Abstract
Background
The decision-making processes used for out-of-hospital trauma triage and hospital selection in regionalized trauma systems remain poorly understood. The objective of this study was to understand the process of field triage decision-making in an established trauma system.
Methods
We used a mixed methods approach, including EMS records to quantify triage decisions and reasons for hospital selection in a population-based, injury cohort (2006 - 2008), plus a focused ethnography to understand EMS cognitive reasoning in making triage decisions. The study included 10 EMS agencies providing service to a 4-county regional trauma system with 3 trauma centers and 13 non-trauma hospitals. For qualitative analyses, we conducted field observation and interviews with 35 EMS field providers and a round-table discussion with 40 EMS management personnel to generate an empirical model of out-of-hospital decision making in trauma triage.
Results
64,190 injured patients were evaluated by EMS, of whom 56,444 (88.0%) were transported to acute care hospitals and 9,637 (17.1% of transports) were field trauma activations. For non-trauma activations, patient/family preference and proximity accounted for 78% of destination decisions. EMS provider judgment was cited in 36% of field trauma activations and was the sole criterion in 23% of trauma patients. The empirical model demonstrated that trauma triage is driven primarily by EMS provider “gut feeling” (judgment) and relies heavily on provider experience, mechanism of injury, and early visual cues at the scene.
Conclusions
Provider cognitive reasoning for field trauma triage is more heuristic than algorithmic and driven primarily by provider judgment, rather than specific triage criteria.
Introduction
The goal of regionalized care is to improve patient outcomes and efficient use of limited resources by directing patients with certain clinical conditions to hospitals with optimized capabilities to care for them.1 For trauma patients, the model of bypassing closer hospitals to concentrate seriously injured patients in specialized trauma centers has been shown to improve patient outcomes2-5 and serves as the primary model for regionalized care. Regionalized care systems are increasingly being developed and advocated for other time-dependent, high-acuity clinical conditions, such as ST-segment elevation myocardial infarction, stroke, and cardiac arrest.
To optimize such regionalized care systems, there must be a practical mechanism and/or criteria with good predictive value to identify patients with specific clinical conditions early in their course by emergency medical services (EMS) personnel. Most U.S. trauma systems use an out-of-hospital triage protocol based on the American College of Surgeons Committee on Trauma (ACSCOT) Field Triage Decision Scheme6,7 for this purpose. The ACSCOT decision scheme is a 4-step algorithm containing 24 criteria that is designed to identify seriously injured patients for immediate transport to major trauma centers.6,7 Although implementation of a trauma system can modify the hospital distribution of seriously injured patients,4 studies have suggested that many patients with minor injuries are transported to trauma centers (i.e., over-triage)8,9 and that a substantive number of patients with serious injuries are cared for in non-trauma hospitals (under-triage).10,11 It remains unclear whether the field triage criteria are insufficiently discriminating or whether other less defined factors (e.g., EMS provider decision-making, patient or provider preferences) are influencing triage decisions and the resulting regional distribution of trauma patients. Understanding factors affecting the selection of hospitals is imperative in facilitating the vision for a fully integrated emergency care delivery system1,12 and in developing models of regionalized care for other acute conditions.
In this study, we evaluate how decisions are made in the out-of-hospital setting, EMS provider cognitive reasoning, reasons for selecting specific hospitals, and the resulting hospital distribution of injured patients in a well-established trauma system.
Materials and Methods
Study Design
We conducted a mixed methods study, including population-based quantitative data for injured patients activating the 9-1-1 EMS system in a 4-county region, plus a focused ethnography to qualitatively describe the cognitive processes EMS personnel use in making triage and hospital selection decisions.
