The diagnosis of Parkinson's disease (PD) is clinical and there are no biological markers to confirm it during life.[1] Confirmation is possible only post mortem. There are no accepted neuropathological criteria for PD[2] and there is an ongoing debate on whether PD is a single entity.[3,4] This is because of the description of genetic forms of PD with clinical features typical of sporadic PD but pathological features distinct from it.[5] Early accurate diagnosis of PD may be important for institution of disease course -modifying treatments when they become available, for prognostication and for research purposes.[6] Recognizing early PD is not easy. It is also well known that in the early stages of the disease, PD and other forms of degenerative parkinsonism share common features and clinical distinction may be difficult.[7] The certainty of diagnosis increases as the disease advances and in specialist clinics.[8] Even though PD is considered as a predominantly motor disorder, non-motor symptoms occur at all stages of the disease[9] and may even antedate it.[10,11] However, the diagnosis of PD rests on motor signs. The three cardinal motor manifestations of PD which are essential to make a diagnosis are rest tremor, rigidity, and bradykinesia.
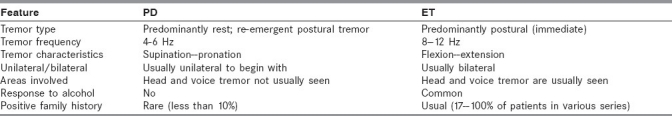
Rest tremor (4-6 Hz) tremor occurring when the limb is fully supported). It can be brought out by mental stress, during walking, or while performing alternating finger taps with the opposite hand. Some patients have postural tremor but appears only after a latency of seconds to a minute of assuming the outstretched posture of arms (re-emergent tremor).[12] This feature, if present, helps to differentiate PD tremor from postural tremor due to other causes, e.g. essential tremor (ET) in which tremor appears immediately on assuming the posture. Typically, rest tremor of the hands in PD has a pill rolling appearance and abates during action. In the head region, tremor occurs in the lips, chin, and jaw but is infrequent in the neck. About 75% of PD patients have tremor during the course of their illness.[13]
Rigidity (resistance offered to passive flexion-extension or rotation movement of major joints with the patient sitting relaxed. It does not include cog-wheel rigidity caused by tremor). Rigidity in PD is lead pipe-like, is present throughout the range of movement, and is not velocity dependent. In PD, rigidity involves both neck and limbs while in progressive supranuclear palsy (PSP) there is a disproportionate axial preponderance of rigidity.[14]
Bradykinesia (slowness of initiation of voluntary movements with progressive reduction in speed and amplitude of repetitive actions). It is tested by asking the patient to do repeated finger taps, alternate pronation and supination of forearm, opening and closing of fist and foot taps. Look for speed, regularity, arrests of ongoing movement and slowness. Fatiguing or gradual reduction in amplitude during continued activity and arrests are typical of true bradykinesia.
