Abstract
Objective
Anorexia nervosa (AN) is a severe mental illness with high rates of relapse and rehospitalization. New treatment approaches are needed. We aimed to evaluate the potential utility of addressing eating-related fear in the treatment of AN using psychotherapy techniques known to be effective in the treatment of anxiety disorders and OCD, namely exposure therapy and response prevention.
Method
We developed a brief treatment intervention for AN (AN-EXRP) and evaluated its effects in an open series of 9 individuals with AN towards the end of acute weight restoration. We focused on eating behavior as the primary outcome, as it is related both to anxiety and to longer term course.
Results
Change in anxiety with AN-EXRP was associated with greater caloric intake.
Discussion
These findings support the anxiety-centered model of AN, and suggest the potential utility of further developing this treatment approach.
INTRODUCTION
Anorexia nervosa (AN) is an eating disorder with a chronic course and significant morbidity and mortality, affecting approximately 1% of women and one tenth as many men (1). The disorder is characterized by severe restriction of food intake resulting in an inappropriately low body weight, intense fear of weight gain, and self-evaluation closely linked to body shape and weight (2). Mortality rates among individuals with AN can be as high as 10%, with the likelihood of death increasing with longer duration of illness (3-5). Acute treatment consists of structured behaviorally-oriented programs to achieve normal weight (6); medications have not been found to be helpful (7). The rate of relapse following acute treatment is substantial, with as many as 30-50% of adult hospitalized patients requiring re-hospitalization within one year of discharge (8-9). AN is a difficult illness and decades of research have led to frustratingly few advances in treatment (10).
Along with maladaptive eating behavior, patients with AN manifest significant symptoms of anxiety. Patients with AN report high subjective anxiety with high scores on anxiety rating scales (11-12). In one recent case-control study, high levels of trait anxiety differentiated those who ultimately remitted from AN from those who did not (13). Anxiety may be a useful treatment target that has not been fully explored.
There are similarities between the clinical phenomena seen in AN and those described in anxiety disorders and OCD. These include fears related to food, avoidance related to these fears, and abnormal behaviors to manage these fears. More specifically, symptoms of AN include behaviors organized around an irrational belief (14-15): patients report anxiety in anticipation of a meal, concern about the contents of the food they eat, and fear of the effect of food on their shape and weight. Avoidance of sufficient caloric intake is a core disturbance of the illness. In addition, individuals with AN manifest a variety of abnormal behaviors around eating, many similar to symptoms of obsessive compulsive disorder (OCD). For example, some individuals need to consume foods in a particular order; some need to eat slowly so that only small amounts are consumed over time. Some eating behaviors are repetitive, stereotyped behaviors that are often used to decrease anxiety around eating. In short, patients manifest avoidance of feared stimuli, akin to specific phobias (16) and ritualized behaviors to reduce distress akin to OCD. AN also carries a high rate of comorbidity with anxiety disorders; up to 60% of individuals with AN have a lifetime diagnosis of an anxiety disorder (17-20). While there are important differences between AN and anxiety disorders, the shared clinical phenomena suggest that there may be useful overlap in treatment strategies. The link between anxiety and AN has long been noted (21-22), yet there have been limited efforts to address behavioral disturbances of AN utilizing methods of established efficacy in the treatment of anxiety disorders: exposure and response prevention techniques (23-24).
Noting the similarities between these features of AN and anxiety disorders and OCD, we have recently proposed a model of AN that emphasizes the role of anxiety in the perpetuation of illness and suggested that Exposure and Response Prevention treatment is a potentially useful approach to improving long term outcome in this difficult illness (25). Data showing that state anxiety prior to a meal is negatively associated with the amount of caloric intake in the meal provide preliminary support for this model (26).
As a next step in evaluating the validity of this model of AN, we developed a brief Exposure and Response Prevention intervention (AN-EXRP) for recently weight restored individuals with AN receiving inpatient, behaviorally-based treatment. This 12-session intervention emphasizes confronting fear and anxiety around eating-related situations. In this pilot study, our aim was to 1) further evaluate the importance of anxiety in eating behavior in AN; and 2) begin to evaluate the utility of this novel treatment approach. Given the severity of illness in AN, 12 sessions may be considered a modest dose of treatment and the clinical impact may be expected to be small. In this paper, we describe the treatment and present the results from a series of nine acutely weight-restored patients who received AN-EXRP.