Study Setting
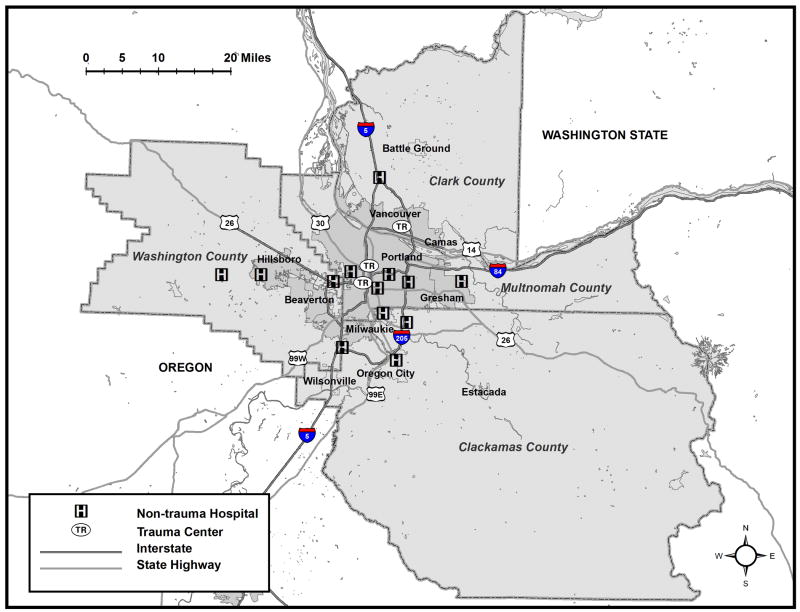
This study was performed with 10 EMS agencies (4 private ambulance agencies and 6 fire departments) and 16 hospitals (two Level I trauma centers, one Level II trauma center, one Veterans Affairs hospital, and 12 community hospitals) in a 4-county region with a mature trauma system. A map of the 4-county region, with trauma and non-trauma hospitals, is depicted in Figure 1, along with a corresponding table of population demographics.13 Based on the geography and population densities in this region, the vast majority of injured patients transported by EMS reasonable transport times to the nearest trauma center. The four counties use a dual-advanced life support EMS system, where the majority of 9-1-1 responses are served by both fire (first responder) and private ambulance agencies. For injured patients evaluated by EMS providers, there is an initial triage decision of whether or not to “enter” the patient into the trauma system (also termed “trauma activation”) based on field criteria to identify patients with serious injury (Table 1). Field trauma activation triggers protocolized, direct transport to one of the three trauma centers. The Oregon Trauma System stipulates that patients meeting predefined triage criteria be transported directly to a Level I or II trauma center, unless EMS providers are unable to establish and maintain an adequate airway or if a Level III or IV hospital is significantly closer. Because there are no Level III/IV hospitals in the Portland-Vancouver metropolitan area (i.e., due to proximity of the three trauma centers), there is a choice among EMS providers of transporting to a major trauma center vs. a non-trauma hospital in almost all instances in this region. The majority of patients entered into the trauma system are done so by EMS providers. For injured patients not entered into the trauma system, EMS providers are instructed to ask patients/families where they want to be transported to better match the receiving hospital to the facility where patients generally receive their care and to minimize subsequent interhospital transfers. Three hospital and one EMS agency Institutional Review Boards reviewed and approved this study protocol.
Figure 1. Map of the 4-county study region, including hospitals, trauma centers, major roadways and rivers.
| County | State | Population | Land area (square miles) | Population density (persons per square mile) | % > 65 years | % < 18 years |
| Multnomah | OR | 726,855 | 435 | 1671 | 10.2% | 21.2% |
| Washington | OR | 537,318 | 724 | 742 | 9.5% | 25.6% |
| Clackamas | OR | 386,143 | 1,868 | 207 | 13.1% | 23.3% |
| Clark | WA | 432,002 | 628 | 688 | 11.2% | 26.2% |
| Totals: | - | 2,082,318 | 3,655 | 570 | 10.7% | 23.7% |
*Population demographics are based on 2009 estimates.13 The two trauma centers (TR) in Portland (Multnomah County) are Level I hospitals and the trauma center (TR) in Vancouver (Clark County) is a Level II hospital.
Table 1.
Oregon Trauma System field trauma triage criteria.*
| Physiologic criteria: |
| Systolic blood pressure < 90 mmHg |
| Respiratory rate < 10, >29, or need for airway management |
| Glasgow Coma Scale score ≤ 12 |
|
|
| Anatomic criteria: |
| Flail chest |
| 2 or more fractures of femur/humerus |
| Penetrating injury, mid-thigh to head |
| Amputation above wrist or ankle |
| Spinal cord injury with paralysis |
|
|
| Mechanism of injury: |
| Heavy extrication > 20 minutes |
| Death of same car occupant |
| Ejection from closed vehicle |
| High energy transfer situation: |
| Fall > 20 feet |
| Pedestrian hit 20 mph or thrown 15 feet |
| Motorcycle/ATV/bicycle crash |
| Vehicle rollover |
| Impact or significant intrusion |
|
|
| Risk factor criteria: |
| Medical illness |
| Pregnancy |
| Presence of intoxicants |
| Hostile environment (heat, cold, etc.) |
| Age < 5 or > 55 years (some use < 12 or > 55 years) |
| EMS provider judgment |
Patient Population
The study sample included all patients activating the 9-1-1 EMS system within the 4-county region where the EMS provider recorded a primary impression of “injury” or “trauma”, regardless of field disposition, destination facility, or outcome. Specifying the sample in this manner allowed for a population-based, out-of-hospital injury cohort of patients with both minor and serious injuries, as perceived by EMS providers (and the population to which the trauma triage criteria are applied). We obtained electronic health records from each of the 10 participating EMS agencies over a 3-year period (January 1, 2006 through December, 31 2008). Interhospital transfers without an initial presentation involving EMS were excluded from the sample.
Quantitative Variables
We identified field-based trauma system activations based on the presence of any of the following factors: EMS provider documented “trauma system entry,” a recorded trauma band number (wrist band applied in the field upon trauma system activation), trauma triage criteria specified in the EMS chart, or a matched record from the Oregon or Washington trauma registry specifying “scene” origin for trauma system activation. We also recorded field disposition, hospital destination, and the EMS provider-recorded reason for selecting a particular hospital (specialty hospital, closest hospital, ambulance diversion, patient/family request, physician request, law enforcement, other). The categories delineating reasons for destination selection were based on the standard National EMS Information System14 definition, with “specialty hospital” generally referring to tertiary care centers. Acute care hospitals were categorized as trauma centers (accredited Level I or II trauma facilities) or non-trauma centers.
