Abstract
This review describes normal bone anatomy and physiology as an introduction to the subsequent articles in this section that discuss clinical applications of iliac crest bone biopsy. The normal anatomy and functions of the skeleton are reviewed first, followed by a general description of the processes of bone modeling and remodeling. The bone remodeling process regulates the gain and loss of bone mineral density in the adult skeleton and directly influences bone strength. Thorough understanding of the bone remodeling process is critical to appreciation of the value of and interpretation of the results of iliac crest bone histomorphometry. Osteoclast recruitment, activation, and bone resorption is discussed in some detail, followed by a review of osteoblast recruitment and the process of new bone formation. Next, the collagenous and noncollagenous protein components and function of bone extracellular matrix are summarized, followed by a description of the process of mineralization of newly formed bone matrix. The actions of biomechanical forces on bone are sensed by the osteocyte syncytium within bone via the canalicular network and intercellular gap junctions. Finally, concepts regarding bone remodeling, osteoclast and osteoblast function, extracellular matrix, matrix mineralization, and osteocyte function are synthesized in a summary of the currently understood functional determinants of bone strength. This information lays the groundwork for understanding the utility and clinical applications of iliac crest bone biopsy.
The Skeleton
The adult human skeleton has a total of 213 bones, excluding the sesamoid bones (1). The appendicular skeleton has 126 bones, axial skeleton 74 bones, and auditory ossicles six bones. Each bone constantly undergoes modeling during life to help it adapt to changing biomechanical forces, as well as remodeling to remove old, microdamaged bone and replace it with new, mechanically stronger bone to help preserve bone strength.
The four general categories of bones are long bones, short bones, flat bones, and irregular bones. Long bones include the clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges. Short bones include the carpal and tarsal bones, patellae, and sesamoid bones. Flat bones include the skull, mandible, scapulae, sternum, and ribs. Irregular bones include the vertebrae, sacrum, coccyx, and hyoid bone. Flat bones form by membranous bone formation, whereas long bones are formed by a combination of endochondral and membranous bone formation.
The skeleton serves a variety of functions. The bones of the skeleton provide structural support for the rest of the body, permit movement and locomotion by providing levers for the muscles, protect vital internal organs and structures, provide maintenance of mineral homeostasis and acid-base balance, serve as a reservoir of growth factors and cytokines, and provide the environment for hematopoiesis within the marrow spaces (2).
The long bones are composed of a hollow shaft, or diaphysis; flared, cone-shaped metaphyses below the growth plates; and rounded epiphyses above the growth plates. The diaphysis is composed primarily of dense cortical bone, whereas the metaphysis and epiphysis are composed of trabecular meshwork bone surrounded by a relatively thin shell of dense cortical bone.
The adult human skeleton is composed of 80% cortical bone and 20% trabecular bone overall (3). Different bones and skeletal sites within bones have different ratios of cortical to trabecular bone. The vertebra is composed of cortical to trabecular bone in a ratio of 25:75. This ratio is 50:50 in the femoral head and 95:5 in the radial diaphysis.
Cortical bone is dense and solid and surrounds the marrow space, whereas trabecular bone is composed of a honeycomb-like network of trabecular plates and rods interspersed in the bone marrow compartment. Both cortical and trabecular bone are composed of osteons.
Cortical osteons are called Haversian systems. Haversian systems are cylindrical in shape, are approximately 400 mm long and 200 mm wide at their base, and form a branching network within the cortical bone (3). The walls of Haversian systems are formed of concentric lamellae. Cortical bone is typically less metabolically active than trabecular bone, but this depends on the species. There are an estimated 21 × 106 cortical osteons in healthy human adults, with a total Haversian remodeling area of approximately 3.5 m2. Cortical bone porosity is usually <5%, but this depends on the proportion of actively remodeling Haversian systems to inactive cortical osteons. Increased cortical remodeling causes an increase in cortical porosity and decrease in cortical bone mass. Healthy aging adults normally experience thinning of the cortex and increased cortical porosity.
Cortical bone has an outer periosteal surface and inner endosteal surface. Periosteal surface activity is important for appositional growth and fracture repair. Bone formation typically exceeds bone resorption on the periosteal surface, so bones normally increase in diameter with aging. The endosteal surface has a total area of approximately 0.5 m2, with higher remodeling activity than the periosteal surface, likely as a result of greater biomechanical strain or greater cytokine exposure from the adjacent bone marrow compartment. Bone resorption typically exceeds bone formation on the endosteal surface, so the marrow space normally expands with aging.
Trabecular osteons are called packets. Trabecular bone is composed of plates and rods averaging 50 to 400 mm in thickness (3). Trabecular osteons are semilunar in shape, normally approximately 35 mm thick, and composed of concentric lamellae. It is estimated that there are 14 × 106 trabecular osteons in healthy human adults, with a total trabecular area of approximately 7 m2.
Cortical bone and trabecular bone are normally formed in a lamellar pattern, in which collagen fibrils are laid down in alternating orientations (3). Lamellar bone is best seen during microscopic examination with polarized light, during which the lamellar pattern is evident as a result of birefringence. The mechanism by which osteoblasts lay down collagen fibrils in a lamellar pattern is not known, but lamellar bone has significant strength as a result of the alternating orientations of collagen fibrils, similar to plywood. The normal lamellar pattern is absent in woven bone, in which the collagen fibrils are laid down in a disorganized manner. Woven bone is weaker than lamellar bone. Woven bone is normally produced during formation of primary bone and may also be seen in high bone turnover states such as osteitis fibrosa cystica, as a result of hyperparathyroidism, and Paget's disease or during high bone formation during early treatment with fluoride.
The periosteum is a fibrous connective tissue sheath that surrounds the outer cortical surface of bone, except at joints where bone is lined by articular cartilage, which contains blood vessels, nerve fibers, and osteoblasts and osteoclasts. The periosteum is tightly attached to the outer cortical surface of bone by thick collagenous fibers, called Sharpeys’ fibers, which extend into underlying bone tissue. The endosteum is a membranous structure covering the inner surface of cortical bone, trabecular bone, and the blood vessel canals (Volkman's canals) present in bone. The endosteum is in contact with the bone marrow space, trabecular bone, and blood vessel canals and contains blood vessels, osteoblasts, and osteoclasts.
