Abstract
Background
Wet cupping is a traditional Chinese medicine therapy commonly used in treating herpes zoster in China, and clinical studies have shown that wet cupping may have beneficial effect on herpes zoster compared with western medication.
Methods
We included randomized controlled trials on wet cupping for herpes zoster. We searched PubMed, the Cochrane Library (Issue 3, 2008), China Network Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), and Wan Fang Database. All searches ended in February 2009. Two authors extracted data and assessed the trials quality independently. RevMan 5.0.18 software was used for data analysis with effect estimate presented as relative risk (RR) and mean difference (MD) with a 95% confidence interval (CI).
Results
8 RCTs involving 651 patients were included, and the methodological quality of trials was generally fair in terms of randomization, blinding and intention-to-treat analysis. Meta-analyses showed wet cupping was superior to medications regarding the number of cured patients (RR 2.49, 95%CI 1.91 to 3.24, p<0.00001), the number of patients with improved symptoms (RR 1.15, 95%CI 1.05 to 1.26, p=0.003), and reducing the incidence rate of postherpetic neuralgia (RR 0.06, 95%CI 0.02 to 0.25, p=0.0001). Wet cupping plus medications was significantly better than medications alone on number of cured patients (RR 1.93, 95%CI 1.23 to 3.04, p=0.005), but no difference in symptom improvement (RR 1.00, 95%CI 0.92 to 1.08, p=0.98). There were no serious adverse effects with related to wet cupping therapy in the included trials.
Conclusions
Wet cupping appears to be effective in treatment of herpes zoster. However, further large, rigorous designed trials are warranted.
Background
Herpes zoster, commonly with the pain and rush on skin, is caused by the infection of latent varicella zoster virus (VZV). VZV usually persists asymptomatically in the dorsal root ganglia of anyone who has had chickenpox, reactivating from its dormant state in about 25% of people to travel along the sensory nerve fibres and cause vesicular lesions in the dermatome supplied by the nerve[1]. The classical clinical presentation of herpes zoster starts with a mild-to-moderate burning or tingling in or under the skin of a given surface, often accompanied by fever, chills, headache, stomach upset and general malaise. The pain associated with shingles varies in intensity from mild to severe, the lesions usually begin to dry and scab 3–5 days after appearing. Total duration of the disease is generally between 7–10 days, and the most common complication associated with herpes zoster is the development of postherpetic neuralgia (PHN), a condition where pain accompanying the rash persists long after the lesions have healed.
Herpes zoster has a high infection rate, which is increasing by years. Some studies showed that the infection rate of herpes zoster and the intensity of the pain were relative with age, and the elderly were at greater risk for developing this disease. Early treatment can be more effective to release the pain and reduce the duration of disease [2]. The objective of conventional therapy in the treatment of herpes zoster is to accelerate the healing of the lesions, reduce the accompanying pain, and prevent complications. Medications typically prescribed included antiviral agents, corticosteroids, analgesics, non-steroidal anti-inflammatory drugs, and tricyclic antidepressants [3].
In Traditional Chinese Medicine, herpes zoster is called She Chuan Chuang, its pathological mechanism is insufficient of anti-pathogenic energy, toxin invades the body and transformation into heat, damp-heat spreading to the skin; or is stagnation of liver qi, and extreme heat generate wind, the fire depressed in skin; or is damp-heat in spleen and stomach, and spreading to the skin [2]. The treatment including herbal decoction, Chinese formulated products, acupuncture, moxibustion, cupping therapy and so on.
Cupping therapy is a method mainly using horn, bamboo or glass cups on patients’ skin by creating minus pressure inside the cups, which exerts as an approach for diagnosis, treatment and prevention of diseases [4]. There are many types of cupping therapy, but 8 types of cupping are commonly used in clinical practice, i.e., empty cupping, moving cupping, retained cupping, needle cupping, moxa cupping, wet cupping, herbal cupping and water cupping [5]. Wet cupping, also called full (bleeding) cupping, was the most favored and practiced cupping method of all by the early practitioners, who particularly in Europe, employed the Bleeding cupping technique in order to purge foul blood, which was considered the source of disease, from the body. It can be used in the treatment of a sudden increase in blood pressure, and in discharging pus from boils and furuncles, which represents excess, with blood-heat and stagnation. Sterilize the selected points with alcohol and make a very small incision with a triangle-edged needle or, using a plum-blossom needle, firmly tap the point for a short time to cause bleeding. Once the point is bled, choose a cup and apply a strong cupping method to the point. The blood will quite quickly be observed being drawn slowly into the cup. If the incision is sufficient, blood with about 30–60 ml can be expected to be drawn into the cup. Remove the cup after 5 or 10 minutes with attention and care. Cupping regulates the flow of qi and blood. It helps to draw out and eliminate pathogenic factors such as damp and heat. Cupping also moves qi and blood and opens the pores of the skin, thus precipitating the removal of pathogens through the skin itself [6].
