Abstract
Borderline personality disorder (BPD) has received significant attention as a predictor of suicidal behavior (SB) and nonsuicidal self-injury (NSSI). Despite significant promise, trait impulsivity has received less attention. Understanding the relations between impulsivity and SB and NSSI is confounded, unfortunately, by the heterogeneous nature of impulsivity. This study examined the relations among 4 personality pathways to impulsive behavior studied via the UPPS model of impulsivity and SB and NSSI in a residential sample of drug abusers (N = 76). In this study, we tested whether these 4 impulsivity-related traits (i.e., Negative Urgency, Sensation Seeking, Lack of Premeditation, and Lack of Perseverance) provide incremental validity in the statistical prediction of SB and NSSI above and beyond BPD; they do. We also tested whether BPD symptoms provide incremental validity in the prediction of SB and NSSI above and beyond these impulsivity-related traits; they do not. In addition to the main effects of Lack of Premeditation and Negative Urgency, we found evidence of a robust interaction between these 2 personality traits. The current results argue strongly for the consideration of these 2 impulsivity-related domains—alone and in interaction—when attempting to understand and predict SB and NSSI.
Keywords: impulsivity, suicidal behavior, urgency, premeditation, UPPS
Suicidal ideation, attempts, and completions are prevalent in the general population (Kessler, Borges, & Walters, 1999), as are incidents of nonsuicidal self-injury (NSSI), defined as the intentional, direct injuring of body tissue without suicidal intent (e.g., Klonsky, 2007). In addition to sociodemographic, psychiatric, and environmental risk factors, personality traits have received increased attention as predisposing factors for suicidal behavior (SB) and NSSI. Among pathological personality traits, borderline personality disorder (BPD) has received strong support as a predisposing factor for SB and NSSI. Patients with BPD represent between 9% and 33% of all suicides, with a risk approximately 50 times that of individuals within the general population (Pomplili, Girardi, Ruberto, & Tatarelli, 2006). SB and NSSI are so common in BPD that they are included as explicit symptoms of Diagnostic and Statistical Manual of Mental Disorders BPD.
In addition, more general personality traits such as those drawn from the five-factor personality model (FFM; Costa & McCrae, 1992) have received attention in relation to suicidality and NSSI. In a recent qualitative review of 90 studies examining suicidal behavior, Brezo, Paris, and Turecki (2006) concluded that “hopelessness and neuroticism … are traits that hold the most promise” (p. 200) and indicated that further studies on the role of impulsivity are warranted. Work by Evans, Platts, and Liebenau (1996) suggests a similar focus for NSSI. It is important to note that the general traits that appear important to the prediction of SB and NSSI are also core components of BPD. More specifically, impulsivity (i.e., “impulsivity in at least two areas”) and neuroticism (i.e., “affective instability” and “inappropriate, intense anger”) are explicit criteria for BPD. Trull (2001) has found that latent “disinhibition” and “negative affectivity” factors accounted for over 90% of the variance in a latent BPD factor, although he did not examine the various aspects of impulsivity.
One of the difficulties inherent in understanding the relations between impulsivity and SB and NSSI (or any outcome) is that the term impulsivity encompasses a variety of distinguishable personality traits. Depue and Collins (1999) indicated that “impulsivity comprises a heterogeneous cluster of lower-order traits that includes terms such as impulsivity, sensation seeking, risk-taking, novelty seeking, boldness, adventuresomeness, boredom susceptibility, unreliability, and unorderliness” (p. 495); similarly, Whiteside and Lynam (2001) called impulsivity “an artificial umbrella term” (p. 687). There is evidence that the traits falling under this “umbrella” come from different personality domains and have different neurobiological underpinnings (Manuck et al., 1998; Wacker, Chavanon, & Stemmler, 2006). Failure to attend to the multiplicity of pathways to impulsive behavior may hinder understanding of the contribution of these traits to SB and NSSI, as these impulsivity-related traits may bear differential relations to these constructs.
One approach to parsing the heterogeneity under the “impulsivity” umbrella lies in the UPPS model, which originally posited four distinct personality pathways to impulsive behavior (Whiteside & Lynam, 2001). The model and its attendant assessment instrument were derived from a factor analysis of widely used measures of impulsivity including four traits from three dimensions of the FFM (Whiteside & Lynam, 2001). The analysis revealed a four-factor structure, with each marked by one of the FFM traits. Negative Urgency measures an individual’s tendency to act “impulsively” when experiencing negative affect. Lack of Perseverance assesses an individual’s tendency to give up in the face of boredom, fatigue, or frustration. Lack of Premeditation assesses an individual’s tendency to act without consideration of the potential consequences of the behavior. Sensation Seeking refers to an individual’s tendency to pursue activities that are exciting and novel. Recent work by Smith and Cyders (Cyders & Smith, 2007; Cyders, Smith, Spillane, Fischer, & Annus, 2007) has identified an important additional dimension, Positive Urgency, which assesses an individual’s tendency to act “impulsively” under conditions of heightened positive affect. Although this fifth dimension has been included in the more recent versions of the UPPS scale (UPPS-P), it was not present in the original version used in the present study.