Bone Growth, Modeling, and Remodeling
Bone undergoes longitudinal and radial growth, modeling, and remodeling during life. Longitudinal and radial growth during growth and development occurs during childhood and adolescence. Longitudinal growth occurs at the growth plates, where cartilage proliferates in the epiphyseal and metaphyseal areas of long bones, before subsequently undergoing mineralization to form primary new bone.
Modeling is the process by which bones change their overall shape in response to physiologic influences or mechanical forces, leading to gradual adjustment of the skeleton to the forces that it encounters. Bones may widen or change axis by removal or addition of bone to the appropriate surfaces by independent action of osteoblasts and osteoclasts in response to biomechanical forces. Bones normally widen with aging in response to periosteal apposition of new bone and endosteal resorption of old bone. Wolff's law describes the observation that long bones change shape to accommodate stresses placed on them. During bone modeling, bone formation and resorption are not tightly coupled. Bone modeling is less frequent than remodeling in adults (4). Modeling may be increased in hypoparathyroidism (5), renal osteodystrophy (6), or treatment with anabolic agents (7).
Bone remodeling is the process by which bone is renewed to maintain bone strength and mineral homeostasis. Remodeling involves continuous removal of discrete packets of old bone, replacement of these packets with newly synthesized proteinaceous matrix, and subsequent mineralization of the matrix to form new bone. The remodeling process resorbs old bone and forms new bone to prevent accumulation of bone microdamage. Remodeling begins before birth and continues until death. The bone remodeling unit is composed of a tightly coupled group of osteoclasts and osteoblasts that sequentially carry out resorption of old bone and formation of new bone. Bone remodeling increases in perimenopausal and early postmenopausal women and then slows with further aging, but continues at a faster rate than in premenopausal women. Bone remodeling is thought to increase mildly in aging men.
The remodeling cycle is composed of four sequential phases. Activation precedes resorption, which precedes reversal, which precedes formation. Remodeling sites may develop randomly but also are targeted to areas that require repair (8,9). Remodeling sites are thought to develop mostly in a random manner.
Activation involves recruitment and activation of mononuclear monocyte-macrophage osteoclast precursors from the circulation (10), lifting of the endosteum that contains the lining cells off the bone surface, and fusion of multiple mononuclear cells to form multinucleated preosteoclasts. Preosteoclasts bind to bone matrix via interactions between integrin receptors in their cell membranes and RGD (arginine, glycine, and asparagine)-containing peptides in matrix proteins, to form annular sealing zones around bone-resorbing compartments beneath multinucleated osteoclasts.
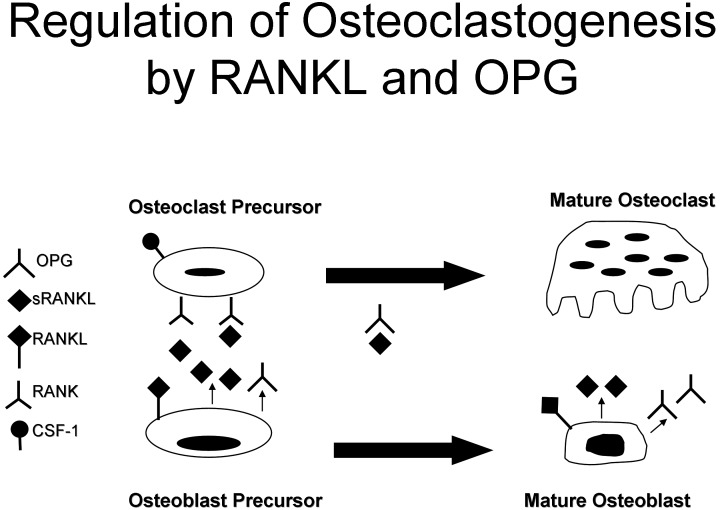
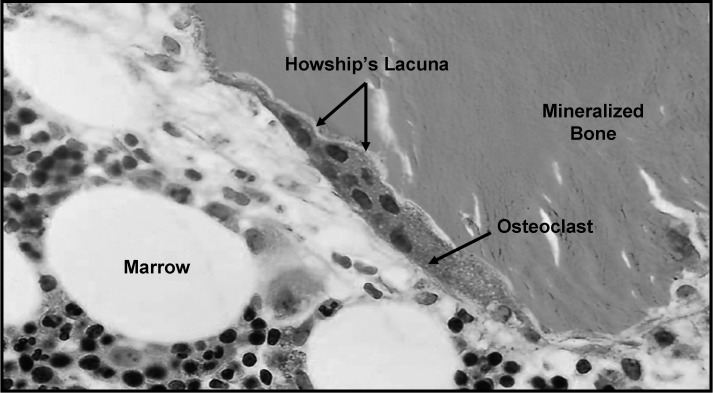
Osteoclast-mediated bone resorption takes only approximately 2 to 4 wk during each remodeling cycle. Osteoclast formation, activation, and resorption are regulated by the ratio of receptor activator of NF-κB ligand (RANKL) to osteoprotegerin (OPG; Figure 1), IL-1 and IL-6, colony-stimulating factor (CSF), parathyroid hormone, 1,25-dihydroxyvitamin D, and calcitonin (11,12). Resorbing osteoclasts secrete hydrogen ions via H+-ATPase proton pumps and chloride channels in their cell membranes into the resorbing compartment to lower the pH within the bone-resorbing compartment to as low as 4.5, which helps mobilize bone mineral (13). Resorbing osteoclasts secrete tartrate-resistant acid phosphatase, cathepsin K, matrix metalloproteinase 9, and gelatinase from cytoplasmic lysosomes (14) to digest the organic matrix, resulting in formation of saucer-shaped Howship's lacunae on the surface of trabecular bone (Figure 2) and Haversian canals in cortical bone. The resorption phase is completed by mononuclear cells after the multinucleated osteoclasts undergo apoptosis (15,16).
