–1611. doi: 10.1016/j.bcp.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Aggarwal BB, Harikumar KB. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol. 2009;41:40–59. doi: 10.1016/j.biocel.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aggarwal BB, Kumar A, Bharti AC. Anticancer potential of curcumin: preclinical and clinical studies. Anticancer Res. 2003;23:363–398. [PubMed] [Google Scholar]
- 16.Aggarwal BB. Apoptosis and nuclear factor-kappa B: a tale of association and dissociation. Biochem Pharmacol. 2000;60:1033–1039. doi: 10.1016/s0006-2952(00)00393-2. [DOI] [PubMed] [Google Scholar]
- 17.Bierhaus A, Zhang Y, Quehenberger P, Luther T, Haase M, Muller M, et al. The dietary pigment curcumin reduces endothelial tissue factor gene expression by inhibiting binding of AP-1 to the DNA and activation of NF-kappa B. Thromb Haemost. 1997;77:772–782. [PubMed] [Google Scholar]
- 18.Brennan P, O'Neill LA. Inhibition of nuclear factor kappaB by direct modification in whole cells--mechanism of action of nordihydroguaiaritic acid, curcumin and thiol modifiers. Biochem Pharmacol. 1998;55:965–973. doi: 10.1016/s0006-2952(97)00535-2. [DOI] [PubMed] [Google Scholar]
- 19.Thangapazham RL, Sharma A, Maheshwari RK. Multiple molecular targets in cancer chemoprevention by curcumin. AAPS J. 2006;8:E443–E449. doi: 10.1208/aapsj080352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh SV, Hu X, Srivastava SK, Singh M, Xia H, Orchard JL, et al. Mechanism of inhibition of benzo[a]pyrene-induced forestomach cancer in mice by dietary curcumin. Carcinogenesis. 1998;19:1357–1360. doi: 10.1093/carcin/19.8.1357. [DOI] [PubMed] [Google Scholar]
- 21.Balogun E, Hoque M, Gong P, Killeen E, Green CJ, Foresti R, et al. Curcumin activates the haem oxygenase-1 gene via regulation of Nrf2 and the antioxidant-responsive element. Biochem J. 2003;371:887–895. doi: 10.1042/BJ20021619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kasim NA, Whitehouse M, Ramachandran C, Bermejo M, Lennernas H, Hussain AS, et al. Molecular properties of WHO essential drugs and provisional biopharmaceutical classification. Mol Pharm. 2004;1:85–96. doi: 10.1021/mp034006h. [DOI] [PubMed] [Google Scholar]
- 23.Pan MH, Huang TM, Lin JK. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos. 1999;27:486–494. [PubMed] [Google Scholar]
- 24.Shoba G, Joy D, Joseph T, Majeed M, Rajendran R, Srinivas PS. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64:353–356. doi: 10.1055/s-2006-957450. [DOI] [PubMed] [Google Scholar]
- 25.Ravindranath V, Chandrasekhara N. Metabolism of curcumin--studies with [3H]curcumin. Toxicology. 1981;22:337–344. doi: 10.1016/0300-483x(81)90027-5. [DOI] [PubMed] [Google Scholar]
- 26.Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of curcumin: problems and promises. Mol Pharm. 2007;4:807–818. doi: 10.1021/mp700113r. [DOI] [PubMed] [Google Scholar]
- 27.Carroll RE, Benya RV, Turgeon DK, Vareed S, Neuman M, Rodriguez L, et al. Phase IIa Clinical Trial of Curcumin for the Prevention of Colorectal Neoplasia. Cancer Prev Res. 2011;4:354–364. doi: 10.1158/1940-6207.CAPR-10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wahlang B, Pawar YB, Bansal AK. Identification of permeability-related hurdles in oral delivery of curcumin using the Caco-2 cell model. Eur J Pharm Biopharm. 2011;77:275–282. doi: 10.1016/j.ejpb.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Ireson CR, Jones DJ, Orr S, Coughtrie MW, Boocock DJ, Williams ML, et al. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidemiol Biomarkers Prev. 2002;11:105–111. [PubMed] [Google Scholar]
