Abstract
Context:
Research has established the relation between diabetes and depression. Both diabetes and anxiety/depression are independently associated with increased morbidity and mortality.
Aims:
The present study aims at assessing the prevalence of anxiety/depression among outpatients receiving treatment for type 2 diabetes.
Settings and Design:
The study was conducted in the endocrinology outpatient department of an urban tertiary care center.
Materials and Methods:
The instruments used included a semi-structured questionnaire, HbA1c levels, fasting blood glucose and postprandial blood glucose, Brief Patient Health Questionnaire, and Hospital Anxiety and Depression Scale (HADS).
Statistical Analysis Used:
Analysis was carried out using the SPSS version 16.0. Pearson's correlation coefficient was calculated to find out the correlations. ANOVA was carried out for the in between group comparisons.
Results:
There was a significant correlation between the HADS-Anxiety scale and Body Mass Index (BMI) with a correlation coefficient of 0.34 (P = 0.008). Also, a significant correlation existed between HADS-Depression scale and BMI (correlation coefficient, 0.36; P = 0.004). Significant correlation were observed between the duration of daily physical exercise and HADS-Anxiety (coefficient of correlation, -0.25; P = 0.04) scores. HADS-Anxiety scores were found to be related to HbA1c levels (correlation-coefficient, 0.41; P = 0.03) and postprandial blood glucose levels (correlation-coefficient, 0.51; P = 0.02).
Conclusions:
Monitoring of biochemical parameters like HbA1c and postprandial blood glucose levels and BMI could be a guide to development of anxiety in these patients. Also, physical exercise seems to have a protective effect on anxiety in those with type 2 diabetes mellitus.
Keywords: Anxiety, depression, type 2 diabetes mellitus
INTRODUCTION
The prevalence of Type 2 diabetes mellitus has been estimated to vary from 8 to 15% among the urban population in India, with a significantly increasing trend over the years.[1] Research has established the relation between diabetes and depression.[2] The prevalence of depression and anxiety in diabetes is considerably higher than normal population and ranges between 12 and 28%.[3–5] High glucose levels appear to be associated with negative mood ratings.[4,6] Anxiety and depression were found to be 58% and 45% of the outpatients with type 2 diabetes, respectively, in a recent multicenter study from Pakistan.[7] Both diabetes and anxiety/depression are independently associated with increased morbidity and mortality. Co-occurrence of these conditions adds to the cost, morbidity, and mortality.[8] Both depression and anxiety have been found to be associated with a negative impact on diabetes.[9] Presence of depressive symptoms significantly impairs the Health Related Quality of Life among those with type 2 diabetes.[10]
Diabetes has been associated with poor quality of life in previous Indian studies.[11,12] Also, the issues of stress and role of psychosocial factors in diabetes has also been addressed by Indian authors.[13,14]
There is limited literate on the association between depression/anxiety and type 2 diabetes from South-Asian countries.[15] The present study aims at assessing the prevalence of anxiety/depression among outpatients receiving treatment for type 2 diabetes. It also explores the correlation between different parameters of diabetes and anxiety/depression.
MATERIALS AND METHODS
The study was conducted in the endocrinology outpatient department of an urban tertiary care center. Making use of a cross-sectional study design, data were collected from the consecutive patients receiving treatment from the outpatient department for their type 2 diabetes mellitus. Only those subjects giving valid informed consent were included in the study. Based on the findings of a recent study from the region, a minimum sample size of 55 was required for the study to have adequate power.[7]
The instruments used included a semi-structured questionnaire to collect the sociodemographic profile and the details of the diabetes and its treatment. The details regarding the diabetes included the duration of the condition, duration of treatment, type of treatment being received, complications due to diabetes, family history of diabetes, and Body Mass Index (BMI). The level of diabetes control was assessed using the HbA1c levels, fasting blood glucose, and postprandial blood glucose.
Brief Patient Health Questionnaire (brief PHQ) was used to screen for the presence of depressive disorder and generalized anxiety disorder. Hospital Anxiety and Depression Scale (HADS) was used to score the anxiety and depression among the study subjects. Use of PHQ and HADS has been recommended for assessment of anxiety and depression in those with type 2 diabetes.[16] It is a validated and standardized instrument with good sensitivity and specificity.[17] It has been used in various previous studies on this issue and it allowed us to make comparisons with the previous findings.