Several studies have confirmed the four-factor structure of the original UPPS (Lynam & Miller, 2004; Smith, Fischer, Cyders, Annus, & Spillane, 2007), and others have provided evidence for differential relations between UPPS dimensions and outcomes including crime and aggression (Lynam & Miller, 2004), eating disorders (Fischer, Smith, & Anderson, 2003), alcohol and substance use (Magid & Colder, 2007), and pathological gambling (Whiteside, Lynam, Miller, & Reynolds, 2005). Thus, the conceptual model underlying the UPPS has potential to clarify the relations among traits related to impulsive behaviors, BPD, SB, and NSSI.
The study reported here had several specific aims. First, we examined the relations between the personality pathways to impulsive behavior and SB and NSSI. In addition to the observed relations among BPD, “impulsivity,” SB, and NSSI, various theoretical accounts highlight the role of one or more personality pathways to impulsive behavior in SB and NSSI. Most theories of NSSI include a difficulty in constraining impulses. Decades ago, Pattison and Kahan (1983) suggested that a “deliberate self-harm syndrome” be included in the diagnostic system as an impulse-control disorder based on their conceptualization of self-injury resulting from an inability to resist an impulse or urge to self-injure. Evans and Lacey (1992) proposed that NSSI be considered as part of a “multi-impulsive personality disorder,” based on the overlap of NSSI with a variety of other seemingly impulsive behaviors (e.g., binge eating, substance abuse, and gambling). Given the role of negative affect in self-injury (Klonsky, 2007), it seems likely that Negative Urgency may play an especially prominent role. Increased episodes of negative affect should increase impulsive acts among those who are dys-regulated by such affects. Impulsivity in one form or another also figures prominently in theories of suicidal behavior, although whether it has a distal or proximal influence differs across theories. Many theories (e.g., Baumeister, 1990) suggest that reduced inhibition has a proximal influence by allowing suicidal impulses to be acted on; within this model, lack of deliberation seems most likely to have an impact. In Joiner’s (2005) interpersonal–psychological theory of suicide, impulsivity plays a more distal role by increasing the likelihood of exposure to painful and provocative experiences. From this view, Negative Urgency might again be expected to be particularly important. Thus, theories of SB and NSSI highlight the importance of “impulsivity.” This is not to say, however, that SB and NSSI are identical; there is a literature suggesting that SB and NSSI manifest different relations with constructs such as psychopathology (e.g., Muehlenkamp & Gutierrez, 2004; Wong, Stewart, Ho, & Lam, 2007). We simply mean to suggest they may share a common risk factor.
Overall, we expected Negative Urgency to be strongly related to both sets of behaviors; individuals who have a difficult time restraining impulses when feeling depressed, angry, anxious, ashamed, or embarrassed will be at particular risk. We also expected low levels of Premeditation to relate to these behaviors as individuals who fail to consider the consequences of their behavior should be more apt to engage in behaviors offering short-term relief at the expense of long-term consequences (e.g., injury, hospitalization).
A second aim of the study was to test whether impulsivity-related traits manifest incremental validity in the statistical prediction of SB and NSSI above BPD. Third, we tested whether BPD manifests incremental validity in the statistical prediction of SB and NSSI above the impulsivity-related domains. In addition to examining the main effects of the UPPS domains, we also explored possible interactions between Negative Urgency and the remaining three UPPS traits. Given the relations between negative affect and SB and NSSI, Negative Urgency seems a particularly important construct, and such interactions have been observed previously for gambling and disordered eating (Anestis, Selby, Fink, & Joiner, 2007; Fischer & Smith, 2008). These analyses were conducted in a clinical sample of inpatient residents at a substance use treatment facility. The sample primarily comprised Black/African American participants, which provided a unique and understudied sample in which to study SB and NSSI. The nature of the sample also ensured that there would be adequate levels of impulsivity, given the relations between UPPS impulsivity-related traits and substance use (e.g., Miller, Flory, Lynam, & Leukefeld, 2003).
