Abstract
Mindfulness-Based Stress Reduction is a secular behavioral medicine program that has roots in meditative spiritual practices. Thus, spirituality may partly explain Mindfulness-Based Stress Reduction outcomes. Participants (N = 279; M (SD) age = 45(12); 75% women) completed an online survey before and after an 8-week Mindfulness-Based Stress Reduction program. Structural equation modeling was used to test the hypothesis that, following Mindfulness-Based Stress Reduction, the relationship between enhanced mindfulness and improved health-related quality of life is mediated by increased daily spiritual experiences. Changes in both spirituality and mindfulness were significantly related to improvement in mental health. Although the initial mediation hypothesis was not supported, an alternate model suggested that enhanced mindfulness partly mediated the association between increased daily spiritual experiences and improved mental health-related quality of life (indirect effect: β = 0.07, P = 0.017). Effects on physical health-related quality of life were not significant. Findings suggest a novel mechanism by which increased daily spiritual experiences following Mindfulness-Based Stress Reduction may partially explain improved mental health as a function of greater mindfulness.
Keywords: Mindfulness-Based Stress Reduction, Spirituality, Quality of life, Meditation, Mediation
Introduction
Seven in ten adults in the United States express a desire to experience spiritual growth (Gallup and Johnson 2003). While there is some controversy over the precise usage of the term spirituality, a functional definition includes “the personal quest for understanding answers to ultimate questions about life, about meaning, and about relationship to the sacred or transcendent” (Koenig et al. 2001). Although prayer is a common means to spiritual growth, mindfulness meditation offers another method of cultivating spirituality irrespective of religious affiliation, or non-affiliation (Kornfield 1993). In theory, mindfulness meditation can foster an increased sense of spirituality by disengaging from a narrow self-focus, and engaging a much broader view of interconnectedness in which oneself is not seen as separate from everyday activities, other people, or the world (Kabat-Zinn 1994; Kristeller and Johnson 2005). As such, the experience of mindfulness has been described as a method of self-transcendence (Phelan 2010; Singh 2010).
Buddhist teachings include the development of mindfulness as one of five spiritual faculties, along with faith, effort, concentration, and wisdom (Goldstein and Kornfield 1987). From the Western psychological perspective, when individuals practice mindfulness in their own way, during both formal meditation and during engagement in everyday activities, an awakening process occurs (Kabat-Zinn 1999). Theoretically, this awakening is part of an integrated developmental process during which one realizes the interconnection between all dimensions of experience— cognitive, emotional, physical, behavioral, social, and spiritual (Kristeller 2007). Therefore, systematic training in mindfulness is expected to generate a predictable pattern of interrelated changes in psychological, spiritual and health-related factors.
Mindfulness-Based Stress Reduction is a standardized 8-week program that incorporates Buddhist traditions of mindfulness meditation into a secular instructional class designed to teach skills that reduce suffering associated with stress, pain and illness (Kabat-Zinn 2003). Recent reviews of clinical and non-clinical populations report that Mindfulness-Based Stress Reduction training enhances mental health and quality of life (Baer 2003; Bohlmeijer et al. 2010; Chiesa and Serretti 2009; Greeson 2009; Grossman et al. 2004; Hofmann et al. 2010). These positive outcomes have been related in part to enhanced mindfulness (Carmody and Baer 2008; Carmody et al. 2008; Nyklíček and Kuijpers 2008; Shapiro et al. 2008).
Given the theoretical and phenomenological link between mindfulness practice and self-transcendence, spiritual engagement has also been proposed as a key mechanism of change in mindfulness-based therapies (Kristeller 2010). There is consistent evidence that spirituality can contribute to emotional well-being and can provide resilience to stress (Southwick et al. 2005). A small number of clinical studies have shown that Mindfulness-Based Stress Reduction is associated with increased aspects of spirituality, including personal faith, meaning and peace, and a sense of engagement and closeness with some form of higher power or God (Astin 1997; Birnie et al. 2010; Carmody et al. 2008; Shapiro et al. 1998). Enhanced spirituality may be considered an important outcome in and of itself, yet spiritual experiences also may be related to greater quality of life (Underwood and Teresi 2002). Carmody et al. (2008) reported that a change in spiritual well-being following Mindfulness-Based Stress Reduction was correlated with a change in mindfulness and distress. Similarly, a non-randomized study of cancer outpatients found that Mindfulness-Based Stress Reduction appeared to be more helpful than a creative arts program in enhancing spiritual well-being and reducing stress, depression, and anger (Garland et al. 2007).
Cultivating spirituality and mindfulness thus may play a role in Mindfulness-Based Stress Reduction outcomes. However, it is still unclear how changes in specific aspects of spirituality account for the mental and physical health benefits of mindfulness meditation training. The current study, therefore, evaluated whether one specific aspect of increased spirituality—ordinary spiritual experiences of transcendent awareness and connection in daily living— may account for health-related quality of life outcomes associated with Mindfulness-Based Stress Reduction. Since a change in mindfulness is presumably a key factor in determining the health benefits of mindfulness meditation training, we tested the hypothesis that improved health-related quality of life after participating in Mindfulness-Based Stress Reduction would be related to enhanced mindfulness, and that this relationship would be partially explained by changes in spirituality. Given mixed findings regarding the effects of homework on Mindfulness-Based Stress Reduction outcomes (Vettese et al. 2009), we also examined the specific role of meditation practice during the course and the non-specific role of positive expectancy in accounting for individual variation in outcomes.
Method
Participants
This study was approved by the Duke University Medical Center Institutional Review Board (IRB) and was conducted between April 2008 and March 2010. Participants were recruited from a self-pay, community-based Mindfulness-Based Stress Reduction program provided by Duke Integrative Medicine. The study was limited to individuals who were at least 18 years of age, proficient in English, and able to access an online survey.