From literature, we found some clinical trial reports on wet cupping therapy for herpes zoster, but there is no systematic review about the therapeutic effect of the therapy. Therefore, this review aims to evaluate the beneficial and harmful effects of wet cupping therapy for treatment of herpes zoster in randomized trials.
Methods
Inclusion Criteria
Parallel randomized controlled trials (RCTs) of wet cupping compared with no treatment, placebo or basic medical therapy in patients with herpes zoster and PHN were included. Combined therapy of wet cupping and other interventions compared with other interventions in RCTs was also included. Outcome measures include reductions in severity of pain, duration of relief of pain, percentage of cured patients and the incidence rate of PHN. Multiple publications reporting the same groups of participants were excluded. Combined therapy of wet cupping and acupuncture compared with medication or other interventions except acupuncture was also excluded. There was no limitation on language and publication type.
Identification and selection of studies
We searched China Network Knowledge Infrastructure (CNKI) (1979–2009), Chinese Scientific Journal Database VIP (1989–2009), Wan Fang Database (1985–2009), PubMed (1966–2009) and the Cochrane Library (Issue 3, 2008), all the searches ended at February 2009. The search terms included “post-herpetic neuralgia”, “PHN”, “herpes zoster”, “zona”, or “shingles” combined with “venesection”, “phlebotomy therapy”, “three edged needle”, “triangle-edged needle”, “ventouse”, “cupping” or “blood-letting”. Two authors (HJ Cao and CJ Zhu) selected studies for eligibility and checked against the inclusion criteria independently.
Data extraction and quality assessment
Two authors (HJ Cao and CJ Zhu) extracted the data from the included trials independently. Quality of the included trials was evaluated according to following categories [7]. Category A (good): studies have the least biases and their results are considered valid. These studies are likely to consist of (1) clear description of the population, setting, interventions and comparison groups; (2) appropriate measurement of outcomes; (3) appropriate statistical and analytical methods; (4) no reporting errors; (5) less than 20 percent dropouts; (6) clear reporting of dropouts; and (7) appropriate consideration and adjustment for potential confounders. Category B (fair): studies are susceptible to some degrees of biases that are not sufficient to invalidate the results. These studies may have sub-optimal adjustments for potential confounders and may also lack certain information that is needed to assess limitations and potential problems. Category C (poor): studies have significant biases which may invalidate the results. These studies either do not consider potential confounders or do not make adjustments for them appropriately. These studies may have critical flaw in design, analysis and/or reporting, missing information and/or discrepancies in reporting.
Data analysis
Data were summarized using relative risk (RR) with 95% confidence intervals (CI) for binary outcomes or mean difference (MD) with 95% CI for continuous outcomes. Revman5.0.18 software was used for data analyses. Meta-analysis was used if the trials had a good homogeneity on study design, participants, interventions, control, and outcome measures. Publication bias was explored by funnel plot analysis.
Results
Description of studies
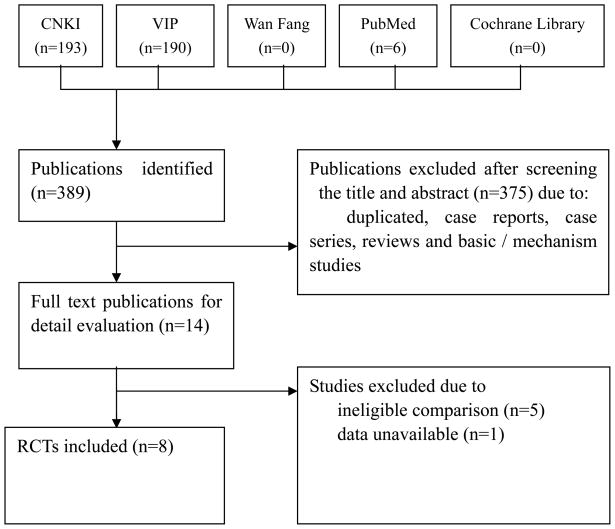
After primary searches from seven databases, 389 citations were identified, and the majority was excluded due to obvious ineligibility, and full text papers of 14 studies were retrieved. At last, 8 [8–15] trials were included in this review, 5 trials [16–20] were excluded as they used wet cupping therapy combined with acupuncture or moxibustion compared with other medications, 1 trial [21] was excluded due to the ineligible data reporting (Figure 1: The process of including and excluding studies). The characteristics of included and excluded trials were listed in Table 1 (Characteristics of included studies) and Table 2 (Studies excluded from the review and reasons for exclusion).