Method
Participants and Procedure
Participants were 76 inpatient residents in a drug and alcohol abuse treatment center in Northeast Washington, DC, a sample expected to have elevated rates of suicide and NSSI behaviors (Nock & Kessler, 2006). Participants ranged in age from 18 to 62 years, with a mean of 42.21 years (SD = 8.16; 67% male; 80% Black/African American, 11% White, 1% Hispanic/Latino, 1% Native American, and 7% declined to report). Twenty-eight percent had not completed high school or received a GED, 33% had completed high school or received a GED, 34% had attended at least some college or technical school, and 5% had completed college or beyond. After informed consent was obtained, participants completed diagnostic clinical interviews and self-report questionnaires and were debriefed.
According to the clinical interviews (described below), all participants met criteria for substance dependence for at least one type of substance; 51% of the sample met dependence criteria for more than one type of substance. The most frequently occurring categories of dependence were crack/cocaine (75%) and alcohol (40%). In addition, 31.6% of participants met criteria for BPD, 27.6% met criteria for current major depression, and 15.8% met criteria for bipolar disorder.
Measures
Structured Clinical Interview for DSM–IV Axis II Disorders (SCID–II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997)
The SCID–II was used to assess the total number of BPD symptoms (M = 3.0, SD = 2.5). For the current study, interviews were conducted by the fourth author (M.A.B), trained in the administration of the interviews; these interviews were conducted with no knowledge of participant performance on other study measures. Twenty-five percent of these interviews were reviewed by another PhD-level clinician (C.W.L.). In the three cases for which there was a discrepancy, a consensus was reached.
UPPS Impulsive Behavior Scale (UPPS; Whiteside & Lynam, 2001)
The UPPS is a 45-item self-report measure used to assess four impulsivity-related traits: Negative Urgency (M = 20.24, SD = 2.99), (Lack of) Premeditation (M = 13.24, SD = 2.86), (Lack of) Perseverance (M = 12.77, SD = 2.42), and Sensation Seeking (M = 18.10, SD = 3.03).
Personality Assessment Inventory—Borderline scale (PAI–BPD; Morey, 1991)
The PAI–BPD contains 24 items and was used to measure BPD symptomatology (M = 33.20, SD = 11.58).
Suicidal Behaviors Questionnaire—14 (SBQ–14; Linehan, 1996)
The SBQ–14 contains 34 items that assess five domains, including past suicidal ideation, future suicidal ideation, past suicide threats, future suicide attempts, and likelihood of dying in a future suicide attempt. Each item is rated according to several time periods. In the current study, we used the past suicidal ideation scale (M = 2.39, SD = 9.59), an overall suicide risk index (M = 3.37, SD = 9.9), a dichotomous variable representing the presence of a past suicide attempt (11% of the sample reported an attempt), and an index of future suicidality comprising future ideation, future attempts, and likelihood of dying as a result of a suicide attempt (M = 0.29, SD = 0.84).
Deliberate Self-Harm Inventory (DSHI; Gratz, 2001)
The DSHI is a behavior-based questionnaire, which contains 11 items providing information about nonsuicidal self-harming behaviors (e.g., cutting). The current study examined the variety of different forms of NSSI across the lifetime; 20% of the sample engaged in at least one of these behaviors (M = 0.29, SD = 0.64).
Negative emotionality
Negative emotionality was assessed using the Stress Reaction scale (M = 7.30, SD = 4.78) from the Multidimensional Personality Questionnaire—Brief Form (MPQ; Patrick, Curtin, & Tellegen, 2002), which has been shown to be the best assessment of general negative emotionality on the MPQ (Gaughan, Miller, Pryor, & Lynam, 2009).
Statistical Analyses
First, distributions were examined for skewness and kurtosis; past ideation, overall risk, and variety of NSSI were log-transformed to reduce skewness. Second, we examined the bivariate correlations between all study variables. Third, hierarchical regression analyses were calculated in which the SB and NSSI variables were regressed onto sex, two BPD scores, and the four UPPS domains at Step 1. At Step 2, three product terms were added representing the three two-way interaction terms between UPPS Negative Urgency and the remaining UPPS domains. To test whether the findings involving Negative Urgency were due to its overlap with general negative emotionality, we included the Stress Reaction scale from the MPQ and its interaction with Premeditation in a third step. Inclusion of the two BPD scores, one from a semistructured interview and one from a self-report inventory, provided a gold-standard assessment protocol for BPD symptoms (i.e., semistructured interview) and a methodology that shares the same method variance (i.e., self-report) as the impulsivity domains, so as to not put BPD at a disadvantage. The overlap between the two BPD scores makes it more difficult for either to make an independent contribution in the regression analyses; to examine the contribution of BPD symptoms generally, we report the variance accounted for by the two scores together above and beyond other variables in the model at Step 2.