METHODS
Subjects
Participants were individuals between the ages of 16 and 45 who met criteria for AN, with or without amenorrhea (27) at the time of hospital admission and had achieved near normal weight (body mass index (BMI) ≥19.5 kg/m2) during inpatient treatment. All patients were participating in the standard eating disorder treatment protocol at the New York State Psychiatric Institute (NYSPI). This treatment consists of a structured, behaviorally based program in which unit privileges are contingent on eating all meals and making regular weight gain (6). During the weight gain phase of treatment, patients are expected to gain 2.25 lbs per week. Treatment is provided by a multidisciplinary team and includes group and individual treatment. Exclusion criteria were other Axis I disorders requiring immediate clinical intervention (psychotic illness, bipolar illness, substance abuse), obsessive compulsive disorder, or acute suicidality. Stable antidepressant medication was allowed. All participants provided informed consent in accordance with the NYSPI Institutional Review Board
Study Intervention
Exposure and response prevention for AN (AN-EXRP)
AN-EXRP was adapted primarily from exposure and response prevention treatment of OCD (based on the manual of Kozak & Foa (28)) with additional influences from the treatment of social phobia(29). Treatment was gradually developed and manualized over the course of treatment with 17 individuals in an iterative process. Then, nine patients received this manualized intervention and their data are presented here.
The intervention consisted of 12 individual 90-minute sessions occurring Monday, Wednesday and Friday for 4 weeks. Study procedures were initiated immediately upon achieving minimally normal weight, defined by the inpatient treatment protocol as 90% ideal body weight (IBW) according to the 1959 Metropolitan Life Tables (30) and corresponding to a BMI of approximately 19.5 kg/m2. The experimental intervention was delivered as an adjunct to the standard weight maintenance treatment on the inpatient unit.
In Session 1, the therapist elicited a description of the patients feared eating situations (including feared foods), avoidance behaviors, and ritualized behaviors. The therapist provided psychoeducation regarding the rationale for exposure based treatment, including education about anxiety. A Subjective Units of Distress scale, a widely used metric for subjective report of anxiety (31), was created using non-eating disordered related fears as a frame of reference. This scale was then used to formulate a detailed hierarchy of feared eating situations on a scale of 1-100.
The remaining 11 sessions each included an exposure to a feared eating situation, beginning with content low on the patient’s individualized hierarchy and progressively moving up the hierarchy over time. Sessions began with collaborative engagement of the patient in the session (e.g. review of the rationale for the treatment, review of the patient’s between session work) and moved as quickly as possible into the act of eating. Each session concluded with a de-briefing in which a “take-home message” was identified and between session assignments were created. The aim of each session was to engage the patient in experiencing, not avoiding, the anxiety and fear raised by the exposure content and then experiencing the habituation of anxiety and the disconfirmation of feared consequences. Interventions included enhancing the patient’s awareness of the physical symptoms of anxiety (nausea, sensations of fullness, feeling warm, tense, etc.), articulation of the feared consequences (fear of chaos, loss of control, immediate obesity), and recognition that the feared outcome did not occur. Subjective ratings of anxiety were obtained at regular intervals throughout the session. Each session included exposure to anticipation of eating, ingesting food, and exposure to having eaten.
Assessments
Eating behavior and anxiety were assessed before and after study treatment, as described below. Analyses focused on post-treatment eating behavior. Change in eating behavior was considered, however caloric prescriptions and intake requirements decrease over the course of this phase of treatment making it difficult to interpret in an open series.
Laboratory eating assessment
The laboratory eating assessment offers an objective measurement of intake in an observed setting. On the morning of the test meal, participants received a standardized breakfast (yogurt, fruit, and juice; ~300kcal) at 8 am and had nothing to eat or drink between breakfast and the test meal at noon. For the test meal, they were brought to the Biological Studies Unit (BSU) where they participated in a lunch meal Behavior Avoidance Task, modeled after social phobia assessments (32-33). After 3 minutes of acclimating to the room, they were provided with a tray consisting of a large sandwich (600 kcal, i.e. a foot long sub with turkey, turkey and cheese, or grilled chicken), a large bowl of potato chips (455 kcal), and a small bottle of water (8 oz).
