Abstract
The study tests the hypothesis that in patients admitted with acutely decompensated heart failure (ADHF), achievement of adequate body hydration status with intensive medical therapy, modulated by combined bioelectrical vectorial impedance analysis (BIVA) and B-type natriuretic peptide (BNP) measurement, may contribute to optimize the timing of patient’s discharge and to improve clinical outcomes. Three hundred patients admitted for ADHF underwent serial BIVA and BNP measurement. Therapy was titrated to reach a BNP value of <250 pg/ml, whenever possible. Patients were categorized as early responders (rapid BNP fall below 250 pg/ml); late responders (slow BNP fall below 250 pg/ml, after aggressive therapy); and non-responders (BNP persistently >250 pg/ml). Worsening of renal function (WRF) was evaluated during hospitalization. Death and rehospitalization were monitored with a 6-month follow-up. BNP value on discharge of ≤250 pg/ml led to a 25% event rate within 6 months (Group A: 17.4%; Group B: 21%, Chi2; n.s.), whereas a value >250 pg/ml (Group C) was associated with a far higher percentage (37%). At discharge, body hydration was 73.8 ± 3.2% in the total population and 73.2 ± 2.1, 73.5 ± 2.8, 74.1 ± 3.6% in the three groups, respectively. WRF was observed in 22.3% of the total. WRF occurred in 22% in Group A, 32% in Group B, and 20% in Group C (P = n.s.). Our study confirms the hypothesis that combined BNP/BIVA sequential measurements help to achieve adequate fluid balance status in patients with ADHF and can be used to drive a “tailored therapy,” allowing clinicians to identify high-risk patients and possibly to reduce the incidence of complications secondary to fluid management strategies.
Keywords: Acute kidney injury, Diuretics, Heart failure, Natriuretic peptides, Water-electrolyte balance
Introduction
Acute decompensated heart failure (ADHF) is characterized by a combination of clinical, hemodynamic, and neurohormonal abnormalities [1]. Patient-oriented management aiming at minimizing morbidity, hospitalizations, and mortality is a challenging but important target [2]. Patients at risk of events after hospitalization are often difficult to identify [3]; moreover, in spite of technological advances and the search for objective, evidence-based criteria, discharging a patient hospitalized for ADHF, is still largely based on subjective feelings of the treating physician [4]. Recently, natriuretic peptide (NP) levels have emerged as robust prognostic indicators in ADHF [5, 6]. NP levels obtained at the time of hospital discharge predict clinical outcomes following hospitalization for ADHF [6–8].
NP levels rapidly decrease after short-term therapeutic strategies [9], and decreased levels correlate with a reduction in fluid overload and improvement of hydration status [10, 11]. Nevertheless, targeting a specific reduction in body weight is often difficult because of the complexity of determining accurate body fluid status [12]. Furthermore, levels of BNP can remain high even after achieving an adequate hydration status because of a stretched myocardium (i.e., dry BNP), renal failure, liver failure, pulmonary embolus, and acute coronary syndromes [6, 10].
Recently, bio-impedance vector analysis (BIVA) has been suggested as a tool to assist in volume status assessment in patients with heart failure. BIVA allows a rapid, accurate, and non-invasive determination of body hydration status, correlates with NYHA class, and seems to demonstrate high diagnostic accuracy for the differential diagnosis of HF-induced dyspnea [14]. Moreover, type 1 cardiorenal syndrome (CRS) may often complicate the course of ADHF where the use of loop diuretics typically reduces congestion at the cost of renal hypoperfusion and worsening of renal function (WRF) [15, 16]. Thus, by providing an accurate index of total body fluid, BIVA may be used to guide fluid-related therapies [10, 11, 13].
The technologies of BIVA and BNP may be applied in combination and when used together may provide greater accuracy for volume assessment in heart failure. In fact, one study found that this combination provided better diagnostic accuracy than either used alone [14]. Furthermore, we previously reported that BNP-guided treatment and body hydration status monitoring helped to optimize the patient’s discharge volume status as well as predict the occurrence of cardiovascular events [17]. Thus, by using both technologies simultaneously, BIVA and BNP may represent a useful tool, providing accurate insights into body volume status, and may be an aid to drive therapeutic interventions in these patients. The hypothesis of this present study is that in patients hospitalized with ADHF, effective reduction in congestion with intensive medical therapy guided by BIVA and BNP measurements may contribute achieving optimal hydration status and therefore help optimize discharge timing and decrease long-term complications. A second end point was also prespecified to determine whether optimization of dry weight by BIVA contributes to reduction in the development of WRF.
Methods
Population
Subjects (age ≥18 years) admitted to the heart failure unit (HFU) of two large community hospitals with a primary diagnosis of ADHF were consecutively enrolled over a period of 24 months. Eligibility criteria included the following: (1) symptoms of HF [18]; (2) NYHA functional classes III or IV, with an acute exacerbation of symptoms of at least 1 class (ADHF); (3) evidence of systolic and/or diastolic dysfunction by echocardiography; (4) BNP ≥250 pg/ml, in the absence of end-stage renal failure or acute coronary syndromes. The value of 250 pg/ml was selected to increase specificity [17, 19]. Institutional review boards of participating centers approved this project. Informed consent was obtained for hospitalization and treatment and was documented in the medical records. Data were collected per medical chart review.
Clinical monitoring and medical therapy during hospitalization
All patients were treated at the direction of the treating physician per international ADHF guidelines [20]. BNP, serum creatinine, and blood urea nitrogen values were recorded on admission and at least every other day throughout hospitalization, including the day of discharge. BIVA measurement was taken at admission, on the day of restoration of clinical stability, and at discharge. Restoration of clinical stability was defined by 6 criteria [17], including the following: (a) subjective improvement on the basis of NYHA class (improvement of orthopnoea in refractory NYHA class IV); (b) systolic blood pressure between 90 and 120 mmHg; (c) heart rate <100 bpm; (d) pulse oxymetry in ambient air >90%; (e) diuresis >1,000 ml/24 h; (f) improvement in fluid overload (migration trend of the BIVA value toward normal in the relevant nomogram).