Results
Bivariate Correlations
Table 1 presents the bivariate correlations between study variables. Sex was significantly correlated only with the SCID–II BPD ratings (r = −.34) such that women had more BPD symptoms. The two BPD scores were significantly related with one another (r = .70) and showed nearly identical correlations with the UPPS traits in that both were significantly positively related to Negative Urgency, as well as Lack of Premeditation and Lack of Perseverance. The BPD scores were significantly related to past suicide attempts, past ideation, overall suicide risk, and the NSSI count but not the future suicidality score.
Table 1.
Bivariate Correlations Among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | — | ||||||||||||
| 2. SCID BPD | −.34** | .81 | |||||||||||
| 3. PAI–BPD | −.19 | .70** | .85 | ||||||||||
| 4. UPPS Negative Urgency | −.18 | .41** | .61** | .78 | |||||||||
| 5. UPPS Sensation Seeking | .11 | −.01 | .20 | .14 | .75 | ||||||||
| 6. UPPS (Lack of) Premeditation | −.11 | .32** | .37** | .25* | .04 | .86 | |||||||
| 7. UPPS (Lack of) Perseverance | −.13 | .27* | .30** | .28* | .00 | .60** | .74 | ||||||
| 8. Past suicide attempt | −.13 | .28* | .39** | .37** | .02 | .21 | .26* | — | |||||
| 9. Past suicide ideation | −.15 | .31** | .35** | .35** | .04 | .38** | .31** | .68** | .93 | ||||
| 10. Future suicidality | −.06 | .17 | .22 | .27* | .14 | .43** | .15 | .22 | .58** | .97 | |||
| 11. Overall risk composite | −.19 | .35** | .37** | .28* | .02 | .44** | .17 | .27* | .66** | .74** | .86 | ||
| 12. NSSI—Count | −.20 | .24* | .25* | .25* | −.05 | .31** | .29** | .41** | .46** | .33** | .33** | .70 | |
| 13. MPQ—Stress Reaction | −.27* | .68*** | .72*** | .47*** | .06 | .18 | .19 | .39*** | .36** | .15 | .26* | .34** | .91 |
Note. SCID = Structured Clinical Interview for DSM–IV Axis II Disorders; BPD = borderline personality disorder; PAI = Personality Assessment Inventory; NSSI = nonsuicidal self-injury; MPQ = Multidimensional Personality Questionnaire. Bolded scores along the diagonal are reliability coefficients.
p < .05.
p < .01.
p < .001.
The four UPPS trait manifested interrelations ranging from .00 (Sensation Seeking and Lack of Perseverance) to .60 (Lack of Premeditation and Lack of Perseverance), with a median r = .19. With regard to suicidality and NSSI, Negative Urgency manifested significant positive correlations with all five variables (median r = .28). Next, Lack of Premeditation manifested four significant positive correlations (median r = .38), whereas Lack of Perseverance manifested three (median r = .26). Sensation Seeking manifested no significant correlations (median r = .02). Finally, the five suicidality and NSSI variables manifested generally significant interrelations ranging from .22 (future suicidality and past suicide attempt) to .74 (future suicidality and overall risk composite), with a median r = .44.
Incremental Validity of the UPPS in Predicting Suicidality and NSSI
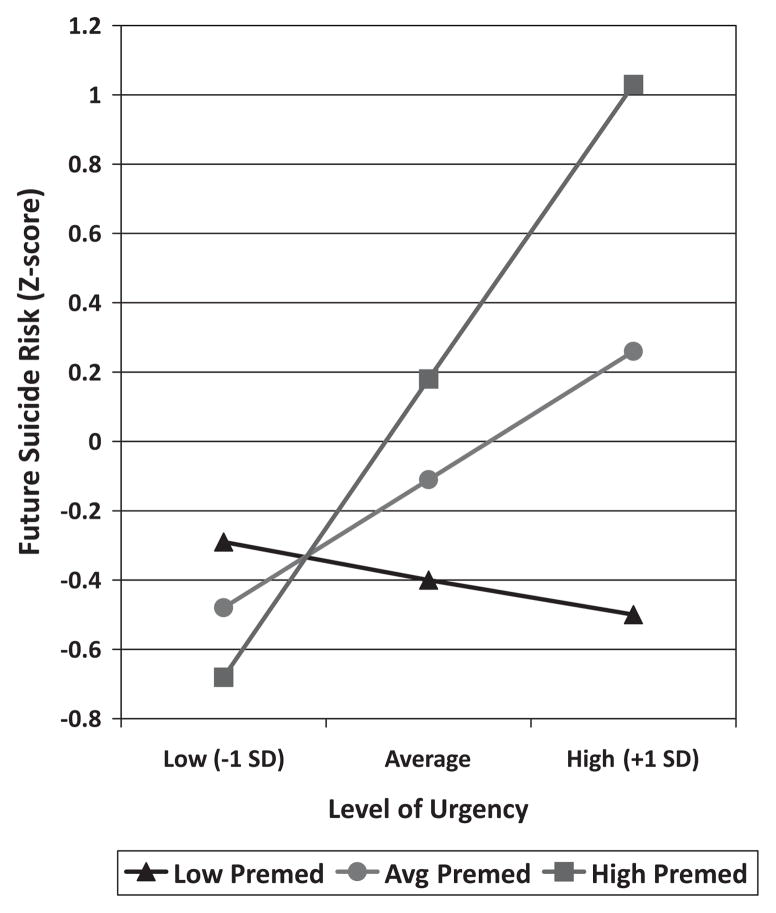
Table 2 presents the results from five hierarchical regression analyses in which we tested the incremental predictive utility of the four UPPS domains above and beyond BPD symptoms (and vice versa) along with the incremental predictive validity of three two-way interactions involving Negative Urgency. At Step 1, the suicidality and NSSI variables were regressed onto sex, the two BPD measures, and the four UPPS scales. These variables accounted for between 16% and 52% of the variance, with an average R2 of .29. The variance accounted for was significant