Quantitative Data Analysis
Because two or more EMS records are typically generated for each patient in this system, we used probabilistic linkage15 (LinkSolv v8.2, Strategic Matching, Inc., Morrisonville, NY) to match fire department and ambulance agency records and to ensure comprehensive information from the field. The resulting database was then linked to base hospital and trauma registry records using the same methodology. We have previously validated the use of probabilistic linkage for matching similar databases in our EMS system.16 We used descriptive statistics to characterize field disposition, triage criteria, reasons for selecting hospitals, and the resultant hospital distribution of patients (SAS v9.2, SAS Institute, Cary, NC).
Qualitative data collection and analysis
To better understand the decision-making process for field trauma activation and hospital selection, we also conducted a focused ethnography using participant observation and interviews with 35 EMS providers. Three investigators (CDN, MN, MK) spent approximately 60 hours in the field during 10 scheduled “ride-alongs,” which were split evenly between fire and ambulance crews in each of the 4 counties. Field observation and interviews were conducted with the same “team” setting used in field care (i.e., two EMS personnel for ambulance agencies; 3 to 8 EMS personnel for fire crews) to replicate the dynamic and team-based cognitive reasoning processes used in actual triage situations. Field observation and interviews were conducted apart from supervisory personnel to avoid conditioned responses and lack of complete candor with answers. Due to concerns about patient confidentiality, we did not use audio recorders in the field. Investigators followed a standardized interview script with “probes” to assure comprehensive and uniform coverage of each topic17 (Appendix 1), took copious notes during the sessions, and transcribed notes within 24 hours. To supplement the field sessions and assess perspectives from supervisory EMS personnel, we also held a round-table discussion with high-ranking EMS officials (i.e., EMS administrators, training officers, fire chiefs, and EMS medical directors) during an annual regional EMS meeting (n = 40). We used a focus group approach in facilitating this discussion.17
We followed standard qualitative methods for the analysis of interviews, field observations, and the group discussion.17,18 Investigators read through all transcribed notes and identified key ideas, phrases, recurrent themes, and how these themes interacted with and influenced each other. All transcripts were then iteratively re-evaluated to assess the frequency of such ideas and phrases, precipitating themes, and how recurring concepts fit into major content domains.17 Subcategories within these domains were developed, along with illustrative quotes and phrases that demonstrated relevant ideas. Findings were compared to the current 4-step algorithm for field triage and used to develop a conceptual framework explaining field triage cognitive reasoning.
Results
Quantitative Results
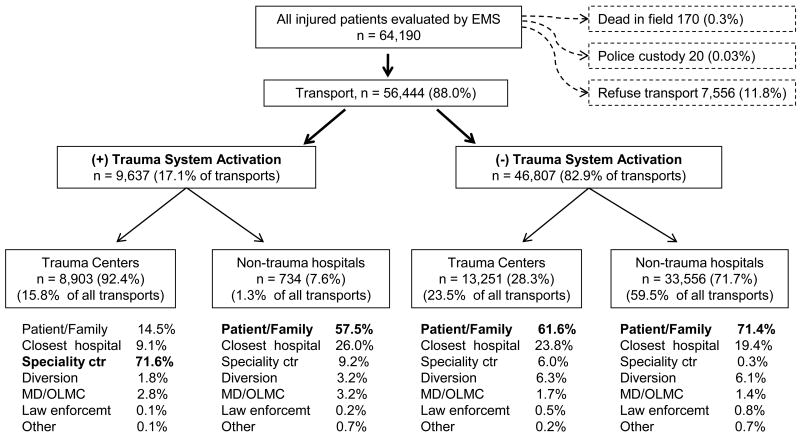
Over the 3-year time period, 64,483 injured patients were evaluated by EMS providers in the 4-county region, of whom 64,190 patients had complete information on field disposition and reasons for hospital selection and form the primary sample. There were 56,444 (88.0%) patients transported to acute care hospitals, of whom 9,637 (17.1% of transported patients) were entered into the trauma system by EMS providers. Among patients entered into the trauma system by field providers, 8,903 (92.4%) were transported to major trauma centers, while 28.3% of non-trauma activations (n = 13,251) were also transported to trauma centers (Figure 2). Patient/family preference and proximity were the prevailing reasons for selecting certain hospitals among injured patients not entered into the trauma system (Figure 2) and overall (Table 2). Among trauma activations, the most commonly cited reasons for field entry into the trauma system (up to three per patient) were: EMS provider judgment (36%), injury in the setting of intoxicants (15%), age extremes (14%), GCS ≤ 13 (10%) and significant vehicle intrusion (10%). When restricted to patients with a single reason for field trauma activation, EMS provider judgment (23%) remained the most common triage criterion.
