Abstract
Background:
Type 2 diabetes mellitus is the most prevalent form of diabetes worldwide. In western countries majority of the cases are obese. The scenario may be different in certain parts of India. Various studies have reported a high prevalence of lean type 2 diabetes mellitus with a body mass index < 19 kg/m2.
Materials and Methods:
We evaluated 100 cases of lean type 2 diabetes mellitus (62 males and 38 females).
Results and Conclusion:
The mean duration of diabetes was 51.7 months (range 5-180 months). The glycemic control was poor according to standard guidelines. The majority of them showed response to oral hypoglycemic agents. Secondary failure to oral hypoglycemic agents was seen in 27 patients. The prevalence of microvascular complications was much higher than macrovascular complications. Neuropathy was the commonest complication seen in 70%, followed by retinopathy in 25%. Only 12 patients had hypertension, one had coronary artery disease and two had cerebrovascular accident. Lipid profile was not significantly deranged in our patients.
Keywords: Lean type diabetesmellitus, macrovasuclar, microvascular
INTRODUCTION
Type 2 diabetes mellitus is the most prevalent form of diabetes seen worldwide. Epidemiological data over the past decades have shown that the pattern and profile of type 2 diabetes mellitus are very different in India compared to the West.[1] In Europe and America majority of type 2 diabetes are obese. In 1965 Tripathy and Kar highlighted that 27% of elderly diabetics were lean.[2] Following that various studies in India have reported a prevalence of low body weight/lean (Body mass index, BMI<19 kg/m2) type 2 diabetes mellitus ranging from 1.6% to 26%.[3–7] The clinical and biochemical profile of these patients are different from classic type 2 diabetes mellitus.[5,6,8,9] These patients are neither related clinically or pathophysiologically to latent autoimmune diabetes of adults (LADA). Markers of autoimmune destruction of β-cells are absent in the vast majority of these patients.[5,10,11] Homeostatic model assessments by Das et al., suggest that they are typical cases of type 2diabetes and the low body weight does not reflect poor beta cell function or loss of body weight due to long-standing uncontrolled diabetes.[11] However, more recent study by Bera et al., suggested poor β-cell function in such patients.[12]
With this background, we studied the clinical and biochemical profile of lean type 2 diabetic patients in Manipur, as there is no published data from our part of the country.
Aims and objectives
To study the clinical and biochemical profile of lean type 2 diabetes mellitus.
MATERIALS AND METHODS
Cross-sectional study carried out in the Diabetes Clinic, Department of Medicine, Regional Institute of Medical Sciences Hospital, Imphal, Manipur. One hundred cases of lean type 2 diabetes mellitus were evaluated.
Inclusion criteria
All patients with type 2 diabetes mellitus irrespective of age, sex with BMI less than 19. Diagnosis of diabetes mellitus was based on American Diabetes Association (ADA) criteria.
Exclusion criteria
Type 2 diabetes mellitus with BMI more than 19.
Any seriously ill patient whose sensorium and higher functions are altered.
Patients suffering from acute myocardial infarction, renal failure, liver disease, critical illness, tuberculosis, carcinoma and any severe infection.
Methods
A detailed history of clinical information including the age, sex and intercurrent illness was taken. Anthropometric parameters – height, weight, waist and hip circumference were recorded and clinical examination performed to detect diabetic complications.
Glycemic status was assessed using fasting and two hours postprandial blood glucose (BG) and HbA1c (glycosylated haemoglobin). HbA1c level was estimated by Fast Ion Exchange Resin separation method using REF 10657 kit from Human Wiesbaden, Germany. Lipid profile was assessed for each patient. Urinary microalbumin was examined using dipstick. Nephropathy was diagnosed on basis of persistent proteinuria in the absence of urinary tract infection. Fundus examination was done by expert ophthalmologist. Neuropathy was diagnosed on the basis of subjective symptoms, objective evidence of absence of ankle jerk, glove stocking type of anesthesia or monofilament testing. Patients were considered to have ischemic heart disease based on electrocardiogram (ECG).
RESULTS
In this study 100 cases of lean diabetic patients were evaluated from August 2008 to 2010. Among the patients 62 (62%) were males and 38 (38%) were females. The age of patients ranged from 32 to 75 years with a mean of 53 years.