Figure 1.
Regulation of osteoclastogenesis by receptor activator of NF-κB ligand (RANKL) and osteoprotegerin (OPG): Colony-stimulating factor 1 (CSF-1) normally stimulates osteoclast recruitment. Two forms of RANKL are produced by osteoblasts and osteoblast precursors to stimulate osteoclast recruitment and activation. The membrane-bound form directly interacts with membrane-bound RANK molecules on adjacent osteoclast precursors. The soluble form is released from osteoblasts or osteoblast precursors to diffuse through the intercellular space and interact with membrane-bound RANK molecules on nearby osteoclast precursors. OPG acts as a decoy receptor to prevent RANKL or sRANKL from interacting with RANK. The ratio between RANKL and OPG produced by osteoblasts and osteoblast precursors controls RANKL-stimulated osteoclastogenesis.
Figure 2.
Multinucleated osteoclasts resorb bone to form resorption pits known as Howship's lacunae.
During the reversal phase, bone resorption transitions to bone formation. At the completion of bone resorption, resorption cavities contain a variety of mononuclear cells, including monocytes, osteocytes released from bone matrix, and preosteoblasts recruited to begin new bone formation. The coupling signals linking the end of bone resorption to the beginning of bone formation are as yet unknown. Proposed coupling signal candidates include bone matrix—derived factors such as TGF-β, IGF-1, IGF-2, bone morphogenetic proteins, PDGF, or fibroblast growth factor (17–19). TGF-β concentration in bone matrix correlates with histomorphometric indices of bone turnover and with serum osteocalcin and bone-specific alkaline phosphatase. TGF-β released from bone matrix decreases osteoclast resorption by inhibiting RANKL production by osteoblasts. The reversal phase has also been proposed to be mediated by the strain gradient in the lacunae (20,21). As osteoclasts resorb cortical bone in a cutting cone, strain is reduced in front and increased behind, and in Howship's lacunae, strain is highest at the base and less in surrounding bone at the edges of the lacunae. The strain gradient may lead to sequential activation of osteoclasts and osteoblasts, with osteoclasts activated by reduced strain and osteoblasts by increased strain. The osteoclast itself has also been proposed to play a role during reversal (22).
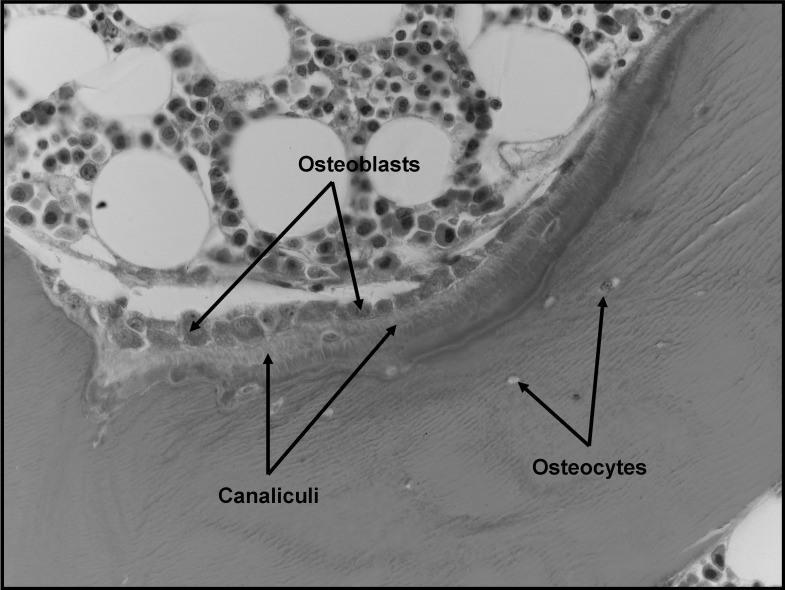
Bone formation takes approximately 4 to 6 mo to complete. Osteoblasts synthesize new collagenous organic matrix (Figure 3) and regulate mineralization of matrix by releasing small, membrane-bound matrix vesicles that concentrate calcium and phosphate and enzymatically destroy mineralization inhibitors such as pyrophosphate or proteoglycans (23). Osteoblasts surrounded by and buried within matrix become osteocytes with an extensive canalicular network connecting them to bone surface lining cells, osteoblasts, and other osteocytes, maintained by gap junctions between the cytoplasmic processes extending from the osteocytes (24). The osteocyte network within bone serves as a functional syncytium. At the completion of bone formation, approximately 50 to 70% of osteoblasts undergo apoptosis, with the balance becoming osteocytes or bone-lining cells. Bone-lining cells may regulate influx and efflux of mineral ions into and out of bone extracellular fluid, thereby serving as a blood-bone barrier, but retain the ability to redifferentiate into osteoblasts upon exposure to parathyroid hormone or mechanical forces (25). Bone-lining cells within the endosteum lift off the surface of bone before bone resorption to form discrete bone remodeling compartments with a specialized microenvironment (26). In patients with multiple myeloma, lining cells may be induced to express tartrate-resistant acid phosphatase and other classical osteoclast markers.
Figure 3.
Osteoblasts synthesize proteinaceous matrix, composed mostly of type I collagen, to fill in resorption pits. The proteinaceous matrix is gradually mineralized to form new bone.
The end result of each bone remodeling cycle is production of a new osteon. The remodeling process is essentially the same in cortical and trabecular bone, with bone remodeling units in trabecular bone equivalent to cortical bone remodeling units divided in half longitudinally (27). Bone balance is the difference between the old bone resorbed and new bone formed. Periosteal bone balance is mildly positive, whereas endosteal and trabecular bone balances are mildly negative, leading to cortical and trabecular thinning with aging. These relative changes occur with endosteal resorption outstripping periosteal formation.