Postural instability (not due to cerebellar, vestibular, posterior column or visual dysfunction). In the clinic this may be demonstrated by the “pull test.” This is assessed from the response to the sudden strong posterior displacement produced by a pull on shoulders while the patient stands erect with eyes open and feet slightly apart. The patient is prepared for the test and can have a few practice runs. Many experts do not consider postural instability by itself for the early diagnosis of PD as it is seldom present in early stages and is nonspecific. Onset with postural instability and gait disturbance (PIGD) tends to be more often due to atypical parkinsonism.[15]
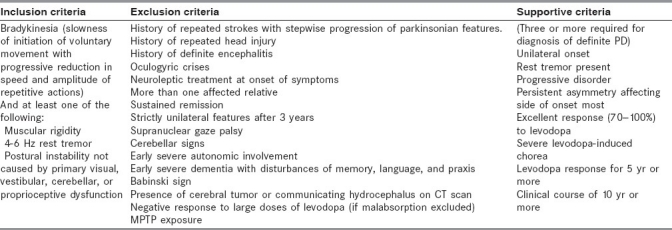
Although several clinical criteria have been proposed for PD, most have not been evaluated for reliability and validity. The United Kingdom Parkinson's disease Society Brain Bank Clinical Diagnostic Criteria[16] [Table 1] is based on a retrospective clinico- pathological study and has been tested in autopsy confirmed cases and found to have an accuracy of around 75% to 80%.[17] The misdiagnosis in the remaining cases was from conditions such as multiple system atrophy (MSA), progressive supranuclear palsy (PSP), vascular parkinsonism and Alzheimer's disease. These criteria are useful for improving diagnostic accuracy but may not be useful in monosymptomatic and early stages of PD.[18] Early PD can have a wide variety of presentations including non-specific symptoms like generalized stiffness, pain and paresthesia, reduced appetite, constipation, sleeplessness, shoulder pain, and reduction in volume of voice or more specific ones like tremor during anxiety, sense of inner tremor, reduced arm swing, reduced facial expression, personality changes noticed by others, slowness, monotonous speech, micrographia, problems with fine motor task, dragging of leg, dystonia of limbs (especially in young onset PD due to Parkin mutations), mood changes, decreased smell, and increased salivation.[19–21] Response to treatment may support the diagnosis. Excellent response to levodopa and levodopa-induced chorea are seen more often in PD but can occur in MSA[22] where it wanes with time. Orofacial dystonia, spontaneous or levodopa induced, is often seen in MSA. Partial response to levodopa can be seen in PSP[23] and other atypical parkinsonism.
Table 1.
UK Parkinson's disease society brain bank clinical diagnostic criteria[16]
In order to address the issue of improving the early diagnosis of PD, Calne et al. proposed a designation of escalating levels of diagnostic confidence [Table 2].[24] Three categories were defined.
Table 2.
Distinguishing features between tremor of Parkinson's disease and essential tremor
Clinically possible: Presence of any one of tremor, rigidity, or bradykinesia could qualify for clinically possible PD. Impairment in postural reflexes was not included. Tremor must be of recent onset and may be rest or postural.
Clinically probable: Two of the cardinal features of rest tremor, rigidity, bradykinesia, or impaired postural reflexes are required to make this diagnosis. Alternatively, asymmetrical rest tremor, asymmetrical rigidity, or asymmetrical bradykinesia alone may be sufficient.
Clinically definite PD: A combination of three of the features - rest tremor, rigidity, bradykinesia or impairment in postural reflexes - is required to make the diagnosis of PD clinically definite. Alternatively, two of the features are sufficient if one of the first three displays asymmetry. Laboratory support for the diagnosis could be applied to each category. However, these criteria have not been validated in pathologically confirmed cases.
There are certain conditions which are commonly mistaken for PD, especially in the early stages of PD. ET can have rest tremor[25] and also cogwheel type of rigidity. ET can be asymmetric; however, long-duration asymmetric postural tremor is more likely to be due to PD than ET.[26] The distinguishing features between the tremor of PD and ET are shown in Table 2. The other conditions producing rest tremor include dystonic tremor (tremor in a dystonic body part, irregular and abolished in certain positions), tardive tremor related to neuroleptic exposure, and Wilson's disease. The slowness of activities seen in hypothyroidism may be mistaken for bradykinesia. The slowness of activities and reduced facial expression in depression can resemble PD. Slowness of activities, slow gait, instability, and hypomimia of the elderly may also resemble PD. Diagnosis of PD should be made carefully in very old people in whom the presence of a rest tremor may be the most specific sign.[27]