The study included 279 subjects who signed an informed consent and completed an online survey battery before the first Mindfulness-Based Stress Reduction class. Sixty-four percent (n = 180) of these individuals also participated in the post-course survey assessment, which was administered within the week following the final class. The sample consisted primarily of women (75.3%) with a mean age of 45.0 years (SD = 11.6, range = 20–77 years). The majority of participants identified themselves as Caucasian (93.9%). Racial and ethnic minorities identified themselves as African-American (3.6%), Hispanic (2.9%), Asian (2.5%), and American Indian or Alaskan native (1.8%). Participants were generally well-educated (94.9% college graduates), and the majority were married or living with a partner (69.2%). Most were employed full-time (69.9%) with 10.4% working part time, 8.2% unemployed, 7.2% disabled, and 7.2% retired. Nearly half of the participants (44.8%) reported annual household income over $100,000 per year, while 22.6% earned $65,000–$100,000 and 25.4% reported less than $65,000 per year. These characteristics were consistent with the general demographics of the Duke Mindfulness-Based Stress Reduction program and were similar to those reported in previous outcome studies at large academic medical centers (Carmody and Baer 2008; Carmody et al. 2009; Reibel et al. 2001).
The sample included a balance of denominational Christians (39.4%) and persons without religious affiliation (36.9%); the remainder of the participants identified themselves as non-denominational Christians (8.2%), Jewish (5.0%), Unitarian-Universalist (5.0%), Buddhist (1.1%), Muslim (0.7%) or other (2.9%). The primary reasons participants sought to attend Mindfulness-Based Stress Reduction included: “improving mental health” (90.2%), “helping manage stress” (89.3%), “personal growth/self-discovery” (81.3%), and “improving physical health” (61.2%). Half (49.6%) of the participants reported that “exploring or deepening my sense of spirituality” was a reason for taking the course.
Intervention
The study sample participated in a standard 8-week Mindfulness-Based Stress Reduction program that was taught by highly experienced instructors with an average of 13 years (range: 10–20; SD = 5) teaching the course and a minimum of seven days of professional education and training coordinated by the Center for Mindfulness in Medicine, Health Care and Society (Worcester, MA). The 8-week Mindfulness-Based Stress Reduction program has been described elsewhere in detail (Kabat-Zinn 1990). In brief, the program consisted of classes that lasted for 2.5 h each week. Classes included didactic instruction on mindfulness and its relationship to stress and health, guided meditation practices, and group discussion. Mindfulness meditation practices included awareness of breathing, awareness of emotions, body scan, mindful hatha yoga, mindful walking, mindful eating, mindful listening, and lovingkindness (metta). Course instructors recommended that participants practice formal meditation outside of class for 20–45 min per day, 6 days per week. Instructors also encouraged individuals to supplement formal meditation with informal mindfulness practices, which apply mindfulness to everyday activities like eating, communicating with others, and hobbies. Class instruction and home meditation practice were supported with written materials and audio CDs (guided meditations and yoga), which were distributed at the beginning of the course. The course also included one full day (7-h) of meditation on the Saturday following the 6th week of class.
Procedure
Study participants were invited to complete an online survey comprised of demographic questions and validated self-report measures during a 7-day period between the course orientation and the first day of class. The survey was administered again within the week following the last class. Surveys were administered using ViewsFlash software version 6 (Cogix, Monterey, CA). The resulting de-identified data were maintained on a secure server.
Surveys administered to participants within the first year of the study required approximately 45–60 min to complete. In order to decrease response burden and to increase accrual and retention in study year two, the survey was shortened by omitting five scales, including the Short-Form Health Survey (see “Measures”). Grant funding also became available to compensate participants $10 for each survey completed during study year two. Individuals who participated during the second year of the study were therefore offered compensation and were asked to devote less time to each survey (approximately 30 min).1
Measures
Cognitive and Affective Mindfulness Scale-Revised (CAMS-R)
This 12-item scale assesses mindfulness of thoughts and feelings using four domains: attention, present-moment focus, awareness, and acceptance/non-judgment. A higher total score indicates greater self-reported mindfulness. The scale has demonstrated good convergent and discriminate validity with other measures of mindfulness, emotional regulation, well being, and distress (Feldman et al. 2007). The measure demonstrated good internal reliability in the present study with a Cronbach’s α of .81.
Daily Spiritual Experiences Scale (DSES)
This 16-item scale is intended to transcend the boundaries of specific religions by measuring one’s subjective experience of ordinary spiritual experiences on a daily basis (Underwood and Teresi 2002). This scale was chosen because everyday spiritual experiences, characterized by awareness of and a relationship with the transcendent, are expected to increase with intensive training in mindfulness. Items were reverse scored so that higher total scores indicated increased perceptions of self-transcendence and daily spiritual experiences (Underwood 2006). Scores on this well-validated scale have previously been related to quality of life and positive psychosocial status in normative samples (McCauley et al. 2007; Underwood and Teresi 2002). Scores can be transformed to or from the original metric by subtracting the total score from 112. Because our sample included a diverse range of religious affiliations and non-affiliation, the term “A Higher Power” was substituted for eight items that used the word “God”. The internal reliability of the scale was high (α = .93) in this sample.
12-item Short-Form Health Survey (SF-12)
The SF-12 is a valid and reliable means of assessing health-related quality of life in both normative and clinical samples (Gandhi et al. 2001). Standardized scores (M = 50, SD = 10) are reported separately for mental health and physical health as referenced by the mental component summary score and the physical component summary score. Higher scores indicate greater levels of mental and physical functioning and well-being, respectively. The internal reliability (Cronbach’s α) of the mental and physical health scales with weighted components was .71 and .72, respectively.