Figure 2. Regional distribution of injured patients in 4-county region.
*“(+) Trauma System Activation” patients were entered into the trauma system from the field by EMS personnel (i.e., field trauma “activations” or “trauma system entries”) based on standard trauma triage criteria. Patient/Family = destination requested by the patient or family; Closest hospital = hospital selected based on proximity to field location/event site; MD = medical doctor; OLMC = on-line medical control; Specialty ctr = hospital with specialized clinical resources for patient care, as interpreted by the field provider; Diversion = hospital emergency department closed to ambulance traffic; Law enforcemt = police or sheriff requested destination facility; Other = HMO, EMS supervisor request, other reason.
Table 2.
Reasons for selecting hospital destinations by out-of-hospital providers among all injured patients transported by EMS (n = 56,444).
| Patient/family request | 29,461 (52.2%) |
| Proximity | 9,349 (16.6%) |
| Specialty hospital | 6,732 (11.9%) |
| Ambulance diversion | 2,688 (4.8%) |
| Physician choice/on-line medical control | 851 (1.5%) |
| Law enforcement | 313 (0.6%) |
| Other (HMO, protocol, supervisor) | 225 (0.4%) |
| Not reported | 6,825 (12.1%) |
Qualitative Results
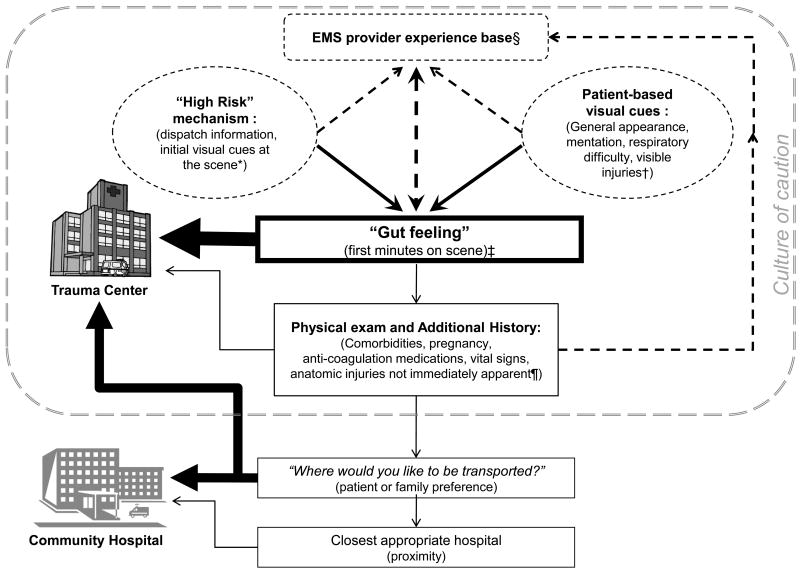
Our interviews and observations revealed that decisions about field trauma triage are driven largely by provider judgment, rather than specific triage criteria. EMS personnel rationalize their decision-making processes based on experience and a culture that encourages conservative decision-making and accommodates over-triage. A schematic summarizing the findings detailed below in a cognitive reasoning model of field trauma triage is illustrated in Figure 3.
Figure 3. Model of out-of-hospital provider decision making for identifying seriously injured patients and selecting hospital destinations.
*“High Risk Mechanism” involves all the mechanisms of injury listed in the ACSCOT field decision scheme,6,7 but also includes contextual factors about how the injury occurred.
†Patient-based visual cues include all information gleaned through a rapid visual assessment of the patient (e.g., general mentation, responsiveness, work of breathing, and visually obvious injuries) and surrounding scene (e.g., property damage, vehicle damage), which are generally done before making contact with the patient.
‡ Field provider “gut feeling” is the primary driver for determining whether the patient may have a serious injury and therefore require care at a major trauma center. This assessment is a summation of information available before arrival on scene and visually available immediately after arrival on scene. The cognitive processing involved in this step is estimated to occur in 1-2 minutes, is closely tied to and influenced by the provider's experience level.
¶ Physical exam and additional history often occur after the primary decision-making process for trauma patients. This step involves formal assessment of vital signs (including Glasgow Coma Scale score), physical exam assessment for anatomic injuries that were not immediately apparent (e.g., abdominal tenderness, evidence of pelvis fracture, paralysis, evidence of penetrating injury, etc.), and relevant medical history (e.g., anti-coagulation medications, hemodialysis, pregnancy, significant cardiovascular or pulmonary disease).6,7 Field providers believe this step identifies a minority of patients with serious injuries that were not previously identified by provider “gut feeling.”
§ Provider experience level is closely tied to the ability to quickly generate a “gut feeling” and therefore early decision-making for suspicion of serious injury.
