Abstract
Though the US passed the Genetic Information Non-Discrimination Act, many questions remain of how individuals confronting genetic disease view and experience possible discrimination. We interviewed, for 2 hours each, 64 individuals who had, or were at risk for, Huntington’s Disease, breast cancer, or Alpha-1 antitrypsin deficiency. Discrimination can be implicit, indirect and subtle, rather than explicit, direct and overt; and be hard to prove. Patients may be treated “differently” and unfairly, raising questions of how to define “discrimination”, and “appropriate accommodation”. Patients were often unclear and wary about legislation. Fears and experiences of discrimination can shape testing, treatment, and disclosure. Discrimination can be subjective, and take various forms. Searches for only objective evidence of it may be inherently difficult. Providers need to be aware of, and prepared to address, subtle and indirect discrimination; ambiguities, confusion and potential limitations concerning current legislation; and needs for education about these laws. Policies are needed to prevent discrimination in life, long-term care, and disability insurance, not covered by GINA.
Keywords: Discrimination, Stigma, Ethics, Genetic testing, Law, Policy, Insurance, Disclosure, Education
Introduction
Fears of potential genetic discrimination have been voiced in the United States (U.S.) since the beginning of the Human Genome Project (Miller 2000), yet many critical questions remain concerning how and when individuals at risk for genetic disease perceive or experience discrimination. In the US, the Genetic Information Non-Discrimination Act (GINA) became law in May 2008, and some patients, family members, and even providers may feel that potential problems have thus now been resolved. But it is still not clear how patients, family members, and health care providers proceed in their decisions about testing and disclosure.
According to the Oxford English Dictionary, Discrimination is “…an act of distinguishing…discriminating against people on grounds of race, color, sex, social status…; an unjust or prejudicial distinction” (Oxford English Dictionary, 1993)
Debates continue as to how much actual genetic discrimination exists. In a 1996 study of members of genetic support groups at risk for 101 different disorders, a proportion felt that they or their family were refused life insurance (25%), or health insurance (22%), or were denied or fired from a job (13%) (Lapham et al. 1996). In the UK, 34% of members of genetic support groups (vs. 5% of the general population) have had problems obtaining life insurance (Low 1998). Hall found (Hall et al. 2005) that 40% of patients agreed that genetic testing might prompt difficulties in obtaining or maintaining health insurance.
Yet, critics have argued that complaints of discrimination have been exaggerated (Nowlan 2002; Nowlan 2003; Wertz 2002), based on “subjective impressions”, and have been anecdotal, rather than objective; and that objective data are needed to assess whether alleged instances of discrimination have in fact occurred, and if so, been legal or illegal (Otlowski 2005; Otlowski et al. 2003; Treloar et al. 2004). Hall and Rich suggested that pre-symptomatic individuals with serious genetic conditions had little or no problems obtaining health insurance (Hall and Rich 2000); however, these researchers interviewed mostly individuals in the insurance industry, and did not interview patients themselves, which may have skewed the sample (35 worked for insurance companies, 30 were insurance agents, 12 were regulators, 29 genetic counselors or medical geneticists, 5 patient advocates, and one was a medical director).
In the U.S., the only case for which the Equal Employment Opportunity Commission has ruled that discrimination on the basis of a genetic disease has occurred has been when a woman was fired after diagnosis with Alpha-1 Anti-trypsin Deficiency (referred to below as “Alpha”) and initiation of treatment due to symptoms (Oveson and Yarborough 2001; Jones and Smith 2003). Hence, this case appears to represent disability more than genetic discrimination. A case settlement also mandated that one company stop from secretly conducting genetic testing on employees with medical complaints (Rothenberg and Terry 2002).
Given the need for data, the Australia Genetic Discrimination Project recently used a large scale survey in that country to try to assess experiences of 951 genetic clients. In response to binary (yes/no) questions, 10% reported discrimination, which occurred in life insurance (42%), employment (5%), family (22%), social (11%), and health domains (20%) (Taylor et al. 2007, 2008). Yet questions remain concerning the degrees and circumstances of such discrimination. Experiences may also differ between countries, based on factors such as whether national health insurance is present (as in Australia and the UK) or absent (as in the US), and the nature and scope of implementation and enforcement of anti-discrimination and other relevant legislation.
