Abstract
Purpose
An important issue in spinal cord injury (SCI) research is whether standing can yield positive health benefits. However, quantifying dose of standing and establishing subject compliance with a standing protocol is difficult. This case report describes a method to monitor dose of standing outside the laboratory, describes the standing patterns of one subject, and describes this subject’s satisfaction with the standing protocol.
Method
A man with T-10 complete paraplegia agreed to have his commercially available standing wheelchair instrumented with a custom-designed logging device for a 2-year period. The micro-controller-based logger, under custom software control, was mounted to the standing wheelchair. The logger recorded date, duration, angle of standing, and start/stop times.
Results
The client exceeded a suggested minimum dosage of standing per month (130.4% of goal), choosing to stand for short bouts (mean = 11.57 min) at an average angle of 61 °, on an average 3.86 days per calendar week. He was generally very satisfied with the standing device and provided subjective reports of improved spasticity and bowel motility.
Conclusions
This case report describes a standing and surveillance system that allows quantification of standing dose. Future controlled studies are needed to evaluate whether standing can beneficially affect secondary complications after SCI.
Keywords: Quality of life, bone density, paralysis, mobility
Introduction
Ten to 20,000 people sustain spinal cord injury (SCI) each year, [1], and almost all use wheelchairs to regain mobility. Despite the obvious advantages that wheelchairs provide, there are also serious consequences associated with their chronic use. The loss of standing posture causes hypercalciuria [2 – 4] and urinary calculi [5], severe osteoporosis and increased fracture risk [6], postural deviations that can lead to decubitus ulcers [7], and joint contractures that can limit functional tasks like dressing and transferring.
Because so many of the secondary complications of SCI are attributable to chronic seated posture, there may be some benefit in offering alternative positions from the seated posture after SCI. Passive standing frames are available, but because they are stationary and heavy, they are not always convenient to use for functional purposes. Long leg braces (LLBs) provide people with SCI the opportunity to stand and move with crutches, but the time associated with donning and doffing the braces restricts their usefulness in daily life [8, 9]. As few as 25% of people who receive LLBs continue to use them after 5 years [8]. Wheelchairs that enable people with SCI to stand appear ideal, but the excessive weight of standing wheelchairs has traditionally limited their widespread use. However, recent technological advancements have yielded lighter, more maneuverable standing wheelchairs. The extent to which individuals with SCI will use the standing feature of such wheelchairs is unknown.
Accordingly, the first purpose of this paper is to describe a method to monitor the use of a standing wheelchair. Secondly, we report the standing patterns of an individual with SCI who used a standing wheelchair for a 2-year period. Finally, we report this subject’s level of satisfaction with the standing device and his perceptions of the standing protocol. Our long-term goal is to understand the patterns of use of this system so that the dose of standing can be better defined for future studies.
Methods
Subject description
Mr. R is a 25-year-old Caucasian male who sustained complete T10 paraplegia after a fall at age 22 (American Spinal Injury Association [ASIA] Impairment Scale score ‘A’: No motor or sensory function preserved in the sacral segments S4 – S5 [10]). He underwent standard inpatient care at a tertiary medial facility, followed by several weeks at a rehabilitation center. Mr. R lives independently as a university student and plays intercollegiate wheelchair basketball. Four months after his injury, Mr. R received a standing wheelchair to use in a home standing protocol. Mr. R gave informed consent for this protocol in accordance with institutional guidelines. He underwent acclimation to standing posture under the supervision of a physical therapist.
Standing apparatus and monitoring method
The standing chair was commercially available (Levo USA Inc., PO Box 3869, Peachtree City, GA 30269, USA) with manual propulsion and electrically powered standing. Knee, waist, and chest straps secured Mr. R into the chair. He raised himself to standing by pressing a button on a control panel mounted on the chair’s armrest. A custom-designed tilt sensor and data-logging device (‘logger’) mounted beneath the chair recorded the date, bout (start/end time), duration, and standing angle.