The HADS comprises statements which the patient rates based on their experience over the past week. The 14 statements are relevant to either generalized anxiety (seven statements) or depression (seven statements). Each question has four possible responses. Responses are scored on a scale from 3 to 0.
Finally, information was collected on the physical exercise (walking/running/jogging) being done by the study subjects.
The study was approved by the local institutional ethical committee and the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and the Helsinki Declaration of 1975.
Analysis was carried out using the SPSS version 16.0. Descriptive statistics were carried out for different sociodemographic- and diabetes-related parameters. In between group difference were calculated for male and female study subjects using independent sample t test. Pearson's correlation coefficient was calculated to find out the correlation between different diabetes-related parameters and the scores on HADS-Anxiety and HADS-Depression scale. Additionally, ANOVA was carried out for the in between group comparisons. The level of significance for all the statistical tests was kept at P<0.05.
RESULTS
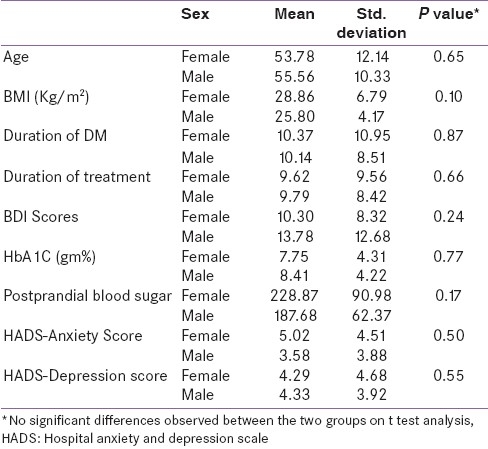
The study included 77 consecutive subjects with type 2 diabetes visiting the endocrinology outpatient department. The mean age of the study subjects was 54.66 (SD ± 11.22) years. The study sample comprised of 51% females (n = 39) and 49% males (n = 38). The mean duration of type 2 diabetes among the subjects was 10.25 (SD ± 9.75) years and the mean duration for treatment was 9.7 (SD ± 8.94) years [Table 1]. There was no significant difference between the males and females on different study variables as assessed by t test [Table 2].
Table 1.
Sociodemographic- and diabetes-related parameters of the study subjects
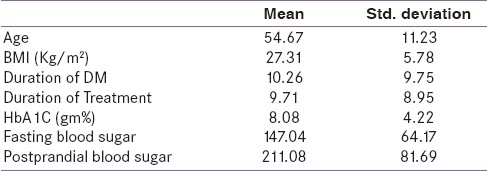
Table 2.
In-between group differences between male and female subjects for different study variables
The mean BMI was found to be 27.3 Kg/ m2 (SD ± 5.78) and the mean Hb1Ac levels were 8.08 (SD ± 4.22) gm%. The mean fasting and postprandial blood glucose level were found to be 147.04 (SD ± 64.17) and 211.08 (SD ± 81.69) mg/dl, respectively [Table 1].
Seventy-four percent (n = 57) of the subjects were without any diabetic complications. Six (7.8%) had retinopathy, five (6.5%) had neuropathy, and three (3.9%) had nephropathy. One case each had retinopathy with nephropathy and retinopathy with neuropathy and nephropathy.
The current psychiatry diagnosis was assessed using the Brief PHQ. Majority of the subjects (n = 61, 79%) were without any depressive or anxiety disorder. Depressive episode was present in 13 (16.9%) of the subjects and three (3.9%) had generalized anxiety disorder.
There was a significant correlation between the HADS-Anxiety scale and BMI with a correlation coefficient of 0.34 (P = 0.008). Also, a significant correlation existed between HADS-Depression scale and BMI (correlation coefficient, 0.36; P = 0.004).
Significant correlation was observed between the duration of daily physical exercise and HADS-Anxiety (coefficient of correlation, -0.25; P = 0.04) scores. However, no such association was found between the HADS-Depression and daily physical exercise [Table 3].
Table 3.
Correlation between hospital anxiety and depression scale-anxiety and hospital anxiety and depression scale-depression scales scores and body mass index and daily physical exercise
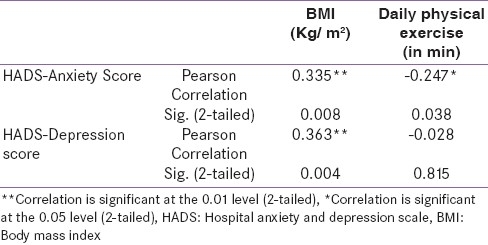
Using linear regression analysis, HADS-Anxiety scores were found to be related to HbA1c levels (correlation-coefficient, 0.41; P = 0.03) and postprandial blood glucose levels (correlation-coefficient, 0.51; P = 0.02).