Other measures
On the baseline survey, participants reported the extent to which they expected to benefit from Mindfulness-Based Stress Reduction (1 = none, 2 = a little bit, 3 = somewhat, 4 = quite a bit, 5 = a great deal). Individuals who endorsed the highest two ratings (quite a bit or a great deal) were categorized as having “high” pre-course expectations, compared to other individuals who reported “lower” levels of expectancy. On the post-course survey, participants were asked to report how frequently they typically practiced meditation, mindfulness, or contemplative prayer during the course (1 = no practice, 2 = 1–2 times per month, 3 = once weekly, 4 = 2–3 times per week, 5 = 4–5 times per week, or 6 = daily or near-daily). Meditative practice was included as an ordinal variable in the path models.
Study design and data analysis
The study was designed as a prospective, observational trial with open enrollment. Chi-Square tests were used to compare demographic characteristics of survey completers and non-completers. Paired samples t-tests were used to test for changes in outcome measures. Effect sizes for pre-post change scores were determined using the formula for paired samples (d = t/√df) (Rosenthal 1991).
Structural equation modeling (SEM) was used to test hypothesized relationships among study measures (Kline 2004). Models for mental and physical health-related quality of life were analyzed using Mplus version 5 (Muthén and Muthén, Los Angeles, CA). Variables were screened for distributional assumptions prior to analysis, and all were relatively normally distributed with skewness and kurtosis less than 2.0. Models were fitted to the intention to treat sample using maximum likelihood (ML) estimation. Age, gender, income, and expectation to benefit from Mindfulness-Based Stress Reduction were included in the model as covariates in order to test if the relationship among outcome measures was independent of demographic characteristics and expectation to benefit from mindfulness training. Post-intervention values for mindfulness (CAMS-R), daily spiritual experiences (DSES), and health-related quality of life (SF-12) were adjusted for pre-intervention scores, thus permitting an analysis of residualized change in study measures.
Parameter estimates for path coefficients and R2 values were tested for statistical significance (z = 1.96, α = .05, two-tailed). The following recommended values were used as criteria for good model fit: (1) non-significant χ2 value; (2) comparative fit index (CFI) >.95; (3) root mean square error of approximation (RMSEA) <.06; and (4) standardized root mean squared residual (SRMR) <.08 (Hu and Bentler 1999; Kline 2004). The fit of the original hypothesized model was improved using modification indices generated by Mplus, and the relative fit of each modified model was tested using a chi-square difference test (Kline 2004).
Results
Preliminary analyses
At baseline, self-rated mental health (SF-12 mental component summary: M = 38.5, SD = 12.2) for the study sample fell more than one standard deviation below the norm for US adults suggesting that subjects’ emotional well-being interfered with work and other regular daily activities (Ware et al. 1998). In contrast, self-rated physical health (SF-12 physical component summary: M = 51.0, SD = 10.8) was close to the population mean, indicating an apparently physically healthy population. Most individuals reported a high expectation to benefit from Mindfulness-Based Stress Reduction, with 50% expecting to benefit quite a bit and an additional 24% expecting to benefit a great deal. Prior to beginning the course, 57% of participants reported that they had previous experience with meditation, mindfulness, or contemplative prayer; the median length of meditative practice was less than 1 year (interquartile range 0–3.5 years). The level of daily spiritual experiences at baseline (M = 49.0, SD = 17.5), fell within the normative ranges reported for national samples (Underwood and Teresi 2002; Underwood 2006). The baseline mindfulness score (M = 29.3, SD = 5.6) was nearly one standard deviation below the validation sample mean (Feldman et al. 2007).
The group of study participants that completed the post-course survey was similar to the group that did not complete the post course survey on all demographic and motivational variables except for three: (1) completers had a higher proportion with prior meditative experience (62% vs. 49%, P = .04), (2) completers more often endorsed spirituality as a motivation for enrolling in Mindfulness-Based Stress Reduction (57% vs. 37%, P <.01), and (3) completers more frequently endorsed curiosity or interest in mindfulness training as a motivation for enrolling (64% vs. 44%, P <.01).
Outcome analyses
Following Mindfulness-Based Stress Reduction, 54% of survey respondents reported that the course deepened their sense of spirituality. On average, participants who completed both pre- and post-course surveys reported significant increases in mindfulness of thoughts and feelings, daily spiritual experiences, and mental health (Table 1). Effect sizes were large for mindfulness and medium for spirituality and mental health. Physical health did not change significantly.
Table 1.