The logger began and ended recording at a threshold of 20 ° from horizontal and sampled the standing angle every second. The logger was calibrated with a jig that had a resolution of 0.5 °. The percent error for linearity, accuracy, and repeatability was 1.1, 0.9 and 1.4% of full scale.
The logger measured standing angle using an integrated-circuit accelerometer, which provided an analog voltage proportional to the static g-force in the plane of the logger circuit board. The logger circuitry consisted of a micro-controller, memory, a real-time clock, an accelerometer, an amplifier for the accelerometer, and the power supply. The microcontroller contained internal analog to digital converters for digitizing the response of standing angle on the accelerometer. The standing angle was sampled and recorded to memory with time and date stamps, according to custom programmed criteria. A parallel port interface allowed the recorded data to be read by a host computer, and allowed the logger to be controlled or programmed. Data from the logger were periodically downloaded into the serial port of a microcomputer using custom designed software, and then they were analyzed in a standard software spreadsheet. Date, time, duration, and angle data were used to quantify Mr. R’s typical pattern of use of the standing wheelchair.
Computation of dose of standing
The experimental protocol requested that Mr. R stand a minimum of 20 min each day during 5 days of each calendar week. This dose was requested as a minimum because it is consistent with recommended times for exercise of able-bodied. However, the experimenters placed no constraints on Mr. R regarding maximum use of the standing chair. Dosage of standing was calculated in minutes per month, then was expressed as a percent compliance with the recommended monthly dosage. These monthly compliance values were computed as the quotient of the actual standing duration and the goal duration. Goal duration was computed with the following formula: Goal Duration = (20 - min standing/day)(5 days/week)(week fraction/month). The week fraction was a mathematical constant used to correct for months with more than 28 days. It was computed with the following formula: Week fraction = [(# days in excess of 28)/(7days per week)]+ 4 weeks. For example, the week fraction for a month with 30 days is 4.286 weeks, and the goal duration for such a month is 428.6 min.
Standing questionnaire