“Gut Feeling”
EMS providers consistently stated that the decision of whether or not to enter a patient into the trauma system is driven primarily by field provider “gut feeling,” rather than by explicit triage criteria. This decision is typically made early at the scene (i.e., often within the first several minutes), frequently before even making physical contact with the patient. The triage process is heavily influenced by initial dispatch information (e.g., mechanism of injury and location of event), early visual cues from the scene (including appearance of patient), and provider experience. The triage process was repeatedly described as done by “feel,” with one paramedic stating “You can tell right when you see the patient… you just know.” The majority of EMS providers felt that mechanism of injury plays a large role in triage decisions, as this is often the earliest available information, and noted that the role of mechanism of injury is highly contextual. Mechanism of injury tends to be considered “high risk,” “concerning,” or “worrisome,” rather than describing specific mechanisms of injury (e.g., exact number of feet in a fall). Information gathered during the subsequent phase of patient assessment (history from the patient and/or bystanders, vital signs, and physical exam) is generally used to support the already-made decision for trauma system activation, but not to refute it. Occasionally, there will be no concerning “gut-feeling” by the EMS provider from the initial visual assessment, with the second phase of assessment (hands-on) revealing a concerning finding (e.g., abdominal tenderness, low blood pressure, previously unrecognized injury), though this was thought to be uncommon. All EMS personnel recognized judgment (discretion) to be the most common reason for identifying seriously injured patients.
Provider Experience
Provider experience was repeatedly mentioned as a significant factor in interpreting key information and visual cues from the scene. With multiple EMS personnel at the scene, the most experienced provider will often guide the decision to enter a patient into the trauma system. However, concern by any field provider for serious injury is generally upheld as a reason to triage a patient to a trauma center. Statements such as “I've been burned by that before,” referring to specific clinical situations (e.g., patient with abdominal pain who appeared well, but subsequently was found to have serious injury) were mentioned by several participants as examples of provider experience that guide decision-making on more subtle presentations of serious injury. Several providers stated that the triage algorithm was “for newbies” and generally not useful for more experienced field providers, though all providers supported the triage algorithm for provider education and developing a framework for trauma triage.
Patient and Provider Preferences
For patients not identified as seriously injured (i.e., non-trauma system activations), EMS providers consistently stated patient/family preference to be the next most important factor for hospital selection. Patients are simply asked “Where would you like to be transported?” If the patient/family does not have a preference, proximity (closest hospital) is the next most important factor. Ambulance diversion status plays a smaller but important role, and periodically modifies the options for hospital transport. EMS provider perceptions of patient needs (e.g., surgical intervention, specialty care), costs to the patient, perceived availability of hospital resources, and avoidance of subsequent interhospital transfers were also repeatedly noted as factors influencing hospital selection. Several EMS participants perceived that “certain hospitals don't have adequate PM staff” or provided “poor care” for certain types of patients. Providers will often attempt to match patient needs to hospital resources.
The Culture of Field Triage
Out-of-hospital providers repeatedly noted that the culture of trauma triage in this EMS system “encourages over-triage.” All participants stated there was little or no penalty to field providers for activating the trauma system for a patient that ultimately was found not to have serious injury. Multiple participants stated, “We tend to err on the side of caution.” The main disincentives for over-triage are personal, coming from physicians and nurses that may “question our judgment,” “roll their eyes,” or “grumble under their breath.” Alternatively, under-triage (i.e., transporting patients with serious injury to non-trauma centers) is strongly discouraged and penalized on multiple levels. If an apparent “trauma” patient is transported to a local non-trauma hospital, receiving staff may directly question the field provider, “Why did you come here?” EMS agency quality improvement processes and trauma committees track and may further penalize field providers for taking seriously injured patients to non-trauma hospitals. To minimize these occurrences, EMS providers tend to activate the trauma system for such patients.
Discussion
In this study, we explored out-of-hospital triage decisions, field cognitive reasoning and other factors affecting the distribution of injured patients transported in a well-established trauma system. While previous studies on cognitive reasoning in acute care settings have focused on reducing medical errors and understanding diagnostic reasoning,19-22 we evaluated cognitive processes as they apply to field triage and hospital selection in a regionalized trauma system. The current approach to trauma triage is assumed to follow an algorithmic, risk-based process for identifying patients with serious injuries, yet our results demonstrate that actual triage decision-making is complex and dynamic, relying on high-level cognition to generate rapid decisions. EMS provider “gut feeling” (provider judgment) had the greatest influence on identifying seriously injured patients in this system, a finding that was supported by both quantitative and qualitative study results. For injured patients not felt to have serious injuries, patient/family preference and proximity were the dominant factors in hospital selection, with modification by provider perceptions about hospital resources and quality of care. Our findings also demonstrate that a substantial number of injured patients not meeting field triage criteria are still transported to high-resource hospitals, most commonly based on patient/family preference (i.e., request).