Changes in mindfulness, spirituality, and health-related quality of life after mindfulness-based stress reduction (MBSR)
| Measure | Pre-MBSR M (SD) |
Post-MBSR M (SD) |
t | df | P | Cohen’s d |
|---|---|---|---|---|---|---|
| Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) | 29.3 (5.6) | 35.4 (5.2) | 14.7 | 179 | <.001 | 1.10 |
| Daily Spiritual Experiences Scale (DSES) | 49.0 (17.5) | 56.9 (19.5) | 7.7 | 166 | <.001 | 0.60 |
| Short-Form Health Survey, Mental Component Summary (SF-12 MCS) | 40.5 (12.3) | 48.5 (10.0) | 5.9 | 72 | <.001 | 0.69 |
| Short-Form Health Survey, Physical Component Summary (SF-12 PCS) | 51.3 (9.9) | 51.6 (8.5) | 0.5 | 72 | .64 | 0.05 |
Path analyses
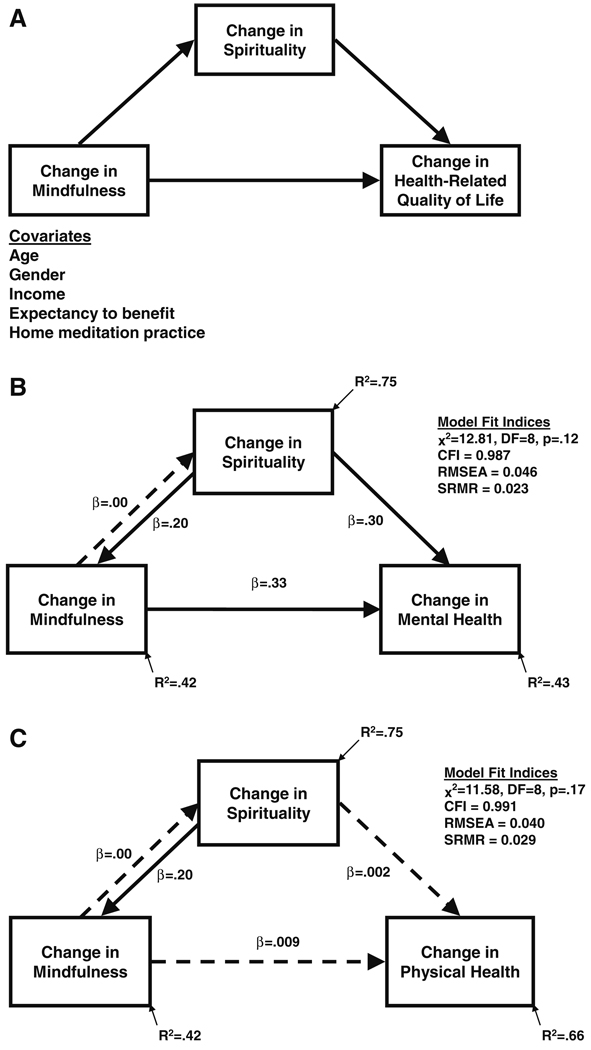
Our conceptual model is shown in Fig. 1a. We hypothesized that changes in mindfulness would explain changes in spirituality and health-related quality of life, and that changes in spirituality would be a mediator of mindfulness-related changes in quality of life. Consistent with predictions (see Fig. 1b), the hypothesized path model demonstrated that increases in spirituality (β = .30, P = .001) and mindfulness (β = .33, P < .001) scores were directly associated with improved mental health following Mindfulness-Based Stress Reduction. However, because the direct path linking change in mindfulness to change in spirituality was not significant, increased day-today perceptions of spiritual experience did not explain the relationship between post-intervention improvements in mindfulness and mental health, thus failing to support our original mediation hypothesis. Overall, the initial path model did not fit the data well (χ2 = 23.45, df = 8, P = .003, CFI = .959, RMSEA = .083, SRMR = .033).
Fig. 1.
a Hypothetical model where change in spirituality is a partial mediator of the relationship between change in mindfulness and change in health-related quality of life following Mindfulness-Based Stress Reduction. Covariates included in all modeling analyses are shown. b Standardized solution is presented for the final path model linking residualized changes in spirituality, mindfulness, and mental health. The pattern of associations did not support the original conceptual model. The data suggested an alternative mediation model in which increased ratings of daily spiritual experiences were significantly associated with increased mental health in two ways: (1) directly, and (2) indirectly, as a function of greater mindfulness. c Changes in self-reported spirituality and mindfulness were not significantly associated with physical health, thereby precluding the possibility of mediation. Path coefficients are standardized regression (β) weights. Statistical tests were conducted for direct and indirect (mediational) pathways linking predictor and criterion variables. Solid arrows represent statistically significant associations (P < .05). Dashed arrows represent non-significant (ns) relationships (P > .05). R2 is the total percentage of variance explained, including the effects of baseline status, expectancy, home meditation practice, and demographic variables (age, gender, and income) that are not shown for simplicity. The final models shown in b and c provided good fit with one modification of the original hypothesized model; a significant direct path was added from spirituality to mindfulness, thus allowing bidirectionality. The non-significant direct path from change in mindfulness to change in spirituality was fixed to zero without a significant loss of fit
In order to find the best-fitting model, we shifted from a confirmatory to an exploratory mode of data analysis (Kline 2004). Model modification indices were examined to see whether adding or removing one or more paths might lead to better fit. The strongest modification index suggested that adding a direct path from post-intervention spirituality to post-intervention mindfulness would lower the χ2 statistic by 12.53 points, thereby improving model fit. As shown in Fig. 1b, adding the additional direct path allowed changes in spirituality and mindfulness to be bidirectional, which we considered theoretically conceivable. That is, greater Mindfulness-Based Stress Reduction-related increases in spirituality could contribute to greater increases in mindfulness and vice versa. The recommended modification resulted in a significant direct path linking post-intervention increases in spirituality to increases in mindfulness (β = .26, P < .01), with a significant improvement in fit relative to the original model (χ2 difference = 11.87, df = 1, P = .001). The direct path from change in mindfulness to change in spirituality, however, remained nonsignificant; this parameter was fixed to zero without a significant decrement in fit (χ2 difference = 1.23, df = 1, P = .28). The final model shown in Fig. 1b exhibited good fit according to all four fit statistics (χ2 = 12.81, df = 8, P = .12, CFI = 0.987, RMSEA = .046, SRMR = .023). In summary, this exploratory mediation model suggested an alternative possibility that increased spirituality following Mindfulness-Based Stress Reduction accounted for improved mental health both directly (β = .30, P = .001) and indirectly (β = .07, P = .017), as a function of increased mindfulness.
Greater expectancy to benefit from Mindfulness-Based Stress Reduction was significantly associated with greater increases in post-intervention mindfulness (β = .15, P = .009) and spirituality (β = .11, P = .005). When accounting for pre-course expectancy, baseline status on outcome variables, and demographic covariates, self-reported frequency of meditation practice during the course was not independently associated with changes in mindfulness (β = .04, P = .47) or spirituality (β = .05, P = .18). The final model accounted for 42% of the variance in post-course mindfulness scores, 43% of the variance in post-course mental health scores, and 75% of the variance in post-course spirituality scores. Notably, inaddition to exhibiting a significant change during mindfulness training, the Daily Spiritual Experiences Scale was highly stable over time (r = .87, P <.0001).