DISCUSSION
The current study aimed at assessment of anxiety and depression among those with type 2 diabetes in Indian outpatient settings. Furthermore, we aimed at exploring the correlation among different diabetes-related parameters and anxiety/depression among the study subjects.
The study sample had both the sexes equally represented. The mean duration of type 2 diabetes among the subjects was 10.25 (SD ± 9.75) years and the mean duration for treatment was 9.7 (SD ± 8.94) years.
Majority of the study subjects (79%) were found to be free of anxiety and depression at the time of assessment. The prevalence of Depressive disorder and Generalized Anxiety Disorder were found to be 16.9% and 3.9%, respectively. Prevalence of depression was found to be 41% among patients with type II diabetes in a previous work from a tertiary care hospital in India. However, the mean duration of diabetes (eight years) was lesser in this study compared with the current study (10.25 years).[18] Some of the recent studies from Asia have reported the prevalence to be higher. The study by Khuwaja et al. found the prevalence of depression and anxiety at 44% and 58%, respectively.[7] However, the studies from the western countries have found the prevalence of both depression and anxiety to be relatively lower.[16,19,20] Collins et al (2009) found the prevalence of depression and anxiety to be 32.0% and 22.4%, respectively, as assessed by HADS in a cross-sectional study.[20]
No differences were observed between the males and females on the HADS score and the scores were comparable. Traditionally, female sex has been associated with higher rates of depression among the general population as well as those suffering from diabetes.[7,21–24] A previous study by Roupa et al. (2009) reported that sex was strongly related to the occurrence of anxiety and depression symptoms with women appearing to have three times the percentages of anxiety (62%) in comparison with men (21.5%). Also, there was a preponderance of evidence pointing that women in symptomatology of depression have a doubled percentage (41.4%) than men (17.8%).[22]
However, the comparable rates found in our study warrant a cautious approach while dealing with men with diabetes as the co-morbid depression and anxiety might get ignored, owing to the usual notion of lower rates among them.
Duration of diabetes has also been found to be associated with a higher prevalence of depression.[25,26] Chronic disease and disease duration were significantly associated with anxiety and depressive disorders in a study from Bahrain.[27] However, no such association was observed between depression/anxiety and duration of diabetes and duration of treatment of diabetes in the current study. These findings were similar to that of Raval et al. who failed to find any significant association between duration of diabetes and depression.[18] Rather, there was significant association of both HADS-Anxiety and HADS-Depression scores with the BMI (correlation coefficient of 0.34; P = 0.008 and correlation coefficient, 0.36; P = 0.004, respectively). BMI has been found to be a risk factor for diabetes and has also been associated with an increased prevalence of depression/anxiety.[7,27–29] Roupa et al. also found a higher rate of both anxiety and depression among individuals with higher BMI.[22] Obesity is often associated with a reduction in self-esteem, with economical, social, and psychological problems.[30] This might contribute to the negative affective states in these individuals. In a work by Krook et al., the participants reported an improved psychological status and reduced anxiety following a reduction in weight.[31] This lead to a significant improvement of clinical parameters. Hence, it needs to be explored further that whether the BMI is a better predictor of future occurrence of depression/anxiety in those with type 2 diabetes as compared to the total duration of illness. Also, one needs to consider the role of multiple modulators of the effect of duration of diabetes and the emergence of anxiety/depression.
Similarly, a significant correlation between the HADS-Anxiety scores and HbA1c levels (correlation-coefficient, 0.41; P = 0.03) and postprandial blood glucose levels (correlation-coefficient, 0.51; P = 0.02) also suggests that the quality of care and level of diabetes control might be a better predictor of occurrence of anxiety disorder among those having type 2 diabetes. The lack of association between HbA1c and the depression scores on HADS-Depression scale has been observed in previous studies as well. It has been postulated that high HbA1c is more strongly related to depressive affect and diabetes distress than to affective disorders.[32]
Protective effect of physical exercise on depression and anxiety has been reported.[33,34] The release of neurotransmitters including beta-endorphins has been proposed as an underlying mechanism for this protective effect of exercise. The current study also found an inverse correlation between the duration of physical exercise (in form of walking/jogging/running) and HADS-Anxiety scores (coefficient of correlation, -0.25; P = 0.04). Hence, encouraging physical exercise by those with type 2 diabetes would not only help control the body weight, blood glucose levels, and diabetes control, but also would contribute control of anxiety in this population group.