- 30.Ravindranath V, Chandrasekhara N. In vitro studies on the intestinal absorption of curcumin in rats. Toxicology. 1981;20:251–257. doi: 10.1016/0300-483x(81)90056-1. [DOI] [PubMed] [Google Scholar]
- 31.Ravindranath V, Chandrasekhara N. Absorption and tissue distribution of curcumin in rats. Toxicology. 1980;16:259–265. doi: 10.1016/0300-483x(80)90122-5. [DOI] [PubMed] [Google Scholar]
- 32.Holder GM, Plummer JL, Ryan AJ. The metabolism and excretion of curcumin (1,7-bis-(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione) in the rat. Xenobiotica. 1978;8:761–768. doi: 10.3109/00498257809069589. [DOI] [PubMed] [Google Scholar]
- 33.Ma Z, Haddadi A, Molavi O, Lavasanifar A, Lai R, Samuel J. Micelles of poly(ethylene oxide)-b-poly(epsilon-caprolactone) as vehicles for the solubilization, stabilization, and controlled delivery of curcumin. J Biomed Mater Res A. 2008;86:300–310. doi: 10.1002/jbm.a.31584. [DOI] [PubMed] [Google Scholar]
- 34.Thangapazham RL, Puri A, Tele S, Blumenthal R, Maheshwari RK. Evaluation of a nanotechnology-based carrier for delivery of curcumin in prostate cancer cells. Int J Oncol. 2008;32:1119–1123. [PMC free article] [PubMed] [Google Scholar]
- 35.Anand P, Nair HB, Sung B, Kunnumakkara AB, Yadav VR, Tekmal RR, et al. Design of curcumin-loaded PLGA nanoparticles formulation with enhanced cellular uptake, and increased bioactivity in vitro and superior bioavailability in vivo. Biochem Pharmacol. 2009 doi: 10.1016/j.bcp.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Bisht S, Feldmann G, Soni S, Ravi R, Karikar C, Maitra A. Polymeric nanoparticle-encapsulated curcumin ("nanocurcumin"): a novel strategy for human cancer therapy. J Nanobiotechnology. 2007;5:3. doi: 10.1186/1477-3155-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaikh J, Ankola DD, Beniwal V, Singh D, Kumar MN. Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur J Pharm Sci. 2009;37:223–230. doi: 10.1016/j.ejps.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 38.Ganta S, Amiji M. Coadministration of Paclitaxel and curcumin in nanoemulsion formulations to overcome multidrug resistance in tumor cells. Mol Pharm. 2009;6:928–939. doi: 10.1021/mp800240j. [DOI] [PubMed] [Google Scholar]
- 39.Maiti K, Mukherjee K, Gantait A, Saha BP, Mukherjee PK. Curcumin-phospholipid complex: Preparation, therapeutic evaluation and pharmacokinetic study in rats. Int J Pharm. 2007;330:155–163. doi: 10.1016/j.ijpharm.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 40.Wahlstrom B, Blennow G. A study on the fate of curcumin in the rat. Acta Pharmacol Toxicol (Copenh) 1978;43:86–92. doi: 10.1111/j.1600-0773.1978.tb02240.x. [DOI] [PubMed] [Google Scholar]
- 41.Sharma RA, Ireson CR, Verschoyle RD, Hill KA, Williams ML, Leuratti C, et al. Effects of dietary curcumin on glutathione S-transferase and malondialdehyde-DNA adducts in rat liver and colon mucosa: relationship with drug levels. Clin Cancer Res. 2001;7:1452–1458. [PubMed] [Google Scholar]
- 42.Ireson C, Orr S, Jones DJ, Verschoyle R, Lim CK, Luo JL, et al. Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production. Cancer Res. 2001;61:1058–1064. [PubMed] [Google Scholar]
- 43.Baum L, Lam CW, Cheung SK, Kwok T, Lui V, Tsoh J, et al. Six-month randomized, placebo-controlled, double-blind, pilot clinical trial of curcumin in patients with Alzheimer disease. J Clin Psychopharmacol. 2008;28:110–113. doi: 10.1097/jcp.0b013e318160862c. [DOI] [PubMed] [Google Scholar]
- 44.Dhillon N, Aggarwal BB, Newman RA, Wolff RA, Kunnumakkara AB, Abbruzzese JL, et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14:4491–4499. doi: 10.1158/1078-0432.CCR-08-0024. [DOI] [PubMed] [Google Scholar]