A similar path model shown in Fig. 1c was run using physical health as the outcome measure. Because neither change in mindfulness nor change in spirituality was significantly associated with change in physical health, the model did not meet statistical criteria for mediation. Correlation coefficients for the modeled variables are shown in Table 2.
Table 2.
Correlations between modeled variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | – | ||||||||||||
| 2. Age | −.06 | – | |||||||||||
| 3. Income | −.05 | .21*** | – | ||||||||||
| 4. Practice | .03 | .22** | .15 | – | |||||||||
| 5. Hi expectancy | .15* | .04 | .00 | .06 | – | ||||||||
| Pre-MBSR | |||||||||||||
| 6. Spirituality | .05 | .21*** | −.03 | .21** | .20*** | – | |||||||
| 7. Mindfulness | −.04 | .24*** | .10 | .04 | .03 | .26*** | – | ||||||
| 8. Physical health | −.25** | −.26** | .07 | −.14 | −.09 | −.06 | .16 | – | |||||
| 9. Mental health | −.03 | .22* | .19* | −.06 | −.05 | .38*** | .63*** | −.12 | – | ||||
| Post-MBSR | |||||||||||||
| 10. Spirituality | .09 | .18* | .00 | .24** | .28*** | .87*** | .17* | .01 | .25* | – | |||
| 11. Mindfulness | −.03 | .16* | .07 | .05 | .24*** | .34*** | .59*** | −.05 | .47*** | .35*** | – | ||
| 12. Physical health | −.15 | −.38*** | .05 | −.17 | .00 | −.02 | .10 | .76*** | −.06 | −.01 | −.06 | – | |
| 13. Mental health | .11 | .08 | .13 | .20 | .00 | .42*** | .40*** | .04 | .48*** | .48*** | .56*** | −.15 | – |
Age = years; Gender = female; Hi expectancy = high expectations of benefiting from MBSR; Income = >$65,000 household/year; MBSR = Mindfulness-Based Stress Reduction; Mental Health = Short-Form Health Survey, Mental Component Summary; Mindfulness = Cognitive and Affective Mindfulness Scale-Revised; Physical Health = Short-Form Health Survey, Physical Component Summary; Practice = frequency of meditation, mindfulness or contemplative practices during 8-week course; Spirituality = Daily Spiritual Experiences Scale
P < 0.05;
P <.01;
P <.001
Discussion
Previous studies of Mindfulness-Based Stress Reduction have consistently documented correlations between self-reported changes in mindfulness, spirituality, and indicators of mental and physical health. However, little empirical research has explored the specific ways in which increases in daily spiritual experiences and mindfulness may, together, explain individual differences in the health benefits of Mindfulness-Based Stress Reduction, including improvements in health-related quality of life. This study provides preliminary evidence for changes in mindfulness as a mediating mechanism through which changes in spirituality may partly explain the mental health benefits of Mindfulness-Based Stress Reduction—a secular behavioral medicine intervention that focuses on intensive training in mindfulness meditation. The main findings from a relatively large group of apparently healthy but mentally stressed adults showed that increases in daily spiritual experiences were directly related to increases in mindfulness, which, in turn, was associated with improved mental health-related quality of life following Mindfulness-Based Stress Reduction. These data are consistent with the possibility that increases in spirituality, characterized by an awareness of and sense of connection with the transcendent in daily life, are not only an important outcome of mindfulness meditation training, but also a key mechanism by which Mindfulness-Based Stress Reduction produces mental health benefits.
The present findings are consistent with previous reports that mindfulness meditation training can enhance certain aspects of spirituality (Astin 1997; Shapiro et al. 1998), and that increases in spirituality following Mindfulness-Based Stress Reduction are associated with greater levels of mindfulness and mental health (Birnie et al. 2010; Carmody et al. 2008; Garland et al. 2007). This investigation extends prior studies of bivariate relationships among these variables by comparing alternative path models that help elucidate possible mechanisms underlying the health benefits of Mindfulness-Based Stress Reduction. Although the original hypothesis that spiritual experiences mediate the relationship between enhanced mindfulness and improved health-related quality of life was not upheld, the data suggested an alternative possibility that mindfulness may partly explain the association between increased perceptions of spirituality and improved mental health following Mindfulness-Based Stress Reduction. The possibility that enhanced attention to and awareness of the divine, the transcendent, and the interconnectedness of all things engenders greater mindfulness and mental health is consistent with both Eastern contemplative traditions and Western psychological theory (Wallace and Shapiro 2006).
In Buddhist teachings, a critical moment comes when a person’s meditation practice has developed sufficiently enough that the mind actually turns away from its usual absorption with shifting moment-by-moment worldly and sensory experience, and focuses instead on an also-present, more subtle quality of present-moment reality (Flickstein 2001). Flickstein suggests this process of spiritual transformation in the Buddhist “path of purification” has similarity to a principle in Gestalt Psychology, the “figure/ground perception” (p. 158). Without claiming deep Buddhist realizations or extensive Gestalt transformations for the participants in this study, we do speculate that the training in mindfulness that our participants undertook perhaps enabled them to shift their “view,” moving more easily between the foreground and background of experience in ways that made their personal awareness and experience of the “spiritual” in their lives (whatever that meant to each of them) more apparent. For example, much as depressed patients are reported to benefit from becoming mindful and dis-identifying from the cognitions associated with depression (Segal et al. 2002), it is conceivable that our participants may have noticed their own “foreground” experience of self-centered narratives or distractions more accurately; perhaps they were able to disengage from these “foreground” distractions more readily, and to more easily notice the everyday “background experiences” often associated with spirituality—for instance, beauty, joy, connection, and awe, all of which were measured by the Daily Spiritual Experiences Scale. We also wonder if their experience of more explicit inspiring or spiritually meaningful events may have been enhanced because of being more mindful of the entire experience.