for four of the five outcome variables. As a set, the two BPD variables did not account for significant unique variance (i.e., above and beyond variance accounted for by sex and the four UPPS scales) in any of the analyses; individually, neither BPD construct was statistically significant in any of the five analyses. In contrast, the four UPPS scales provided significant increments in R2 in three of the five analyses; the increments ranged from 7% for DSHI to 20% for past ideation and future suicide risk, with an average increment of 14%. Of the UPPS domains, Lack of Premeditation was a significant predictor for two of the five outcomes, whereas Negative Urgency was a predictor for one. At Step 2, three product terms were entered to examine interactions between Negative Urgency and each of the other three UPPS scales: Negative Urgency by Sensation Seeking, Negative Urgency by Lack of Premeditation, and Negative Urgency by Lack of Perseverance. The addition of these three product terms accounted for additional variance that ranged from 10% to 18%, with an average change in R2 of .13. This step was significant in four of five analyses. The interaction between Negative Urgency and Lack of Premeditation was significant for four of the five suicidality and NSSI variables. We examined these interactions in terms of the effect of Negative Urgency at high and low levels of Premeditation. The interaction was consistent; relations between Negative Urgency and SB–NSSI were stronger among those low in Premeditation; in each case, the effect of Negative Urgency was nonsignificant among those who premeditate more (βs range from .01 to −.31, ts < 1.72) but significant and strong among those who premeditate less (βs range from .67 to .86, ts > 2.6). Figure 1 provides a graphic illustration of the interaction for future suicidality.
Table 2.
Incremental Validity of UPPS Dimensions Above Borderline Personality Disorder in the Prediction of Suicidality and Self-Harm
| Model | SBQ–14
|
DSHI
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Past suicide attempt
|
Past suicide ideation
|
Future suicidality
|
Overall risk composite
|
Variety of DSH acts—lifetime
|
||||||
| OR | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | |
| Step 1 | .52** a | .23** | .25** | .29** | .16 | |||||
| Sex | 0.66 | −.05 | −.01 | −.08 | −.10 | |||||
| SCID BPD | 0.98 | .07 | .00 | .11 | .08 | |||||
| PAI–BPD | 1.08 | .05b | .07 | .01 | −.06 | .00 | .13 | .03 | .02 | .01 |
| Negative Urgency | 2.99* | .20 | .22 | .09 | .13 | |||||
| SenSeek | 0.94 | .00 | .10 | −.02 | −.07 | |||||
| (Lo) Premed | 0.94 | .25 | .51** | .45** | .16 | |||||
| (Lo) Persev | 1.21 | .20* c | .06 | .10* | −.21 | .20** | −.20 | .13* | .12 | .07 |
| Step 2 | .10 | .18** | .13** | .14** | .10* | |||||
| Sex | 0.74 | −.06 | −.03 | −.12 | −.11 | |||||
| SCID BPD | 1.06 | .10 | −.01 | .10 | .08 | |||||
| PAI–BPD | 1.08 | .06 | −.05 | .12 | .03 | |||||
| Negative Urgency | 4.92 | .38** | .37** | .23 | .27 | |||||
| SenSeek | 0.55 | .01 | .12 | −.01 | −.06 | |||||
| (Lo) Premed | 1.04 | .04 | .29* | .20 | −.03 | |||||
| (Lo) Persev | 0.37 | −.02 | −.20 | −.18 | .11 | |||||
| Urg × SenSeek | 1.17 | .07 | .10 | .02 | .08 | |||||
| Urg × Premed | 0.91 | .37* | .48** | .55** | .41* | |||||
| Urg × Persev | 1.58 | .21 | −.07 | −.13 | −.03 | |||||
| Step 3 | .07 | .02 | .00 | .00 | .05 | |||||
| Sex | 1.20 | −.04 | −.03 | −.12 | −.09 | |||||
| SCID BPD | 1.04 | .02 | −.04 | .10 | −.04 | |||||
| PAI–BPD | 1.05 | −.06 | −.08 | .14 | −.14 | |||||
| Negative Urgency | 5.46 | .36** | .37** | .23 | .25 | |||||