A BNP value <250 pg/ml was used as a further criterion to document the achieved “clinical stability” and to drive discharge, per our previously published protocol [17]. Patients with a BNP value >250 pg/ml were given one or more of the following measures: (a) “prolonged” i.v diuretic treatment (up to 500 mg/day of furosemide) unless a status of dehydration was documented by BIVA or serum creatinine increased >0.3 mg/dl was observed; (b) scaling up of the ACE inhibitor dose (up to enalapril equivalent of 20 mg/12 h); (c) strict blood pressure monitoring (target systolic value <100 mmHg); and heart rate control (<80 bpm); d) oral/i.v. vasodilators.
Responses to treatment classification
For the analysis, patients were stratified into three groups based on BNP changes in response to therapy. These included early-, late-, and persistent categories.
Early responders: This group consisted of patients with initially high BNP levels that tended to drop rapidly after early pharmacological management and represents patients who often could be discharged early with a low rate of complications in the follow-up period [17].
Late responders: This cohort represents patients with limited initial response to medical therapy but, who subsequently, after a more aggressive treatment, demonstrated a late reduction in BNP and decreased in congestion. These patients can be discharged later with a slightly higher long-term complication rate as compared with the early responders [17].
Non-responders: These subsets are those patients who never achieve a significant reduction in BNP level despite aggressive therapy. Although having nearly normal fluid status, these patients have high BNP levels (Dry BNP) and display a very narrow window of adequate hydration, easily falling into conditions of hyper- or hypovolemia. These patients have a significantly worse prognosis than either early- or late responder groups [17].
Cardiorenal interactions and kidney function measurement
We defined WRF as an increase in serum creatinine of ≥0.3 mg/dl during hospitalization, consistent with several previous investigations [21–23] and the most recent classification of acute kidney injury [24, 25]. Estimated glomerular filtration rate (eGFR) was calculated using the simplified modification of diet in renal disease equation [26].
BNP assay
Whole blood samples were immediately analyzed by the immunofluorescent BNP Triage point of care (Alere, San Diego, CA, USA) platform. The method requires a minimum sample volume of 250 μl and has a detection limit of 10 pg/ml.
Doppler echocardiography
Echocardiography examinations were carried out on admission, blinded to the BNP value. Left ventricular systolic dysfunction was defined as an ejection fraction (EF) <50%. The left ventricular EF was measured using Simpson’s biplane method. Diastolic function was defined per classifications used in prior studies [17, 27].
Bioelectrical impedance vectorial analysis
Assessment of body fluid status was made with an electrical impedance analyser and Cardio EFG software (Akern, Pontassieve, Florence, Italy). The bioelectrical parameters of resistance, reactance, and phase angle were determined using an electric alternating current flux of 800 microA and an operating frequency of 50 kHz. Whole-body impedance measurements were taken by using a standard position of outer and inner electrodes on the right hand and foot. The entire procedure was performed per the National Institutes of Health technology assessment conference statements [28]. For each patient, a database was created including anthropometric data (height, weight, and body mass index). Bioelectrical impedance vector analysis simultaneously evaluates total body by resistance and reactance (reactance is a form of opposition that electronic components exhibit to the passage of alternating current because of capacitance or inductance; in some respects, reactance is like an alternating current counterpart of direct current and indicates an absolute amount of body cell mass), presenting them graphically to provide indices of total body hydration status. BIVA can also provide data regarding the ratio of extracellular water and total body water.
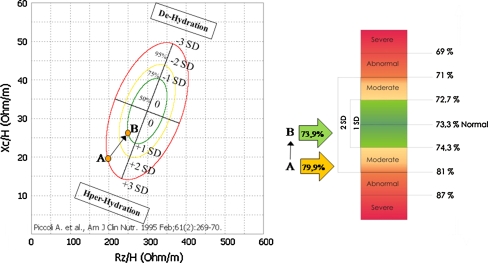
BIVA data can be visually presented as a nomogram classifying patients into 3 classes as follows: normally hydrated, hyperhydrated, or dehydrated. The latter classes can be further subdivided into mild, moderate, or severe volume abnormalities [29, 30]. Using BIVA [31] (Fig. 1), a forward or backward displacement of vectors parallel to the major axis of the standard deviation ellipses is associated with dehydration or fluid overloading, respectively, reaching extremes out of the poles (left panel Fig. 1). Vectors above or below the minor axis (meaning upper-left or lower-right half of ellipses) are associated with more or less cell mass in soft tissues, respectively, with extremes along the minor axis. The need of a numerical value has led to the construction of a numerical scale (right panel in Fig. 1) in which the normal level of hydration is set at 73.3%. Values above or below represent, respectively, dehydration or overhydration and are correlated with specific points in the BIVA nomogram. The migration of the vector in the nomogram results in variations of the numerical value of the hydration status (example A to B in Fig. 1).
Fig. 1.
Graphic representation of the nomogram (left panel) and the numerical scale (right panel) for BIVA. A typical example of vector migration (A to B) in response to aggressive fluid depletion therapy is reported. Corresponding values are reported in the numerical scale. Impedance (Z vector) is a combination of Resistance (R) and Reactance (Xc) across ionic solutions of soft tissues, tissue interfaces and cell membranes. Impedance at 50 kHz is represented with a complex number (a point) in the real-imaginary plane (Z vector), that is a combination of R (i.e. the opposition to flow of an alternating current through intra- and extra cellular ionic solutions, representing the real part of Z) and Xc (i.e. the capacitative component of tissue interfaces, and cell membranes and organelles, representing the imaginary part of Z). The volume of intra and extra cellular ionic solutions is (inversely) related to the R component of Z. The amount of soft tissue structures containing the solutions is (directly) related to the Xc component of Z. The arc tangent (Xc/R) is called the phase angle (Xc on the ordinate and R on the abscissa axis)
Follow-up
Before discharge, all patients underwent medical and nurse visit for evaluation and comprehensive education of the patient and family. Eligible patients were then discharged with guideline compliant pharmacologic therapy, a thorough prescription of diet and behavioral recommendations at home. Clinic visits were scheduled at 2, 6, 12, 24, and 36 weeks.