One other explanation for the unexpected finding that increased mindfulness did not directly predict increased spirituality following Mindfulness-Based Stress Reduction may have been because the Daily Spiritual Experiences Scale was highly stable over time during the assessment period. Because over 75% of the variance in residualized DSES scores was explained by other variables the model, there was relatively little unique variability for increased mindfulness to explain. Furthermore, because the Cognitive and Affective Mindfulness Scale is limited to the assessment of thoughts and feelings, this specific measure of mindfulness may not have been independently associated with an increase in a transcendent sense of spiritual experiences above and beyond other variables.
Although Mindfulness-Based Stress Reduction is designed as a secular program, over 60% of the participants in this study identified with a spiritual or religious group, and half of the participants reported taking the mindfulness course to explore or deepen their sense of spirituality. Meditation and mindfulness have roots in various religious traditions (Kabat-Zinn 2003; Walsh and Shapiro 2006), and this study found that over 50% of survey respondents said that taking Mindfulness-Based Stress Reduction deepened their sense of spirituality. This finding is consistent with our observation that, following Mindfulness-Based Stress Reduction, 63% of survey respondents reported practicing meditation, mindfulness, or contemplative prayer at least 4–5 times per week, whereas only 13% reported such a level of meditative practice before the course. Although we did not measure participation in private religious activities other than meditation and contemplative prayer, it is also possible that participants may have used mindfulness principles, such as present-moment attention and kind-hearted compassion, to bolster religious beliefs and practices such as forgiveness, empathy, or altruistic acts of kindness that are shared among many faith traditions (Kristeller and Johnson 2005). It is also possible that whatever our subjects “saw” or experienced in their daily lives that was spiritually inspiring, including religious ceremonies or other practices, somehow strengthened their motivation and capacity to be more mindful, as articulated by Western Buddhist teachers (Goldstein and Kornfield 1987). Future studies are needed to formally assess this possibility, since religious and spiritual beliefs and their associated behaviors and biology may represent an important mechanism linking contemplative practices to improved mental and physical health (Park 2007; Wachholtz et al. 2007).
In contrast to results concerning mental health, physical health did not increase significantly across the 8-week Mindfulness-Based Stress Reduction program. Whereas at least two previous outcome studies (Carmody and Baer 2008; Carmody et al. 2008) documented a significant association between increased mindfulness following Mindfulness-Based Stress Reduction and reduced self-reported medical symptoms, the current study did not find a significant relationship between increased mindfulness and improved physical health as measured by health-related quality of life. Self-rated physical health following Mindfulness-Based Stress Reduction in this study also was not significantly associated with changes in spirituality. These predicted relationships may have been absent because the study sample, on average, had a normal level of physical functioning and well-being at baseline. Several previous studies of self-selected community Mindfulness-Based Stress Reduction program participants with lower levels of self-rated physical health at study entry reported significant improvement in physical health-related quality of life following mindfulness meditation training (Reibel et al. 2001; Rosenzweig et al. 2010; Roth and Robbins 2004). Thus, it is possible that a ceiling effect may have limited further improvements in physical health-related quality of life in the current study. Moreover, a restricted range of variance in physical health-related quality of life scores may have made it difficult to detect relationships with other measures. Alternatively, Mindfulness-Based Stress Reduction as an intervention may not have a strong effect on the physical component of the Short Form Health Survey (Plews-Ogan et al. 2005). Based on the present findings, future studies should test the possibility that baseline health and quality of life may serve to moderate the association between changes in mindfulness, spirituality, and physical dimensions of health-related quality of life. Specifically, there is a need to test whether changes in spirituality partially explain changes in mindfulness and quality of life in less physically healthy populations.
Home meditative practice during the 8-week Mindfulness-Based Stress Reduction program was not independently associated with changes in mindfulness when simultaneously accounting for baseline levels of mindfulness, the non-specific effect of high course expectations, and demographic variables, including age, gender, and income. This finding adds to mixed evidence for the direct association of adherence to home practice with Mindfulness-Based Stress Reduction outcomes (Vettese et al. 2009). Results did suggest that an individual’s expectancy to benefit from Mindfulness-Based Stress Reduction plays a modest explanatory role in determining course-related changes in spirituality and in mindfulness. These findings are consistent with a wealth of medical literature, which reports an association between positive expectancy and non-specific treatment effects (Harrington 1999; Stewart-Williams and Podd 2004). While expectancy may be considered a component of the placebo response, it is also closely related to motivation and may direct intentions and behavior (Delsignore and Schnyder 2007; Maddux et al. 1986; Wigfield 1994). Thus, expectancy may be an important component of the treatment effect that should be included in future research on the psychological mechanisms of Mindfulness-Based Stress Reduction.