PD needs to be differentiated from the secondary causes of parkinsonism. Vascular parkinsonism results from infarcts involving frontal lobe, deep subcortical white matter, and basal ganglia. The patients are more likely to present with gait difficulty and postural instability rather than tremor. They usually have a history of stroke and report risk factors for stroke. Focal signs like pyramidal signs and vascular dementia may co-exist. The patients usually have a more upright posture, wide based stance, and well-preserved arm swing compared to PD. Response to levodopa therapy is usually poor.[28] A variety of drugs including neuroleptics, dopamine receptor blocking agents, dopamine depletors (tetrabenazine), and calcium channel blockers can cause drug-induced parkinsonism (DIP). This could develop 1 to 3 months after introduction of a D2 receptor blocker neuroleptic or an increase in dose and generally resolves in weeks to months after discontinuation. Freezing and festination are rare in DIP. DIP is often difficult to differentiate from PD; useful clues for differentiation include parkinsonism associated with tardive dyskinesia or akathisia , symmetric signs, action greater than resting tremor and presence of a low-frequency, high-amplitude jaw tremor (“Rabbit syndrome”).[29–31] The classical features of normal pressure hydrocephalus include gait disturbance, urinary incontinence and cognitive changes; however the triad is seen only in advanced cases.[32] Bradykinesia of upper limbs is seen in around 50% and frank parkinsonism, usually symmetrical, in less than 15% of patients.[33] Rest tremor and upper limb rigidity are rare. Gait is more wide-based and apractic in NPH. Gait difficulty is not usually overcome by stepping over examiners foot as it happens in PD. Wilson's disease is yet another cause for parkinsonism; most cases also have other signs like coarse “wing beating” tremor, dystonia, a “mixed” dysarthria, and neurobehavioral disturbances. Investigations like serum copper and ceruloplasmin measurement, slit lamp examination for Kayser-Fleischer ring, 24 h urinary free copper estimation, and liver biopsy are helpful in establishing the diagnosis in suspected cases. Infections (SSPE, mycoplasma pneumonia, HIV, viral encephalitis), metabolic disturbances (hyperparathyroidism), toxins (MPTP, manganese, carbon monoxide, cyanide, methanol), anoxia, and structural lesions (frontal, temporal, brainstem and posterior fossa space occupying lesions causing hydrocephalus) are relatively rare causes of secondary parkinsonism.
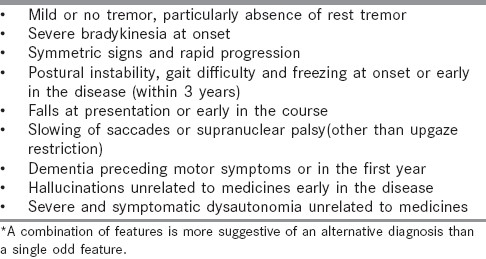
Differentiation of PD from other neurodegenerative causes of Parkinsonism is important from the treatment and prognostication point of view. MSA is characterized by a combination of varying degrees of parkinsonism, early and prominent autonomic dysfunction, and cerebellar dysfunction. Parkinsonism is predominant in MSA-P and cerebellar dysfunction is more prominent in MSA-C.[34] Red flags that suggest MSA are disproportionate anterocollis (chin on chest), severe lateroflexion of trunk, head and neck (Pisa syndrome), orofacial dystonia that are spontaneous or L-dopa induced, irregular action and postural tremor of hands, severe hypophonic quivering high pitched dysarthria, emotional incontinence, nocturnal strider, or excessive snoring. Dementia and behavioral changes are not usually seen.[35] MRI may be supportive. Patients with PSP present with progressive unexplained and unexpected falls or tendency to fall (backwards or in any direction) within 1 year of onset of parkinsonism.[36] Vertical supranuclear gaze paresis (any downward or moderate to severe upgaze) is characteristic. The parkinsonism is generally symmetric with axial more than appendicular rigidity, behavioral and cognitive changes, early dysphagia, and dysarthria.[37] MRI may be supportive. Cortico-basal degeneration (CBD) results in progressive cortical dysfunction such as asymmetric ideomotor or constructional apraxia, alien limb phenomenon, cortical sensory loss, focal myoclonus, apraxia of speech, or nonfluent aphasia. Extrapyramidal dysfunction such as asymmetric appedicular rigidity that is levodopa unresponsive and asymmetric appendicular dystonia is also part of the clinical picture.[38] MRI findings may support the diagnosis. Dementia with Lewy bodies (DLB) is a dementia syndrome associated with visual hallucinations, fluctuating levels of attention, and spontaneous parkinsonism. Dementia precedes motor symptoms or occurs within 1 year. The parkinsonism is symmetric with early gait and postural instability.[39] Moderate L-dopa response may be seen. In Alzheimer's disease, parkinsonism follows dementia, is symmetric, and rest tremor is rare. Dementia of AD is dominated by early and severe memory impairment. Clinical features which suggest an alternative diagnosis other than PD in a patient presenting with parkinsonism are listed in Table 3.