- 45.Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21:2895–2900. [PubMed] [Google Scholar]
- 46.Garcea G, Jones DJ, Singh R, Dennison AR, Farmer PB, Sharma RA, et al. Detection of curcumin and its metabolites in hepatic tissue and portal blood of patients following oral administration. Br J Cancer. 2004;90:1011–1015. doi: 10.1038/sj.bjc.6601623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bawarski WE, Chidlowsky E, Bharali DJ, Mousa SA. Emerging nanopharmaceuticals. Nanomedicine. 2008;4:273–282. doi: 10.1016/j.nano.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 48.Khan JA, Kainthan RK, Ganguli M, Kizhakkedathu JN, Singh Y, Maiti S. Water soluble nanoparticles from PEG-based cationic hyperbranched polymer and RNA that protect RNA from enzymatic degradation. Biomacromolecules. 2006;7:1386–1388. doi: 10.1021/bm050999o. [DOI] [PubMed] [Google Scholar]
- 49.Schluep T, Hwang J, Hildebrandt IJ, Czernin J, Choi CH, Alabi CA, et al. Pharmacokinetics and tumor dynamics of the nanoparticle IT-101 from PET imaging and tumor histological measurements. Proc Natl Acad Sci U S A. 2009;106:11394–11399. doi: 10.1073/pnas.0905487106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Italia JL, Bhatt DK, Bhardwaj V, Tikoo K, Kumar MN. PLGA nanoparticles for oral delivery of cyclosporine: nephrotoxicity and pharmacokinetic studies in comparison to Sandimmune Neoral. J Control Release. 2007;119:197–206. doi: 10.1016/j.jconrel.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 51.Grabovac V, Bernkop-Schnurch A. Development and in vitro evaluation of surface modified poly(lactide-co-glycolide) nanoparticles with chitosan-4-thiobutylamidine. Drug Dev Ind Pharm. 2007;33:767–774. doi: 10.1080/03639040601050163. [DOI] [PubMed] [Google Scholar]
- 52.Koo OM, Rubinstein I, Onyuksel H. Role of nanotechnology in targeted drug delivery and imaging: a concise review. Nanomedicine. 2005;1:193–212. doi: 10.1016/j.nano.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 53.Volkheimer G, Schulz FH, Lehmann H, Aurich I, Hubner R, Hubner M, et al. Primary portal transport of persorbed starch granules from the intestinal wall. Med Exp Int J Exp Med. 1968;18:103–108. doi: 10.1159/000137143. [DOI] [PubMed] [Google Scholar]
- 54.Hussain N, Jaitley V, Florence AT. Recent advances in the understanding of uptake of microparticulates across the gastrointestinal lymphatics. Adv Drug Deliv Rev. 2001;50:107–142. doi: 10.1016/s0169-409x(01)00152-1. [DOI] [PubMed] [Google Scholar]
- 55.Hobbs SK, Monsky WL, Yuan F, Roberts WG, Griffith L, Torchilin VP, et al. Regulation of transport pathways in tumor vessels: role of tumor type and microenvironment. Proc Natl Acad Sci U S A. 1998;95:4607–4612. doi: 10.1073/pnas.95.8.4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yuan F, Dellian M, Fukumura D, Leunig M, Berk DA, Torchilin VP, et al. Vascular permeability in a human tumor xenograft: molecular size dependence and cutoff size. Cancer Res. 1995;55:3752–3756. [PubMed] [Google Scholar]
- 57.Gerlowski LE, Jain RK. Microvascular permeability of normal and neoplastic tissues. Microvasc Res. 1986;31:288–305. doi: 10.1016/0026-2862(86)90018-x. [DOI] [PubMed] [Google Scholar]
- 58.Siflinger-Birnboim A, Del Vecchio PJ, Cooper JA, Blumenstock FA, Shepard JM, Malik AB. Molecular sieving characteristics of the cultured endothelial monolayer. J Cell Physiol. 1987;132:111–117. doi: 10.1002/jcp.1041320115. [DOI] [PubMed] [Google Scholar]