Moreover, crucial questions persist about individuals who are aware that they are at risk of a genetic disease (e.g., HD), and may even have early symptoms, but do not want to see a genetic counselor because of fears of discrimination.
In the U.S., despite this lack of data on the exact extent of genetic discrimination, prior to GINA, 46 states passed genetic non-discrimination laws (NCSL 2006). These laws vary widely in scope—e.g., in definitions of genetic disease, types of insurance policies covered, and disclosures of genetic information without consent. The intent of GINA was to prevent “genetic discrimination”, which is generally defined as discrimination faced by an asymptomatic individual who has a genetic mutation—since discrimination faced by a symptomatic individual would be discrimination on the basis of a disability and presumably covered, in the US, by the Americans with Disabilities Act (ADA) (National Human Genome Research Institute 2008). Indeed, recent U.S. Supreme Court rulings have attempted to curtail the scope of the ADA, and to suggest that accommodation under this law is not required for asymptomatic persons (Toyota Motor Manufacturing, Kentuck, Inc. v Ella Williams 2002; Sutton v United Airlines, Inc. 1999). Greely (2005) articulated three strong arguments for enacting GINA: that it can still be important even if only a small number of people may be at risk of genetic discrimination, that discrimination may occur even when it is not economically rational, and that fear of discrimination itself is worth countering through legislation. GINA stipulates that employers and insurance companies cannot discriminate against individuals on the basis of potential genetic conditions, punishable with fines of up to $300,000 (Genetic Information Nondiscrimination Act 2008; New York Times 2008). Potentially, GINA can help reduce fears of discrimination that may deter individuals from undergoing testing (Geer et al. 2001), or participating in research (Otlowski et al. 2003). Yet patient advocates have argued that GINA does not go far enough, as it does not cover life or long term care insurance (Pollack 2008). Hence, whether and to what degree GINA will yield beneficial effects is unclear. In part, GINA was written and passed based on fears more than actual cases of discrimination. Though actual cases may have been avoided because fears and caution have been articulated, evidence of this possibility is lacking. Thus, it is crucial to understand the landscapes and contexts into which GINA has been introduced.
Yet, surprisingly, little empirical data have been published concerning how patients who have or are at risk of genetic disorders view these issues, and when, how and to what degree they have had experiences with discrimination. These issues are important because they may affect patients’ and family members’ decisions of whether to consult with genetic counselors, undergo genetic testing, and disclose risk information to family members, health care providers, friends who may be potential social supports, and others.
Thus, we decided to interview individuals who have, or are at risk for, genetic disorders about these and related issues. We investigated the following major research questions:
How do individuals confronting genetic disease view threats of discrimination?
What concerns, if any, do they have about discrimination?
Have they faced any discrimination, and if so, what was its nature, and when and how did it occur?
What factors, if any, may be involved in experiences and concerns with discrimination that these individuals may have had?
Do these individuals’ experiences and concerns with discrimination have any implications for health care decisions or behaviors, and if so, what and how?
Methods
Sample
We interviewed, for 2 h each, 64 individuals who had or were at risk for one of three disorders—Huntington’s Disease (HD), breast cancer (BC), and Alpha-1 antitrypsin deficiency (Alpha). Demographic information about the sample appears on Table 1. Given how little is known about the actual views, concerns and experiences of discrimination among individuals confronting genetic disease from their own perspective, we chose to examine these three diseases, to understand as fully as possible the ranges of issues and perspectives that could arise. We selected these three disorders since they vary in prevalence and treatability—two critical factors that could potentially affect discriminatory and other responses to them. Alpha is the only genetic disease for which a case of discrimination has been documented as occurring in the US, and on which the EEOC has ruled—that of Terry Sargent when she was fired after requiring treatment. Treatment is available, but expensive, and the disease is relatively rare. (Oveson and Yarborough 2001; Jones and Smith 2003) HD was the first disease for which a mutation in humans was identified, and a genetic test was developed, and is also relatively rare. This disease is fatal, and no effective treatment exists. Breast cancer is far more common—a leading cause of death among women. Treatment is available, but problematic, since prophylactic mastectomies and oophorectomies are invasive and potentially traumatic, and radiation and chemotherapy have many adverse effects. Thus, these three disorders may pose both similarities and difference in terms of any discrimination they may engender. To detect possible differences that may affect discrimination that these individuals may confront, we included in the sample a range in testing and symptom status (i.e., untested, mutation-positive, and mutation-negative; and symptomatic and asymptomatic). Indeed, individuals may have occupied various of these categories over time—i.e., going from untested to tested, and asymptomatic to symptomatic.