Figure 1.
The process of including and excluding studies
Table 1.
Characteristics of included studies
| Trials | Patients (M/F) | Average age (y) | Diagnostic criteria | Interventions | Duration of treatment | Outcome measure | ||
|---|---|---|---|---|---|---|---|---|
| treatment | control | Cupping treatment | Control | |||||
| Guo L 2006 [8] | 19/17 | 17/18 | unclear | Chinese criteria for diagnosis | Prick with triangle-edged needle and cupping on lesion for 10 minutes, once every two days, plus aciclovir 200mg 3 times daily, VitB1 100mg, VitB12 250mg injection once daily. | Aciclovir 200mg 3 times daily, VitB1 100mg, VitB12 250mg injection once daily. | 10 days | * Cure, improve, ineffective; average time of cure. |
| Jin M 2008 [9] | 26/19 | 25/20 | 55.5 | Professional criteria in China | Prick with seven-star needle and cupping on the lesion for 10–15min, once daily for first 3 days, then once every two days and last for 4 days | Aciclovir capsule 0.2g five times daily, cimetidine 0.2g three times daily, indometacin tablet 50mg three times daily, Mecobalamin tablets 0.5mg three times daily, washout with calamin and use aciclovir cream | 10 days |
* Cure, improve, ineffective. Incidence rate of postherpetic neuralgia (PHN) |
| Lin L 2003 [10] | 28/22 | 19/15 | 55.1 | Criteria in text book in China | Group1: prick with plum needle on lesion then cupping on the same place for 10–15min, once every two days, plus aciclovir 0.2g five times daily, VitB1 20mg three times daily, VB12 500mg injection once every two days, 2%–3% aciclovir cream for external use. | Aciclovir 0.2g five times daily, VitB1 20mg three times daily, VB12 500mg injection once every two days, 2%–3% aciclovir cream for external use. | 10 days |
** cure, markedly effective, effective, ineffective. The average time of cure. Incidence rate of PHN. |
| 16/14 | 19/15 | 54.2 | Group 2: prick with plum needle on lesion then cupping on the same place for 10–15min, once every two days. | Aciclovir 0.2g five times everyday, VitB1 20mg three times everyday, VB12 500mg injection once every two days, 2%–3% aciclovir cream for external use. | ||||
| Liu Q 2004 [11] | 32 | 32 | 55.6 | unavailable | Prick with triangle-edged needle and cupping on lesion. | Aciclovir 1.2g five times everyday, poly I-C injection 2mg once every two days. | 10 days | ** cure, markedly effective, effective, ineffective. |
| Long W 2003[12] | 34 | 30 | 44.5 | unavailable | Prick with plum needle on lesion then cupping on the same place plus ultraviolet radiation once every two days. | Ultraviolet radiation once every two days. | 10 days | Times of treatment for * cured |
| Xiong Z 2007[13] | 20/28 | 16/24 | 49 | Criteria in text book in China | Prick on lesion and cupping for 5 minutes. | Aciclovir plus normal saline 250ml intravenous drip once daily. | 7 days | Incidence rate of PHN. |
| Xu L 2004 [14] | 20/20 | 21/19 | unclear | unavailable | Prick with triangle-edged needle and cupping on lesion for 15min, aciclovir cream for external use plus aciclovir 0.5g and glucose 250ml intravenous drip twice daily. | Aciclovir cream for external use plus aciclovir 0.5g and glucose 250ml intravenous drip twice daily. | 7 days |
* cure, improve, effective, ineffective. Scores given by patients according to their symptom of disease. Average dry up time of lesion; average time of pain disappear |
| Zhang Q 2008[15] | 14/26 | 12/28 | unclear | Criteria in text book in China | Aciclovir 200mg five times daily, acupuncture beside the lesion 30min once daily, plus prick with triangle-edged needle on Dazhui, Feishu (double), Ganshu (double) and cupping for 10min once every two days, blood-letting on auditive apex twice every week | Aciclovir 200mg five times daily, acupuncture beside the lesion 30min once daily | 14 days | * cure, improve, effective, ineffective. |
Definition of “cure”, “markedly effective “, “effective”, and “ineffective”:
cure: rush totally faded, the clinical symptoms are disappeared, no accompanying pain.
markedly effective: rush faded more than 70% (including 70%), the accompanying pain was almost disappeared.
improved: rush faded 30%–69%, the accompanying pain was obviously alleviated.
ineffective: rush faded less than 30%, no alleviation of the accompanying pain.
cure: rush totally fade, no accompanying pain.
markedly effective: rush faded more than 50%, the accompanying pain was almost disappeared.
effective: rush faded 10%–50%, the accompanying pain was alleviated a little.
ineffective: rush faded less than 10%, no alleviation of the accompanying pain.