Table 3.
Baseline features that suggest an alternative diagnosis other than PD
There is no diagnostic test which can reliably differentiate PD from other causes of parkinsonism. Acute levodopa challenge (with 250 mg/25 mg of levodopa/carbidopa) and assessment for changes in Unified Parkinson's Disease Rating Scale Part III (UPDRS-III) score of 30% or more have a sensitivity of around 70% and specificity of around 80% for predicting an eventual diagnosis of PD.[40] Around 30% will have false positive or false negative results. Subcutaneous apomorphine challenge (1-4.5 mg of apomorphine given subcutaneously)[41] has similar utility but apomorphine is not freely available in India. Patients need to be pre-treated with domperidone for 2-3 days to prevent dopaminergic side effects.
Decreased smell in standardized smell identification tests (like the University of Pennsylvania Smell Identification Test - UPSIT) may be useful to discriminate PD from PSP and CBD. The smell is preserved in these conditions unlike PD in which there is moderate to severe impairment of smell. MSA and PD have overlapping levels of impairment.[42,43]
Significant overlap in levels of impairment does not allow reliable distinction between PD and atypical parkinsonism based on neuropsychological testing, electro-oculogram, sphincter and urethral EMG or autonomic function tests.[44]
Conventional and advanced MR modalities may help distinguish PD from atypical parkinsonism. However, the evidence is insufficient and MRI has low sensitivity.[44] Iodine-123 meta-iodobenzylguanidine (MIBG) cardiac imaging is normal in multiple system atrophy and PSP, while it is abnormal in PD.[45] However, the level of evidence is currently not considered high enough to recommend for routine diagnostic purposes. Hyperechogenicity of substantia nigra detected by brain ultrasonography has been shown to differentiate PD from atypical parkinsonism.[46–49] Evidence is not strong to recommend it for routine diagnostic purposes. Beta CIT and IBZM SPECT can differentiate PD from ET[44] but are not freely available.
References
- 1.Rao G, Fisch L, Srinivasan S, D’Amico F, Okada T, Eaton C, et al. Does this patient have Parkinson disease? JAMA. 2003;289:347–53. doi: 10.1001/jama.289.3.347. [DOI] [PubMed] [Google Scholar]
- 2.Dickson DW, Braak H, Duda JE, Duyckaerts C, Gasser T, Halliday GM, et al. Neuropathological assessment of Parkinson's disease: refining the diagnostic criteria. Lancet Neurol. 2009;8:1150–7. doi: 10.1016/S1474-4422(09)70238-8. [DOI] [PubMed] [Google Scholar]
- 3.Calne DB. Is “Parkinson's disease” one disease? J Neurol Neurosurg Psychiatry. 1989;52:18–21. doi: 10.1136/jnnp.52.suppl.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiner WJ. There is no Parkinson disease. Arch Neurol. 2008;65:705–8. doi: 10.1001/archneur.65.6.705. [DOI] [PubMed] [Google Scholar]
- 5.Mori H, Kondo T, Yokochi M, Matsumine H, Nakagawa-Hattori Y, Miyake T, et al. Pathologic and biochemical studies of juvenile parkinsonism linked to chromosome 6q. Neurology. 1998;51:890–2. doi: 10.1212/wnl.51.3.890. [DOI] [PubMed] [Google Scholar]
- 6.Becker G, Muller A, Braune S, Buttner T, Benecke R, Greulich W, et al. Early diagnosis of Parkinson's disease. J Neurol. 2002;249:III/40–8. doi: 10.1007/s00415-002-1309-9. [DOI] [PubMed] [Google Scholar]