Table 1.
Characteristics of Sample
| Disease
|
Total (n=64) | |||
|---|---|---|---|---|
| Breast cancer (n=32) | Huntington Disease (n=21) | Alpha anti-trypsin deficiency (n=11) | ||
| Gender | ||||
| Female | 32 | 9 | 7 | 48 |
| Male | 0 | 12 | 4 | 16 |
| Ethnicity | ||||
| White | 21 | 18 | 11 | 50 |
| Black | 6 | 2 | 0 | 8 |
| Asian | 2 | 0 | 0 | 2 |
| Hispanic | 2 | 1 | 0 | 3 |
| Other | 1 | 0 | 0 | 1 |
| Symptom status | ||||
| Symptomatic | 20 | 6 | 11 | 37 |
| Asymptomatic | 12 | 15 | 0 | 27 |
| Tested | ||||
| Yes | 20 | 14 | 11 | 45 |
| No | 12 | 7 | 0 | 19 |
| Test status | ||||
| Positive | 8 | 10 | 11 | 29 |
| Negative | 11 | 4 | 0 | 15 |
| Indeterminate | 1 | 0 | 0 | 1 |
To recruit participants, we distributed information about the study through disease-focused clinics, studies at our institution, and newsletters; flyers displayed on bulletin boards of our institution; and word of mouth. We recruited separately for each disease. The recruitment materials did not mention, or refer to, discrimination in any way. Individuals contacted the principal investigator if they were interested.
Procedures
With each participant, the PI conducted a confidential in-depth semi-structured interview concerning experiences of having, or being at risk for disease. Interviews were conducted in the PI’s office and took approximately 2 h. The Columbia University Department of Psychiatry Institutional Review Board approved the study, and all participants gave informed consent. Relevant sample sections of the semi-structured interview guide are attached (see Appendix), through which we sought to obtain detailed descriptions of individuals’ views and decision processes concerning genetic testing, and discrimination, and related issues. We chose these probes since they appeared potentially able to yield useful and valuable data that could address the major research questions above. We piloted the interview guide; and used follow-up questions, as needed.
On theoretical grounds, Geertz (1973) has advocated studying aspects of individuals’ lives and social situations not by imposing external theoretical structures, but by trying to understand individuals’ own experiences, drawing on their own words and perspectives to obtain a “thick description.” Hence, to understand more fully the range of factors and issues that may be involved in genetic testing decisions, we used qualitative methods.
Data analysis
We have adapted elements from Grounded Theory, as described by Strauss and Corbin (1990), to aid in our understanding of complex social processes. We have used these methods in several other studies involving genetics (Klitzman et al. 2007a, b, c) and other aspects of health behavior and doctor-patient relationships and communications (Klitzman 2006). Specifically, grounded theory involves both deductive and inductive thinking, building inductively from the data to an understanding of themes and patterns within the data, and deductively, drawing on frameworks from previous research and theories. For example, interviewees introduced topics such as interactions with providers that were then explored further in these and other interviews. Our approach was informed by constant comparison in which data from different individuals were compared for similarities and differences to see whether these suggested hypotheses. Transcriptions and initial analyses of interviews were done during the period in which the interviews were being conducted and helped guide subsequent interviews. Interviews were conducted until “saturation” was reached (i.e., “the point at which no new information or themes are observed in the data”) (Strauss and Corbin 1990; Guest et al. 2006).