The main recognized functions of bone remodeling include preservation of bone mechanical strength by replacing older, microdamaged bone with newer, healthier bone and calcium and phosphate homeostasis. The relatively low adult cortical bone turnover rate of 2 to 3%/yr is adequate to maintain biomechanical strength of bone. The rate of trabecular bone turnover is higher, more than required for maintenance of mechanical strength, indicating that trabecular bone turnover is more important for mineral metabolism. Increased demand for calcium or phosphorus may require increased bone remodeling units, but, in many cases, this demand may be met by increased activity of existing osteoclasts. Increased demand for skeletal calcium and phosphorus is met partially by osteoclastic resorption and partly by nonosteoclastic calcium influx and efflux. Ongoing bone remodeling activity ensures a continuous supply of newly formed bone that has relatively low mineral content and is able to exchange ions more easily with the extracellular fluid. Bone remodeling units seem to be mostly randomly distributed throughout the skeleton but may be triggered by microcrack formation or osteocyte apoptosis. The bone remodeling space represents the sum of all of the active bone remodeling units in the skeleton at a given time.
Osteoclasts
Osteoclasts are the only cells that are known to be capable of resorbing bone (Figure 2). Activated multinucleated osteoclasts are derived from mononuclear precursor cells of the monocyte-macrophage lineage (11). Mononuclear monocyte-macrophage precursor cells have been identified in various tissues, but bone marrow monocyte-macrophage precursor cells are thought to give rise to most osteoclasts.
RANKL and macrophage CSF (M-CSF) are two cytokines that are critical for osteoclast formation. Both RANKL and M-CSF are produced mainly by marrow stromal cells and osteoblasts in membrane-bound and soluble forms, and osteoclastogenesis requires the presence of stromal cells and osteoblasts in bone marrow (28). RANKL belongs to the TNF superfamily and is critical for osteoclast formation. M-CSF is required for the proliferation, survival, and differentiation of osteoclast precursors, as well as osteoclast survival and cytoskeletal rearrangement required for bone resorption. OPG is a membrane-bound and secreted protein that binds RANKL with high affinity to inhibit its action at the RANK receptor (29).
Bone resorption depends on osteoclast secretion of hydrogen ions and cathepsin K enzyme. H+ ions acidify the resorption compartment beneath osteoclasts to dissolve the mineral component of bone matrix, whereas cathepsin K digests the proteinaceous matrix, which is mostly composed of type I collagen (11).
Osteoclasts bind to bone matrix via integrin receptors in the osteoclast membrane linking to bone matrix peptides. The β1 family of integrin receptors in osteoclasts binds to collagen, fibronectin, and laminin, but the main integrin receptor facilitating bone resorption is the αvβ3 integrin, which binds to osteopontin and bone sialoprotein (30).
Binding of osteoclasts to bone matrix causes them to become polarized, with the bone resorbing surface developing a ruffled border that forms when acidified vesicles that contain matrix metalloproteinases and cathepsin K are transported via microtubules to fuse with the membrane. The ruffled border secretes H+ ions via H+-ATPase and chloride channels and causes exocytosis of cathepsin K and other enzymes in the acidified vesicles (31).
Upon contact with bone matrix, the fibrillar actin cytoskeleton of the osteoclast organizes into an actin ring, which promotes formation of the sealing zone around the periphery of osteoclast attachment to the matrix. The sealing zone surrounds and isolates the acidified resorption compartment from the surrounding bone surface (32). Disruption of either the ruffled border or actin ring blocks bone resorption. Actively resorbing osteoclasts form podosomes, which attach to bone matrix, rather than focal adhesions as formed by most cells. Podosomes are composed of an actin core surrounded by αvβ3 integrins and associated cytoskeletal proteins.
Osteoblasts
Osteoprogenitor cells give rise to and maintain the osteoblasts that synthesize new bone matrix on bone-forming surfaces (Figure 3), the osteocytes within bone matrix that support bone structure, and the protective lining cells that cover the surface of quiescent bone. Within the osteoblast lineage, subpopulations of cells respond differently to various hormonal, mechanical, or cytokine signals. Osteoblasts from axial and appendicular bone have been shown to respond differently to these signals.
Self-renewing, pluripotent stem cells give rise to osteoprogenitor cells in various tissues under the right environmental conditions. Bone marrow contains a small population of mesenchymal stem cells that are capable of giving rise to bone, cartilage, fat, or fibrous connective tissue, distinct from the hematopoietic stem cell population that gives rise to blood cell lineages (33). Cells with properties that are characteristic of adult bone marrow mesenchymal stem cells have been isolated from adult peripheral blood and tooth pulp and fetal cord blood, liver, blood, and bone marrow. Multipotential myogenic cells that are capable of differentiating into bone, muscle, or adipocytes have also been identified. Mesenchymal cells that are committed to one phenotype may dedifferentiate during proliferation and develop another phenotype, depending on the local tissue environment. Blood vessel pericytes may develop an osteoblastic phenotype during dedifferentiation under the right circumstances (34).
Commitment of mesenchymal stem cells to the osteoblast lineage requires the canonical Wnt/β-catenin pathway and associated proteins (35). Identification of a high bone mass phenotype associated with activating mutations of LDL receptor–related protein 5 highlighted the importance of the canonical Wnt/β-catenin pathway in embryonic skeletal patterning, fetal skeletal development, and adult skeletal remodeling (36,37). The Wnt system is also important in chondrogenesis and hematopoiesis and may be stimulatory or inhibitory at different stages of osteoblast differentiation.
Flattened bone-lining cells are thought to be quiescent osteoblasts that form the endosteum on trabecular and endosteal surfaces and underlie the periosteum on the mineralized surface. Osteoblasts and lining cells are found in close proximity and joined by adherens junctions. Cadherins are calcium-dependent transmembrane proteins that are integral parts of adherens junctions and together with tight junctions and desmosomes join cells together by linking their cytoskeletons (38).
Osteoblast precursors change shape from spindle-shaped osteoprogenitors to large cuboidal differentiated osteoblasts on bone matrix surfaces after preosteoblasts stop proliferating. Preosteoblasts that are found near functioning osteoblasts in the bone remodeling unit are usually recognizable because of their expression of alkaline phosphatase. Active mature osteoblasts that synthesize bone matrix have large nuclei, enlarged Golgi structures, and extensive endoplasmic reticulum. These osteoblasts secrete type I collagen and other matrix proteins vectorially toward the bone formation surface.