This study demonstrates that out-of-hospital triage involves more independent thinking by field providers than has previously been understood. Studies assessing the utility of paramedic judgment in identifying seriously injured patients have shown mixed results.23-27 However, the cognitive processes behind such “judgment” have not been previously described. As opposed to the current algorithmic model for identifying seriously injured patients,6,7 we demonstrate that the cognitive processes for arriving at this determination are fast, intuitive, heuristic, and based largely on early scene information and visual cues, rather than specific criteria. Early information, often obtained and processed before patient contact, feeds the cognitive reasoning process, while information that cannot be assessed with rapid visual or auditory assessment (e.g., blood pressure, heart rate, respiratory rate, non-obvious anatomic injuries, detailed history) is generally not part of the primary triage decision-making process. This type of decision-making model has been termed “System 1” by Croskerry,28,29 with thought processes similar to experienced clinicians,19,20,22,28 and illustrates a form of “forward thinking” where a provisional hypothesis is rapidly formed (e.g., by dispatch information), then quickly tested with a smaller number of data points (e.g., visual cues from the scene) that allows the provider to expedite care.22 In the frequently chaotic and time-constrained environment of out-of-hospital care, quick decision-making and efficient critical thinking are rewarded and reflected in these cognitive processes. While the System 1 model of diagnostic reasoning can occasionally fail, “sometimes catastrophically,”28 this risk is accommodated by a trauma system culture that accepts high rates of over-triage. EMS provider judgment is included as a triage criterion in the most recent version of the ACSCOT Field Decision Scheme, referred to as “EMS Provider Judgment.”6,7
When there is not an immediate “gut feeling” regarding serious injury, EMS providers move into a “System 2” decision-making approach using a slower, deductive process based on additional data and more time-consuming, analytic cognitive functions.20,28 Our findings suggest that such “gray area” cases using System 2 processes are relatively uncommon and present impractical scenarios in a setting that favors rapid decision-making and short time intervals. When System 1 and 2 processing suggest no serious injuries, patient preference for hospital selection is given priority. While patient autonomy is minimized in patients believed to have serious injury, it is otherwise maximized similar to medical decision-making that weighs outcomes according to patient preference and satisfaction.
Our findings are notable because the ACSCOT Field Triage Decision Scheme, which has been used as the basis for field trauma triage in most U.S. trauma systems since 1987, was generally replaced by higher level decision-making among EMS providers. Although the field triage guidelines are comprehensive and sensible from a scientific perspective, the algorithmic format does not match the flow of information to field providers and does not cater to the fast, heuristic cognitive processes favored in the out-of-hospital setting. Providers in this system tend to proceed through the Field Triage Decision Scheme in generally reverse order, starting with EMS provider judgment (integrated with mechanism of injury and visual cues from the scene), then anatomic criteria (i.e., by physical exam, unless these injuries were apparent by visual assessment), and vital signs. These findings suggest that small modifications to individual triage criteria (e.g., the exact height of a fall or the specific Glasgow Coma Scale (GCS) value) may have little impact on triage processes, particularly among experienced out-of-hospital providers. Field provider insights and perceptions about patient needs and hospital resources (or lack thereof) also appear to play a role in hospital selection. Our findings suggest that provider perceptions about the availability, quality, staffing, cost, and comprehensiveness of hospital care can influence hospital selection for some patients. In addition, hospital proximity is an important factor, which may explain why hospitals that reside in areas with heavier EMS call volumes may see larger volumes of patients.
Provider intuition in this system is based on training and previous experience. While we did not assess the amount of experience needed to reach this level of intuition, there is likely some point at which EMS providers transition from a “learner” model requiring proscribed algorithms and highly structured protocols to more experienced providers with higher-level, faster, and less algorithmic decision-making. David and Brachet evaluated the relationship between EMS work experience, volume of trauma patients cared for (both recent and cumulative), and out-of-hospital time intervals (a proxy for provider performance).30 These authors found that more than two years of field experience, plus past and recent volume of trauma patients were all associated with reductions in out-of-hospital time.30 While the highly structured format of the ACSCOT Field Triage Decision Scheme appears to work well for learners, more experienced providers in this system use cognitive processes that match the flow of information, integrate provider experience and yield rapid, intuitive decision-making.
Our sample was limited to patients and EMS providers from a single trauma system. While this region includes urban, suburban, and some rural areas, most patients presented within reasonable proximity to a major trauma center. The decision-making process and order of priorities may be different in settings far from major trauma centers (e.g., rural or frontier regions), in regions where trauma resources are more constrained, or where EMS systems and respective protocols are inherently different. In addition, we did not assess other out-of-hospital decision-making topics, such as when to activate air medical transport from the scene. In this 4-county sample, only a small proportion of patients (0.1%) were transported from the scene by helicopter.
EMS provider experience surfaced as an important aspect of cognitive processing for trauma triage, however we did not collect information on provider experience. It is possible that the EMS crews participating in interviews were generally more experienced, which was reflected in development of the cognitive model. However, less experienced EMS personnel (e.g., first-year EMS personnel) were included in the field observation and interview process, particularly among the fire crews interviewed. Because the more senior EMS providers on-scene tend to guide the trauma triage process, we believe our findings are representative of actual field decision-making processes, where teams of EMS providers have a mix of experience levels. EMS systems or regions with fewer personnel on-scene or operating with less experienced providers may behave differently.