Once the full set of interviews was completed, subsequent analyses were conducted in two phases, primarily by the PI together with a research assistant (RA) who had social science training. In phase I of the subsequent coding, the PI and the RA independently examined a subset of interviews to assess factors that shaped participants’ experiences, identifying categories of recurrent themes and issues that were subsequently given codes. These two coders assessed similarities and differences between participants, examining themes and categories that emerged, ranges of variation within categories, and variables that may be involved. The coders systematically coded blocks of test to assign “core” codes or categories. While reading the interviews, a topic name (code) was inserted beside each excerpt of the interview to indicate the themes being discussed. The coders then worked together to reconcile their independently developed coding schemes into a single scheme, developing a coding manual and examining areas of disagreement until reaching consensus between them. New themes that did not fit into the original coding framework were discussed, and modifications were made in the manual when deemed appropriate.
In the next phase of the analysis, we subdivided these thematic categories into secondary or subcodes, and then refined and merged these, when suggested by associations or overlap in the data. Codes and subcodes were then used in analysis of all of the interviews. Major codes (or categories) of text included, for example: occasions when participants felt discrimination. Subcodes (or subthemes) were conceptual and thematic subdivisions of these larger categories and included, for example, types of settings where discrimination occurred, and perceived precipitants of the discrimination, etc. To ensure coding reliability, the two coders analyzed all interviews. We examined areas of disagreement until consensus was reached. To ensure trustworthiness, we triangulated the data with existing literature relating to genetic discrimination. These data also have a certain face validity that, we would suggest, further substantiates their trustworthiness. We have also presented below text from the interviews to allow readers to judge these data for themselves.
Results
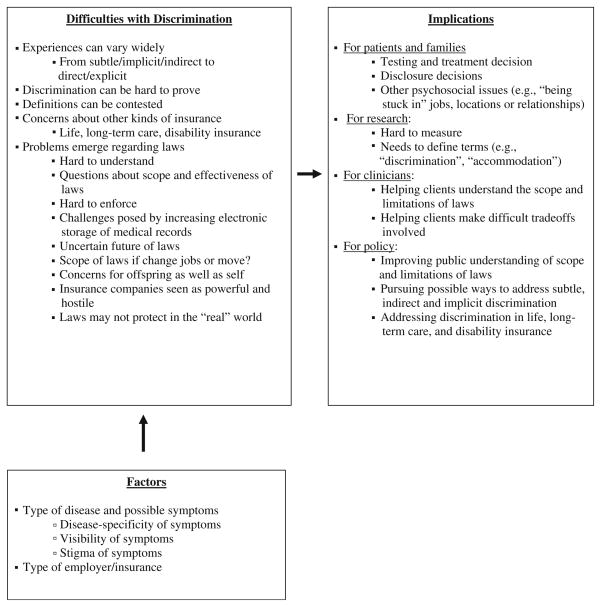
As described below (and outlined on Fig. 1), four major themes emerged in the data:
Fig. 1.
Themes Concerning Discrimination.
Discrimination can take a wide range of forms, from explicit and overt to implicit and subtle
As a result, it can be hard to prove, and laws may be limited in their protections and effectiveness.
Several factors, including the visibility and disease-specificity of symptoms and the nature and age of employers may be involved in concerns about discrimination.
Concerns about discrimination can impede genetic testing, as well as disclosure, treatment, and major career and life decisions, causing stress that could potentially exacerbate illness.
Within each of these major themes, several subthemes emerged.
Importantly, as elucidated below: interviewees feared that discrimination may not be wholly eliminated through legislation; and many interviewees (even if they themselves already had symptoms), and their at-risk family members had strong concerns and experiences over time concerning real or potential discrimination in the absence of symptoms. Symptomatic patients often discussed how, before undergoing testing, they, their families and fellow patients feared and/or experienced discrimination. Moreover, many individuals have had symptoms in the past—e.g., having had breast cancer—but are now asymptomatic. Yet, if they are mutation-positive, or are untested and concerned that they might possess a mutation, they are often concerned that they may be subject to discrimination, despite the ADA. In part, they are not now disabled, but nevertheless would not be covered by GINA, since they have had symptoms. As indicated below, they are often very concerned about potential discrimination they may face, but may “fall between the cracks”, uncovered by either GINA or ADA, or uncertain whether they are covered. Interviewees commented on experiences and concerns that they as well as family members and friends have had in both the past and present, when at various stages of testing and/or symptoms.