Every 3 months for a total of 12 months, Mr. R completed a questionnaire designed to assess his satisfaction with the standing apparatus. Questionnaire items included ease of use of the system for wheeling, sitting, and standing, likelihood of using the standing wheelchair for everyday mobility, and whether Mr. R attributed any health changes (positive or negative) to standing. The questionnaire also asked if, based on his experiences with the standing device, Mr. R would recommend standing to other people with SCI.
Results
Temporal use pattern of the apparatus
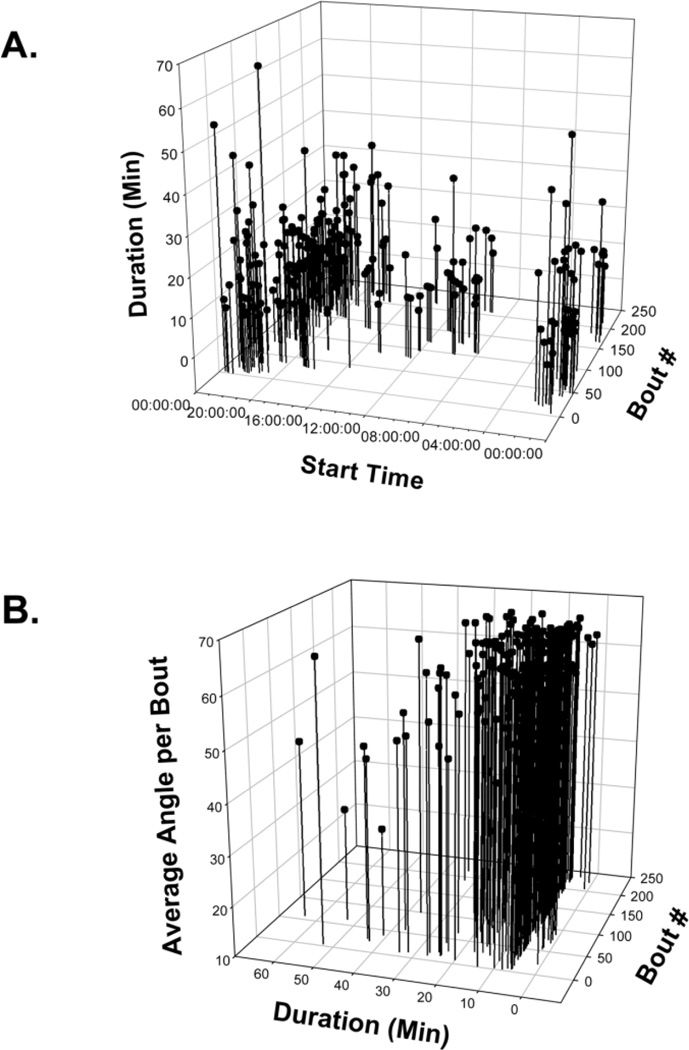
Figure 1 shows representative examples of Mr. R’s pattern of use of the standing wheelchair. The data shown are from May 2002 to October 2002, about midway through his 2-year monitoring period. He performed a total of 238 bouts of standing in this 5-month sample period, divided among 77 daily standing sessions. The start times of each bout of standing cluster toward the late evening, most often after 08:00 h.
Figure 1.
Representative examples of the pattern of use of the standing wheelchair. A: Time is given in military units. Bouts starting between 00:00:00 and 02:00:00 were carry-overs from standing sessions beginning just before midnight on the previous date (the logger clock rolled over to 00:00:00 at midnight). B: Mr R often stood at various angles within a single bout. For each bout, average angle appears on the vertical axis.
Mr. R tended to divide his standing time into multiple short bouts during the day. Average bout time illustrated in Figure 1 was 12.5865 min (SD = 9.6104), which is commensurate with the average bout time for his entire 2-year data set (mean = 12.3021 min, SD=11.3629). This overall average bout time does not reflect any standing that Mr. R performed for less than 1 min. As a member of a dart throwing team, Mr. R often performed several bouts of less than 1 min in the upright position as he threw a dart. When these sessions are included, the average bout duration for the entire data set drops to 4.1775 min (SD = 7.8794). In addition to recreational activities, Mr. R reported that he frequently used the standing wheelchair to assist with household tasks such as changing light bulbs, painting walls, and remodeling his bathroom.
When standing, Mr. R elevated his chair to an average of 61 ° above horizontal (SD = 13.06). For the subset of data shown in Figure 1b, mean angle per bout of standing was 60 ° above horizontal (SD = 16.5).
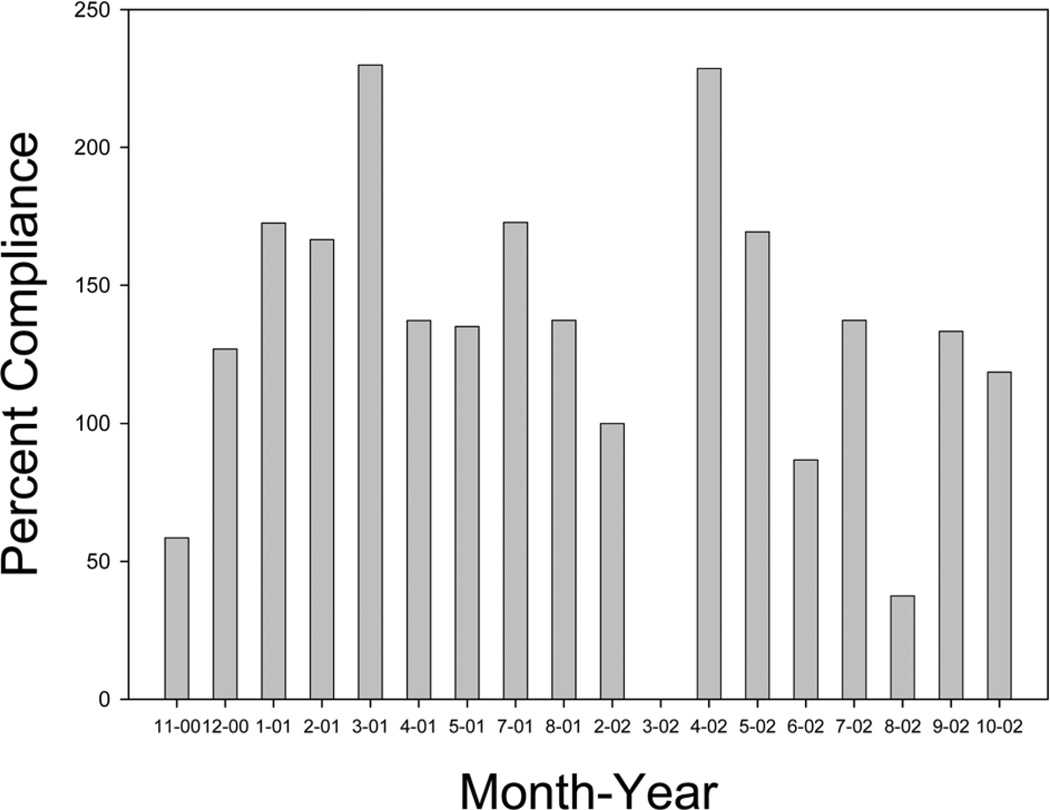
Compliance with standing recommendations