Clinical end points
Primary clinical end points were death and/or hospital readmissions for ADHF during the 6 months after discharge. Other end points included discharge hydration status (with measures of BIVA and BNP), determination of “dry” BNP levels, and if AKI occurred at any time during hospitalization.
Statistical analysis
Categorical data are presented as numbers (percent) and continuous data as means ± standard deviation. Alpha was defined as P < 0.05 was considered significant. Mann–Whitney U-test and Wilcoxon test were used for comparisons between samples, while associations between variables were verified by Fisher’s exact test. One-way ANOVA was also used. Cox proportional hazards regression models were used to examine the relation of clinical variables, BNP levels, and echocardiographics parameters with the incidence of the combined end point during the 6 months after discharge. A ROC (receiver-operated curve) analysis was performed to show various cutoff values for BNP and to identify patients likely to suffer an event in the 6 months after discharge. BNP levels were evaluated both as a continuous variable and as a categorical variables (based on cutoff values). To evaluate clinical events in relation to BNP levels, Kaplan–Meier curves are presented. Analyses were performed using SPSS software per Windows, release 11.0, SPSS Inc., Chicago, USA).
Results
Patient parameters
Three hundred patients were enrolled in the study over 24 months. Table 1 summarizes their characteristics and the evolution of several parameters throughout hospitalization and follow-up. Overall, most patients were elderly (average age 77 ± 10 years), equally distributed for sex, with a high ischemic heart disease (39%). The ratio of isolated diastolic dysfunction (EF >50%) accounted for 38% of the total population, and 24% had a restrictive mitral pattern. The average length of stay was 6.3 ± 4.1 days.
Table 1.
Clinical characteristics of the 300 patients studied, according to BNP changes
| Parameters | All patients (n = 300) | Early responders Group A, n = 46 | Late responders Group B, n = 56 | Non-responders Group C, n = 198 |
|---|---|---|---|---|
| Age (years) | 77 ± 10 | 76 ± 9 | 78 ± 10 | 77 ± 11 |
| Male (%) | 55 | 50 | 45 | 59 |
| Ischemic etiology (%) | 39* | 22 | 34 | 44 |
| Echocardiographic parameters | ||||
| Left ventricular ejection fraction (%) | 46 ± 17 | 54 ± 12 | 56 ± 14 | 44 ± 15a,b |
| Preserved left ventricular (≥50%) (%) | 45** | 65 | 69 | 33 |
| Diastolic restrictive pattern (%) | 22 | 22 | 14 | 24 |
| Laboratory parameters | ||||
| BNP on admission (pg/ml) | 1,017 ± 968 | 406 ± 202 | 569 ± 499 | 1,285 ± 1061a,b |
| BNP on clinical stability (pg/ml) | 844 ± 885 | 151 ± 74 | 344 ± 392 | 1,114 ± 950a,b |
| BNP on discharge (pg/ml) | 665 ± 803 | 145 ± 67 | 143 ± 60 | 933 ± 874a,b |
| Creatinine on admission (mg/dl) | 1.66 ± 1.21 | 1.18 ± 0.33 | 1.70 ± 1.40 | 1.76 ± 1.27a |
| Creatinine on discharge (mg/dl) | 1.72 ± 1.31 | 1.28 ± 0.42 | 1.87 ± 1.59 | 1.78 ± 1.31 |
| eGFR on admission (ml/min/m2) | 50 ± 22 | 60 ± 20 | 48 ± 21a | 48 ± 21a |
| eGFR on discharge (ml/min/m2) | 49 ± 22 | 57 ± 22 | 47 ± 23 | 47 ± 21a |
| Worsening renal function (%) | 22 | 22 | 32 | 20 |
| Transient AKI (%) | 2.0 | 0 | 1.8 | 2.5 |
| Creatinine ≥2.5 mg/dl) on admission | 13** | 0 | 9 | 17 |
| Creatinine ≥2.5 mg/dl) on discharge | 13* | 0 | 14 | 16 |
| Body hydration on admission (%) | 76.4 ± 4.5 | 75.1 ± 3.6 | 76.5 ± 5.1 | 76.7 ± 4.9 |
| Body hydration on clinical stability (%) | 74.2 ± 0.3 | 73.3 ± 0.1 | 74.0 ± 0.4 | 74.5 ± 0.4 |
| Body hydration on discharge (%) | 73.8 ± 3.2 | 73.2 ± 2.1 | 73.5 ± 2.8 | 74.1 ± 3.6 |
| Distribution of body hydration on discharge | ||||
| Moderate o severe dehydration (%) | 5.7 | 4.3 | 7.1 | 5.6 |
| Mild dehydration (%) | 7.6 | 4.3 | 3.6 | 7.6 |
| Normal hydration (%) | 76.3 | 87.0 | 82.1 | 72.2 |
| Mild hyperhydration (%) | 7.3 | 4.3 | 3.6 | 9.1 |
| Moderate/severe hyperhydration (%) | 5.6 | 0 | 3.6 | 5.6 |