Difficulties with Discrimination
Subtle, Implicit, and Hence Hard to Prove
Discrimination can vary widely in clarity and straightforwardness, and occur across a spectrum from direct and overt to indirect and subtle. Discrimination may be subtle, and not fully visible, making it hard to prove. For example, supervisors may not fire an employee, but rather give him or her fewer or less interesting projects.
I just was worried about being viewed differently…. I don’t know if discrimination is the right word—but it’s probably the best word….An analogy is: women who are young and probably going to have kids. Although they aren’t discriminated against, everybody knows: if you hire this person, you might be stuck with a huge maternity leave bill. That influences people, even good people, indirectly. They have reservations, want a back-up plan, and may not give these employees all the work: “I won’t give you all these projects.” It would be illegal. But I’m sure a little bit of that goes on. HD11 (Asymptomatic/Tested/Negative)
Discrimination could be indirect, resulting not from employers’ explicit knowledge of an employee’s mutation-positive test results, but from assumptions that may or may not be correct about his or her risk. Fears arose that even merely knowledge that one is a caregiver of an ill family member could be held against one. One woman said that her sisters kept their HD risk secret, afraid of being fired as a result.
My sisters don’t want anyone at work knowing. Someone asked me, ‘How’s your mother?’ I say, ‘She’s doing OK. She has cancer and Huntington’s disease.’ It’s a little like Parkinson’s, a little like Alzheimer’s. My sister says, ‘You’re so open about that!’ HD8 (Asymptomatic/Not Tested)
Her sister instead advocates and adopts more caution. Yet again, this indirectness can make discrimination difficult to prove. Discrimination can result from absences or gaps in an employee’s work history, due to the indirect effects of being at risk of a genetic disorder, such as having to care for affected relatives and/or dealing with psychological difficulties arising from the potential diagnosis. Having to explain gaps in one’s work history can lead to discrimination in job hiring—e.g., losing jobs because of being “supposed to be able to explain” time when not working due to such care-giving.
Co-workers didn’t know my diagnosis, but knew my father was sick. At times, I actually had to call in sick because of his illness. I told my supervisor about the situation. According to my mom, I got laid off because I called in sick too many days…They just said they couldn’t “afford the position” anymore. The first thing out of my mouth was: did I do anything wrong? They said absolutely not. Maybe, it’s a combination. I was the youngest employee—there less than a year. There were always budget cut issues. They were talking about out-sourcing the whole department…I told a supervisor the disease was Huntington’s, and explained it...But I don’t think that was an issue. HD17 (Not Tested/Asymptomatic)
Still, uncertainty lingers here. In the “messiness” of the “real world”, pinpointing explicit evidence of discrimination can be hard in part since factors other than genetics may be involved in a company’s decision to lay off an employee. As one asymptomatic lawyer said,
If the partners knew about this, it might unconsciously affect them: should we make this guy partner? They wouldn’t say it. They would just think to themselves, “I’m gonna vote no,” and raise their hand when the “no” vote comes along. There are so many factors that go into it, you couldn’t necessarily pinpoint this one thing. It could be a decisive factor, and you would never know…Maybe one person in 10…makes partner. You could easily not make partner, and you wouldn’t have much to say about it. HD4 (Asymptomatic/Tested/Mutation positive)
He felt he would have little recourse.
Contested Definitions
Aspects of discrimination, particularly perceived insensitivity and lack of accommodation, often turned out to be difficult to define. For example, with Alpha, environmental exposures could precipitate symptoms in individuals who have not yet developed any symptoms and thus are still technically asymptomatic. Hence, questions arise of whether they require accommodation which would not however be covered by the ADA—since they are not as of yet symptomatic. GINA does not, however, concern itself with questions of accommodation. Discrimination can arise through failure of a workplace to accommodate an asymptomatic individual at risk for Alpha by limiting possible exposures to environmental irritants, exacerbants or toxins. Employers vary in their willingness to accommodate individuals for types of environmental exacerbants, including co-workers’ perfumes that can precipitate Alpha symptoms in asymptomatic patients. Though on the one hand, a few patients felt well accommodated at work, others felt compelled to accommodate on their own—even by quitting, if need be. Still other patients felt that accommodation was not feasible, and hence unreasonable (i.e., it would be “asking too much” of bosses). Definitions of “appropriate accommodation” can thus be contested.