- 59.Mulik R, Mahadik K, Paradkar A. Development of curcuminoids loaded poly(butyl) cyanoacrylate nanoparticles: Physicochemical characterization and stability study. Eur J Pharm Sci. 2009;37:395–404. doi: 10.1016/j.ejps.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 60.Petri B, Bootz A, Khalansky A, Hekmatara T, Muller R, Uhl R, et al. Chemotherapy of brain tumour using doxorubicin bound to surfactant-coated poly(butyl cyanoacrylate) nanoparticles: revisiting the role of surfactants. J Control Release. 2007;117:51–58. doi: 10.1016/j.jconrel.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 61.Werle M, Takeuchi H, Bernkop-Schnurch A. Modified chitosans for oral drug delivery. J Pharm Sci. 2009;98:1643–1656. doi: 10.1002/jps.21550. [DOI] [PubMed] [Google Scholar]
- 62.Werle M, Hoffer M. Glutathione and thiolated chitosan inhibit multidrug resistance P-glycoprotein activity in excised small intestine. J Control Release. 2006;111:41–46. doi: 10.1016/j.jconrel.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 63.Ai H, Jones SA, Lvov YM. Biomedical applications of electrostatic layer-by-layer nano-assembly of polymers, enzymes, and nanoparticles. Cell Biochem Biophys. 2003;39:23–43. doi: 10.1385/CBB:39:1:23. [DOI] [PubMed] [Google Scholar]
- 64.Shutava TG, Balkundi SS, Vangala P, Steffan JJ, Bigelow RL, Cardelli JA, et al. Layer-by-Layer-Coated Gelatin Nanoparticles as a Vehicle for Delivery of Natural Polyphenols. ACS Nano. 2009 doi: 10.1021/nn900451a. [DOI] [PubMed] [Google Scholar]
- 65.Koppolu BP, Rahimi M, Nattama SP, Wadajkar A, Nguyen K. Development of multiple-layer polymeric particles for targeted and controlled drug delivery. Nanomedicine. 2009 doi: 10.1016/j.nano.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Willis M, Forssen E. Ligand-targeted liposomes. Adv Drug Deliv Rev. 1998;29:249–271. doi: 10.1016/s0169-409x(97)00083-5. [DOI] [PubMed] [Google Scholar]
- 67.Salmaso S, Bersani S, Semenzato A, Caliceti P. New cyclodextrin bioconjugates for active tumour targeting. J Drug Target. 2007;15:379–390. doi: 10.1080/10611860701349752. [DOI] [PubMed] [Google Scholar]
- 68.Gasco MR. Lipid nanoparticles: perspectives and challenges. Adv Drug Deliv Rev. 2007;59:377–378. doi: 10.1016/j.addr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 69.Siekmann B, Westesen K. Sub-micron sized parenteral carrier systems based on solid lipid. Pharmacol Lett. 1992;1:123–126. [Google Scholar]
- 70.Muller RH, Mader K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery - a review of the state of the art. Eur J Pharm Biopharm. 2000;50:161–177. doi: 10.1016/s0939-6411(00)00087-4. [DOI] [PubMed] [Google Scholar]
- 71.Kaur IP, Bhandari R, Bhandari S, Kakkar V. Potential of solid lipid nanoparticles in brain targeting. J Control Release. 2008;127:97–109. doi: 10.1016/j.jconrel.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 72.Marengo E, Cavalli R, Caputo O, Rodriguez L, Gasco MR. Scale-up of the preparation process of solid lipid nanospheres. Part I. Int J Pharm. 2000;205:3–13. doi: 10.1016/s0378-5173(00)00471-3. [DOI] [PubMed] [Google Scholar]
- 73.Mehnert W, Mader K. Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev. 2001;47:165–196. doi: 10.1016/s0169-409x(01)00105-3. [DOI] [PubMed] [Google Scholar]
- 74.Sou K, Inenaga S, Takeoka S, Tsuchida E. Loading of curcumin into macrophages using lipid-based nanoparticles. Int J Pharm. 2008;352:287–293. doi: 10.1016/j.ijpharm.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 75.Kristl J, Teskac K, Caddeo C, Abramovic Z, Sentjurc M. Improvements of cellular stress response on resveratrol in liposomes. Eur J Pharm Biopharm. 2009;73:253–259. doi: 10.1016/j.ejpb.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 76.Viriyaroj A, Ngawhirunpat T, Sukma M, Akkaramongkolporn P, Ruktanonchai U, Opanasopit P. Physicochemical properties and antioxidant activity of gamma-oryzanol-loaded liposome formulations for topical use. Pharm Dev Technol. 2009;14:665–671. doi: 10.3109/10837450902911937. [DOI] [PubMed] [Google Scholar]