Finally, this study was designed to assess the process of out-of-hospital triage and hospital selection, rather than outcomes or the accuracy of such cognitive processing, though studies addressing these questions have been published.23-27 We do note that the survival benefit of this trauma system, as well as the effective redistribution of seriously injured patients with trauma system implementation, have been previously demonstrated.3,4 Additional studies to further explore the predictive value of EMS provider “gut feeling” relative to other triage criteria in identifying seriously injured patients are underway.
In summary, we derived an empirical, out-of-hospital cognitive reasoning model of trauma triage decision-making rooted in provider intuition, experience, and early informative cues. In this system, EMS provider judgment was the most frequently cited criteria for entering patients into the trauma system, a finding what was consistent with qualitative results from interviews and focus groups. For patients not felt to have serious injuries, patient/family preference and hospital proximity were the most important factors in selecting hospitals. It will be important to replicate this study in other EMS and trauma systems to assess whether the cognitive processing demonstrated here is similar in other systems. Understanding the flow of information to field providers, cognitive processing, consumer choice, and geographic location is likely critical in further modifying the regional distribution of injured patients and other persons with high-acuity clinical conditions served by EMS providers.
Acknowledgments
This project was supported by a grant from the Robert Wood Johnson Foundation Physician Faculty Scholars Program and the Oregon Clinical and Translational Research Institute (grant number UL1 RR024140) from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Dr. Somnath Saha is supported by the Department of Veterans Affairs.
Appendix 1. Field interview script for determining the process of out-of-hospital trauma triage and hospital transport decisions*
-
I'm interested in the process of trauma triage from the field perspective. What can you tell me about it?
Utility of overall vs. specific criteria (are they useful? do they work? which criteria are most useful? which are least useful?)
Complexity of use in the field (how do you use them? simple or complicated?)
Timing (at what point in field care is the triage decision made?)
Discretionary entries (how do you decide to enter a patient into the trauma system that doesn't meet specific criteria?)
Changes (If you could, what changes would you make in the trauma triage process? What aspects do you dislike about the triage process or specific criteria? Why?)
Mis-triage (how does under- vs. over-triage influence your decision making? Are there consequences for transporting injured patients to the wrong hospital?)
-
For injured patients that need to be transported, how do you select a hospital?
Trauma system entry (Is hospital selected before or after the decision to enter into the trauma system?)
Trauma center vs. non-trauma center (For patients not meeting specific criteria, how do you decide to use the “discretionary” entry criteria? When do you transport non-trauma system patients to trauma centers?)
Type of patient (e.g., homeless, intoxicated, other medical problems)
Patient requests (how is patient request factored into transport decisions? Family requests?)
Proximity (how does proximity to a given hospital affect transport decision?)
ED diversion (do you ever enter patients in the trauma system to bypass ED diversion status?)
Specific ED factors (friendliness of staff, food or drink availability, place to chart, other amenities? do these factors differ between trauma centers? Between other hospitals?)
Fire vs. ambulance personnel (who decides which hospital? Is it a joint/team decision?)
-
What are the most important factors that influence transport decisions?
Patient (clinical factors, requests)
Family
Protocols (e.g., trauma system criteria)
ED/hospital specific (are there specific hospitals you enjoy transporting to? That you try to avoid? Why?)
Proximity, traffic, duration of transport
Ambulance or trauma diversion
Other
Footnotes
Questions were intentionally broad to promote conversation. Specific “probes” are listed under each question to prompt further discussion if not touched upon otherwise during conversation. ED = emergency department.
Presentations: An abstract of this project was presented at the 2009 Society for Academic Emergency Medicine Annual Meeting in New Orleans, LA (May 2009).
Contributor Information
Craig D. Newgard, Email: newgardc@ohsu.edu.
Maria J. Nelson, Email: nelsomar@ohsu.edu.
Michael Kampp, Email: kamppm@ohsu.edu.
Somnath Saha, Email: sahas@ohsu.edu.
Dana Zive, Email: zived@ohsu.edu.
Terri Schmidt, Email: schmidtt@ohsu.edu.
Mohamud Daya, Email: dayam@ohsu.edu.
Jonathan Jui, Email: jui@ohsu.edu.
Lynn Wittwer, Email: wittwermpd@iinet.com.
Craig Warden, Email: wardenc@ohsu.edu.
Ritu Sahni, Email: sahnir@ohsu.edu.
Mark Stevens, Email: Mark.Stevens@tvfr.com.
Kyle Gorman, Email: kylegor@ccfd1.com.
Karl Koenig, Email: karlfoe@ccfd1.com.
Dean Gubler, Email: dgubler@lhs.org.
Pontine Rosteck, Email: Pontine.Rosteck@amr.net.
Jan Lee, Email: Janl@metrowest.fm.
Jerris R. Hedges, Email: jerris@hawaii.edu.