| Length of stay (days) | 6.3 ± 4.1 | 3.0 ± 0.9 | 8.0 ± 3.5a | 6.6 ± 4.2a,b |
| 6-month event-free survival (%) | 69.0** | 82.6 | 78.6 | 63.1 |
| 6-month death (%) | 6.0 | 2.2 | 5.3 | 7.1 |
| 6-month readmission for heart failure (%) | 25.0** | 15.2 | 16.1 | 29.8 |
The values are expressed as mean ± SD, unless otherwise specified. * and ** P < 0.05 and P < 0.01 Chi2 test. a and b = P < 0.05, ONE-WAY ANOVA and Tukey’s test, respect to “early-” and “non-responders” respectively. Severe dehydration (<69.0%); moderate dehydration (69.1–71.0%); mild dehydration (71.1–72.70%); normohydration (72.71–74.30%); mild hyperhydration (74.31–81.0%); moderate hyperhydration (81.1–87.0%); severe hyperhydration (≥87.1%)
BNP B-type natriuretic peptide, eGFR estimated glomerular filtration rate
BNP and clinical response data
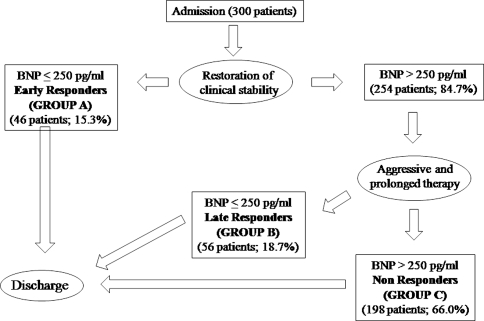
BNP in the whole population was elevated, with a marked reduction from admission to discharge (1,017 ± 968 to 665 ± 803 pg/ml; Wilcoxon test, Z = −8.5; P < 0.001). Of the total 300 patients, 46 (15.3%) achieved restoration of clinical stability with a BNP <250 pg/ml within 72 h (early responders) and were discharged (Fig. 2). The remaining 254 patients underwent “aggressive treatment.” Among this cohort, 56 patients (18.7%) were discharged several days later with a BNP value <250 pg/ml (Late responders). The remaining 198 patients (66%) were discharged with a BNP value >250 pg/ml in spite of a prolonged aggressive therapy (non-responders). Length of stay was significantly shorter in early responders than in either the late- or non-responders groups: 3.0 ± 0.9 days in early responders vs. 8.0 ± 3.5 and 6.6 ± 4.2 days for late and non-responders, respectively (one-way ANOVA and Tukey’s test, P < 0.05) (Table 1 and Fig. 3).
Fig. 2.
Flow-chart of patient’s outcome based on BNP values and BIVA measurements
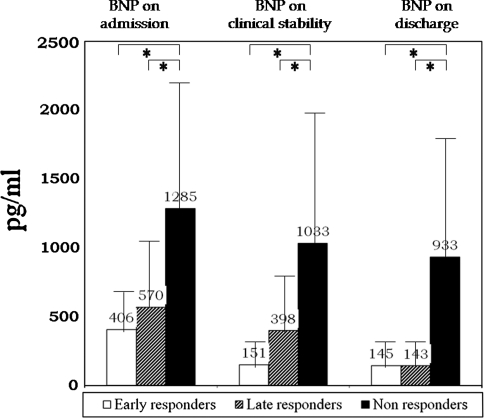
Fig. 3.
BNP levels (pg/ml) on admission, clinical stability, and discharge. Length of stay was 3.0, 8.1 and 6.6 days in the three groups respectively. * P < 0.05; Oneway Anova + Tukey’s Test
BNP levels at discharge were similar in the early- and late responders (145 ± 67 and 143 ± 60 pg/ml, respectively) and significantly lower than those observed in the non-responders (933 ± 873 pg/ml; one-way ANOVA and Tukey’s test, P < 0.05). (Figure 3). The decrease in discharge BNP levels compared with that of the admission levels was larger in both early- and late responders than in the remaining patients: −61 ± 20% and −66 ± 20% versus −4 ± 84% (one-way ANOVA and Tukey’s test, P < 0.05). The most significant reduction in BNP levels in late responders (P < 0.001) was obtained after clinical stabilization (admission: 570 ± 498 pg/ml, clinical stability: 398 ± 293 pg/ml, discharge: 142 ± 69 pg/ml).
Non-responders had higher frequency of ischemic etiology and worse LVEF than patients in groups early- or late responders. Early responders showed lower creatinine levels at all time points (Table 1). Additionally, higher doses of furosemide were prescribed to the late- and non-responders (89 ± 145 and 99 + 165 mg/day) than to early responder group (30 ± 29 mg/day; P < 0.05).
Body hydration status
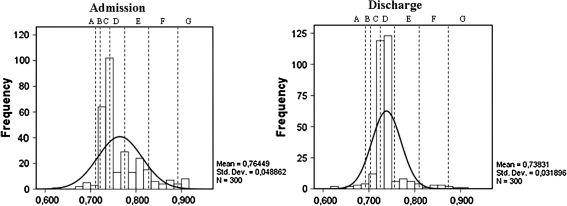
For purposes, of this study, we selected the percentage hydration scale values to characterize patients at admission and at discharge (Fig. 1). At admission, the overall population presented an average value of body hydration of 76.4 ± 4.5%, confirming a trend toward fluid overload. Although hyperhydration was the prevalent feature of our cohort, the accurate assessment of body hydration by BIVA demonstrated that a wide distribution of fluid balance disorders is present in our population (Table 1, Fig. 4). The average values did not differ significantly in the three groups (75.1 ± 3.6, 76.5 ± 5.1, 76.7 ± 4.9%, P = n.s.), and therefore, a case-by-case analysis was carried out to drive therapy during and after admission.
Fig. 4.