Participants were instructed to imagine that they were on a trip, had ordered a sandwich from room service, knew that they would not be able to eat again for several hours and wanted to have a sufficient lunch. They pressed a bell on the table to indicate when they were finished eating. Anxiety was measured prior to and every three minutes during the meal as Subjective Units of Distress, on a 0-10 scale. Intake was calculated by measuring the weight of the food (Acculab 7200 balance, readability 0.1 g) before and after the meal and calculating calories consumed based on kcal/gram weight of the foods.
Food Records
Self-report food records were collected to measure and individuals average eating patterns. Participants completed detailed food records prospectively for 4 days, including 3 weekdays and one weekend day. Verbal and written instructions were provided for estimation of food portions, and food records were checked for accuracy, following the protocol of Schebendach et al. (34). Records were analyzed using NUTRITIONIST PRO Software (version 1.2.207, 2003, First DataBank, Inc., San Bruno, CA). Nutrient analysis included calories (kcal) and fat (g). These data were used to calculate average daily intake (kcal) and percent fat. In addition, diet energy density (DEDS) and diet variety (DVS) scores were calculated following the procedures described by Schebendach et al (34).
Anxiety
There were three measures of eating-related anxiety, each addressing a different aspect: 1) pre-meal anxiety was measured using the Spielberger State Anxiety Inventory (STAI-S), administered prior to entering the room for the laboratory test meal; 2) anxiety during the meal was measured as the mean of the Subjective Units of Distress (SUDS) reported every 3 minutes during the meal; 3) a Food Fear and Avoidance Hierarchy score (FAH) was calculated for each individual, as follows. At baseline, a semi-structured interview was conducted based on the Fear and Avoidance Hierarchy protocol that is a standard component of exposure therapy. Participants were asked to complete levels on a 0-100 scale, divided as 10 separate levels, to rate food-related distress. Several standard items were rated (macaroni and cheese, yogurt, potato chips, turkey and cheese on whole wheat, and mayonnaise) and patients rated their own individually-selected items to complete the 10 levels of the rating scale. After completion of the study treatment, and without seeing their original ratings, patients re-rated the standardized items and any items that had been included in the treatment sessions, for a total of 9-15 items. The FAH score was calculated as the average of the difference between the ratings at Time 2 – Time 1. For example, an individual might have reported, prior to study intervention, that eating “pasta with red sauce” was associated with a SUDS level of 90. If this item was included in at least one study session, then she would be asked to re-rate this after treatment, and she might report it as a SUDS level of 70. Her score for that item is −20. Her FAH score is the mean of her item scores. In addition, participants completed a Beck Anxiety Inventory (BAI) at baseline and termination.
Quality Assurance
Therapists participated in a weekly supervision with the study PI (JS) and a senior clinician with expertise conducting and supervising exposure therapy for anxiety disorders (AMA). Through didactic training and weekly review of treatment, including supervision of videotaped material, competence in provision of AN-EXRP was determined.
Statistical Analysis
Means and standard deviations were calculated for demographic characteristics. Pre-treatment and post-treatment means and standard deviations were calculated for STAI-S, mean SUDS, BAI, food records (average daily intake, percent of calories from fat, and diet variety and diet energy density), and test meal intake. FAH was calculated as described above. Associations between post-intervention intake and change in eating related anxiety (STAIS, SUDS, FAH) were examined using Pearson’s correlation coefficient. All statistical analyses were carried out using SPSS for Windows, version 17.0, and means are reported plus or minus standard deviations.
RESULTS
Demographics
Nine women with AN were enrolled and completed the protocol, 6 women were binge-purge subtype, 3 were restricting subtype. Mean age was 28.1 years (ranging from 17-38 years). Three participants met full DSM-IV criteria for AN; two were menstruating with oral contraceptives, two others menstruated irregularly, and two menstruated regularly. Patients had been ill, on average 11.3 years (range 3-19 years) with 2.8 hospitalizations (range 1-9). The average BMI on admission was 16.1 ± 1.9 kg/m2. Two patients had current diagnoses of Anxiety Disorder NOS, and 1 had a diagnosis of specific phobia, situational. Lifetime diagnoses included 2 patients with past major depressive disorder, 1 with past post-traumatic stress disorder, and 3 with past alcohol abuse or dependence. Three of the nine participants had no co-morbid diagnoses.