Mr. R regularly exceeded the requested minimal dose of 20 minutes of standing per day (Figure 2). Mean percent compliance for the standing protocol from November 2000 to October 2002 was 130.4% of goal duration (SD = 59.3). The percent compliance for each month was substantially influenced by events in the subject’s life. For example, Mr. R developed thoracic pain in spring of 2002 and underwent removal of his Harrington rods. Based on his physician’s recommendation, Mr. R did no standing in the month of March 2002. During other months, Mr. R elected to use his standing wheelchair for recreational activities (for example, when he joined a darts league in spring of 2001). This tended to elevate his compliance values.
Figure 2.
Compliance with standing recommendations, expressed as percentage of the goal of standing for each month. Average percent compliance was 130.4%. Data for June 2001 and for September 2001 through January 2002 were not collected. Mr. R did no standing during March 2002 due to removal of his Harrington rods.
A more detailed analysis of Mr. R’s compliance data reveals that although he exceeded the monthly recommended standing duration, he typically stood fewer than the suggested 5 days of each calendar week. Between November 2000 and October 2002, he used his standing chair on an average of 3.86 days in each calendar week (range: 0 to 7 days). This indicates that Mr. R tended to use the chair less frequently than suggested, but for a much longer duration than the 20-min per day guideline.
Satisfaction with the standing wheelchair
Mr. R rated the standing wheelchair on ease of use and provided specific suggestions to improve the usefulness of the device. At each measurement interval he rated the ‘ease of use in standing’ as ‘very easy’. During the first measurement period he rated the ‘ease of use in the sitting position for moving about’ as ‘easy’, but for all remaining measurement periods this improved to ‘very easy’.
Mr. R consistently stated that he was ‘very satisfied’ with the device for standing and that he would ‘very likely’ continue to use the device for standing. His responses ranged between ‘dissatisfied’ and ‘very satisfied’ with the device for sitting. He was consistently ‘satisfied’ with the device for moving while sitting, stated he was either ‘likely’ or ‘very likely’ to continue to use the chair for sitting or moving, but stated he was ‘unlikely’ to use the standing wheelchair instead of his conventional wheelchair for everyday mobility.
Several characteristics of the standing wheelchair diminished its usefulness for everyday mobility, in Mr. R’s opinion. He found the chair to be heavy and bulky. He stated that he could not go up curbs in the chair, that the wheels had no adjustable camber, and that the chair lacked the suspension of his conventional chair. Mr. R stated that the 70 ° front leg rests (a safety necessity for the standing feature) made maneuverability difficult, especially in tight spaces.