Patients felt that employers and co-workers could be insensitive, chastising, antagonistic or even hostile to an employee’s missed work to attend his or her own doctors’ appointments. One might argue that these experiences reflect disability discrimination, rather than genetic discrimination per se (i.e., occurring in the absence of symptoms). But these experiences may not be due to explicit symptoms or actual disability, and in fact reflect critical challenges and ambiguities that patients face, and that thus deserve attention. In these situations, co-workers may think a patient is “taking advantage of the situation”, raising questions of how much leeway patients should receive, who should decide, and what should be done when disagreements occur.
Questions arose, too, as to when “being treated differently” constituted discrimination. For example, coworkers may become “overly concerned”, closely monitoring an at-risk individual, implicitly questioning his or her decisions to enter and/or exit the sick role. Over-solicitude can itself potentially verge on discrimination. Before testing mutation-negative, one woman said about an office-mate,
I felt she was watching me, listening to my phone calls, wondering if I’m ok. When the whole Huntington’s nightmare started, when I drop or forget something I definitely felt exposed, and wished I had kept it to myself. HD12 (Asymptomatic/Tested/Mutation Negative)
Concerns About Other Kinds of Insurance
Concerns emerge about not only health insurance (which is covered by GINA), but life, disability and long-term care insurance. Patients fears of not being able to obtain these other types of coverage. Some thus try to get such insurance before initiating testing. As one man said about his sibling,
He still gets a pretty good chunk of money from his disability policy because he had it in place beforehand, which is good. HD13 (Asymptomatic/Tested/Negative)
Insurance companies were seen as having an inherent conflict of interest in seeking and obtaining patient’s genetic test results—providing care vs. saving costs.
It’s a conflict of interest. Their duties are different than a physician’s duties to help people. BC16 (Asymptomatic/Not Tested)
But individuals at risk may not be aware of the possible advantages of obtaining insurance before testing, or they may be unable to get it. Hard questions persist, too, about whether and when to use insurance, if one has it—e.g., whether to pay for genetic testing out-of-pocket.
Many concerns surfaced, too, about life insurance companies discriminating based on pre-existing conditions. Questions arose concerning the definitions of “pre-existing condition”. For example, some individuals feared that companies could see even the suspicion of an Alpha mutation as constituting a pre-existing condition. Individuals worried that they did not even have to be tested or diagnosed for companies to argue that such a pre-existing condition existed, justifying decisions not to provide coverage.
There are homozygote asymptomatics who couldn’t get life insurance. The insurance company asked if they’ve had any genetic tests. A guy I knew had an identical twin brother who had liver disease and died. The guy I knew was asymptomatic, but couldn’t get life insurance at the normal rate. He didn’t have to be tested. If his identical twin had it, he had it. Is that a pre-existing condition? I think not. If you’re Z-Z, and you’re wife’s Z-Z, do your kids have a pre-existing condition when you get diagnosed? I don’t know. A10 (Symptomatic/Tested/Positive)
Children may be known to be carriers based simply on parents’ test results, without being tested themselves.
Similar questions about discrimination for life insurance emerged for breast cancer as well. Relatedly, uncertainties arose of how health as well as life insurance companies would respond if one had testing done, and then surgery. Would discrimination occur? It may, because statistically, the risk of recurrence of a second cancer increases.
Let’s say I’ve never had breast cancer, and I get the genetic test, and it says “Ok, I’m going to get breast cancer, and I shouldn’t be hired.” That will affect life insurance. But if I decide to have this prophylactic surgery, will the insurance company still pay for it because I’m doing it as a protective? I’m assuming yes. BC4 (Symptomatic/Tested/Positive)
Uncertainties and anxieties persist about what insurance companies will or will not cover both at present and in the future.
