(See pages 94–95 for the Answer to the Photo Quiz.)
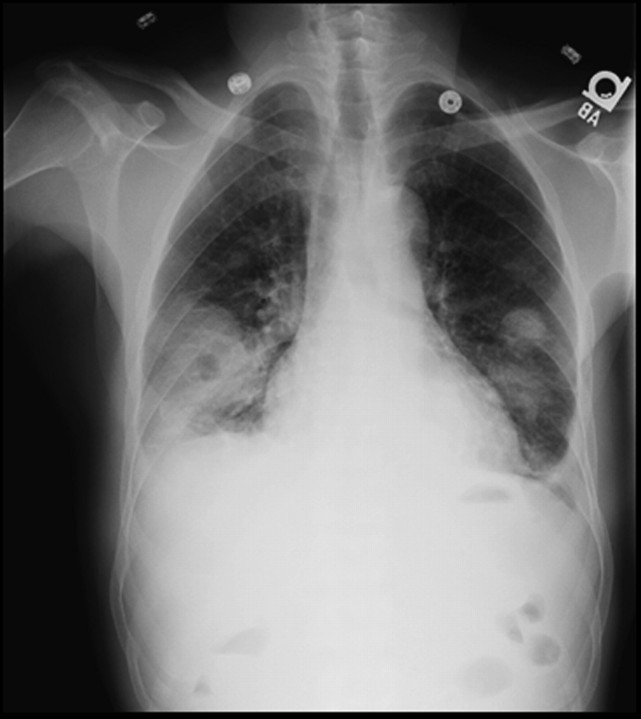
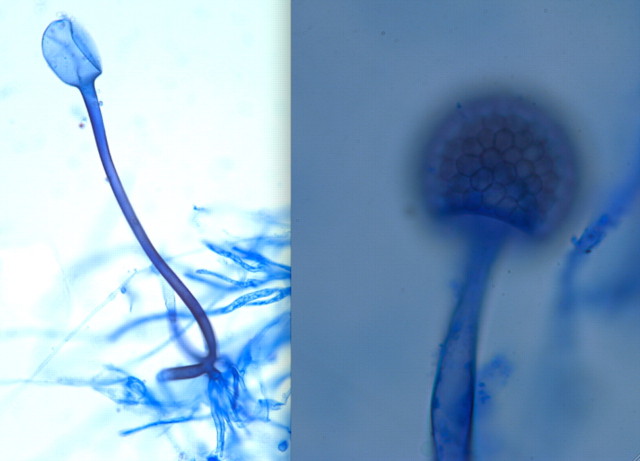
A 60-year-old Jamaican man with a history of diabetes mellitus and receipt of a deceased-donor renal transplant 11 months earlier presented with 3 days of left flank pain. He described associated nausea and a mild cough but denied fever, shortness of breath, weight loss, or other symptoms. He had no complications since his transplantation, and his immunosuppressive regimen consisted of 5 mg of prednisone, 4 mg of tacrolimus twice daily, and 1000 mg of mycophenolate mofetil twice daily. He also took glimepiride for his diabetes. The patient was retired, had no pets, and had not recently traveled. He had a history of an untreated positive tuberculin skin test result. Physical examination was remarkable for a fever (temperature, 38.6°C) and bibasilar pulmonary crackles. Significant laboratory results included a white blood cell count of 13,800 cells/μL, with 83% segmented neutrophils and sputum negative for acid-fast bacilli. A chest radiograph revealed bilateral nodular consolidations with cavitation in the lower lobes (Figure 1). A microscopic image of a positive culture is shown in Figure 2.
Figure 1.
Chest radiograph.
Figure 2.
Microscopic image of a positive culture stained with lactophenol cotton blue.
What is your diagnosis?