| SenSeek | 0.54 | .02 | .12 | −.01 | −.05 | |||||
| (Lo) Premed | 0.61 | .08 | .29* | .21 | .02 | |||||
| (Lo) Persev | 0.33 | −.01 | −.20 | −.18 | .12 | |||||
| Urg × SenSeek | 1.24 | .08 | .10 | .02 | .09 | |||||
| Urg × Premed | 1.00 | .38* | .47** | .56** | .43* | |||||
| Urg × Persev | 1.63 | .19 | −.08 | −.12 | −.06 | |||||
| MPQ–SR | 1.69 | .23 | .07 | −.03 | .34 | |||||
| MPQ–SR × Premed | 1.11 | −.02 | .03 | −.04 | −.03 | |||||
Note. SBQ–14 = Suicidal Behaviors Questionnaire—14; DSHI = Deliberate Self-Harm Inventory; OR = odds ratio; SCID = Structured Clinical Interview for DSM–IV Axis II Disorders; BPD = borderline personality disorder; (Lo) = (Lack of; PAI = Personality Assessment Inventory; SenSeek = Sensation Seeking; Premed = Lack of) Premeditation; Persev = (Lack of) Perseverance; Urg = Negative Urgency; MPQ–SR = Multidimensional Personality Questionnaire—Stress Reaction scale.
Change in R2 is due to the new variables included in that step.
Increment in variance accounted for by the two BPD measures above and beyond other variables in the model.
Increment in variance accounted for by the four UPPS scales above and beyond other variables in the model.
p < .05.
p < .01.
* p < .001.
Figure 1.
Interaction between Negative Urgency and Lack of Premeditation in the prediction of suicide risk composite.
Specificity Analyses
To ensure that the effects observed for Negative Urgency were not due to its overlap with negative emotionality, we included the Stress Reaction scale and a product term representing its interaction with Premeditation in a third and final step. Results for this step are reported in the bottom of Table 2. Across the five analyses, inclusion of these terms did not provide significant increments in the variance accounted for. More important, the inclusion of these terms did not influence the interaction between Negative Urgency and Premeditation; in fact, the coefficients were unchanged, indicating that Negative Urgency is not standing as a proxy for general negative emotionality.
Discussion
Research on normal and pathological personality suggests that individual differences in personality are important predisposing factors for SB and self-harm. Impulsivity is one “domain” in which the relations with SB and NSSI may be unclear because of the heterogeneous nature of this personality construct. Because of this heterogeneity, it is not known which of the traits underlying impulsive behavior are related to SB and NSSI. In the current study, we used a broad and relatively comprehensive model to examine how impulsivity-related traits are related to SB and NSSI in a sample of inpatient residents at a substance use treatment facility. We also tested whether these impulsivity domains add to our prediction of SB and NSSI above and beyond BPD symptoms—a well-known correlate.
Our first analyses revealed that three of the four UPPS impulsivity domains were relatively consistently related to SB and NSSI; only Sensation Seeking demonstrated no relation with these variables. In general, Negative Urgency and Lack of Premeditation manifested the largest and most consistent effect sizes across the five SB and NSSI variables. These effect sizes were quite consistent with those produced by the BPD scores. In addition, three of the UPPS domains—Negative Urgency, Lack of Premeditation, and Lack of Perseverance—manifested significant relations with the BPD scores. These initial results suggest a substantial degree of overlap among the impulsivity-related traits (minus Sensation Seeking), BPD, and both SB and NSSI.