At each 3-month questionnaire administration interval, Mr. R ‘highly recommend’ that people with SCI stand ‘1 – 2 hours per day’ to ‘as much as time permits’. During his visits to the laboratory, Mr. R often stated that he believed his standing program had a beneficial effect on his lower extremity spasticity. He frequently and intentionally performed his standing program before tasks such as dressing and showering, which would be more difficult if spasms occurred. He stated that on the days he did no standing, his spasms were more frequent and more bothersome. On two occasions when Mr. R returned his chair for repairs, he stated he was quite anxious to get it back because of the detrimental changes he noticed on his spasticity and on his bowel program.
Discussion
This case report quantifies the use patterns of a subject with a standing wheelchair. Innovative monitoring technology enabled us to have day-today surveillance of the subject’s use of the chair. This subject showed excellent compliance with recommendations for standing. Tracking his standing habits with a data logging system revealed that he tended to stand fewer than the recommended 5 days per week, but that he stood for longer than the recommended duration per day. These parameters may be useful for future controlled studies that attempt to formulate reasonable standing duration recommendations for subjects with SCI.
Mr. R was generally satisfied with the standing protocol and with the standing feature of the experimental apparatus. He was less satisfied, however, with the standing wheelchair as an option for everyday mobility. However, it is important to note that Mr. R was accustomed to an everyday wheelchair with a high-performance configuration (lightweight metal frame, fiberglass wheel spokes, front caster suspension, and rear wheels in 9 ° of camber). It is uncertain whether the average wheelchair user has such stringent performance demands. Mr. R found numerous household and recreational uses for the standing wheelchair, above and beyond his participation in the research protocol.
We report good compliance with standing recommendations for a standing wheelchair, but other standing devices may have similar levels of usability. Retrospective studies have shown that people who receive standing frames also frequently utilize their devices. Several years after purchasing standing frames, 100% of people surveyed by Hawran and Biering-Sørenson used their frames at least once monthly, with 40% using them daily [8]. Walter et al. [11] reported that 74% of their subjects stood at least once per week.
An intriguing, though not unique finding was that Mr. R reported improvements in his spasticity and bowel program with standing. This anecdotal report corresponds with other case studies and surveys that reveal that subjects who stand perceive health benefits to this activity [11 – 15]. Mr. R believed standing would be useful for other people with SCI, an opinion shared by 79% of people with SCI who did standing in a study by Dunn et al. [15]. However, before standing can be widely recommended for people with SCI, controlled studies are necessary to determine conclusively whether standing can improve spasticity, bowel and bladder function, decubitus ulcer incidence, range of motion, and overall quality of life in people with SCI.
This case report demonstrates the feasibility of precise monitoring of standing dosage. Standing with a standing wheelchair was convenient and enjoyable for a subject, and compliance with standing recommendations was good. In the present healthcare environment, the cost for durable medical equipment requires that we have some assurance the equipment will be regularly used, and may therefore be an effective adjunct to the overall management of a client.
Conclusion
We present a standing and surveillance system that can precisely monitor duration and angle of standing, so that a dosage of standing may be computed. Preliminary investigation with a single subject indicates that compliance with this device is good. This case report lays the foundation for a method to quantify dose of standing so that effective and economically feasible standing interventions can be developed. Controlled studies are needed to evaluate whether standing can beneficially affect the secondary complications of SCI.
Acknowledgements
Dr. Shields is funded by an award (R01-HD39445) from the National Center for Medical Rehabilitation Research (NIH). Shauna Dudley-Javoroski received a Doctoral Scholarship from the Foundation for Physical Therapy. We thank Levo Corporation (Switzerland and USA) for providing the standing chair.