Table 2.
Studies excluded from the review and reasons for exclusion
| Study | Reasons for exclusion |
|---|---|
| Cai P 2006[16] | Randomized controlled trial (RCT) which used wet cupping therapy combined with acupuncture compared with western medications |
| Huo H 2007[17] | RCT which used wet cupping therapy combined with acupuncture and needle prick round the rush compared with western medications |
| Luo S 2008[18] | RCT which used wet cupping therapy combined with moxibustion compared with western medications |
| Pang S 2003[19] | RCT which used wet cupping therapy combined with needle prick round the rush compared with western medications |
| Wang H 2007[20] | RCT which used wet cupping therapy combined with acupuncture compared with western medications |
| Zhang J 2004[21] | RCT but data were not available for analysis due to inadequate reporting |
The 8 trials involved a total of 651 patients with herpes zoster. The variation in the age of subjects was 12–82 years and disease duration was from 1 day to 14 days. Five trials specified four diagnostic criteria, including two criteria in different kind of text books in China, two national criteria in China. The interventions included wet cupping therapy (prick on lesion with triangle-edged needle, plum needle, or seven-star needle), wet cupping therapy plus conventional medications or acupuncture. The controls included medications or acupuncture. The total treatment duration ranged from 7 days to 10 days. All the included trials used two, three or four of four classes to evaluate treatment effects including cure, markedly effective, effective/improve, and ineffective according to the degree of overall symptom improvement.
Methodological quality
According to our pre-defined quality assessment criteria, all the included trials had clear description of the population, setting, interventions and comparison groups, appropriate statistical and analytical methods, the sample size varied from 30 to 50 participants, with average of 43 patients per group, though none of the trials reported sample size calculation, method for allocation concealment and blinding. Two trials [8, 9] described the randomization procedure, using random number table, and drawing. All the included trials chose the improvement of the symptoms as the outcome measurement, but whether the assessors of outcome were blinding were not reported in all the 8 trials. There was no participant dropped during all the studies, only two trials [9, 13] mentioned follow-up, but intention-to-treat was not used. No trials had appropriate consideration and adjustment for potential confounders. It has high potential to have some degrees of biases that are not sufficient to invalidate the results, so we generally concluded that all the 8 trials (100%) were evaluated as fair (B).
Effect estimates (Table 3: Effect of estimates of wet cupping treatment in 8 RCTs)
Table 3.
Effect of estimates of wet cupping treatment in 8 RCTs
| Trials | Comparisons | Effect Estimates( [95%CI]) | P Value | |
|---|---|---|---|---|
| 3.1 Numbers of cured patients | ||||
| 3.1.1 wet cupping plus other interventions versus other interventions alone | ||||
| Guo L 2006[8] | Wet cupping plus aciclovir, VitB1, VitB12 versus aciclovir, VitB 1, VitB12 | RR | 1.48 [1.05, 2.09] | |
| Liu L 2003[10] | Wet cupping plus aciclovir, VitB1, VitB12 and aciclovir cream versus aciclovir, VitB1, VitB12 and aciclovir cream | RR | 3.83 [2.07, 7.06] | |
| Long W 2003[12] | Wet cupping plus ultraviolet radiation versus ultraviolet radiation alone | RR | 1.30 [1.06, 1.59] | |
| Xu L 2004[14] | Wet cupping plus aciclovir cream, aciclovir 0.5g and glucose 250ml intravenous drip versus aciclovir cream, aciclovir 0.5g and glucose 250ml intravenous drip | RR | 1.35 [0.93, 1.97] | |