Our analyses sought to provide information on the incremental predictive utility of the UPPS impulsivity-related traits: Do these traits provide information not captured by the BPD construct? BPD was chosen because of its empirical salience with regard to the prediction of SB and NSSI. The analyses in Table 2 demonstrate quite clearly that the impulsivity domains provide a substantial amount of predictive validity for SB and NSSI. The four UPPS domains and the three interactions involving Negative Urgency accounted for, on average, an additional 27% of the variance in SB and NSSI. Lack of Premeditation manifested the most consistent main effect; however, this effect was qualified by a significant Negative Urgency by Lack of Premeditation interaction (found in four of the five regression analyses). These interactions worked such that individuals who were high in Negative Urgency and Lack of Premeditation were at particular risk for suicidal ideation and behavior, as well as past nonsuicidal self-injury. Given the difficulty of detecting interactions, particularly in smaller field samples, it is noteworthy that this same interaction emerged for four variables that were derived from two assessment tools. Because of the more exploratory nature of these analyses, however, these findings require further replication.
Our analyses also addressed whether BPD accounted for additional variance in the prediction of SB and NSSI above and beyond that provided by sex and the UPPS impulsivity traits. Unlike the earlier results for the UPPS, the two measures of BPD provided no increment in predictive utility (mean change in R2 = .02) in any of the five analyses. The fact that BPD failed to provide any incremental validity above the UPPS, whereas the UPPS did provide substantial incremental validity above the two BPD scores, is all the more impressive when one considers that both BPD scores include specific content related to suicidality and self-harm. We purposely conducted the analyses with this predictor–criterion overlap in place so as to set a particularly high threshold for the impulsivity-related traits.
Finally, it is interesting to note that the correlates of the suicidality variables and the NSSI variable were quite similar. Both constructs were, in general, significantly related to measures of BPD and to the impulsivity-related traits, with the exception of Sensation Seeking. These findings are somewhat contrary to arguments that suggest that suicide may be associated with different correlates than those related to NSSI (e.g., Muehlenkamp & Gutierrez, 2004; Wong et al., 2007). The previous studies were conducted with adolescents, whereas the current sample comprised adults in a substance use facility. In addition, the current study focused on personality correlates, whereas the previous studies focused more closely on environmental factors, thoughts of suicide, and Axis I symptoms (e.g., depression, anxiety). From an impulsivity perspective, the two sets of behaviors seem to be linked to similar problems with resisting impulses when experiencing negative affect, considering the consequences of one’s behavior prior to acting, and persevering in the face of frustration or distress.
It is important to note certain limitations regarding the present sample. The sample is rather small, which raises concerns about statistical power. Power was adequate, greater than .70, to detect population correlations of .30 or greater. Similarly, in terms of increments in variance accounted for (i.e., accounting for variance above and beyond other variables in the model), power was actually quite high, around .90, to detect increments of 10% or more—increments quite similar in size to those observed for the UPPS scales and the interactions in the present study. Power was still generally adequate, .60, to detect an increment in variance accounted for of 5%. Although power appears adequate for detecting main effects of variables, it was certainly lower to detect interactions that are more difficult to find in observational studies due to typically large main effects, the necessary unreliability of product terms, and the typical multivariate distributions of the variables (Aiken & West, 1991). The sample is also rather unique in that it was selected on the basis of substance abuse rather than suicide, NSSI, or BPD, and was predominantly African American. Thus, the study requires replication in other samples. The sample may also have led to restrictions in range given that all participants had diagnoses of substance dependence and almost one third of the sample received diagnoses of BPD. Such range restriction typically results in attenuated relations among variables; although this leads to greater caution in accepting our null findings (e.g., the absence of effects for BPD), it actually increases confidence in the findings we did observe (e.g., the UPPS scales) as these relations should be even stronger in a less selected sample. It is important to note that there seems little reason to suppose that range restriction differentially influenced the associations among BPD, UPPS, SB, and NSSI.
Overall, these results have important implications for our understanding of the predisposing factors for SB and NSSI. The current findings suggest that impulsivity-related traits from two relatively distinct personality domains—Neuroticism (Negative Urgency) and Conscientiousness (Lack of Premeditation)—are important to understanding SB and NSSI. Specifically, individuals who are high on both of these traits appear to be at substantial risk for suicidal ideation and behavior, both past and future, and NSSI. BPD was related to SB and NSSI when considered alone, but it provided no incremental validity above and beyond the impulsivity-related traits, whereas these impulsivity-related traits provided important information about SB and NSSI even after considering BPD. If these findings can be replicated, they suggest that these two impulsivity traits should be given relative prominence during the assessment of suicidality and NSSI. In fact, if one had limited assessment time, one could make the case that these traits should be among the first individual differences constructs assessed (after other important variables such as previous attempts, means, and degree of planning).