Populations of osteoblasts are heterogeneous, with different osteoblasts expressing different gene repertoires that may explain the heterogeneity of trabecular microarchitecture at different skeletal sites, anatomic site-specific differences in disease states, and regional variation in the ability of osteoblasts to respond to agents used to treat bone disease.
Bone Extracellular Matrix
Bone protein is composed of 85 to 90% collagenous proteins (Table 1). Bone matrix is mostly composed of type I collagen (39), with trace amounts of types III and V and FACIT collagens at certain stages of bone formation that may help determine collagen fibril diameter. FACIT collagens are members of the family of Fibril-Associated Collagens with Interrupted Triple Helices, a group of nonfibrillar collagens that serve as molecular bridges that are important for the organization and stability of extracellular matrices. Members of this family include collagens IX, XII, XIV, XIX, XX, and XXI. Noncollagenous proteins compose 10 to 15% of total bone protein. Approximately 25% of noncollagenous protein is exogenously derived, including serum albumin and α2-HS-glycoprotein, which bind to hydroxyapatite because of their acidic properties. Serum-derived noncollagenous proteins may help regulate matrix mineralization, and α2-HS-glycoprotein, which is the human analogue of fetuin, may regulate bone cell proliferation. The remaining exogenously derived noncollagenous proteins are composed of growth factors and a large variety of other molecules in trace amounts that may affect bone cell activity.
Table 1.
Extracellular matrix proteinsa
| Protein (Chromosome Location) | Function | Human Disease |
|---|---|---|
| Collagen-related proteins | ||
| type I (17q21.23, 7q22.1) | Most abundant bone matrix protein | Osteogenesis imperfecta |
| type X (6q21) | Found in hypertrophic cartilage | None known |
| type III (2q31) | Trace amounts in bone; may regulate collagen fibril diameter | Ehlers-Danlos syndrome |
| type V (9q34.2-34.3; 2q24.3-31; 19q13.2) | Trace amounts in bone; may regulate collagen fibril diameter | |
| Serum proteins in bone matrix | ||
| albumin (4q11-13) | Decreases hydroxyapatite crystal growth | None |
| α2-HS glycoprotein (3q27) | Bovine analog is fetuin | None |
| Glycoaminoglycan-containing proteins and leucine-rich repeat proteins | ||
| aggrecan (15q26.1) | Matrix organization, retention of calcium/phosphorus | None |
| versican (5q14.3) | Defines space destined to become bone | None |
| decorin (12q21.3) | Regulates collagen fibril diameter; binds TGF-β | Progeroid form of Ehlers-Danlos syndrome with decorin/biglycan double knockout |
| biglycan (Xq28) | Binds collagen; binds TGF-β; genetic determinant of peak bone mass | |
| hyaluronan (multigene complex) | May work with versican to define space destined to become bone | None |
| Glycoproteins | ||
| alkaline phosphatase (1p36.1-p34) | Hydrolyzes mineral deposition inhibitors | Hypophosphatasia |
| osteonectin (5q31.3-32) | Regulates collagen fibril diameter | None |
| SIBLING proteins | ||
| osteopontin (4q21) | Inhibits mineralization and remodeling | None |
| bone sialoprotein (4q21) | Initiates mineralization | None |
| MEPE (4q21.1) | Regulator of phosphate metabolism | Tumor-induced osteomalacia |
| RGD-containing glycoproteins | ||
| thrombospondins (15q15, 6q27, 1q21, 5q13, 19p13.1) | Cell attachment | None |
| fibronectin (2q34) | Binds to cells | None |
| vitronectin (17q11) | Cell attachment | None |
| fibrillin 1 and 2 (15q21.1, 5q23-31) | Regulates elastic fiber formation | Fibrillin 1: Marfan syndrome |
| γ-Carboxy glutamic acid–containing proteins | ||
| matrix Gla protein (12p13.1-p12.3) | Inhibits mineralization | None |
| osteocalcin (1q25-q31) | Regulates osteoclasts; inhibits mineralization | None |
| protein S (3p11.2) | Liver product, may be made by osteoblasts | Osteopenia |
SIBLING proteins, Small Integrin-Binding Ligand, N-glycosylated proteins.
Osteoblasts synthesize and secrete as much noncollagenous protein as collagen on a molar basis. The noncollagenous proteins are divided broadly into several categories, including proteoglycans, glycosylated proteins, glycosylated proteins with potential cell-attachment activities, and γ-carboxylated (gla) proteins. The roles of each of the bone proteins are not well defined at present, and many seem to serve multiple functions, including regulation of bone mineral deposition and turnover and regulation of bone cell activity. Serum osteocalcin synthesized by osteoblasts was previously thought to function as a promoter or initiator of calcium deposition at the nidus between the ends of collagen fibrils and therefore regarded as a marker of bone formation. The observation that the osteocalcin knockout mouse has a high bone mass phenotype suggests that osteocalcin normally inhibits bone formation. Because serum osteocalcin is derived from both matrix release by osteoclast activity and osteoblast synthesis, it is currently regarded as a marker of bone turnover rather than a specific marker of bone formation.
The main glycosylated protein present in bone is alkaline phosphatase. Alkaline phosphatase in bone is bound to osteoblast cell surfaces via a phosphoinositol linkage and also is found free within mineralized matrix. Alkaline phosphatase plays an as-yet-undefined role in mineralization of bone (40). The most prevalent noncollagenous protein in bone is osteonectin, accounting for approximately 2% of total protein in developing bone. Osteonectin is thought to affect osteoblast growth and/or proliferation and matrix mineralization.
Bone Matrix Mineralization
Bone is composed of 50 to 70% mineral, 20 to 40% organic matrix, 5 to 10% water, and <3% lipids. The mineral content of bone is mostly hydroxyapatite [Ca10(PO4)6(OH)2], with small amounts of carbonate, magnesium, and acid phosphate, with missing hydroxyl groups that are normally present. Compared with geologic hydroxyapatite crystals, bone hydroxyapatite crystals are very small, measuring only approximately 200 Å in their largest dimension. These small, poorly crystalline, carbonate-substituted crystals are more soluble than geologic hydroxyapatite crystals, thereby allowing them to support mineral metabolism.