| Zhang Q 2008[15] | Wet cupping and blood-letting on auditive apex plus aciclovir and acupuncture versus aciclovir and acupuncture | RR | 4.17 [1.92, 9.05] | |
| meta-analysis | RR | 1.93 [1.23, 3.04]* | 0.005 | |
| 3.1.2 wet cupping versus medications | ||||
| Jin M 2008[9] | Wet cupping versus aciclovir, cimetidine, indometacin, mecobalamin, calamin and aciclovir cream. | RR | 2.15 [1.54, 3.00] | |
| Liu L 2003[10] | Wet cupping versus aciclovir, VitB1, VitB12 and aciclovir cream | RR | 2.83 [1.47, 5.46] | |
| Liu Q 2004[11] | Wet cupping versus aciclovir and poly I-C injection | RR | 2.90 [1.71, 4.91] | |
| meta-analysis | RR | 2.49 [1.91, 3.24] | <0.00001 | |
| 3.2 Numbers of patients with PHN after treatment | ||||
| Jin M 2008[9] | Wet cupping versus aciclovir, cimetidine, indometacin, mecobalamin, calamin and aciclovir cream. | RR | 0.09 [0.01, 1.60] | |
| Liu L 2003[10] | Wet cupping versus aciclovir, VitB1, VitB12 and aciclovir cream | RR | 0.06 [0.00, 1.09] | |
| Xiong Z 2007[13] | Wet cupping versus aciclovir plus normal saline 250ml intravenous drip | RR | 0.05 [0.01, 0.38] | |
| meta-analysis | RR | 0.06 [0.02, 0.25] | 0.0001 | |
| 3.3 Numbers of patients with improved symptom after treatment | ||||
| 3.3.1 wet cupping plus other interventions versus other interventions alone | ||||
| Guo L 2006[8] | Wet cupping plus aciclovir, VitB1, VitB12 versus aciclovir, VitB1, VitB12 | RR | 1.00 [0.92, 1.08] | |
| Liu L 2003[10] | Wet cupping plus aciclovir, VitB1, VitB12 and aciclovir cream versus aciclovir, VitB1, VitB12 and aciclovir cream | Not estimable | ||
| Xu L 2004[14] | Wet cupping plus aciclovir cream, aciclovir 0.5g and glucose 250ml intravenous drip versus aciclovir cream, aciclovir 0.5g and glucose 250ml intravenous drip | Not estimable | ||
| Zhang Q 2008[15] | Wet cupping and blood-letting on auditive apex plus aciclovir and acupuncture versus aciclovir and acupuncture | Not estimable | ||
| meta-analysis | RR | 1.00 [0.92, 1.08] | 0.98 | |
| 3.3.2 wet cupping versus medications | ||||
| Jin M 2008[9] | Wet cupping versus aciclovir, cimetidine, indometacin, mecobalamin, calamin and aciclovir cream. | RR | 1.07 [0.98, 1.17] | |
| Liu L 2003[10] | Wet cupping versus aciclovir, VitB1, VitB12 and aciclovir cream | Not estimable | ||
| Liu Q 2004[11] | Wet cupping versus aciclovir and poly I-C injection | RR | 1.27 [1.05, 1.54] | |
| meta-analysis | RR | 1.15 [1.05, 1.26] | 0.003 | |
| 3.4 Average cure time | ||||
| 3.4.1 wet cupping plus other interventions versus other interventions alone | ||||
| Guo L 2006[8] | Wet cupping plus aciclovir, VitB1, VitB12 versus aciclovir, VitB1, VitB12 | MD | −2.10 [−3.55, −0.65] | |
| Liu L 2003[10] | Wet cupping plus aciclovir, VitB1, VitB12 and aciclovir cream versus aciclovir, VitB1, VitB12 and aciclovir cream | MD | −5.08 [−8.04, −2.12] | |
| meta-analysis | MD | −2.67 [−3.97, −1.37] | <0.0001 | |
| 3.4.2 wet cupping versus medications | ||||
| Liu L 2003[10] | Wet cupping versus aciclovir, VitB1, VitB12 and aciclovir cream | MD | −3.14 [−6.45, 0.17] | 0.06 |
RR: Relative Risk MD: Mean Difference CI: Confidence Interval
: Random model for data analysis
Wet cupping versus medications
Four trials [9–11, 13] compared wet cupping with medications. Three of them [9–11] showed that wet cupping therapy was significantly better than medications on increasing the number of patients whose herpes zoster were cured (RR 2.49, 95%CI 1.91 to 3.24, p<0.00001), and also on increasing the number of patients whose symptom was improved after treatment (RR 1.15, 95%CI 1.05 to 1.26, p=0.003), though one trial’s result showed not estimable [10].
Three trials [9, 10, 13] reported the incidence rate of PHN after treatment. The meta-analysis showed that wet cupping therapy was significantly more effective to prevent the complications (RR 0.06, 95%CI 0.02 to 0.25, p=0.0001).