Caloric Intake
Pre-AN-EXRP, mean caloric intake (including nutritional supplements) calculated from 4 day food records was 3,251 ± 551 kcal/day. The pre-treatment records generally included a higher caloric prescription, as well as prescribed nutritional supplements (Ensure), which had been discontinued by the time of the post-intervention food records. Post-treatment, mean caloric intake was 2,568 ± 425 kcal/day (data were missing for one participant at Time 1 and two participants at Time 2). In the laboratory test meal, mean intake prior to AN-EXRP was 429 ± 169 kcal. After AN-EXRP mean intake was 434 ± 242 kcal (n=8, one participant completed all sessions and food records but did not complete a post-treatment test meal).
Anxiety
Pre-meal anxiety, as measured by STAI-S prior to entering the test meal room, decreased from 58.4 ± 6.4 before AN-EXRP to 52.3 ± 10.2 after AN-EXRP (Cohen’s d = 0.72). Subjective ratings of anxiety during the laboratory meal decreased from a mean of 65.4 ± 30.5 to 53.8 ± 25.4 (Cohen’s d = 0.99). BAI changed from 14.2 ± 3.4 to 12.5 ± 9.4 (Cohen’s d = 0.37). These changes were not statistically significant. FAH ratings decreased overall, with a mean of −11.5 ± 8.2.
Correlations
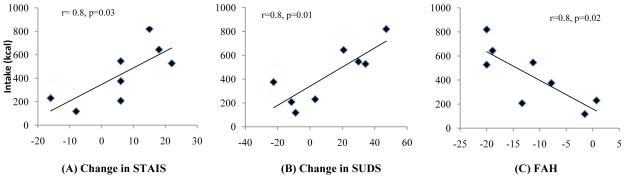
Caloric intake in the laboratory meal after AN-EXRP treatment was significantly associated with change in STAIS (r=0.751, p = 0.03), change in mean SUDS (r= 0.83, p = 0.01), and Food-FAH (r= 0.8, p= 0.02). See Figure 1. There were no significant associations between pre-treatment anxiety (mean SUDS or STAIS) and laboratory intake or between post-treatment (mean SUDS or STAIS) anxiety and laboratory intake.
Figure 1. Intake and change in anxiety.
Caloric intake in the post-AN-EXRP laboratory meal was significantly associated with change in anxiety. Decrease in (A) pre-meal Spielberger State Anxiety Inventory (STAIS), (B) mean Subjective Units of Distress SUDS) during the test meal, (C) Food Fear and Anxiety Hierarchy (FAH) were each significantly associated with increased intake in the post-treatment meal.
DISCUSSION
In this pilot study, change in anxiety over the course of AN-EXRP was significantly associated with intake in the post-treatment laboratory meal. There was no significant change in intake with this modest dose of treatment. The presence of a robust association between change in anxiety and caloric intake provides a measure of support for the proposed model of the persistence of AN and the importance of eating related anxiety as a treatment target. The findings suggest that decreasing pre-meal anxiety may improve eating behavior.
Few previous studies have evaluated exposure and response prevention techniques in AN. One case study describes the successful use of food exposure and response prevention in the weight gain treatment of an individual with AN (35). In a preliminary study of the use of exposure (without response prevention) we found that repeated exposure to feared eating situation can increase intake in the laboratory setting (36). In the treatment of bulimia nervosa (BN), exposure and response prevention in combination with standard cognitive behavior therapy has been studied, with some studies showing promising results (37-39). No psychotherapy or medication has emerged as the treatment of choice for preventing relapse among weight restored patients with AN (9, 40-41). Anti-anxiety medications such as SSRIs, which have proven generally useful for anxiety disorders, have been disappointing in the treatment of AN.(12, 40) Interestingly, some data suggest that exposure and response prevention is more effective than medication in reducing relapse among patients with OCD (42). These findings, together with the results from this open series, support the need for further development and testing of AN-EXRP.
In this study, over the course of AN-EXRP, mean meal related anxiety decreased across three measures of anxiety (STAI-S, SUDS, and FAH). Though these changes were not statistically significant in this very small sample size, and the individual results were variable, the effect sizes were medium to large for STAI-S and SUDS (Cohen’s d =0.72 and 0.99). This suggests that AN-EXRP may have benefit in the proximal goal of reducing pre-meal anxiety. This is particularly important, as pre-meal anxiety has been shown to be associated with food intake (26). Factors contributing to treatment response will be important to evaluate in future study, as some individuals did not manifest a change in eating-related anxiety. Notably, there was only minimal change in the BAI with AN-EXRP (Cohen’s d = 0.37), suggesting that the STAI-S may be better measure of this phenomenon. There are limitations of this study, of course, as the AN-EXRP was delivered while patients were receiving active structured treatment therefore we cannot conclude that exposure was the agent of change. Controlled trials will be needed to further evaluate this.