We have included a consecutive sample. Additionally, standardized instruments were used for assessment of anxiety and depression. Moreover, use of biochemical parameters of diabetes added to the objectivity of the findings.
However, the study has certain limitations. The cross-sectional nature of the study precludes deriving any causal association between different variables. Also, the subjects were not followed up and hence the future course of depressive and anxiety symptoms in relation to different variables cannot be commented up on. It would be informative to prospectively follow up these subjects in order to assess the time course of the symptoms and outcome.
CONCLUSIONS
Diabetes mellitus is a chronic condition with progressively increasing trends over the years. Prevalence of anxiety and depression tends to be higher among this population group. This adds to the cost, morbidity, and mortality. Association of anxiety/depression with type 2 diabetes could be detrimental to the care of either of these conditions and could worsen the prognosis. Monitoring of biochemical parameters like HbA1c and postprandial blood glucose levels and BMI could be a guide to development of anxiety in these patients. Also, physical exercise seems to have a protective effect on anxiety in those with type 2 diabetes mellitus.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gupta R, Misra A. Type 2 Diabetes in India: Regional Disparities. Br J Diab Vasc Dis. 2007;7:12–6. [Google Scholar]
- 2.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of co-morbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 3.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 4.Hermanns N, Scheff C, Kulzer B, Weyers P, Pauli P, Kubiak T, et al. Association of glucose levels and glucose variability with mood in Type 1 diabetic patients. Diabetologia. 2007;50:930–3. doi: 10.1007/s00125-007-0643-y. [DOI] [PubMed] [Google Scholar]
- 5.Shaban MC, Fosbury J, Kerr D, Cavan DA. The prevalence of depression and anxiety in adults with Type 1 diabetes. Diabet Med. 2006;23:1381–4. doi: 10.1111/j.1464-5491.2006.02012.x. [DOI] [PubMed] [Google Scholar]
- 6.Hislop AL, Fegan PG, Schlaeppi MJ, Duck M, Yeao BB. Prevalence and associations of psychological distress in young adults with Type 1 diabetes. Diabet Med. 2008;25:91–6. doi: 10.1111/j.1464-5491.2007.02310.x. [DOI] [PubMed] [Google Scholar]
- 7.Khuwaja AK, Lalani S, Dhanani R, Azam IS, Rafique G, White F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr. 2010;2:72. doi: 10.1186/1758-5996-2-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: A prospective cohort study. Diabetes Care. 2010;33:264–9. doi: 10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prisciandaro JJ, Gebregziabher M, Grubaugh AL, Gilbert GE, Echols C, Egede LE. Impact of psychiatric comorbidity on mortality in veterans with type 2 diabetes. Diabetes Technol Ther. 2011;13:73–8. doi: 10.1089/dia.2010.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ali S, Stone M, Skinner TC, Robertson N, Davies M, Khunti K. The association between depression and health-related quality of life in people with type 2 diabetes: A systematic literature review. Diabetes Metab Res Rev. 2010;26:75–89. doi: 10.1002/dmrr.1065. [DOI] [PubMed] [Google Scholar]
- 11.Sridhar GR, Madhu K, Veena S, Radha Madhavi P, Sangeetha B, Asha Rani S. Living with diabetes: Indian experience. Diab Met Syndr Clin Res Rev. 2007;1:181–7. [Google Scholar]
- 12.Shobhana R, Rama Rao P, Lavanya A, Padma C, Vijay V, Ramachandran A. Quality of life and diabetes integration among subjects with type 2 diabetes. J Assoc Physicians India. 2003;51:363–5. [PubMed] [Google Scholar]
- 13.Sridhar GR, Madhu K. Psychosocial and cultural issues in diabetes mellitus. Curr Sci. 2002;83:1556–64. [Google Scholar]
- 14.Madhu K, Sridhar GR. Stress Management in Diabetes Mellitus. Int J Diabetes Dev Ctries. 2005;25:7–11. [Google Scholar]
- 15.Sridhar GR. Psychiatric co-morbidity and diabetes. Indian J Med Res. 2007;125:311–20. [PubMed] [Google Scholar]