References
- 1.Eichenholtz SN. Management of long-bone fractures in paraplegic patients. Journal of Bone & Joint Surgery - American Volume. 1963;45-A:299–310. [Google Scholar]
- 2.Issekutz B, Jr, Blizzard JJ, Birkhead NC, Rodahl K. Effect of prolonged bed rest on urinary calcium output. Journal of Applied Physiology. 1966;21:1013–1020. doi: 10.1152/jappl.1966.21.3.1013. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan PE, Roden W, Gilbert E, Richards L, Goldschmidt JW. Reduction of hypercalciuria in tetraplegia after weight-bearing and strengthening exercises. Paraplegia. 1981;19:289–293. doi: 10.1038/sc.1981.55. [DOI] [PubMed] [Google Scholar]
- 4.Uebelhart D, Demiaux-Domenech B, Roth M, Chantraine A. Bone metabolism in spinal cord injured individuals and in others who have prolonged immobilisation. A review. Paraplegia. 1995;33:669–673. doi: 10.1038/sc.1995.140. [DOI] [PubMed] [Google Scholar]
- 5.Abramson AS. Bone disturbances in injuries to the spinal cord and cauda equina (paraplegia) The Journal of Bone and Joint Surgery. 1948;30-A:982–987. [PubMed] [Google Scholar]
- 6.Shields RK. Muscular, skeletal, and neural adaptations following spinal cord injury. Journal of Orthopaedic & Sports Physical Therapy. 2002;32:65–74. doi: 10.2519/jospt.2002.32.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shields RK, Cook TM. Lumbar support thickness: effect on seated buttock pressure in individuals with and without spinal cord injury. Physical Therapy. 1992;72:218–226. doi: 10.1093/ptj/72.3.218. [DOI] [PubMed] [Google Scholar]
- 8.Hawran S, Biering-Sorensen F. The use of long leg calipers for paraplegic patients: a follow-up study of patients discharged 1973 – 82. Spinal Cord. 1996;34:666–668. doi: 10.1038/sc.1996.120. [DOI] [PubMed] [Google Scholar]
- 9.Coghlan JK, Robinson CE, Newmarch B, Jackson G. Lower extremity bracing in paraplegia – a follow-up study. Paraplegia. 1980;18:25–32. doi: 10.1038/sc.1980.5. [DOI] [PubMed] [Google Scholar]
- 10.Maynard FM, Jr, Bracken MB, Creasey G, et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord. 1997;35:266–274. doi: 10.1038/sj.sc.3100432. [DOI] [PubMed] [Google Scholar]
- 11.Walter JS, Sola PG, Sacks J, Lucero Y, Langbein E, Weaver F. Indications for a home standing program for individuals with spinal cord injury. Journal of Spinal Cord Medicine. 1999;22:152–158. doi: 10.1080/10790268.1999.11719564. [DOI] [PubMed] [Google Scholar]
- 12.Eng JJ, Levins SM, Townson AF, Mah-Jones D, Bremner J, Huston G. Use of prolonged standing for individuals with spinal cord injuries. Physical Therapy. 2001;81:1392–1399. doi: 10.1093/ptj/81.8.1392. [DOI] [PubMed] [Google Scholar]
- 13.Bohannon RW. Tilt table standing for reducing spasticity after spinal cord injury. Archives of Physical Medicine & Rehabilitation. 1993;74:1121–1122. doi: 10.1016/0003-9993(93)90073-j. [DOI] [PubMed] [Google Scholar]
- 14.Hoenig H, Murphy T, Galbraith J, Zolkewitz M. Case study to evaluate a standing table for managing constipation. Sci Nursing. 2001;18:74–77. [PubMed] [Google Scholar]
- 15.Dunn RB, Walter JS, Lucero Y, et al. Follow-up assessment of standing mobility device users. Assistive Technology. 1998;10:84–93. doi: 10.1080/10400435.1998.10131966. [DOI] [PubMed] [Google Scholar]