The goal of AN-EXRP is to improve eating behavior, specifically to encourage increased diet variety and increased intake of high-fat or energy dense foods. The absence of change in intake in this study is potentially discouraging. However, several factors may have contributed to this, including small sample size and the timing of the intervention. In this pilot open series, we were unable to fully examine the impact of AN-EXRP in changing eating behavior because the measurement of absolute change in intake before and after treatment was confounded by changes that occur over that timeframe of treatment. That is, patients entered the study immediately upon achieving their target weight. Over the next 4 weeks, treatment focused on determining the appropriate caloric prescription for weight maintenance, which often entailed a decrease in daily calories. In addition, over these 4 weeks patients’ privileges were increased to include more meals off the unit. This change commonly leads to increasing restrictive practices by patients, evidenced as a decline in caloric intake, high fat foods, and variety over time. Pattern of dietary intake even prior to hospital discharge has been shown to be associated with relapse in the year following weight restoration. Schebendach et al (34) collected 4 day food records from acutely weight restored inpatients and found that diet energy density and diet variety prior to hospital discharge predicted relapse at one year post-hospitalization. This finding suggests that eating behavior at the time of weight restoration is an important treatment target in improving the long term course of AN. If AN-EXRP is successful, it will support patients in making healthier choices and prevent this decline in healthy eating behavior.
AN is a severe illness and treatment research has been disappointing. New approaches to treatment are clearly needed. We have developed a model for the perpetuation of AN that proposes that fear and anxiety are integral to the persistence of detrimental eating habits. AN-EXRP is a novel approach that builds from the utility of CBT in eating disorders and creates a new direction for AN that relies on in-session exposure and intensive between-session confrontation of eating-related anxiety with an additional emphasis on response prevention. Participants in this study overall agreed with the potential utility of the approach at the outset, were engaged in the treatment, and described finding it useful. In formal ratings of treatment expectations, mean treatment appropriateness (on a 10 point Likert scale) was 6.1 ± 3.0, with 78% of patients reporting a score of “moderately appropriate” or above, and mean likelihood of treatment success was 5.2 ± 2.1, with 67% reporting a score of “moderately likely” or above.
This preliminary study suggests that targeting eating-related anxiety is important in improving intake in patients with AN, as reducing eating related anxiety was associated with increased intake after receiving the treatment intervention. Further study is needed to fully evaluate the utility of AN-EXRP in accomplishing this goal, including a randomized trial to compare AN-EXRP with an alternative treatment. Future research would also include development of this limited intervention to create a more extensive treatment that could significantly impact long-term outcome.
Acknowledgements
The authors would like to acknowledge the contributions of Deborah Glasofer, Ph.D., and Sarah Parker, Ph.D. as the study therapists, as well as the Eating Disorders Research Unit staff, and the patients who participated in this study. The authors wish to acknowledge Tim Walsh, MD for his expert guidance in this project.
This work was supported by the National Institute of Mental Health grants K23MH076195-02 and R01MH08273602
Footnotes
Disclosures:
Dr. Steinglass has received support from NARSAD and the Klarman Family Foundation.
Dr. Albano received royalties from Oxford University Press and The Guilford Press.
Dr. Simpson has received medication at no cost from Janssen Pharmaceuticals for an NIMH funded trial.
Dr. Schebendach has no financial disclosures to report.
Dr. Attia has received medication at no cost from Eli Lilly & Co for an NIMH-funded trial.