Distribution of body hydration status on admission and discharge. A: severe de-hydration (<69.0%); B: moderate de-hydration (69.1–71.0%); C: mild de-hydration (71.1–72.70%); D: normo-hydration (72.71–74.30%); E: mild hyper-hydration (74.31–81.0%); F: moderate hyper-hydration (81.1–87.0%); G: severe hyper-hydration (≥87.1%)
At discharge, body hydration was 73.8 ± 0.03% in the total population and 73.2, 73.5, and 74.1% in the early-, late-, and non-responder groups, respectively; 76.3% of patients were classified as normohydrated, while 6.3 and 5.7% demonstrated mild or moderate–severe dehydration, and 7.3 and 4.3% mild or moderate–severe hyperhydration, respectively (Table 1; Fig. 4). Normohydration at discharge was achieved in 72% of non-responders (after 2.0 ± 3.4 days), 82% of late responders (after 1.9 ± 2.4 days), and 87% of early responders (after 1.0 ± 1.2 days) (Chi2 5.8; P = 0.05). Patients free from hyperhydration at discharge (i.e., normohydrated plus dehydrated) were 96, 93, and 85% of early-, late-, and non-responders (Chi2 5.2; n.s.). It should be noted, however, that at discharge, the distribution of hydration status in the population presents a narrower bell-shaped curve indicating a trend toward normalization (Fig. 4, right panel).
Cardiorenal interactions and kidney function parameters
Overall mean admission creatinine was 1.7 ± 1.2 mg/dl. It was lower in early responders (1.2 ± 0.3 mg/dl) in comparison with late- and non-responders: 1.7 ± 1.4 and 1.8 ± 1.3 mg/dl (one-way ANOVA and Tukey’s test, P < 0.05), respectively. Discharge creatinine showed a similar pattern, being 1.7 ± 1.2 mg/dl in the overall population and 1.3 ± 0.4, 1.9 ± 1.6 and 1.8 ± 1.3 mg/dl in the early-, late-, and non-responder groups, respectively (one-way ANOVA and Tukey’s test; P < 0.05). Creatinine levels at discharge were >2.5 mg/dl in 13% of all patients and in 0, 14.3, and 16.2%, of early-, late-, and non-responders in comparison with 0, 8.9, and 16.7% at admission, respectively.
At discharge, eGFR was 49 ± 22 ml/min/m2 (57 ± 22, 47 ± 21, and 49 ± 22 ml/min/m2 in the early-, late-, and non-responders, respectively; one-way ANOVA and Tukey’s test, P < 0.05), being unchanged with respect to admission values: 50 ± 22 ml/min/m2 overall and 60 ± 20, 48 ± 21, and 48 ± 21 ml/min/m2 (one-way ANOVA and Tukey’s test, P = n.s.), in the early-, late-, and non-responder groups. Considering the overall population, WRF was observed in 67 patients (22.3% of the total). WRF occurred in 22, 32, and 20% of the early-, late-, and non-responder groups, while a transient WRF was seen in 0, 2, and 3% of patients, respectively (P = n.s.) (Table 1). These data suggest that a significant number of hospitalized ADHF patients presents with a wide spectrum of kidney dysfunctions already present at admission. This may result from a cardiorenal syndrome type 2 or from a preexisting general condition of chronic kidney disease (CKD). However, in comparison with previously reported data of AKI occurring in 34% [21] and 37% [32] of hospitalized ADHF patients, BIVA/BNP-driven therapy seems to limit the occurrences of WRF (Table 1). This may be due to a more appropriate management of the fluid balance and hydration status, but will require validation in randomized studies.
BNP, body hydration status, and clinical events during the follow-up period
BNP levels at discharge were significantly lower in the event-free patients than in the patients who had suffered at least one event: 780 ± 734 pg/ml versus 1,156 ± 1,052 pg/ml Mann–Whitney U-test, Z = −3.0, P = 0.003, and 468 ± 606 versus 751 ± 808 pg/ml, Mann–Whitney U-test Z = −3–7, P = 0.000).
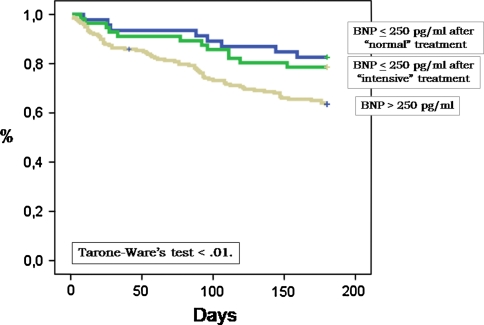
Patients with BNP <250 pg/ml at discharge (early- and late responders) showed less cumulative events (20%) in comparison with non-responders (36%) (P = 0.003). No significant differences in event rate were seen in relation to the time necessary to obtain a reduction in BNP values below 250 pg/ml (18 vs. 21% for early—vs. late responders, respectively, P = 0.31) (Fig. 5).
Fig. 5.
Kaplan–Meier curves showing the cumulative incidence of death and readmission in early- and late-responders and non-responders (see text)
Discussion
In the present study, patients hospitalized for ADHF presented with various degrees of congestion, and all displayed high BNP levels. Despite a reduction in congestion in all groups, changes of BNP in response to therapy, described as early-, late-, and non-responders, were subsequently associated with post-discharge outcomes (Fig. 5). This, together with an accurate determination of the hydration status by BIVA, helped identifying the true hydration status, also described as “dry” BNP in patients with HF. We found the combination of BNP and BIVA measurement, helped to avoid unnecessary aggressive diuretic therapy, reducing the level of renal complications, especially in the early- and non-responder groups. This was in distinction to the late responders group, who received the more aggressive and prolonged diuretic therapy in order to achieve BNP reduction, occurring at the expense of a trend of more WRF and AKI. These results, confirm that the status of hydration and myocardial performance in patients with HF, are linked by a complex relationship. Analyzing case by case, it is possible to establish that every patient has a “personal” threshold of hyper- or hypohydration leading to congestion or organ hypoperfusion and hemodynamic instability, respectively.
As reported elsewhere, the majority of patients admitted with ADHF display a good response to loop diuretics and vasoactive agents [35]; however, in some cases, subclinical volume expansion may result in diuretic under-treatment and progressive worsening of symptoms [33, 34]. On the other hand, excessive diuretic therapy in patients with mild overhydration may lead to dehydration and organ hypoperfusion. For this reason, an accurate assessment of body fluid status is essential in HF patients.