Clinical profiles
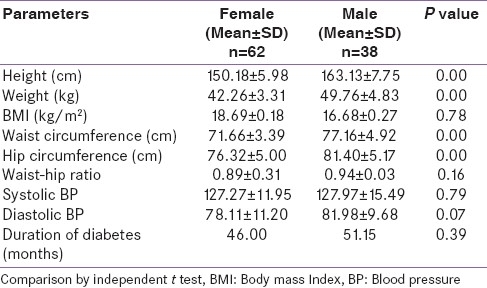
In the present study, the mean age of the patient was 53 years (range 32-75 years). The mean duration of diabetes mellitus is 51.7 months (range 5-180 months). The mean height of patients was 158.2 cm ± 9.5 and weight was 46.9 kg ± 5.6 with BMI of 18.7 kg/m2 ± 0.2. The mean waist and hip circumferences was 75.1cm ± 5.1 and 79.5 cm ± 5.7, respectively, with waist-hip ratio of 0.9 ± 0.2, the systolic and diastolic blood pressure are 127.6 ±14.2 and 80.5 ±10.4. The clinical parameters according to sex distribution are shown in Table 1.
Table 1.
Clinical parameters in male and female lean diabetic patients
In the present study secondary OHA (oral hypoglycemic agent) failure was seen in 27 patients (27%) (20 males and 7 females).
Biochemical parameters
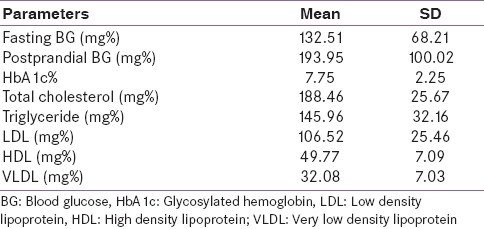
The mean fasting blood glucose in the present study was 132.5 ± 68.2 mg% and postprandial was 193.9 ± 100.1 mg%. The mean HbA1c was 7.7 ± 2.2%. Total cholesterol was 188.5 ± 25.8 mg%, triglyceride 146.0 ± 32.2 mg%, low density lipoprotein (LDL) 106.5 ± 25.5 mg%, high density lipoprotein (HDL) 49.8 ± 7.1 mg% and very low density lipoprotein (VLDL) 32.1 ± 7.0 mg% as shown in Table 2. There was no significant difference in biochemical parameters between the male and the female lean diabetic patients.
Table 2.
Biochemical parameters of lean diabetic patients
Diabetics with OHA failure had higher blood glucose (fasting BG-192.8± 89.6 vs 119.2 ± 40.4; postprandial BG-291.6 ± 127.5 vs 157.8 ± 54.6; P=0.00), higher HbA1c (9.9 ± 2.9 vs 6.9 ± 1.2; P=0.00) and total cholesterol level (202.4 ± 33.0 vs 183.3 ± 20.3; P=0.001) than the diabetics without OHA failure significantly. However, there was no significant difference in other parameters between the patients with and without OHA failure.
Diabetic complications
It was found that the prevalence of peripheral neuropathy (70%) and retinopathy (25%) is higher among the lean diabetic patients as compared to macrovascular complications. When data of both micro and macrovascular complications were clubbed together in the present study, it was found that 73% of the patients suffers from either micro or macrovascular complications or both. Among the 100 patients, 12 patients (12%) had hypertension one (1%) had coronary artery disease and two patients (2%) had cerebrovascular accident. And 8 patients presented with foot or systemic infections.
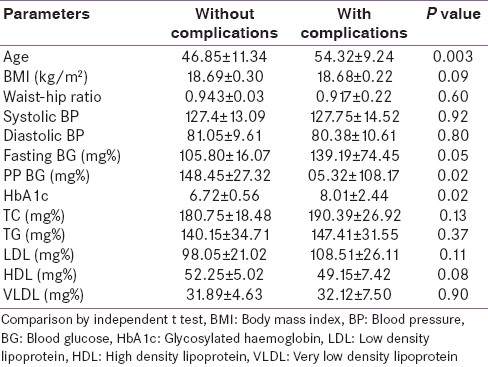
Comparison of clinical and biochemical parameters between those with complications and without complications is shown in Table 3.
Table 3.
Comparison of parameters between lean diabetic patients with and without complications
Neuropathy
In the present study 70 patients (70%) were suffering from peripheral neuropathy. And the prevalence of neuropathy was found to be higher in the older patients (54.3 ± 9.4 vs 49.5 ± 11.0; P=0.03), with lesser body weight (45.8 ± 5.2 vs 49.4 ± 5.8; P=0.003), shorter (156.4 ± 8.8 vs 162.4 ± 9.9; P=0.003) and narrower waist circumference (74.3 ± 5.2 vs 77.0 ± 4.4; P=0.02). There was no statistically significant difference in other parameters between those with neuropathy and those without neuropathy.