- 7.Jankovic J, Rajput AH, McDermott MP. Perl DP for the Parkinson Study Group. The evolution of diagnosis in early Parkinson disease. Arch Neurol. 2000;57:369–70. doi: 10.1001/archneur.57.3.369. [DOI] [PubMed] [Google Scholar]
- 8.Hughes AJ, Daniel SE, Ben-Shlomo Y, Lees AJ. The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain. 2002;125:861–70. doi: 10.1093/brain/awf080. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhuri KR, Schapira AHV. Non-motor symptoms of Parkinson's disease: Dopaminergic pathophysiology and treatment. Lancet Neurol. 2009;8:464–74. doi: 10.1016/S1474-4422(09)70068-7. [DOI] [PubMed] [Google Scholar]
- 10.Webster Ross G, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, et al. Association of olfactory dysfunction with risk of future Parkinson's disease. Ann Neurol. 2008;63:167–73. doi: 10.1002/ana.21291. [DOI] [PubMed] [Google Scholar]
- 11.Schenck CH, Bundlie SR, Mahowald MW. Delayed emergence of a Parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder. Neurology. 1996;46:388–93. doi: 10.1212/wnl.46.2.388. [DOI] [PubMed] [Google Scholar]
- 12.Jankovic J, Schwartz KS, Ondo W. Re-emergent tremor of Parkinson's disease. J Neurol Neurosurg Psychiatry. 1999;67:646–50. doi: 10.1136/jnnp.67.5.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hughes AJ, Daniel SE, Blankson S, Lees AJ. A clinicopathologic study of 100 cases of Parkinson's disease. Arch Neurol. 1993;50:140–8. doi: 10.1001/archneur.1993.00540020018011. [DOI] [PubMed] [Google Scholar]
- 14.Lubarsky M, Juncos JL. Progressive supranuclear palsy: A current review. Neurologist. 2008;14:79–88. doi: 10.1097/NRL.0b013e31815cffc9. [DOI] [PubMed] [Google Scholar]
- 15.Wenning GK, Ebersbach G, Verny M, Chaudhuri KR, Jellinger K, McKee A, et al. Progression of falls in postmortem-confirmed parkinsonian disorders. Mov Disord. 1999;14:947–50. doi: 10.1002/1531-8257(199911)14:6<947::aid-mds1006>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 16.Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55:181–4. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hughes AJ, Ben-Shlomo Y, Daniel SE, Lees AJ. What features improve the accuracy of clinical diagnosis in Parkinson's disease: A clinicopathologic study. Neurology. 1992;42:1142–4. doi: 10.1212/wnl.42.6.1142. [DOI] [PubMed] [Google Scholar]
- 18.Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson's disease. Lancet Neurol. 2006;5:75–86. doi: 10.1016/S1474-4422(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 19.Siderowf A, Stern MB. Premotor Parkinson's disease: Clinical features, detection and prospects for treatment. Ann Neurol. 2008;64:S139–47. doi: 10.1002/ana.21462. [DOI] [PubMed] [Google Scholar]
- 20.Stephenson R, Siderowf A, Stern MB. Premotor Parkinson's disease: Clinical features and detection strategies. Mov Disord. 2009;24:S665–70. doi: 10.1002/mds.22403. [DOI] [PubMed] [Google Scholar]
- 21.Wolters EC, Francot C, Bergmans P, Winogrodzk A, Booij J, Berendse HW, et al. Preclinical (premotor) Parkinson's disease. J Neurol. 2000;247:II/103–9. [PubMed] [Google Scholar]