- 16.Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc. 2006;106(5 Suppl 2):S9–14. [PubMed] [Google Scholar]
- 17.Herrmann C. International experiences with the Hospital Anxiety and Depression scale -- a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 18.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 19.Bouwman V, Adriaanse MC, van ‘t Riet E, Snoek FJ, Dekker JM, Nijpels G. Depression, anxiety and glucose metabolism in the general Dutch population: The new Hoorn study. PloS One. 2010;5:e9971. doi: 10.1371/journal.pone.0009971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collins MM, Corcorant P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med. 2009;26:153–61. doi: 10.1111/j.1464-5491.2008.02648.x. [DOI] [PubMed] [Google Scholar]
- 21.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 22.Roupa Z, Koulouri A, Sotiropoulou P, Makrinika E, Marneras X, Lahana I, Gourni M. Anxiety and depression in patients with type 2 diabetes mellitus, depending on sex and body mass index. Health Sci J. 2009;3:32–40. [Google Scholar]
- 23.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systemic review. BMJ. 2004;328:794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Almawi W, Tamim H, Al-Sayed N, Arekat MR, Al-Khateeb GM, Baqer A, et al. Association of co-morbid depression, anxiety and stress disorders with type 2 diabetes in Bahrain, a country with a very high prevalence of type 2 diabetes. J Endocrinol Invest. 2008;31:1020–4. doi: 10.1007/BF03345642. [DOI] [PubMed] [Google Scholar]
- 25.Iype T, Shaji SK, Balakrishnan A, Charles D, Varghese A, Antony TP. Cognition in type 2 diabetes: Association with vascular risk factors, complications of diabetes and depression. Ann Indian Acad Neurol. 2009;12:25–7. doi: 10.4103/0972-2327.48848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perveen S, Otho MS, Siddiqi MN, Hatcher J, Rafique G. Association of depression with newly diagnosed type 2 diabetes among adults aged between 25 to 60 years in Karachi, Pakistan. Diabetol Metab Syndr. 2010;2:17. doi: 10.1186/1758-5996-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Almawi W, Tamim H, Al-Sayed N, Arekat MR, Al-Khateeb GM, Baqer A, Tutanji H, Kamel C. Association of comorbid depression, anxiety, and stress disorders with Type 2 diabetes in Bahrain, a country with a very high prevalence of Type 2 diabetes. J Endocrinol Invest. 2008;31:1020–4. doi: 10.1007/BF03345642. [DOI] [PubMed] [Google Scholar]
- 28.Takeuchi T, Nakao M, Nomura K, Inoue M, Tsurugano S, Shinozaki Y, et al. Association of the metabolic syndrome with depression and anxiety in Japanese men: A 1-year cohort study. Diabetes Metab Res Rev. 2009;25:762–7. doi: 10.1002/dmrr.1041. [DOI] [PubMed] [Google Scholar]
- 29.Hildrum B, Mykletun A, Midthjell K, Ismail K, Dahl AA. No association of depression and anxiety with the metabolic syndrome: The Norwegian HUNT study. Acta Psychiatr Scand. 2009;120:14–22. doi: 10.1111/j.1600-0447.2008.01315.x. [DOI] [PubMed] [Google Scholar]
- 30.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329:1008–12. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 31.Krook A, Holm I, Pettersson S, Wallberg-Henriksson H. Reduction of risk fact ors following lifestyle modification program in subjects with type 2 (non insulin depended) diabetes mellitus. Clin Physiol Funct Imaging. 2003;23:21–30. doi: 10.1046/j.1475-097x.2003.00463.x. [DOI] [PubMed] [Google Scholar]
- 32.Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with Type 2 diabetes. Diabet Med. 2008;25:1096–101. doi: 10.1111/j.1464-5491.2008.02533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hong X, Li J, Xu F, Tse LA, Liang Y, Wang Z, et al. Physical activity inversely associated with the presence of depression among urban adolescents in regional China. BMC Public Health. 2009;9:148. doi: 10.1186/1471-2458-9-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khuwaja AK, Qureshi R, Azam SI. Prevalence and factors associated with anxiety and depression among family practitioners in Karachi, Pakistan. J Pak Med Assoc. 2004;54:45–9. [PubMed] [Google Scholar]