References
- 1.Hudson JI, Hiripi E, Pope HG, Jr., Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association AP . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association Press; Washington, D.C.: 2000. Text Revision. [Google Scholar]
- 3.Crisp AH, Callender JS, Halek C, Hsu LK. Long-term mortality in anorexia nervosa. A 20-year follow-up of the St George’s and Aberdeen cohorts. Br J Psychiatry. 1992;161:104–7. doi: 10.1192/bjp.161.1.104. [DOI] [PubMed] [Google Scholar]
- 4.Moller-Madsen S, Nystrup J, Nielsen S. Mortality in anorexia nervosa in Denmark during the period 1970-1987. Acta Psychiatr Scand. 1996;94(6):454–9. doi: 10.1111/j.1600-0447.1996.tb09890.x. [DOI] [PubMed] [Google Scholar]
- 5.Patton GC. Mortality in eating disorders. Psychol Med. 1988;18(4):947–51. doi: 10.1017/s0033291700009879. [DOI] [PubMed] [Google Scholar]
- 6.Attia E, Walsh BT. Behavioral management for anorexia nervosa. N Engl J Med. 2009;360(5):500–6. doi: 10.1056/NEJMct0805569. [DOI] [PubMed] [Google Scholar]
- 7.Crow SJ, Mitchell JE, Roerig JD, Steffen K. What potential role is there for medication treatment in anorexia nervosa? Int J Eat Disord. 2009;42(1):1–8. doi: 10.1002/eat.20576. [DOI] [PubMed] [Google Scholar]
- 8.Eckert E, Halmi KA, Marchi P, Grove W, Crosby R. Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychological Medicine. 1995;25:143–56. doi: 10.1017/s0033291700028166. [DOI] [PubMed] [Google Scholar]
- 9.Pike KM, Walsh BT, Vitousek K, Wilson GT, Bauer J. Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. Am J Psychiatry. 2003;160(11):2046–9. doi: 10.1176/appi.ajp.160.11.2046. [DOI] [PubMed] [Google Scholar]
- 10.Steinhausen HC. The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry. 2002;159(8):1284–93. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- 11.Pollice C, Kaye WH, Greeno CG, Weltzin TE. Relationship of depression, anxiety, and obsessionality to state of illness in anorexia nervosa. Int J Eat Disord. 1997;21(4):367–76. doi: 10.1002/(sici)1098-108x(1997)21:4<367::aid-eat10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 12.Attia E, Haiman C, Walsh BT, Flater SR. Does fluoxetine augment the inpatient treatment of anorexia nervosa? Am J Psychiatry. 1998;155(4):548–51. doi: 10.1176/ajp.155.4.548. [DOI] [PubMed] [Google Scholar]
- 13.Yackobovitch-Gavan M, Golan M, Valevski A, Kreitler S, Bachar E, Lieblich A, et al. An integrative quantitative model of factors influencing the course of anorexia nervosa over time. Int J Eat Disord. 2009;42(4):306–17. doi: 10.1002/eat.20624. [DOI] [PubMed] [Google Scholar]
- 14.Sunday SR, Halmi KA, Einhorn A. The Yale-Brown-Cornell Eating Disorder Scale: a new scale to assess eating disorder symptomatology. Int J Eat Disord. 1995;18(3):237–45. doi: 10.1002/1098-108x(199511)18:3<237::aid-eat2260180305>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. Guilford Press; New York: 2008. [Google Scholar]
- 16.Barlow DH, Durand VM. Abnormal Psychology: An Integrative Approach. 4th Ed. Thompson-Wadsworth; Belmont, CA: 2005. [Google Scholar]
- 17.Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161(12):2215–21. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- 18.Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand. 1997;96(2):101–7. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- 19.Raney TJ, Thornton LM, Berrettini W, Brandt H, Crawford S, Fichter MM, et al. Influence of overanxious disorder of childhood on the expression of anorexia nervosa. Int J Eat Disord. 2008;41(4):326–32. doi: 10.1002/eat.20508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halmi KA, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J. Comorbidity of psychiatric diagnoses in anorexia nervosa. Archives of General Psychiatry. 1991;48:712–8. doi: 10.1001/archpsyc.1991.01810320036006. [DOI] [PubMed] [Google Scholar]
- 21.Crisp AH, Bhat AV. ‘Personality’ and anorexia nervosa - the phobic avoidance stance. Its origins and its symptomatology. Psychother Psychosom. 1982;38(1):178–200. doi: 10.1159/000287626. [DOI] [PubMed] [Google Scholar]