Matrix maturation is associated with expression of alkaline phosphatase and several noncollagenous proteins, including osteocalcin, osteopontin, and bone sialoprotein. It is thought that these calcium- and phosphate-binding proteins help regulate ordered deposition of mineral by regulating the amount and size of hydroxyapatite crystals formed.
Bone mineral provides mechanical rigidity and load-bearing strength to bone, whereas the organic matrix provides elasticity and flexibility. Bone mineral is initially deposited in “hole” zones between the ends of collagen fibrils (41). This process may be facilitated by extracellular matrix vesicles in bone, as it is in calcifying cartilage and mineralizing turkey tendon (23). Matrix extracellular vesicles are synthesized by chondrocytes and osteoblasts and serve as protected microenvironments in which calcium and phosphate concentrations can increase sufficiently to precipitate crystal formation. The extracellular fluid is not normally supersaturated with hydroxyapatite, so hydroxyapatite does not spontaneously precipitate. Matrix extracellular vesicles contain a nucleational core that is composed of proteins and a complex of acidic phospholipids, calcium, and inorganic phosphate that is sufficient to precipitate hydroxyapatite crystals. It is not yet certain how matrix extracellular vesicles contribute to mineralization at specific sites at the ends of collagen fibrils, because the vesicles apparently are not directly targeted to the ends of fibrils (23).
There is no evidence that noncrystalline calcium phosphate clusters (amorphous calcium phosphate) forms in bone before it is converted to hydroxyapatite (42). As bone matures, hydroxyapatite crystals enlarge and reduce their level of impurities. Crystal enlargement occurs both by crystal growth and by aggregation. Bone matrix macromolecules may facilitate initial crystal nucleation, sequester mineral ions to increase local concentrations of calcium and/or phosphorus, or facilitate heterogeneous nucleation. Macromolecules also bind to growing crystal surfaces to determine the size, shape, and number of crystals formed.
Confirmed mineralization promoters (nucleators) include dentin matrix protein 1 and bone sialoprotein. Type I collagen is not a bone mineralization promoter. Phosphoprotein kinases and alkaline phosphatase regulate the mineralization process. Bone alkaline phosphatase may increase local phosphorus concentrations, remove phosphate-containing inhibitors of hydroxyapatite crystal growth, or modify phosphoproteins to control their ability to act as nucleators.
Vitamin D plays an indirect role in stimulating mineralization of unmineralized bone matrix. After absorption or skin production of vitamin D, the liver synthesizes 25-hydroxyvitamin D and the kidneys subsequently produce biologically active 1,25-dihydroxyvitamin D [1,25-(OH)2D]. Serum 1,25-(OH)2D is responsible for maintaining serum calcium and phosphorus in adequate concentrations to allow passive mineralization of unmineralized bone matrix. Serum 1,25-(OH)2D does this primarily by stimulating intestinal absorption of calcium and phosphorus. Serum 1,25-(OH)2D also promotes differentiation of osteoblasts and stimulates osteoblast expression of bone-specific alkaline phosphatase, osteocalcin, osteonectin, OPG, and a variety of other cytokines. Serum 1,25-(OH)2D also influences proliferation and apoptosis of other skeletal cells, including hypertrophic chondrocytes.
Osteocytes
Osteocytes represent terminally differentiated osteoblasts and function within syncytial networks to support bone structure and metabolism. Osteocytes lie within lacunae within mineralized bone (Figure 3) and have extensive filipodial processes that lie within the canaliculi in mineralized bone (43). Osteocytes do not normally express alkaline phosphatase but do express osteocalcin, galectin 3, and CD44, a cell adhesion receptor for hyaluronate, as well as several other bone matrix proteins. Osteocytes express several matrix proteins that support intercellular adhesion and regulate exchange of mineral in the bone fluid within lacunae and the canalicular network. Osteocytes are active during osteolysis and may function as phagocytic cells because they contain lysosomes.
Osteocytes maintain connection with each other and the bone surface via their multiple filipodial cellular processes. Connexins are integral cellular proteins that maintain gap junctions between cells to allow direct communication through intercellular channels. Osteocytes are linked metabolically and electrically through gap junctions composed primarily of connexin 43 (44). Gap junctions are required for osteocyte maturation, activity, and survival.
The primary function of the osteocyte-osteoblast/lining cell syncytium is mechanosensation (45). Osteocytes transduce stress signals from bending or stretching of bone into biologic activity. Flow of canalicular fluid in response to external forces induces a variety of responses within osteocytes. Rapid fluxes of bone calcium across filipodial gap junctions are believed to stimulate transmission of information between osteoblasts on the bone surface and osteocytes within the bone (46). Signaling mechanisms involved in mechanotransduction include prostaglandin E2, cyclo-oxygenase 2, various kinases, Runx2, and nitrous oxide.
Osteocytes may live for decades in human bone that is not turned over. The presence of empty lacunae in aging bone suggests that osteocytes may undergo apoptosis, probably caused by disruption of their intercellular gap junctions or cell–matrix interactions (47). Osteocyte apoptosis in response to estrogen deficiency or glucocorticoid treatment is harmful to bone structure. Estrogen and bisphosphonate therapy and physiologic loading of bone may help prevent osteoblast and osteocyte apoptosis (48).
Determinants of Bone Strength
Bone mass accounts for 50 to 70% of bone strength (49). Bone geometry and composition are important, however, because larger bones are stronger than smaller bones, even with equivalent bone mineral density. As bone diameter expands radially, the strength of bone increases by the radius of the involved bone raised to the fourth power. The amount and proportion of trabecular and cortical bone at a given skeletal site affect bone strength independently. Bone material properties are important for bone strength. Some patients with osteoporosis have abnormal bone matrix. Mutations in certain proteins may cause bone weakness (e.g., collagen defects cause decreased bone strength in osteogenesis imperfecta, impaired γ-carboxylation of Gla proteins). Bone strength can be affected by osteomalacia, fluoride therapy, or hypermineralization states. Bone microstructure affects bone strength also. Low bone turnover leads to accumulation of microfractures. High bone turnover, with bone resorption greater than bone formation, is the main cause of microarchitectural deterioration.