References
- 1.Committee on the Future of Emergency Care in the United States Health System, Board on Health Care Services. Institute of Medicine of the National Academies. Future of Emergency Care Series: Hospital-Based Emergency Care, At the Breaking Point. The National Academy Press; Washington, D.C.: 2006. [Google Scholar]
- 2.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. NEJM. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 3.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 4.Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40:536–545. doi: 10.1097/00005373-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage. MMWR. 2009;58:1–35. [PubMed] [Google Scholar]
- 8.Norcross ED, Ford DW, Cooper ME, et al. Application of American College of Surgeons' field triage guidelines by pre-hospital personnel. J Am Coll Surg. 1995;181:539–544. [PubMed] [Google Scholar]
- 9.Lerner EB. Studies evaluating current field triage: 1966-2005. Out-of-hospital Emergency Care. 2006;10:303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 10.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 11.Wang NE, Saynina O, Kuntz-Duriseti K, Mahlow P, Wise PH. Variability in pediatric utilization of trauma facilities in California: 1999 to 2005. Ann Emerg Med. 2008;52:607–615. doi: 10.1016/j.annemergmed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Committee on the Future of Emergency Care in the United States Health System, Board on Health Care Services. Institute of Medicine of the National Academies. Future of Emergency Care Series: Emergency Medical Services, At the Crossroads. The National Academy Press; Washington, D.C.: 2006. [Google Scholar]
- 13.U.S. Census Bureau – State and County Quickfacts. [last accessed January 16, 2011]; http://quickfacts.census.gov/qfd/index.html.
- 14.Dawson DE. National Emergency Medical Services Information System (NEMSIS) Prehosp Emerg Care. 2006;10:314–6. doi: 10.1080/10903120600724200. [DOI] [PubMed] [Google Scholar]
- 15.Jaro MA. Probabilistic linkage of large public health data files. Statistics in Medicine. 1995;14:491–498. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 16.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 17.Miles MB, Huberman M. Qualitative Data Analysis: An Expanded Sourcebook. 2nd. Thousand Oaks, CA: Sage; 1994. SAGE Publications. [Google Scholar]
- 18.Giacomini MK, Cook DJ. User's guides to the medical literature XXIII. Qualitative Research in Health Care, A. Are the results of the study valid? JAMA. 2000;284:357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 19.Coderre S, Mandin H, Harasym PH, Fick GH. Diagnostic reasoning strategies and diagnostic success. Medical Education. 2003;37:695–703. doi: 10.1046/j.1365-2923.2003.01577.x. [DOI] [PubMed] [Google Scholar]
- 20.Sandu H, Carpenter C. Clinical decisionmaking: opening the black box of cognitive reasoning. Ann Emerg Med. 2006;48:713–719. doi: 10.1016/j.annemergmed.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Gallagher EJ. Thinking about thinking. Ann Emerg Med. 2003;41:121–122. doi: 10.1067/mem.2003.20. [DOI] [PubMed] [Google Scholar]
- 22.Young JS, Smith RL, Guerlain S, Nolley B. How residents think and make medical decisions: implications for education and patient safety. The American Surgeon. 2007;73:548–553. doi: 10.1177/000313480707300604. [DOI] [PubMed] [Google Scholar]
- 23.Mulholland SA, Gabbe BJ, Cameron P. Is paramedic judgment useful in prehospital trauma triage? Injury, Int J Care Injured. 2005;36:1298–1305. doi: 10.1016/j.injury.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Mulholland SA, Cameron PA, Gabbe BJ, et al. Prehospital prediction of the severity of blunt anatomic injury. J Trauma. 2008;64:754–760. doi: 10.1097/01.ta.0000244384.85267.c5. [DOI] [PubMed] [Google Scholar]
- 25.Fries GR, McCalla G, Levitt MA, Cordova R. A prospective comparison of paramedic judgment and the trauma triage rule in the prehospital setting. Ann Emerg Med. 1994;24:885–889. doi: 10.1016/s0196-0644(94)70207-1. [DOI] [PubMed] [Google Scholar]
- 26.Simmons E, Hedges JR, Irwin L, Maassberg W, Kirkwood HA. Paramedic injury severity perception can aid trauma triage. Ann Emerg Med. 1995;26:461–468. doi: 10.1016/s0196-0644(95)70115-x. [DOI] [PubMed] [Google Scholar]
- 27.Qazi K, Kempf JA, Christopher NC, Gerson LW. Paramedic judgment of the need for trauma team activation for pediatric patients. Acad Emerg Med. 1998;5:1002–1007. doi: 10.1111/j.1553-2712.1998.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 28.Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84:1022–1028. doi: 10.1097/ACM.0b013e3181ace703. [DOI] [PubMed] [Google Scholar]
- 29.Croskerry P. Critical thinking and decisionmaking: avoiding the perils of thin-slicing. Ann Emerg Med. 2006;48:720–722. doi: 10.1016/j.annemergmed.2006.03.030. [DOI] [PubMed] [Google Scholar]
- 30.David G, Brachey T. Retention, learning by doing, and performance in emergency medical services. Health Services Research. 2009;44:902–925. doi: 10.1111/j.1475-6773.2009.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]