- 22.Hsu GLK, Kaye W, Weltzin T. Are the eating disorders related to Obsessive Compulsive Disorder? International Journal of Eating Disorders. 1993;14(3):305–18. doi: 10.1002/1098-108x(199311)14:3<305::aid-eat2260140309>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 23.Goldfarb LA, Fuhr R, Tsujimoto RN, Fischman SE. Systematic desensitization and relaxation as adjuncts in the treatment of anorexia nervosa: a preliminary study. Psychol Rep. 1987;60(2):511–8. doi: 10.2466/pr0.1987.60.2.511. [DOI] [PubMed] [Google Scholar]
- 24.Hallsten EA., Jr. Adolescent anorexia nervosa treated by desensitization. Behav Res Ther. 1965;3(2):87–91. doi: 10.1016/0005-7967(65)90011-2. [DOI] [PubMed] [Google Scholar]
- 25.Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of Exposure and Response Prevention to the treatment of anorexia nervosa. Int J Eat Disord. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steinglass JE, Sysko R, Mayer L, Berner LA, Schebendach J, Wang Y, et al. Pre-meal anxiety and food intake in anorexia nervosa. Appetite. doi: 10.1016/j.appet.2010.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord. 2009;42(7):581–9. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- 28.Kozak MJ, Foa EB. Mastery of Obsessive-Compulsive Disorder. Oxford University Press; New York: 1997. [Google Scholar]
- 29.Albano A, DiBartolo PM. Cognitive-Behavioral Therapy for Social Phobia in Adolescents: Stand Up, Speak Out. Oxford University Press; New York: 2007. [Google Scholar]
- 30.MetropolitanLifeInsurance New weight standards for men and women. Statistical Bulletin. 1959;(40):1–4. [Google Scholar]
- 31.Wolpe J, Lazarus AA. Behavior therapy techniques. Pergamon; New York: 1966. [Google Scholar]
- 32.Becker RE, Heimberg RG. Assessment of social skills. In: Hersen M, Bellack AS, editors. Handbook of behavioral assessment. Pergamon Press; New York: 1988. pp. 365–95. [Google Scholar]
- 33.Beidel DC, Turner SM, Jacob RG, Cooley MR. Assessment of social phobia: Reliability of an impromptu speech task. Journal of Anxiety Disorders. 1989;3:149–58. [Google Scholar]
- 34.Schebendach JE, Mayer LE, Devlin MJ, Attia E, Contento IR, Wolf RL, Walsh BT. Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. Am J Clin Nutr. 2008;87(4):810–6. doi: 10.1093/ajcn/87.4.810. [DOI] [PubMed] [Google Scholar]
- 35.Boutelle KN. The use of exposure with response prevention in a male anorexic. J Behav Ther Exp Psychiatry. 1998;29(1):79–84. doi: 10.1016/s0005-7916(97)00041-4. [DOI] [PubMed] [Google Scholar]
- 36.Steinglass J, Sysko R, Schebendach J, Broft A, Strober M, Walsh BT. The application of exposure therapy and D-cycloserine to the treatment of anorexia nervosa: a preliminary trial. J Psychiatr Pract. 2007;13(4):238–45. doi: 10.1097/01.pra.0000281484.89075.a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leitenberg H, Rosen JC, Gross J, Nudelman S, Vara LS. Exposure plus response-prevention treatment of bulimia nervosa. J Consult Clin Psychol. 1988;56(4):535–41. doi: 10.1037//0022-006x.56.4.535. [DOI] [PubMed] [Google Scholar]
- 38.Wilson GT, Rossiter E, Kleifield EI, Lindholm L. Cognitive-behavioral treatment of bulimia nervosa: a controlled evaluation. Behav Res Ther. 1986;24(3):277–88. doi: 10.1016/0005-7967(86)90187-7. [DOI] [PubMed] [Google Scholar]
- 39.Bulik CM, Sullivan PF, Carter FA, McIntosh VV, Joyce PR. The role of exposure with response prevention in the cognitive-behavioural therapy for bulimia nervosa. Psychol Med. 1998;28(3):611–23. doi: 10.1017/s0033291798006618. [DOI] [PubMed] [Google Scholar]
- 40.Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, et al. Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA. 2006;295(22):2605–12. doi: 10.1001/jama.295.22.2605. [DOI] [PubMed] [Google Scholar]
- 41.Association AP Treatment of patients with eating disorders, 3rd edition. American Journal of Psychiatry. 2006;163(7 Supplement):4–54. [PubMed] [Google Scholar]
- 42.Simpson HB, Liebowitz MR, Foa EB, Kozak MJ, Schmidt AB, Rowan V, et al. Post-treatment effects of exposure therapy and clomipramine in obsessive-compulsive disorder. Depress Anxiety. 2004;19(4):225–33. doi: 10.1002/da.20003. [DOI] [PubMed] [Google Scholar]