Conclusions
The skeleton serves multiple functions. Bone modeling and remodeling preserve skeletal function throughout life. The bone remodeling unit normally couples bone resorption and formation. Bone matrix regulates bone mineralization. Bone strength depends on bone mass, geometry and composition, material properties, and microstructure.
Disclosures
None.
References
- 1.Musculoskeletal system. In: Gray's Anatomy, 39th Ed., edited by Standring S, New York, Elsevier,2004. , pp83 –135
- 2.Taichman RS: Blood and bone: Two tissues whose fates are intertwined to create the hematopoietic stem cell niche. Blood 105 :2631 –2639,2005 [DOI] [PubMed] [Google Scholar]
- 3.Eriksen EF, Axelrod DW, Melsen F. Bone Histomorphometry, New York, Raven Press,1994. , pp1 –12
- 4.Kobayashi S, Takahashi HE, Ito A, Saito N, Nawata M, Horiuchi H, Ohta H, Ito A, Iorio R, Yamamoto N, Takaoka K: Trabecular minimodeling in human iliac bone. Bone 32 :163 –169,2003 [DOI] [PubMed] [Google Scholar]
- 5.Ubara Y, Tagami T, Nakanishi S, Sawa N, Hoshino J, Suwabe T, Kaitori H, Takemoto F, Hara S, Takaichi K: Significance of minimodeling in dialysis patients with adynamic bone disease. Kidney Int 68 :833 –839,2005 [DOI] [PubMed] [Google Scholar]
- 6.Ubara Y, Fushimi T, Tagami T, Sawa N, Hoshino J, Yokota M, Kaitori H, Takemoto F, Hara S: Histomorphometric features of bone in patients with primary and secondary hyperparathyroidism. Kidney Int 63 :1809 –1816,2003 [DOI] [PubMed] [Google Scholar]
- 7.Lindsay R, Cosman F, Zhou H, Bostrom M, Shen V, Cruz J, Nieves JW, Dempster DW: A novel tetracycline labeling schedule for longitudinal evaluation of the short-term effects of anabolic therapy with a single iliac crest biopsy: Early actions of teriparatide. J Bone Miner Res 21 :366 –373,2006 [DOI] [PubMed] [Google Scholar]
- 8.Burr DB: Targeted and nontargeted remodeling. Bone 30 :2 –4,2002 [DOI] [PubMed] [Google Scholar]
- 9.Parfitt AM: Targeted and nontargeted bone remodeling: Relationship to basic multicellular unit origination and progression. Bone 30 :5 –7,2002 [DOI] [PubMed] [Google Scholar]
- 10.Roodman GD: Cell biology of the osteoclast. Exp Hematol 27 :1229 –1241,1999 [DOI] [PubMed] [Google Scholar]
- 11.Boyle WJ, Simonet WS, Lacey DL: Osteoclast differentiation and activation. Nature 423 :337 –342,2003 [DOI] [PubMed] [Google Scholar]
- 12.Blair HC, Athanasou NA: Recent advances in osteoclast biology and pathological bone resorption. Histol Histopathol 19 :189 –199,2004 [DOI] [PubMed] [Google Scholar]
- 13.Silver IA, Murrills RJ, Etherington DJ: Microelectrode studies on the acid microenvironment beneath adherent macrophages and osteoclasts. Exp Cell Res 175 :266 –276,1988 [DOI] [PubMed] [Google Scholar]
- 14.Delaisse JM, Andersen TL, Engsig MT, Henriksen K, Troen T, Blavier L: Matrix metalloproteinases (MMP) and cathepsin K contribute differently to osteoclast activities. Microsc Res Tech 61 :504 –513,2003 [DOI] [PubMed] [Google Scholar]
- 15.Eriksen EF: Normal and pathological remodeling of human trabecular bone: Three-dimensional reconstruction of the remodeling sequence in normals and metabolic bone disease. Endocr Rev 7 :379 –408,1986 [DOI] [PubMed] [Google Scholar]
- 16.Reddy SV: Regulatory mechanisms operative in osteoclasts. Crit Rev Eukaryot Gene Expr 14 :255 –270,2004 [DOI] [PubMed] [Google Scholar]
- 17.Bonewald L, Mundy GR: Role of transforming growth factor beta in bone remodeling. Clin Orthop Rel Res 2S :35 –40,1990 [PubMed] [Google Scholar]
- 18.Hock JM, Centrella M, Canalis E: Insulin-like growth factor I (IGF-I) has independent effects on bone matrix formation and cell replication. Endocrinology 122 :254 –260,2004 [DOI] [PubMed] [Google Scholar]
- 19.Locklin RM, Oreffo RO, Triffitt JT: Effects of TGFbeta and bFGF on the differentiation of human bone marrow stromal fibroblasts. Cell Biol Int 23 :185 –194,1999 [DOI] [PubMed] [Google Scholar]
- 20.Smit TH, Burger EH, Huyghe JM: Is BMU-coupling a strain-regulated phenomenon? A finite element analysis. J Bone Miner Res 15 :301 –307,2002 [DOI] [PubMed] [Google Scholar]
- 21.Smit TH, Burger EH, Huyghe JM: A case for strain-induced fluid flow as a regulator of BMU-coupling and osteonal alignment. J Bone Miner Res 17 :2021 –2029,2002 [DOI] [PubMed] [Google Scholar]
- 22.Martin TJ, Sims NA: Osteoclast-derived activity in the coupling of bone formation to resorption. Trends Mol Med 11 :76 –81,2005 [DOI] [PubMed] [Google Scholar]
- 23.Anderson HC: Matrix vesicles and calcification. Curr Rheumatol Rep 5 :222 –226,2003 [DOI] [PubMed] [Google Scholar]
- 24.Burger EH, Klein-Nuland J, Smit TH: Strain-derived canalicular fluid flow regulates osteoclast activity in a remodeling osteon: A proposal. J Biomech 36 :1452 –1459,2003 [DOI] [PubMed] [Google Scholar]