- 22.Hughes AJ, Colosimo C, Kleedorfer B, Daniel SE, Lees AJ. The dopaminergic response in multiple system atrophy. J Neurol Neurosurg Psychiatry. 1992;55:1009–13. doi: 10.1136/jnnp.55.11.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Sullivan SS, Massey LA, Williams DR, Silveira-Moriyama L, Kempster PA, Holton JL, et al. Clinical outcomes of progressive supranuclear palsy and multiple system atrophy. Brain. 2008;131:1362–72. doi: 10.1093/brain/awn065. [DOI] [PubMed] [Google Scholar]
- 24.Calne DB, Snow BJ, Lee C. Criteria for diagnosing Parkinson's disease. Ann Neurol. 1992;32:S125–7. doi: 10.1002/ana.410320721. [DOI] [PubMed] [Google Scholar]
- 25.Cohen O, Pullman S, Jurewicz E, Watner D, Louis ED. Rest tremor in patients with essential tremor: Prevalence, clinical correlates, and electrophysiologic characteristics. Arch Neurol. 2003;60:405–10. doi: 10.1001/archneur.60.3.405. [DOI] [PubMed] [Google Scholar]
- 26.Chaudhuri KR, Buxton-Thomas M, Dhawan V, Peng R, Meilak C, Brooks DJ. Long duration asymmetrical postural tremor is likely to predict development of Parkinson's disease and not essential tremor: Clinical follow up study of 13 cases. J Neurol Neurosurg Psychiatry. 2005;76:115–7. doi: 10.1136/jnnp.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prettyman R. Extrapyramidal signs in cognitively intact elderly people. Age Ageing. 1998;27:557–60. doi: 10.1093/ageing/27.5.557. [DOI] [PubMed] [Google Scholar]
- 28.Winikates J, Jankovic J. Clinical correlates of vascular parkinsonism. Arch Neurol. 1999;56:98–102. doi: 10.1001/archneur.56.1.98. [DOI] [PubMed] [Google Scholar]
- 29.Quinn NP. Parkinsonism: Recognition and differential diagnosis. BMJ. 1995;310:447–52. doi: 10.1136/bmj.310.6977.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diederich NJ, Goetz CG. Drug-induced movement disorders. Neurol Clin. 1998;16:125–40. doi: 10.1016/s0733-8619(05)70370-4. [DOI] [PubMed] [Google Scholar]
- 31.Montastruc JL, Llau ME, Rascol O, Senard JM. Drug-induced Parkinsonism: A review. Fundam Clin Pharmacol. 1994;8:293–306. doi: 10.1111/j.1472-8206.1994.tb00808.x. [DOI] [PubMed] [Google Scholar]
- 32.Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57:S4–16. doi: 10.1227/01.neu.0000168185.29659.c5. [DOI] [PubMed] [Google Scholar]
- 33.Krauss JK, Regel JP, Droste DW, Orszagh M, Borremans J, Vach W. Movement disorders in adult hydrocephalus. Mov Disord. 1997;12:53–60. doi: 10.1002/mds.870120110. [DOI] [PubMed] [Google Scholar]
- 34.Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias DJ, Trojanowski JQ, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;71:670–6. doi: 10.1212/01.wnl.0000324625.00404.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wenning GK, Ben-Shlomo Y, Hughes A, Daniel SE, Lees A, Quinn NP. What clinical features are most useful to distinguish definite multiple system atrophy from Parkinson's disease? J Neurol Neurosurg Psychiatry. 2000;68:434–40. doi: 10.1136/jnnp.68.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Litvan I, Mangone CA, McKee A, Verny M, Parsa A, Jellinger K, et al. Natural history of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) and clinical predictors of survival: A clinicopathological study. J Neurol Neurosurg Psychiatry. 1996;61:615–20. doi: 10.1136/jnnp.60.6.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nath U, Ben-Shlomo Y, Thomson RG, Lees AJ, Burn DJ. Clinical features and natural history of progressive supranuclear palsy: A clinical cohort study. Neurology. 2003;60:910–6. doi: 10.1212/01.wnl.0000052991.70149.68. [DOI] [PubMed] [Google Scholar]