One trial [10] reported the average cure time, which showed no significant difference between wet cupping with medications (MD −3.14, 95%CI −6.45 to 0.17, p=0.06).
Wet cupping plus other interventions versus other interventions
Five trials [8, 10, 12, 14, 15] compared wet cupping therapy plus other interventions versus other interventions alone. Result of meta-analysis showed significant difference between wet cupping plus medications or ultraviolet radiation compared with the same interventions on increasing the numbers of patients whose herpes zoster were cured (RR 1.93, 95%CI 1.23 to 3.04, p=0.005). Four trials’ [8, 10, 14, 15] results about number of patients whose symptom was improved after treatment were also be synthesized, but three of them showed not estimable, only one trial [8] showed no positive result of this comparison (RR 1.00, 95%CI 0.92 to 1.08, p=0.98).
Two trials [8, 10] reported the average cure time, and the meta-analysis showed significant difference between wet cupping plus medications compared with medications alone on accelerating the time of cure (MD −2.67, 95%CI −3.97 to −1.37, p<0.0001).
Adverse effect
Outcome of adverse effect with related to wet cupping therapy was described in two trials [10, 13], but no adverse effect was observed in wet cupping group. One trial [13] reported one patient with diabetes had several depressed scars on lesion skin in aciclovir group (n=48).
As each comparisons included in this review had less than five trials, it was not meaningful to conduct a funnel plot analysis.
Discussions
Based on the meta-analyses, the results showed that compared with medications, wet cupping therapy was significant better on healing the lesions and reducing the accompanying pain, and the combination of other interventions appears more effective than those interventions alone, though it is possible that the beneficial effect from wet cupping was overvalued because of the small sample size, insufficient reporting of methodology of the included trials.
There are several limitations in this review. First, the quality of the included studies is generally fair, which may cause moderate risk of bias. Because of inadequate application of randomization and lack of blinding in majority trials, it was possible for potential performance bias and detection bias due to patients and researchers being aware of the therapeutic interventions for the subjective outcome measures. Intention-to-treat analysis was not applied in data analyses in the included trials. Though the funnel plot can not be generated due to the limited number of trials in the meta-analysis, all studies reported the positive result favoring the treatment group, it may have publication bias. Further more, all the included trials were published in Chinese, it may also affect the possibility of selection bias. Second, one trial [9] included only the middle-age and senile patients with herpes zoster, one trial [15] only included the patients with head-face herpes zoster, and there were different type of needles used in the trials, included triangle-edged needle in 4 trials, plum-blossom needle in 2 trials, filiform needle in 1 trials, and seven-star needle in 1 trial. Seven trials applied the pricking bloodletting on lesion of skin, 1 trial pricking and cupping on DU14, BL13, BL17, BL18 and bloodletting on ear apex. The variance of participates and the detail of interventions may create the heterogeneity among the included trials, and affect the meta-analysis of therapeutic effect. Forth, the use of composite outcome measures in 8 trials to evaluate overall improvement of symptoms limits the generalization of the findings. The classification of cure, markedly effective, effective or ineffective is not internationally recognized, and it is hard to interpret the effect. We suggest future trials to comply with international standards in the evaluation of treatment effect. Although there is not major statistical heterogeneity among the data analyses, we realized that the clinical heterogeneity would be very significant due to the variations in study quality, participants, intervention, control and outcome measures. The interpretation of the positive findings from the meta-analyses needs to be incorporated with the clinical characteristics of the included trials and evidence strength. Therefore, the conclusion of the beneficial effect of wet cupping therapy for herpes zoster needs to be confirmed in large and rigorously designed randomized controlled trials.
Our searches identified one review of acupuncture and cupping therapy for herpes zoster [22]. It published in Chinese in 2008 included 399 trials, and the purpose of that review was to assess the quality of literature of clinical studies on acupuncture and cupping therapy in treatment of herpes zoster. It reported that in all 399 trials, 86 trials only used acupuncture as the treatment intervention, and 187 of the left 313 trials used wet cupping therapy. It showed that as a very commonly used method in treating herpes zoster, wet cupping therapy combined with acupuncture may have more markedly effect. In our systematic review, we excluded 5 trials which used wet cupping therapy combined with acupuncture to treat herpes zoster compared with medications alone, but all the 5 excluded trials showed positive result of the therapeutic effect of interventions. Therefore the further rigorous trials are warranted to testify this conclusion.