The study had a number of limitations that also merit discussion. Because there was no randomized control or comparison group, the potential mediating mechanism identified in this study cannot be interpreted as a causal pathway. In addition, three rather than two measurement time points are necessary to establish temporal precedence – a key criterion for formal mediation. Participants in this study were sampled from a self-pay community Mindfulness-Based Stress Reduction program, and generalizability is limited by the lack of ethnic and social diversity in the sample. Another limitation was the use of self-report measures. Self-report of mindfulness may not provide accurate assessment, particularly for individuals with little to no meditation experience (Grossman 2008). Self-report of spirituality using the Daily Spiritual Experiences Scale may have been confounded by items such as gratitude, peace, and harmony, which can contribute to both spirituality and positive mental health (Koenig 2008). Whereas survey assessments of both mindfulness and spirituality risk oversimplifying these highly complex constructs, there was relatively little item overlap across the self-report scales used in this study, which helped guard against merely tautological associations. Another limitation is that outcomes measures may have been biased towards participants who were different at baseline in terms of prior meditative experience or spiritual motivation for taking Mindfulness-Based Stress Reduction. Finally, because the initial confirmatory hypothesis test failed to support our conceptual model, we proceeded to use a more exploratory approach to derive the best fitting model of the data, while limiting the number of post-hoc modifications. Our linear approach was overly simplistic. Because traditional teachings and modern theories suggest that relationships between mindfulness meditation practice, spirituality, and health are complex and interdependent, investigators are encouraged to conceptualize and systematically compare more than one a priori model of the data.
In conclusion, this study generated a new hypothesis that daily spiritual experiences are not only an important outcome of mindfulness meditation training, but that they may also be part of a key mechanism underlying mental health benefits. Future studies are needed to (a) replicate these initial results using a controlled study design, (b) establish causal directionality and temporal precedence by including three or more time points, and (c) test whether effects are similar or different as a function of sample characteristics, such as motivations for course participation and baseline levels of physical health. Future research might also further explore the intriguing mechanism of figure/ground reversal and its relationship to mindfulness practice, spirituality, and quality of life.
Acknowledgments
This research was supported by grant K99 AT004945 from the National Center for Complementary & Alternative Medicine (NCCAM) to JMG. MJS was supported by K23 MH087754 from the National Institute of Mental Health (NIMH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health (NIH). Additional support was provided by a research infrastructure grant from the Fannie E. Rippel foundation. We thank Katie Strobush and Janna Fikkan, Ph.D., for their assistance with recruitment. We thank all of the expert Mindfulness-Based Stress Reduction program instructors at Duke Integrative Medicine (Mary Matthews Brantley, M.A., LMFT; Sasha Loring, M.Ed., LCSW; Maya McNeilly, Ph.D.; Jeanne van Gemert, M.A., M.F.A., LMBT, LPC; and Ron Vereen, M.D.) for their intellectual contributions to study design and data interpretation. Finally, we thank all of the study participants who volunteered their time to complete our survey.
Footnotes
When comparing Mindfulness-Based Stress Reduction program cycles with the longer survey format (year 1) versus the shorter format (year 2), one-way ANOVA revealed no significant differences in the number of participants that enrolled in the study (F = 2.53, P = .16), completed the baseline survey (F = .47, P = .52), or completed the endpoint survey (F = .21, P = .67). Likewise the availability of study compensation was not associated with a significant difference in the number of enrolled participants (F = 5.43, P = .06), baseline survey completers (F = 5.45, P = .06), or end-point completers (F = 2.81, P = .15). Pearson’s Chi-Square and Fisher’s Exact Test indicated that demographic characteristics also remained consistent when study compensation was offered.
Contributor Information
Jeffrey M. Greeson, Email: jeffrey.greeson@duke.edu, Duke Integrative Medicine, Duke University Medical Center, Box 102904, Durham, NC 27710, USA.
Daniel M. Webber, Duke Integrative Medicine, Duke University Medical Center, Box 102904, Durham, NC 27710, USA
Moria J. Smoski, Cognitive and Behavioral Research and Treatment Program, Duke University Medical Center, Durham, NC, USA
Jeffrey G. Brantley, Duke Integrative Medicine, Duke University Medical Center, Box 102904, Durham, NC 27710, USA
Andrew G. Ekblad, Centre for Addiction and Mental Health, Toronto, ON, Canada
Edward C. Suarez, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, NC, USA
Ruth Quillian Wolever, Duke Integrative Medicine, Duke University Medical Center, Box 102904, Durham, NC 27710, USA.
References
- Astin JA. Stress reduction through mindfulness meditation. Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychotherapy and Psychosomatics. 1997;66:97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology Science and Practice. 2003;10:125–143. [Google Scholar]
- Birnie K, Speca M, Carlson LE. Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR) Stress and Health. 2010;26:359–371. [Google Scholar]
- Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. Journal of Psychosomatic Research. 2010;68:539–544. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA, Lykins ELB, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2009;65:613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of Psychosomatic Research. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. The Journal of Alternative and Complementary Medicine. 2009;15:593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Delsignore A, Schnyder U. Control expectancies as predictors of psychotherapy outcome: A systematic review. British Journal of Clinical Psychology. 2007;46:467–483. doi: 10.1348/014466507X226953. [DOI] [PubMed] [Google Scholar]
- Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and emotion regulation: The development and initial validation of the cognitive and affective mindfulness scale-revised (CAMS-R) Journal of Psychopathology and Behavioral Assessment. 2007;29:177–190. [Google Scholar]
- Flickstein M. Swallowing the River Ganges: A practice guide to the path of purification. Somerville, MA: Wisdom Publications; 2001. [Google Scholar]
- Gallup G, Johnson BR. New index tracks spiritual state of the union. Gallup Poll News Service. 2003 Retrieved from http://www.gallup.com/poll/7657/New-Index-Tracks-Spiritual-State-Union.aspx.