- 38.Gibb WR, Luthert PJ, Marsden CD. Corticobasal degeneration. Brain. 1989;112:1171–92. doi: 10.1093/brain/112.5.1171. [DOI] [PubMed] [Google Scholar]
- 39.Geser F, Wenning GK, Poewe W, McKeith I. How to diagnose dementia with Lewi bodies: State of the art. Mov Disord. 2005;20:S11–20. doi: 10.1002/mds.20535. [DOI] [PubMed] [Google Scholar]
- 40.Merello M, Nouzeilles MI, Arce GP, Leiguarda R. Accuracy of acute levodopa challenge for clinical prediction of sustained long-term levodopa response as a major criterion for idiopathic Parkinson's disease diagnosis. Mov Disord. 2002;17:795–8. doi: 10.1002/mds.10123. [DOI] [PubMed] [Google Scholar]
- 41.Rossi P, Colosimo C, Moro E, Tonali P, Albanese A. Acute challenge with apomorphine and levodopa in Parkinsonism. Eur Neurol. 2000;43:95–101. doi: 10.1159/000008142. [DOI] [PubMed] [Google Scholar]
- 42.Doty RL, Golbe LI, McKeown DA, Stern MB, Lehrach CM, Crawford D. Olfactory testing differentiates between progressive supranuclear palsy and idiopathic Parkinson's disease. Neurology. 1993;43:962–5. doi: 10.1212/wnl.43.5.962. [DOI] [PubMed] [Google Scholar]
- 43.Wenning GK, Shephard B, Hawkes C, Petruckevitch A, Lees A, Quinn N. Olfactory function in atypical parkinsonian syndromes. Acta Neurol Scand. 1995;91:247–50. doi: 10.1111/j.1600-0404.1995.tb06998.x. [DOI] [PubMed] [Google Scholar]
- 44.Suchowersky O, Reich S, Perlmutter J, Zesiewicz T, Gronseth G, Weiner WJ. Practice parameter: Diagnosis and prognosis of new onset Parkinson disease (an evidence-based review).Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;66:968–75. doi: 10.1212/01.wnl.0000215437.80053.d0. [DOI] [PubMed] [Google Scholar]
- 45.Yoshita M. Differentiation of idiopathic Parkinson's disease from striatonigral degeneration and progressive supranuclear palsy using iodine- 123 meta-iodobenzylguanidine myocardial scintigraphy. J Neurol Sci. 1998;155:60–7. doi: 10.1016/s0022-510x(97)00278-5. [DOI] [PubMed] [Google Scholar]
- 46.Becker G, Seufert J, Bogdahn U, Reichmann H, Reiners K. Degeneration of substantia nigra in chronic Parkinson's disease visualized by transcranial color-coded real-time sonography. Neurology. 1995;45:182–4. doi: 10.1212/wnl.45.1.182. [DOI] [PubMed] [Google Scholar]
- 47.Berg D, Godau J, Walter U. Transcranial sonography in movement disorders. Lancet Neurol. 2008;7:1044–55. doi: 10.1016/S1474-4422(08)70239-4. [DOI] [PubMed] [Google Scholar]
- 48.Walter U, Niehaus L, Probst T, Benecke R, Meyer BU, Dressler D. Brain parenchyma sonography discriminates Parkinson's disease and atypical Parkinsonian syndromes. Neurology. 2003;60:74–7. doi: 10.1212/wnl.60.1.74. [DOI] [PubMed] [Google Scholar]
- 49.Walter U, Dressler D, Probst T, Wolters A, Abu-Mugheisib M, Wittstock M, et al. Transcranial brain sonography findings in discriminating between parkinsonism and idiopathic parkinson disease. Arch Neurol. 2007;64:1635–40. doi: 10.1001/archneur.64.11.1635. [DOI] [PubMed] [Google Scholar]