Most of existing trials are of small size and some risk of bias. Further high quality studies of larger sample size are needed to confirm the effectiveness of wet cupping therapy in treating herpes zoster. Randomization methods need to be clearly described and fully reported. Although blinding of the patients and practitioners might be very difficult, blinding of outcome assessors should be attempted as far as possible to minimize performance and assessment biases. Choosing outcome measures should be according to the international standards, the continuous data may include change in average daily pain score from the baseline week to the final study week, measured on Visual Analogue Scale (VAS), Short Form-36 (SF-36) Quality of Life Questionnaire, Profile of Mood States (POMS), and the Present Pain Intensity (PPI) score [23], the binary outcomes may include the burden of illness due to herpes zoster, and the incidence of postherpetic neuralgia [24], et al. Analysis of outcomes based on intention-to-treat principle is important. In addition, well-defined diagnostic criteria should be employed to make a precise clinical diagnosis of herpes zoster, and hence increase the comparability between trials. In its classical manifestation, the signs and symptoms of zoster are usually distinctive enough to make an accurate clinical diagnosis once the rash has appeared, but in some cases, particularly in immunosuppressed persons, the location of rash appearance might be atypical, or a neurologic complication might occur well after resolution of the rash. In these instances, laboratory testing might clarify the diagnosis [25]. Reporting of trials should follow by the Consolidated Standards of Reporting Trials (CONSORT) [26] to explicitly explain the process of the treatment, so that the clinicians or other researchers can possibly practice. Since herpes zoster may wax and wane with or without treatment, and it may have complications such as postherpetic neuralgia, a longer follow-up period with serial measurement of outcomes is important to determine the effectiveness and long-term effect of wet cupping therapy.
Acknowledgments
Financial Support: National Basic Research Program of China (‘973’ Program, No. 2006CB504602) and the 111 Project (B08006).
HJ Cao and JP Liu were supported by a grant from the National Basic Research Program of China (‘973’ Program, No. 2006CB504602) and the 111 Project (B08006). JP Liu was in part supported by the Grant Number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM) of the US National Institutes of Health.
Footnotes
Potential conflict of interest
None known.
Contributor Information
Huijuan Cao, Beijing University of Chinese Medicine.
Chenjun Zhu, Beijing University of Chinese Medicine.
Jianping Liu, Director of Center for Evidence-Based Chinese Medicine of Beijing University of Chinese Medicine.
References
- 1.Wareham DW, Breuer J. Herpes zoster. BMJ. 2007;334(7605):1211–5. doi: 10.1136/bmj.39206.571042.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu XM, Zhu GM, Chen YL, Fang M, Chen YN. Systematic assessment of acupuncture for treatment of herpes zoster in domestic clinical studies [in Chinese] Chinese Acupuncture and Moxibustion. 2007;27(7):536–40. [PubMed] [Google Scholar]
- 3.Roxas M. Herpes zoster and postherpetic neuralgia: diagnosis and therapeutic considerations. Altern Med Rev. 2006;11(2):102–13. [PubMed] [Google Scholar]
- 4.Gao LW. Practical Cupping Therapy [in Chinese] Beijing: Academy Press; 2004. [Google Scholar]
- 5.Chirali IZ. The cupping procedure. In: Chirali IZ, editor. Traditional Chinese Medicine Cupping Therapy. London: Churchill Livingstone; 1999. pp. 73–86. [Google Scholar]
- 6.Chirali IZ. Benefits of cupping therapy. In: Chirali IZ, editor. Traditional Chinese Medicine Cupping Therapy. London: Churchill Livingstone; 1999. pp. 46–9. [Google Scholar]
- 7.Agency for Healthcare Research and Quality. doi: 10.7326/0003-4819-142-12_part_2-200506211-00012. [ http://www.Ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf] [DOI] [PubMed]
- 8.Guo LX. Observation of effect of prick with triangle-edged needle plus cupping therapy on herpes zoster [in Chinese] Shanxi Journal of Traditional Chinese Medicine. 2006;22(3):41. [Google Scholar]