Retinopathy
Retinopathy was seen in 25 cases (25%). The prevalence was found to be higher in older age group (56.3 ± 8.9 vs 51.7 ± 10.2; P=0.05), higher blood glucose level [(fasting blood glucose - 270.7±103.2 vs 115.9 ± 40.7; P=0.00; postprandial blood glucose - 270.7 ± 152.2 vs 168.4 ± 56.8; P=0.00), and higher HbA1c (9.3 ± 3.3 vs 7.2 ± 1.4; P=0.00)]. Retinopathy was also seen more in patients who are taller, heavier, with broader waist circumference, higher blood pressure and longer duration of diabetes but the findings were not significant statistically.
Nephropathy
Thirteen patients (13%) were suffering from nephropathy. The prevalence of nephropathy was found to be higher in taller (163.8 ± 11.1 vs 157.4 ± 9.0; P=0.02) patients with higher waist (78.0±6.6 vs 74.6 ± 4.8; P=0.03) and hip circumference (82.8 ± 5.6 vs 79.0 ± 5.5; P=0.02), higher blood glucose level [(fasting blood glucose - 235.3 ± 99.5 vs 117.1 ± 46.2; P=0.00; postprandial blood glucose - 333.5 ± 128.7 vs 173.1 ± 76.3; P=0.00), high HbA1c (11.4 ± 2.9 vs 7.2 ± 1.5; P=0.00)], higher total cholesterol (211.5 ± 38.1 vs 185.0 ± 21.5; P=0.00) and triglyceride (178.3 ± 50.9 vs 141.1 ± 25.4; P=0.00) and lower high density lipoprotein level (42.8±9.6 vs 50.8 ± 6.0; P=0.00). The findings with the other parameters were not significant.
DISCUSSION
In the present study of 100 lean type 2 diabetic patients, there were 62 males and 38 females. The mean age of the patient was 53 years and the mean duration of diabetes ranged was 52 months. The mean age of our patients is older than that of Das et al.,[8] who reported a mean age of 48 years and Sinharoy et al.,[9] reported a mean age of 47 years. However, the study Mukhyaprana et al.,[6] reported higher mean age of 60 years.
The glycemic profile of our cases is much better than reported by various authors.[5,6,8,9] These may be because most of our patients are from the vicinity of our hospital and are on regular follow-up.
A high prevalence of microvascular complications [peripheral neuropathy (70%), retinopathy (25%) and nephropathy (13%)] was observed in our patients. Mohan et al.,[5] in their study, also found a higher prevalence of microvascular complications among lean type 2 diabetic patients, compared to diabetics with ideal body weight or obese diabetic patients. The prevalence of complications they found was neuropathy (male-44.6%, female-38.6%) retinopathy (male-37.3%, female-33.3%) and nephropathy (male-4.7%, female-4.4%). Mukhyaparna et al.,[6] reported 35%, 6.6% and 27% prevalence of neuropathy, nephropathy and retinopathy, respectively. Sinharoy et al.,[9] reported the prevalence of neuropathy to be 32%, nephropathy 28% and retinopathy 28%.
Patients with diabetic complications were more aged and had significantly higher blood glucose levels compared to patients without complications in our study. Prevalence of microvascular complications among lean type 2 diabetics are related to duration of diabetes and glycemic control.[6,9] In the study by Singh et al.,[13] patients with diabetic retinopathy had significantly higher prevalence of microalbuminuria but fasting glucose and duration of diabetes were not significantly different from those without retinopathy. Low prevalence of macrovascular complications and hypertension as seen in our study had been reported by various authors. The probable reason for low incidence of ischemic heart disease and hypertension is less obesity in these patients.[6]
Secondary OHA failure was observed in 27% of the patients. In the study by Mohan et al.,[5] nearly 47% of male and 53% of female lean type 2diabetes were successfully treated with diet and OHAs even after a mean duration of 9 years of diabetes. Serum insulin level is lower in lean type 2 diabetics than in obese type 2 diabetics but there was no significant difference in c-peptide level which may be due to excess extraction of insulin by the liver.[8]
In the present study it was observed that the lipid profile was not much deranged. Das et al.,[8] revealed the conspicuous absence of hyperlipidemia in their patients. HDL levels were high among lean diabetic patients. High HDL has been postulated to be due excess hepatic lipase activity.[14] Ikeda et al.,[15] showed no major difference irrespective of glycemic status in lean type 2 diabetics (BMI<25kg/m2). Mukhyaprana et al.,[6] also showed normal lipid profile in their patients. Whereas, study by Sinharoy et al.,[9] showed elevated TG in lean type 2 diabetics compared to normal weight and obese type 2 diabetics. LDL was also elevated although lower than the other two groups.
CONCLUSIONS
The lean type 2 diabetes mellitus is a distinct clinical entity. The clinical presentation and profile of associated complications is different in lean patients of type 2 diabetes, as compared to obese or non-lean diabetics. The prevalence of microvascular complications is much higher than macrovascular complications.The prevalence of peripheral neuropathy is highest, followed by retinopathy and nephropathy. Patients who are more aged or have poor glycemic control are more likely to develop diabetic complications. Lean type 2 diabetics can usually achieve glycemic control with OHAs, but secondary OHA failure is observed in 27% of the patients.