The effect of volume status on plasma BNP levels has been examined previously in patients with HF [36]. In chronic HF, clinically unrecognized hyperhydration is frequently present in non-edematous patients with HF and is associated with increasing filling pressures [37]. Since BNP release is triggered by increased volume load and myocadiac wall stretch [38], the level of BNP has been proposed as a “surrogate” of congestion. It is hypothesized that the BNP level of a patient admitted with ADHF is a result of two components: a baseline, euvolemic “dry” BNP level (reflecting myocardial status), and a volume/pressure-induced “wet” BNP (reflecting hydration status) [6].
Guidelines to assess congestion during hospitalization or pre-discharge are not well established. In fluid overloaded patients requiring diuresis, standard monitoring includes the evaluation of clinical signs and symptoms, chest X-ray, and body weight change. Although an increase in body weight predicts hospitalization [39], its reduction in response to therapy may not result in better outcomes.
Nevertheless, quantifying the extent of congestion and body hydration status in these patients is difficult. In this setting, clinical and radiographic findings show poor correlation with invasive measurements of pulmonary capillary wedge pressures [40]. Other methods that directly measure extravascular lung water are expensive, complicated, and not widely available [13].
We found that the BNP/BIVA combination may add useful information to standard clinical parameters in guiding diuretic therapy and congestion relief strategies.
Our study demonstrates the complex link between body fluid status and BNP levels during hospitalization for ADHF and the importance of “euvolemia” concept. At stable BNP levels, some patients may have a very narrow volume window, with small changes resulting in congestion or organ hypoperfusion. In these patients, failure to achieve an optivolemic state at discharge may result in higher rates of short- and long-term complications. Furthermore, inadequate diuretic use may cause AKI because of renal arterial underfilling and inadequate renal response to hormonal stimuli [41]. In this settings, BNP/BIVA-guided management allows the differentiation of “wet” and “dry” BNP values, thus avoiding over- or under-treatment of patients and preventing long-term complications and WRF.
Finally, despite aggressive therapy, some patients never reach target levels of BNP (<250 pg/ml in our study), despite of apparent euvolemia. These non-responders are subject to higher rates of long-term complications, rehospitalization, and death. When BIVA values describe a nearly normal hydration status in these patients, BNP represents the “dry” component of the neurohormonal response to myocardial dysfunction.
The prognostic role of neurohumoral markers in ADHF is of growing clinical importance. Natriuretic peptides are currently the benchmark against which all new biomarkers must be compared. However, growing evidence shows that hypervolemia by itself is independently associated with mortality and it can be considered a biomarker itself [38, 42, 43]. A recent review [1] states that discharge after complete resolution of signs and symptoms compared with earlier discharge with residual symptoms and close follow-up for further optimization should be compared. This concept has been supported in a contemporary consensus paper [6] where the BNP/NT-proBNP pre-discharge level is suggested as a tool to establish the patient’s “dry weight.” We would like to further extend this concept and introduce the use of BIVA as an additional measure to support clinical decisions. In a previous study, we demonstrated that the extent and rapidity of changes in the BNP level during hospitalization (an average of 5.5 days) is a reliable outcome predictor in ADHF [17]. The current study extends these findings and demonstrates that BIVA/BNP-guided management during hospitalization for HF is associated with lower events after discharge, independently of other prognostic variables. In the present study, the threshold level 250 pg/ml was derived from an ROC analysis and the calculated optimal cutoff was chosen to divide patients according to BNP values on discharge. Among patients with a final concentration of 250 pg/ml, subsequent events were significantly lower in those who reached a BIVA-guided level below this threshold at discharge.
Most patients have rapid symptomatic improvement with loop diuretics and have a relatively short hospital stay [35]. We have characterized the response of patients with ADHF into three groups: early responders, late responders, and non-responders. In the first two groups, where the only difference was the time necessary to obtain a reduction in BNP values below 250 pg/ml, no differences in event rates were noticed (17.4 vs. 21% for “early responders” and “late –responders,” respectively, P = 0.31). On the contrary, the third group of patients that never reached BNP <250 pg/ml at discharge displayed marked modification of the prognosis with high rate of complications, death, and rehospitalization. In other words, patients with an initial BNP concentration above the threshold level have, on average, markedly divergent outcomes depending on whether they maintain or reduce their level of BNP after receiving a BIVA-guided treatment of fluid overload. It must be emphasized, however, that in all groups, mid-long-term complications were markedly lower than those reported in the literature [21, 22, 32], supporting the concept that BIVA-guided therapy may significantly contribute to achieve the best BNP level possible, minimizing and limiting the negative effects of an inadequate and aggressive diuretic or fluid removal therapy.
Therefore, our data support a strategy of serial determinations of BNP concentration during in-hospital phase and classification into categories of changes according to threshold levels combined with and hydration status measured by BIVA. This approach appeared in our study is adequate for risk stratification of patients with ADHF.
Limitations
This study has several limitations, the most important of which is there was no blinded randomized control arm to determine what could be the concurrent effect of contemporary non-BIVA-guided therapy. Thus, a further prospective study is warranted. Secondly, this single-center study may not be generalizable to other populations, as treatment strategies and the specific population enrolled, may explain why the overall rate of adverse events was lower than reported in other large trials. Finally, treatment strategies were left to the attending physician. By not having a standard treatment algorithm, duplication of our results may be challenging.
With regard to the hydration status at discharge, because we could not reach a net separation among the groups, it is impossible to determine whether different classes of hydration described by BIVA correlate with specific outcomes. However, we speculate that the concept of adequate hydration status may be different from case to case and above all, the window of tolerance for hyper- or dehydration may be wider or tighter in patients affected by different heart disorders. Nevertheless, the low incidence of WRF in the overall treated population and the low rate of long-term complications observed in all groups suggests that the combined BIVA/BNP measure as a driving diagnostic tool for fluid removal therapy may represent a significant advance in the management of ADHF patients.