Contributor Information
Donald R. Lynam, Department of Psychological Sciences, Purdue University
Joshua D. Miller, Department of Psychology, University of Georgia
Drew J. Miller, Department of Psychological Sciences, Purdue University
Marina A. Bornovalova, Center for Addictions, Personality, and Emotion Research, University of Maryland
C. W. Lejuez, Center for Addictions, Personality, and Emotion Research, University of Maryland
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Anestis MD, Selby EA, Fink EL, Joiner TE. The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders. 2007;40:718–726. doi: 10.1002/eat.20471. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychological Review. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: A systematic review. Acta Psychiatrica Scandinavica. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences. 2007;43:839–850. [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. Behavioral and Brain Sciences. 1999;22:491–569. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- Evans C, Lacey JH. Multiple self-damaging behaviour among alcoholic women: A prevalence study. British Journal of Psychiatry. 1992;161:643–647. doi: 10.1192/bjp.161.5.643. [DOI] [PubMed] [Google Scholar]
- Evans J, Platts H, Liebenau A. Impulsiveness and deliberate self-harm: A comparison of “first-timers” and “repeaters. Acta Psychiatrica Scandinavica. 1996;93:378–380. doi: 10.1111/j.1600-0447.1996.tb10663.x. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Personality Disorders. Washington, DC: American Psychiatric Press; 1997. User’s guide for the Structured Clinical Interview for the DSM–IV. [Google Scholar]
- Fischer S, Smith GT. Binge eating, problem drinking, and pathological gambling: Linking behavior to shared traits and social learning. Personality and Individual Differences. 2008;44:789–800. [Google Scholar]
- Fischer S, Smith GT, Anderson KG. Clarifying the role of impulsivity in bulimia nervosa. International Journal of Eating Disorders. 2003;33:406–411. doi: 10.1002/eat.10165. [DOI] [PubMed] [Google Scholar]
- Gaughan ET, Miller JD, Pryor LR, Lynam DR. Comparing two alternative measures of general personality in the assessment of psychopathy: A test of the NEO PI-R and the MPQ. Journal of Personality. 2009;77:965–996. doi: 10.1111/j.1467-6494.2009.00571.x. [DOI] [PubMed] [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23:253–263. [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Linehan MM. The Suicidal Behaviors Questionnaire—14 (SBQ–14) 1996 Retrieved from http://depts.washington.edu/brtc/files/SBQ.pdf.
- Lynam DR, Miller JD. Personality pathways to impulsive behavior and their relations to deviance: Results from three samples. Journal of Quantitative Criminology. 2004;20:319–341. [Google Scholar]
- Magid V, Colder CR. The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43:1927–1937. [Google Scholar]
- Manuck SB, Flory JD, McCaffery JM, Matthews KA, Mann JJ, Muldoon MF. Aggression, impulsivity, and central nervous system serotonergic responsivity in a nonpatient sample. Neuropsychopharmacology. 1998;19:287–299. doi: 10.1016/S0893-133X(98)00015-3. [DOI] [PubMed] [Google Scholar]
- Miller JD, Flory K, Lynam DR, Leukefeld C. A test of the four-factor model of impulsivity-related traits. Personality and Individual Differences. 2003;34:1403–1418. [Google Scholar]
- Morey LM. Personality Assessment Inventory: Professional manual. Tampa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-Threatening Behavior. 2004;34:12–23. doi: 10.1521/suli.34.1.12.27769. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: Analysis of the National Comorbidity Survey. Journal of Abnormal Psychology. 2006;115:616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Pattison EM, Kahan J. The deliberate self-harm syndrome. The American Journal of Psychiatry. 1983;140:867–872. doi: 10.1176/ajp.140.7.867. [DOI] [PubMed] [Google Scholar]
- Pomplili M, Girardi P, Ruberto A, Tatarelli R. Suicide in anorexia nervosa and bulimia nervosa. In: Swain PI, editor. Anorexia nervosa and bulimia: New research. Hauppauge, NY: Nova Science Publishers; 2006. pp. 1–26. [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14:155–170. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- Trull TJ. Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology. 2001;110:471–481. doi: 10.1037//0021-843x.110.3.471. [DOI] [PubMed] [Google Scholar]
- Wacker J, Chavanon ML, Stemmler G. Investigating the dopaminergic basis of extraversion in humans: A multilevel approach. Journal of Personality and Social Psychology. 2006;91:171–187. doi: 10.1037/0022-3514.91.1.171. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five-factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS Impulsive Behaviour Scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19:559–574. [Google Scholar]
- Wong JP, Stewart SM, Ho SY, Lam TH. Risk factors associated with suicide attempts and other self-injury among Hong Kong adolescents. Suicide and Life-Threatening Behavior. 2007;37:453–466. doi: 10.1521/suli.2007.37.4.453. [DOI] [PubMed] [Google Scholar]