Limitations of the study
The number of patients in our study is small. We did not evaluate for autonomic neuropathy, and also we did not subject our patients to echocardiography or stress test in the absence of clinical suspicion of ischemic heart disease. This may have led to underreporting of neuropathy and coronary artery disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hoet JJ, Tripathy BB. Report of the international workshop on types of diabetes peculiar to the tropics. Diabetes Care. 1996;19:1014. [PubMed] [Google Scholar]
- 2.Tripathy BB, Kar BC. Observations and clinical patterns of diabetes in India. Diabetes. 1965;14:404–12. doi: 10.2337/diab.14.7.404. [DOI] [PubMed] [Google Scholar]
- 3.Samal KC, Das S, Agarwal BN, Panda NC, Tripathy BB. Nutritional status and profile of NIDDM of recent onset. J Diab Assoc India. 1998;28:99–101. [Google Scholar]
- 4.Ramchandran A, Snehalatha C, Latha E, Vijay V, Vishwanathan M. Rising prevalence of NIDDM in urban population in India. Diabetologia. 1997;40:232–7. doi: 10.1007/s001250050668. [DOI] [PubMed] [Google Scholar]
- 5.Mohan V, Vijayaprabha R, Rema M, Premalatha G, Poongothai S, Deepa R, et al. Clinical profile of lean NIDDM in South India. Diabetes Res Clin Pract. 1997;38:101–8. doi: 10.1016/s0168-8227(97)00088-0. [DOI] [PubMed] [Google Scholar]
- 6.Mukhyaprana MP, Vidyasagar S, Shashikiran U. Clinical prolife of type 2 diabetes mellitus and body mass index- Is there any correlation. Calicut Med J. 2004;2:e3. [Google Scholar]
- 7.Thakural HS, Kaur N, Mahajan DS, Kaur HP, Bilkhu N. Prevalence of lean diabetes mellitus type 2. APICON 2009 Abstract. [Last accessed on 2011 Apr 15]. Available from: http://www.japi.org/march_2009/diabetes.htm .
- 8.Das S, Samal SC, Baliarsinha AK, Tripathy BB. Lean (underweight) NIDDM – Peculiarities and differences in metabolic and hormonal status- A pilot study. J Assoc Physicians India. 1995;43:339–42. [PubMed] [Google Scholar]
- 9.Sinharoy K, Mandal L, Chakrabarti S, Paul UK, Bandyopadhyay R, Basu AK. A study on clinical and biochemical profile of low body weight type 2 diabetes mellitus. J Indian Med Assoc. 2008;106:747–50. [PubMed] [Google Scholar]
- 10.Unnikrishnan AG, Singh SK, Sanjeevi CB. Prevalence of GAD65 antibodies in lean subjects with type 2 diabetes. Ann N Y Acad Sci. 2004;1037:118–21. doi: 10.1196/annals.1337.018. [DOI] [PubMed] [Google Scholar]
- 11.Das S, Bhoi SK, Baliarsinha AK, Baig AA. Autoimmunity, insulin resistance and beta cell function in subjects with low weight type 2 diabetes mellitus. Metab Syndr Relat Disord. 2007;5:136–41. doi: 10.1089/met.2006.0024. [DOI] [PubMed] [Google Scholar]
- 12.Bera C, Pratyush DD, Tiwari S, Rastogi A, Naik DB, Jain P, et al. Study on insulin resistance and beta cell dysfunction in lean type 2 diabetes mellitus. [Last accessed on 2009];J Assoc Physicians India. 2009 57 Available from: http://www.japi.org/december_2009/diabetes.html . [Google Scholar]
- 13.Singh SK, Behre A, Singh MK. Diabetic retinopathy and microalbuminuria in lean type 2 diabetes mellitus. J Assoc Physicians India. 2001;49:439–41. [PubMed] [Google Scholar]
- 14.Baynes C, Henderson AD, Anyaoku V. The role of insulin sensitivity and hepatic lipase in the dyslipidemia of type 2 diabetes. Diabet Med. 1991;8:560–6. doi: 10.1111/j.1464-5491.1991.tb01652.x. [DOI] [PubMed] [Google Scholar]
- 15.Ikeda T, Ochi H, Ohtani I, Fujiyama K, Hoshino T, Tanaka Y, et al. Serum lipid and apolipoprotein levels in non-hypertensive lean NIDDM patients. J Intern Med. 1991;230:131–4. doi: 10.1111/j.1365-2796.1991.tb00420.x. [DOI] [PubMed] [Google Scholar]