- Gandhi SK, Warren Salmon J, Zhao SZ, Lambert BL, Gore PR, Conrad K. Psychometric evaluation of the 12-item short-form health survey (SF-12) in osteoarthritis and rheumatoid arthritis clinical trials. Clinical Therapeutics. 2001;23:1080–1098. doi: 10.1016/s0149-2918(01)80093-x. [DOI] [PubMed] [Google Scholar]
- Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Supportive Care in Cancer. 2007;15:949–961. doi: 10.1007/s00520-007-0280-5. [DOI] [PubMed] [Google Scholar]
- Goldstein J, Kornfield J. Seeking the heart of wisdom: The path of insight meditation. Boston, MA: Shambhala Publications, Inc; 1987. [Google Scholar]
- Greeson JM. Mindfulness research update: 2008. Complementary Health Practice Review. 2009;14:10–18. doi: 10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P. On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research. 2008;64:405–408. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Harrington A. The placebo effect: An interdisciplinary exploration. Cambridge, MA: Harvard University Press; 1999. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delacorte Press; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion Books; 1994. [Google Scholar]
- Kabat-Zinn J. Indra’s net at work: The mainstreaming of dharma practice in society. In: Watson G, Batchelor S, Claxton G, editors. The psychology of awakening: Buddhism, science, and our day-to-day lives. London: Rider; 1999. pp. 225–249. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York, NY: The Guilford Press; 2004. [Google Scholar]
- Koenig HG. Concerns about measuring “spirituality” in research. The Journal of Nervous and Mental Disease. 2008;196:349–355. doi: 10.1097/NMD.0b013e31816ff796. [DOI] [PubMed] [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of religion and health. New York, NY: Oxford University Press, Inc; 2001. [Google Scholar]
- Kornfield J. A path with heart: A guide through the perils and promises of spiritual life. New York, NY: Bantam; 1993. [Google Scholar]
- Kristeller JL. Mindfulness meditation. In: Lehrer PM, Woolfolk RL, Sime WE, Barlow DH, editors. Principles and practice of stress management. 3rd ed. New York, NY: The Guilford Press; 2007. pp. 393–427. [Google Scholar]
- Kristeller J. Spiritual engagement as a mechanism of change in mindfulness- and acceptance-based therapies. In: Baer RA, editor. Assessing mindfulness & acceptance processes in clients: Illuminating the theory & practice of change. Oakland, CA: New Harbinger Publications, Inc; 2010. pp. 155–184. [Google Scholar]
- Kristeller JL, Johnson T. Cultivating loving kindness: A two-stage model of the effects of meditation on empathy, compassion, and altruism. Zygon®. 2005;40:391–408. [Google Scholar]
- Maddux JE, Norton LW, Stoltenberg CD. Self-efficacy expectancy, outcome expectancy, and outcome value: Relative effects on behavioral intentions. Journal of Personality and Social Psychology. 1986;51:783–789. [Google Scholar]
- McCauley J, Tarpley MJ, Haaz S, Bartlett SJ. Daily spiritual experiences of older adults with and without arthritis and the relationship to health outcomes. Arthritis Care & Research. 2007;59:122–128. doi: 10.1002/art.23246. [DOI] [PubMed] [Google Scholar]
- Nyklíček I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine. 2008;35:331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL. Religiousness/spirituality and health: A meaning systems perspective. Journal of Behavioral Medicine. 2007;30:319–328. doi: 10.1007/s10865-007-9111-x. [DOI] [PubMed] [Google Scholar]
- Phelan JP. Mindfulness as presence. Mindfulness. 2010;1:131–134. [Google Scholar]
- Plews-Ogan M, Owens JE, Goodman M, Wolfe P, Schorling J. Brief report: A pilot study evaluating mindfulness-based stress reduction and massage for the management of chronic pain. Journal of General Internal Medicine. 2005;20:1136–1138. doi: 10.1111/j.1525-1497.2005.0247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. General Hospital Psychiatry. 2001;23:183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Roth B, Robbins D. Mindfulness-based stress reduction and health-related quality of life: Findings from a bilingual inner-city patient population. Psychosomatic Medicine. 2004;66:113–123. doi: 10.1097/01.psy.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: The Guilford Press; 2002. [Google Scholar]
- Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: Effects on well-being. Journal of Clinical Psychology. 2008;64:840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine. 1998;21:581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Singh NN. Mindfulness: A finger pointing to the moon. Mindfulness. 2010;1:1–3. [Google Scholar]
- Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: Implications for prevention and treatment. Annual Review of Clinical Psychology. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- Stewart-Williams S, Podd J. The placebo effect: Dissolving the expectancy versus conditioning debate. Psychological Bulletin. 2004;130:324–340. doi: 10.1037/0033-2909.130.2.324. [DOI] [PubMed] [Google Scholar]
- Underwood LG. Ordinary spiritual experience: Qualitative research, interpretive guidelines, and population distribution for the daily spiritual experience scale. Archive for the Psychology of Religion. 2006;28:181–218. [Google Scholar]
- Underwood LG, Teresi JA. The daily spiritual experience scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Annals of Behavioral Medicine. 2002;24:22–33. doi: 10.1207/S15324796ABM2401_04. [DOI] [PubMed] [Google Scholar]
- Vettese LC, Toneatto T, Stea JN, Nguyen L, Wang JJ. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy. 2009;23:198–225. [Google Scholar]
- Wachholtz AB, Pearce MJ, Koenig H. Exploring the relationship between spirituality, coping, and pain. Journal of Behavioral Medicine. 2007;30:311–318. doi: 10.1007/s10865-007-9114-7. [DOI] [PubMed] [Google Scholar]
- Wallace BA, Shapiro SL. Mental balance and well-being. Building bridges between Buddhism and Western psychology. American Psychologist. 2006;61:690–701. doi: 10.1037/0003-066X.61.7.690. [DOI] [PubMed] [Google Scholar]
- Walsh R, Shapiro SL. The meeting of meditative disciplines and western psychology: A mutually enriching dialogue. American Psychologist. 2006;61:227–239. doi: 10.1037/0003-066X.61.3.227. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. SF-12: How to score the SF-12 physical and mental health summary scales. Lincoln, RI: QualityMetric Inc; 1998. [Google Scholar]
- Wigfield A. Expectancy-value theory of achievement motivation: A developmental perspective. Educational Psychology Review. 1994;6:49–78. [Google Scholar]