- 77.Mitsopoulos P, Omri A, Alipour M, Vermeulen N, Smith MG, Suntres ZE. Effectiveness of liposomal-N-acetylcysteine against LPS-induced lung injuries in rodents. Int J Pharm. 2008;363:106–111. doi: 10.1016/j.ijpharm.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 78.Kunwar A, Barik A, Pandey R, Priyadarsini KI. Transport of liposomal and albumin loaded curcumin to living cells: an absorption and fluorescence spectroscopic study. Biochim Biophys Acta. 2006;1760:1513–1520. doi: 10.1016/j.bbagen.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 79.Li L, Braiteh FS, Kurzrock R. Liposome-encapsulated curcumin: in vitro and in vivo effects on proliferation, apoptosis, signaling, and angiogenesis. Cancer. 2005;104:1322–1331. doi: 10.1002/cncr.21300. [DOI] [PubMed] [Google Scholar]
- 80.Chen C, Johnston TD, Jeon H, Gedaly R, McHugh PP, Burke TG, et al. An in vitro study of liposomal curcumin: stability, toxicity and biological activity in human lymphocytes and Epstein-Barr virus-transformed human B-cells. Int J Pharm. 2009;366:133–139. doi: 10.1016/j.ijpharm.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 81.Wang D, Veena MS, Stevenson K, Tang C, Ho B, Suh JD, et al. Liposome-encapsulated curcumin suppresses growth of head and neck squamous cell carcinoma in vitro and in xenografts through the inhibition of nuclear factor kappaB by an AKT-independent pathway. Clin Cancer Res. 2008;14:6228–6236. doi: 10.1158/1078-0432.CCR-07-5177. [DOI] [PubMed] [Google Scholar]
- 82.Lee MH, Lin HY, Chen HC, Thomas JL. Ultrasound mediates the release of curcumin from microemulsions. Langmuir. 2008;24:1707–1713. doi: 10.1021/la7022874. [DOI] [PubMed] [Google Scholar]
- 83.Jung S, Otberg N, Thiede G, Richter H, Sterry W, Panzner S, et al. Innovative liposomes as a transfollicular drug delivery system: penetration into porcine hair follicles. J Invest Dermatol. 2006;126:1728–1732. doi: 10.1038/sj.jid.5700323. [DOI] [PubMed] [Google Scholar]
- 84.Wattanakrai P, Suwanachote S, Kulkollakarn S, Rajatanavin N. The study of human skin irritation of a novel herbal skin care product and ingredients by human single closed patch testing. J Med Assoc Thai. 2007;90:1116–1122. [PubMed] [Google Scholar]
- 85.Campbell RB, Ying B, Kuesters GM, Hemphill R. Fighting cancer: from the bench to bedside using second generation cationic liposomal therapeutics. J Pharm Sci. 2009;98:411–429. doi: 10.1002/jps.21458. [DOI] [PubMed] [Google Scholar]
- 86.Santos P, Watkinson AC, Hadgraft J, Lane ME. Application of microemulsions in dermal and transdermal drug delivery. Skin Pharmacol Physiol. 2008;21:246–259. doi: 10.1159/000140228. [DOI] [PubMed] [Google Scholar]
- 87.Teichmann A, Heuschkel S, Jacobi U, Presse G, Neubert RH, Sterry W, et al. Comparison of stratum corneum penetration and localization of a lipophilic model drug applied in an o/w microemulsion and an amphiphilic cream. Eur J Pharm Biopharm. 2007;67:699–706. doi: 10.1016/j.ejpb.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 88.Boriwanwattanarak P, Ingkaninan K, Khorana N, Viyoch J. Development of curcuminoids hydrogel patch using chitosan from various sources as controlled-release matrix. Int J Cosmet Sci. 2008;30:205–218. doi: 10.1111/j.1468-2494.2008.00437.x. [DOI] [PubMed] [Google Scholar]