- 9.Jin MZ, Xie ZQ, Chen XW, Chen DX, Chen DP. Observations on the efficacy of blood-letting puncture and cupping in treating middle-aged and senile herpes zoster [in Chinese] Shanghai Journal of Acupuncture and Moxibustion. 2008;27(3):20–1. [Google Scholar]
- 10.Liu L, Li ZL. Curative effect observation on treating herpes zoster by Zhong Xi Medicine [in Chinese] Chinese Journal of the Practical Chinese with Modern Medicine. 2003;3(16):2088–9. [Google Scholar]
- 11.Liu QW, Chang HS. Integrated traditional and western medicine for herpes zoster [in Chinese] Journal of External Therapy of Traditional Chinese Medicine. 2004;13(5):53. [Google Scholar]
- 12.Long WH, Liu H. 34 cases observation of combined therapy for herpes zoster [in Chinese] The Journal of Medical Theory and Practice. 2003;16(10):1170. [Google Scholar]
- 13.Xiong ZL, Zhang GH. Fire needle plus cupping therapy for 48 patients with acute herpes zoster [in Chinese] Journal of Clinical Acupuncture and Moxibustion. 2007;23(7):38–9. [Google Scholar]
- 14.Xu L. Therapeutic effect of aciclovir in combination with callateral-puncturing and cupping in the treatment of 40 cases of herpes zoster [in Chinese] Tianjin Pharmacy. 2004;16(3):23–4. [Google Scholar]
- 15.Zhang Q, Liang XS, Guo TZ, Li TN. Observation on treatment of head-face herpes zoster [in Chinese] Liaoning Journal of Traditional Chinese Medicine. 2008;35(4):602. [Google Scholar]
- 16.Cai P. Clinical observation of collateral puncturing and cupping therapy on treatment of lumbar herpes zoster [in Chinese] Liaoning Journal of Traditional Chinese Medicine. 2006;33(4):476. [Google Scholar]
- 17.Huo HM, Yang XP. Observation on therapeutic effect of pricking blood therapy combined with acupuncture on herpes zoster [in Chinese] Chinese Acupuncture and Moxibustion. 2007;27(10):729–30. [PubMed] [Google Scholar]
- 18.Luo SX, Xie YL, Ji DY. Observation of therapeutic effect of collateral puncturing and cupping therapy combined with western medications on treatment of herpes zoster [in Chinese] Chinese Journal of Misdiagnosis. 2008;8(7):1579–80. [Google Scholar]
- 19.Pang SF, Bao JZ. Observation on the therapeutic effect of pricking blood, cupping and surround needling on herpes zoster in the plateau area [in Chinese] Chinese Acupuncture and Moxibustion. 2003;23(4):207–9. [Google Scholar]
- 20.Wang HL, Gao KB. 45 cases observation of surround needling and cupping on treatment of early herpes zoster [in Chinese] Traditional Chinese Medicine Research. 2007;20(12):47–8. [Google Scholar]
- 21.Zhang JW, Wang XL, Zhou SH. Clinical observation of therapeutic effect of aciclovir combined with acupuncture on treatment of 41 cases of herpes zoster [in Chinese] Chinese General Practice. 2004;7(16):1179–80. [Google Scholar]
- 22.Peng WN, Liu ZS, Deng YH, Mao M, Yu JN, Du Y. Evaluation of literature quality of acupuncture for treatment of herpes zoster and approach to the laws of treatment [in Chinese] Chinese Acupuncture and Moxibustion. 2008;28(2):147–50. [PubMed] [Google Scholar]
- 23.Rowbotham M, Harden N, Stacey B, Bernstein P, Miller LM the Gabapentin Postherpetic Neuralgia Study Group. Gabapentin for the treatment of postherpetic neuralgia. JAMA. 1998;280(21):1837–42. doi: 10.1001/jama.280.21.1837. [DOI] [PubMed] [Google Scholar]
- 24.Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, Weinberg A, Boardman KD, Williams HM, Zhang JH, Peduzzi PN, Beisel CE, Morrison VA, Guatelli JC, Brooks PA, Kauffman CA, Pachucki CT, Neuzil KM, Betts RF, Wright PF, Griffin MR, Brunell P, Soto NE, Marques AR, Keay SK, Goodman RP, Cotton DJ, Gnann JW, Jr, Loutit J, Holodniy M, Keitel WA, Crawford GE, Yeh SS, Lobo Z, Toney JF, Greenberg RN, Keller PM, Harbecke R, Hayward AR, Irwin MR, Kyriakides TC, Chan CY, Chan IS, Wang WW, Annunziato PW, Silber JL Shingles Prevention Study Group. . A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. The New England Journal of Medicine. 2005;352(22):2271–84. doi: 10.1056/NEJMoa051016. [DOI] [PubMed] [Google Scholar]
- 25.Harpaz R, Ortega-Sanchez IR, Seward JF Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). . Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2008;57(RR-5):1–30. [PubMed] [Google Scholar]
- 26.CONSORT Statement 2001-Checklist: Items to include when reporting a randomized trial. [ http://www.consort-statement.org]