- 25.Dobnig H, Turner RT: Evidence that intermittent treatment with parathyroid hormone increases bone formation in adult rats by activation of bone lining cells. Endocrinology 136 :3632 –3638,1995 [DOI] [PubMed] [Google Scholar]
- 26.Hauge EM, Qvesel D, Eriksen EF, Mosekilde L, Melsen F: Cancellous bone remodeling occurs in specialized compartments lined by cells expressing osteoblastic markers. J Bone Miner Res 16 :1575 –1582,2001 [DOI] [PubMed] [Google Scholar]
- 27.Parfitt AM: Osteonal and hemiosteonal remodeling: The spatial and temporal framework for signal traffic in adult bone. J Cell Biochem 55 :273 –276,1994 [DOI] [PubMed] [Google Scholar]
- 28.Teitelbaum SL, Ross FP: Genetic regulation of osteoclast development and function. Nat Rev Genet 4 :638 –649,2003 [DOI] [PubMed] [Google Scholar]
- 29.Cohen MM Jr: The new bone biology: Pathologic, molecular, clinical correlates. Am J Med Genet A 140 :2646 –2706,2006 [DOI] [PubMed] [Google Scholar]
- 30.Ross FP, Teitelbaum SL: αvβ3 and macrophage colony-stimulating factor: Partners in osteoclast biology. Immunol Rev 208 :88 –105,2005 [DOI] [PubMed] [Google Scholar]
- 31.Teitelbaum SL, Abu-Amer Y, Ross FP: Molecular mechanisms of bone resorption. J Cell Biochem 59 :1 –10,1995 [DOI] [PubMed] [Google Scholar]
- 32.Vaananen HK, Zhao H, Mulari M, Halleen JM: The cell biology of osteoclast function. J Cell Sci 113 :377 –381,2000 [DOI] [PubMed] [Google Scholar]
- 33.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR: Multilineage potential of adult human mesenchymal stem cells. Science 284 :143 –147,1990 [DOI] [PubMed] [Google Scholar]
- 34.Doherty MJ, Ashton BA, Walsh S, Beresford JN, Grant ME, Canfield AE: Vascular pericytes express osteogenic potential in vitro and in vivo. J Bone Miner Res 13 :828 –838,1998 [DOI] [PubMed] [Google Scholar]
- 35.Logan CY, Nusse R: The Wnt signaling pathway in development and disease. Annu Rev Cell Dev Biol 20 :781 –810,2004 [DOI] [PubMed] [Google Scholar]
- 36.Boyden LM, Mao J, Belsky J, Mitzner L, Farhi A, Mitnick MA, Wu D, Insogna K, Lifton RP: High bone density due to a mutation in LDL receptor-related protein 5. N Engl J Med 346 :1513 –1521,2002 [DOI] [PubMed] [Google Scholar]
- 37.Little RD, Recker RR, Johnson ML: High bone density due to a mutation in LDL receptor-related protein 5. N Engl J Med 347 :943 –944,2002 [DOI] [PubMed] [Google Scholar]
- 38.Shin CS, Lecanda F, Sheikh S, Weitzmann L, Cheng SL, Civitelli R: Relative abundance of different cadherins defines differentiation of mesenchymal precursors into osteogenic, myogenic, or adipogenic pathways. J Cell Biochem 78 :566 –577,2000 [PubMed] [Google Scholar]
- 39.Brodsky B, Persikov AV: Molecular structure of the collagen triple helix. Adv Protein Chem 70 :301 –339,2005 [DOI] [PubMed] [Google Scholar]
- 40.Whyte MP: Hypophosphatasia and the role of alkaline phosphatase in skeletal mineralization. Endocr Rev 15 :439 –461,1994 [DOI] [PubMed] [Google Scholar]
- 41.Landis WJ: The strength of a calcified tissue depends in part on the molecular structure and organization of its constituent mineral crystals in their organic matrix. Bone 16 :533 –544,1995 [DOI] [PubMed] [Google Scholar]
- 42.Weiner S, Sagi I, Addadi L: Structural biology: Choosing the crystallization path less traveled. Science 309 :1027 –1028 [DOI] [PubMed]
- 43.Bonewald LF: Establishment and characterization of an osteocyte-like cell line, MLO-Y4. J Bone Miner Metab 17 :61 –65,1999 [DOI] [PubMed] [Google Scholar]
- 44.Plotkin LI, Manolagas SC, Bellido T: Transduction of cell survival signals by connexin-43 hemichannels. J Biol Chem 277 :8648 –8657,2002 [DOI] [PubMed] [Google Scholar]
- 45.Rubin CT, Lanyon LE: Osteoregulatory nature of mechanical stimuli: Function as a determinant for adaptive bone remodeling. J Orthop Res 5 :300 –310,1987 [DOI] [PubMed] [Google Scholar]
- 46.Jorgensen NR, Teilmann SC, Henriksen Z, Civitelli R, Sorensen OH, Steinberg TH: Activation of L-type calcium channels is required for gap junction-mediated intercellular calcium signaling in osteoblastic cells. J Biol Chem 278 :4082 –4086,2003 [DOI] [PubMed] [Google Scholar]
- 47.Xing L, Boyce BF: Regulation of apoptosis in osteoclasts and osteoblastic cells. Biochem Biophys Res Commun 328 :709 –720,2005 [DOI] [PubMed] [Google Scholar]
- 48.Plotkin LI, Aguirre JI, Kousteni S, Manolagas SC, Bellido T: Bisphosphonates and estrogens inhibit osteocyte apoptosis via distinct molecular mechanisms downstream of extracellular signal-regulated kinase activation. J Biol Chem 280 :7317 –7325,2005 [DOI] [PubMed] [Google Scholar]
- 49.Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PH, Eberl S: Genetic determinants of bone mass in adults: A twin study. J Clin Invest 80 :706 –710,1987 [DOI] [PMC free article] [PubMed] [Google Scholar]