- 89.Tiyaboonchai W, Tungpradit W, Plianbangchang P. Formulation and characterization of curcuminoids loaded solid lipid nanoparticles. Int J Pharm. 2007;337:299–306. doi: 10.1016/j.ijpharm.2006.12.043. [DOI] [PubMed] [Google Scholar]
- 90.Aziz HA, Peh KK, Tan YT. Solubility of core materials in aqueous polymeric solution effect on microencapsulation of curcumin. Drug Dev Ind Pharm. 2007;33:1263–1272. doi: 10.1080/03639040701483967. [DOI] [PubMed] [Google Scholar]
- 91.Shahani K, Swaminathan SK, Freeman D, Blum A, Ma L, Panyam J. Injectable sustained release microparticles of curcumin: a new concept for cancer chemoprevention. Cancer Res. 2010;70:4443–4452. doi: 10.1158/0008-5472.CAN-09-4362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Domb AJ, Israel ZH, Elmalak O, Teomim D, Bentolila A. Preparation and characterization of carmustine loaded polyanhydride wafers for treating brain tumors. Pharm Res. 1999;16:762–765. doi: 10.1023/a:1011995728760. [DOI] [PubMed] [Google Scholar]
- 93.Jain JP, Modi S, Domb AJ, Kumar N. Role of polyanhydrides as localized drug carriers. J Control Release. 2005;103:541–563. doi: 10.1016/j.jconrel.2004.12.021. [DOI] [PubMed] [Google Scholar]
- 94.Langer R. Drug delivery and targeting. Nature. 1998;392:5–10. [PubMed] [Google Scholar]
- 95.Dash AK, Cudworth GC., 2nd Therapeutic applications of implantable drug delivery systems. J Pharmacol Toxicol Methods. 1998;40:1–12. doi: 10.1016/s1056-8719(98)00027-6. [DOI] [PubMed] [Google Scholar]
- 96.Saltzman WM, Fung LK. Polymeric implants for cancer chemotherapy. Adv Drug Deliv Rev. 1997;26:209–230. doi: 10.1016/s0169-409x(97)00036-7. [DOI] [PubMed] [Google Scholar]
- 97.Weinberg BD, Blanco E, Gao J. Polymer implants for intratumoral drug delivery and cancer therapy. J Pharm Sci. 2008;97:1681–1702. doi: 10.1002/jps.21038. [DOI] [PubMed] [Google Scholar]
- 98.Gupta RC, Bansal SS, Aqil F, Cao P, Jeyabalan J, Russel GK, et al. A novel concept in delivering chemopreventive compounds. 100th Annual Meeting of American Association for Cancer Research; 2009 Apr 18–22; Denver, CO. Philadelphia. [Google Scholar]
- 99.Bansal SS, Jeyabalan J, Vadhanam MV, Gupta RC. Effect of Sustained, Low-Dose Curcumin on Benzo[a]Pyrene-Induced Tissue DNA Adducts in Rat Model. 99th Annual Meeting of American Association for Cancer Research; 2008 April 12–16; San Diego, California. [Google Scholar]
- 100.Teskac K, Kristl J. The evidence for solid lipid nanoparticles mediated cell uptake of resveratrol. Int J Pharm. 2010;390:61–69. doi: 10.1016/j.ijpharm.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 101.Wu TH, Yen FL, Lin LT, Tsai TR, Lin CC, Cham TM. Preparation, physicochemical characterization, and antioxidant effects of quercetin nanoparticles. Int J Pharm. 2008;346:160–168. doi: 10.1016/j.ijpharm.2007.06.036. [DOI] [PubMed] [Google Scholar]
- 102.Yuan ZP, Chen LJ, Fan LY, Tang MH, Yang GL, Yang HS, et al. Liposomal quercetin efficiently suppresses growth of solid tumors in murine models. Clin Cancer Res. 2006;12:3193–3199. doi: 10.1158/1078-0432.CCR-05-2365. [DOI] [PubMed] [Google Scholar]
- 103.Hentschel A, Gramdorf S, Muller RH, Kurz T. Beta-carotene-loaded nanostructured lipid carriers. J Food Sci. 2008;73:N1–N6. doi: 10.1111/j.1750-3841.2007.00641.x. [DOI] [PubMed] [Google Scholar]
- 104.Das S, Ng KY, Ho PC. Design of a pectin-based microparticle formulation using zinc ions as the cross-linking agent and glutaraldehyde as the hardening agent for colonic-specific delivery of resveratrol: In vitro and in vivo evaluations. J Drug Target. 2010 doi: 10.3109/1061186X.2010.504272. [DOI] [PubMed] [Google Scholar]