Conclusion
We found the addition of BIVA to serial BNP measurement allowed a more accurate risk stratification of patients undergoing diuretic therapy potentially leading to a better treatment strategy and reduction in complications. Thus, the combination of BNP and BIVA measurements may represent a novel, but logical criteria for discharge and risk stratification.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- ADHF
acute decompensated heart failure
- AHF
acute heart failure
- BNP
B-type natriuretic peptide
- BIVA
bioelectrical impedance vectorial analysis
- CRS
cardiorenal syndrome
- CHF
chronic heart failure
- CKD
chronic kidney disease
- CV
cardiovascular
- eGFR
estimated glomerular filtration rate
- EF
ejection fraction
- HF
heart failure
- HFU
heart failure unit
- LVEF
left ventricular ejection fraction
- NYHA
New York Heart Associaction Functional Class
- WRF
worsening renal function
References
- 1.Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol. 2009;53:557–573. doi: 10.1016/j.jacc.2008.10.041. [DOI] [PubMed] [Google Scholar]
- 2.Maisel A. Practical approaches to treating patients with acute decompensated heart failure. J Card Fail. 2001;7:13–17. doi: 10.1054/jcaf.2001.26646. [DOI] [PubMed] [Google Scholar]
- 3.Philbin EF, DiSalvo TG. Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33:1560–1566. doi: 10.1016/S0735-1097(99)00059-5. [DOI] [PubMed] [Google Scholar]
- 4.Peacock WF. Rapid optimization: strategies for optimal care of decompensated congestive heart failure patients in the emergency department. Rev Cardiovasc Med. 2002;3:S41–S48. [PubMed] [Google Scholar]
- 5.Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type-natriuretic peptide predict death and cardiac events in patients with heart failure: a systematic review. BMJ. 2005;330:625–634. doi: 10.1136/bmj.330.7492.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maisel A, Mueller C, Adams K, Jr, Anker SD, Aspromonte N, Cleland JG, Cohen-Solal A, Dahlstrom U, DeMaria A, Di Somma S, Filippatos GS, Fonarow GC, Jourdain P, Komajda M, Liu PP, McDonagh T, McDonald K, Mebazaa A, Nieminen MS, Peacock WF, Tubaro M, Valle R, Vanderhyden M, Yancy CW, Zannad F, Braunwald E. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10:824–839. doi: 10.1016/j.ejheart.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Logeart D, Thabut G, Jourdain P, Chavelas C, Beyne P, Beauvais F, Bouvier E, Solal AC. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43:635–641. doi: 10.1016/j.jacc.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 8.Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, Saltzberg M, Ellison SR, Bhalla MA, Bhalla V, Clopton P, Jesse R. Rapid emergency department heart failure outpatient trial investigators. primary results of the rapid emergency department heart failure outpatient trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44:1328–1333. doi: 10.1016/j.jacc.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, Maisel A. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001;7:21–29. doi: 10.1054/jcaf.2001.23355. [DOI] [PubMed] [Google Scholar]
- 10.Valle R, Aspromonte N. Use of brain natriuretic peptide and bioimpedance to guide therapy in heart failure patients. Contrib Nephrol. 2010;164:209–216. doi: 10.1159/000313732. [DOI] [PubMed] [Google Scholar]
- 11.Paterna S, Di Pasquale P, Parrinello G, Fornaciari E, Di Gaudio F, Fasullo S, Giammanco M, Sarullo FM, Licata G. Changes in brain natriuretic peptide levels and bioelectrical impedance measurements after treatment with high-dose furosemide and hypertonic saline solution versus high-dose furosemide alone in refractory congestive heart failure. J Am Coll Cardiol. 2005;45:1997–2003. doi: 10.1016/j.jacc.2005.01.059. [DOI] [PubMed] [Google Scholar]
- 12.Peacock WF, Soto KM. Current techniques of fluid status assessment. Contrib Nephrol. 2010;164:128–142. doi: 10.1159/000313726. [DOI] [PubMed] [Google Scholar]
- 13.Tang WH, Tong W. Measuring impedance in congestive heart failure: current options and clinical applications. Am Heart J. 2009;157:402–411. doi: 10.1016/j.ahj.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parrinello G, Paterna S, Di Pasquale P, Torres D, Fatta A, Mezzero M, Scaglione R, Licata G. The usefulness of bioelectrical impedance analysis in differentiating dyspnea due to decompensated heart failure. J Card Fail. 2008;14:676–686. doi: 10.1016/j.cardfail.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Heywood JT. The cardiorenal syndrome: lessons from the ADHERE database and treatment options. Heart Fail Rev. 2004;9:195–201. doi: 10.1007/s10741-005-6129-4. [DOI] [PubMed] [Google Scholar]
- 16.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–1539. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 17.Valle R, Aspromonte N, Giovinazzo P, Carbonieri E, Chiatto M, di Tano G, Feola M, Milli M, Fontebasso A, Barro S, Bardellotto S, Milani L. B-type natriuretic Peptide-guided treatment for predicting outcome in patients hospitalized in sub-intensive care unit with acute heart failure. J Card Fail. 2008;14:219–224. doi: 10.1016/j.cardfail.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 18.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of CHF. The Framingham study. N Engl J Med. 1971;285:1442–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 19.Faggiano P, Valle R, Aspromonte N, D’Aloia A, Di Tano G, Barro S, Giovinazzo P, Milani L, Lorusso R, Dei Cas L. How often we need to measure brain natriuretic peptide (BNP) blood levels in patients admitted to the hospital for acute severe heart failure? Role of serial measurements to improve short-term prognostic stratification. Int J Cardiol. 2010;140:88–94. doi: 10.1016/j.ijcard.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 20.ESC G. uidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Eur Heart J. 2008;29:2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 21.Metra M, Nodari S, Parrinello G, Bordonali T, Bugatti S, Danesi R, Fontanella B, Lombardi C, Milani P, Verzura G, Cotter G, Dittrich H, Massie BM, Cas LD. Worsening renal function in patients hospitalised for acute heart failure: clinical implications and prognostic significance. Eur J Heart Fail. 2008;10:188–195. doi: 10.1016/j.ejheart.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Forman DE, Butler J, Wang Y, Abraham WT, O’Connor CM, Gottlieb SS, Loh E, Massie BM, Rich MW, Stevenson LW, Young JB, Krumholz HM. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43:61–67. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 23.Gottlieb SS, Abraham W, Butler J, Forman DE, Loh E, Massie BM, O’connor CM, Rich MW, Stevenson LW, Young J, Krumholz HM. The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Card Fail. 2002;8:136–141. doi: 10.1054/jcaf.2002.125289. [DOI] [PubMed] [Google Scholar]
- 24.Cruz DN, Ricci Z, Ronco C. Clinical review: RIFLE and AKIN–time for reappraisal. Critical Care. 2009;13:211–216. doi: 10.1186/cc7759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ronco C, Chionh CY, Haapio M, Anavekar NS, House A, Bellomo R. The cardiorenal syndrome. Blood Purif. 2009;27:114–126. doi: 10.1159/000167018. [DOI] [PubMed] [Google Scholar]
- 26.Smilde TD, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Drawbacks and prognostic value of formulas estimating renal function in patients with chronic heart failure and systolic dysfunction. Circulation. 2006;114:1572–1580. doi: 10.1161/CIRCULATIONAHA.105.610642. [DOI] [PubMed] [Google Scholar]
- 27.Valle R, Bagolin E, Giovinazzo P, Barro S, Aspromonte N, Carbonieri E, Milani L. The BNP assay does not identify mild left ventricular diastolic dysfunction in asymptomatic diabetic patients. Eur J Echocardiogr. 2006;7:40–44. doi: 10.1016/j.euje.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 28.(1996) Bioelectrical impedance analysis in body composition measurement. In: Proceedings of a national institutes of health technology assessment conference. Bethesda, Maryland, December 12–14, 1994. Am J Clin Nutr 64(Suppl):387S–532S [DOI] [PubMed]
- 29.Sergi G, Bussolotto M, Perini P, Calliari I, Giantin V, Ceccon A, Scanferla F, Bressan M, Moschini G, Enzi G. Accuracy of bioelectrical impedance analysis in estimation of extracellular space in healthy subject and in fluid retention states. Ann Nutr Metab. 1994;38:158–165. doi: 10.1159/000177806. [DOI] [PubMed] [Google Scholar]
- 30.Piccoli A, Rossi B, Pillon L, Bucciante G. A new method for monitoring body fluid variation by biompedance analysis: the RXc graph. Kidney Int. 1994;46:534–539. doi: 10.1038/ki.1994.305. [DOI] [PubMed] [Google Scholar]
- 31.Piccoli A. Patterns of bioelectrical impedance vector analysis: learning from electrocardiography and forgetting electric circuit models. Nutrition. 2002;18:520–521. doi: 10.1016/S0899-9007(02)00771-2. [DOI] [PubMed] [Google Scholar]
- 32.Logeart D, Tabet JY, Hittinger L, Thabut G, Jourdain P, Maison P, Tartiere JM, Solal AC. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. Int J Cardiol. 2008;127:228–232. doi: 10.1016/j.ijcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW. Young JB; OPTIMIZE-HF Investigators and hospitals characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50:768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 34.Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) database. J Am Coll Cardiol. 2006;47:76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 35.Fonarow GC, Heywood JT, Heidenreich PA, Lopatin M, Yancy CW. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2007;153:1021–1028. doi: 10.1016/j.ahj.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 36.Braunschweig F, Linde C, Eriksson MJ, Hofman-Bang C, Rydén L. Continuous haemodynamic monitoring during withdrawal of diuretics in patients with congestive heart failure. Eur Heart J. 2002;23:59–69. doi: 10.1053/euhj.2001.2690. [DOI] [PubMed] [Google Scholar]
- 37.Androne AS, Hryniewicz K, Hudaihed A, Manciri D, Lamanca J, Katz SD. Relation of unrecognized hypervolemia in chronic heart failure to clinical status, hemodynamics, and patient outcomes. Am J Cardiol. 2004;93:1254–1259. doi: 10.1016/j.amjcard.2004.01.070. [DOI] [PubMed] [Google Scholar]
- 38.Iwanaga Y, Nishi I, Furuichi S, Noguchi T, Sase K, Kihara Y, Goto Y, Nonogi H. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. J Am Coll Cardiol. 2006;47:742–748. doi: 10.1016/j.jacc.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 39.Chaudhry SI, Wang Y, Concato J, Gill TM, Krumholz HM. Patterns of weight change preceding hospitalization for heart failure. Circulation. 2007;116:1549–1554. doi: 10.1161/CIRCULATIONAHA.107.690768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chakko S, Woska D, Martinez H, de Marchena E, Futterman L, Kessler KM, Myerberg RJ. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med. 1991;90:353–359. doi: 10.1016/0002-9343(91)80016-f. [DOI] [PubMed] [Google Scholar]
- 41.Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol. 2009;53:582–588. doi: 10.1016/j.jacc.2008.08.080. [DOI] [PubMed] [Google Scholar]
- 42.Drazner MH, Rame JE, Stevenson LW, Dries DL. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001;345:574–581. doi: 10.1056/NEJMoa010641. [DOI] [PubMed] [Google Scholar]
- 43.Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Critical Care. 2008;12:169–172. doi: 10.1186/cc6948. [DOI] [PMC free article] [PubMed] [Google Scholar]