Views of Laws
Many individuals felt that laws designed to impede discrimination could potentially serve several important functions, but may ultimately be limited in impact.
Laws as Hard to Understand
Many patients were confused and uncertain about current laws. Frequently, they had little knowledge about privacy and anti-discrimination policies that might in fact protect them.
We weren’t sure exactly what was covered where. If things are present before you get sick, there can be issues. BC26 (Asymptomatic/Tested/Negative)
Wariness and uncertainty may persist, despite genetic counselors communicating about these laws. In fact, legislation itself may be unclear, fluid and untested.
I don’t know how much I’m protected. I’m worried, but don’t feel I have much information. Genetic counselors told me you can’t be turned away—pretty much every state has a law that says that genetic testing can’t be held against you in getting coverage through a group. BC13 (Asymptomatic/Tested/Positive)
But she remains uncertain.
In part, policies often entail long and complex forms. Many patients do not have the interest or time to read and understand them fully, which poses serious challenges as to these documents ultimate meaning, purpose, and outcomes. Even the leader of a genetic support group, who was relatively sophisticated about many genetic issues, said,
All I know is that I had to sign a lot of forms, I haven’t read them, because they haven’t been a paragraph—but four, five pages.” A11 (Symptomatic/Tested/Positive)
Questions About the Scope and Effectiveness of Laws
Many were unclear or wary about the scope and limits of laws designed to decrease discrimination. In part, discrimination can involve implicit attitudes, not just explicit, objectively observable behaviors, and thus be hard to identify and reverse.
Genetic privacy and discrimination laws are great, but subtle discrimination could go on. A law couldn’t really intervene in those kinds of situations. The law certainly makes strides, but can’t necessarily affect subtle, hidden attitudes. It hasn’t really affected those with respect to minorities, women, homosexuals, or people with mental illness. I see no reason to believe it would somehow affect subtle, subtle discrimination toward people who have genetic disorders. I’m a firm believer in law, But I don’t think even the best drafted law could really extricate the subtle discrimination that goes on. HD4 (Asymptomatic/Tested/Mutation positive)
He suggests that not only subtle, but “subtle, subtle” discrimination occurs.
Hard to Enforce
Patients do not always trust such policies as reliable safeguards “in the real world,” since enforcement is difficult. Moreover, many individuals feel powerless to challenge violations of anti-discrimination legislation, sensing employers’ power to bypass laws.
Even though morally, they can’t fire you, they can find something. Basically, if they want you out, they can get you out. There are laws, but people finagle. HD9 (Asymptomatic/Not Tested)
Hence, questions arise as to whether laws can or would be enforced, and if so, to what degree. On the one hand, at times, individuals felt that a law, even if not wholly enforced, could still have certain value, even though limited. Legislation may have important symbolic value, and hence some beneficial effect—sending the message that privacy “counts.” One symptomatic woman, who decided not to be tested, clearly voiced these limitations and concerns, which many asymptomatic individuals shared.
The laws are a pain in the ass to enforce. Often, there’s not much penalty attached. Usually, the cat’s already out of the bag—the harm is done. These laws need to be there. They help create a standard, even if they’re not followed all the time. But it’s unrealistic to think that just because a law is there, it’s going to be followed. BC7 (Symptomatic/Not Tested)
Others were even more wary. One asymptomatic woman, who worked for an HIV organization, was highly cognizant of gaps between laws and their enforcement.
A problem is enforcement. Laws don’t protect people. You can say you’re not allowed to discriminate based on sex, race, whatever, but it happens all the time. BC25 (Asymptomatic/Tested/Negative)
These views extended across diseases. A female patient with Alpha similarly recognized limitations of laws—citing common discrepancies between the ideals underlying and prompting legislation vs. the realities of enforcement and implementation.
Universal Health Care! [laughs]—Wouldn’t that be something? But people who have huge bills with genetic or any disease will still have to worry about how to pay, and about discrimination, because laws aren’t necessarily enforced. A1 (Symptomatic/Tested/Positive)
Challenges Posed by Increasing Electronic Storage of Medical Records
Concerns about discrimination and burgeoning electronic storage of medical records exacerbated each other. Information should be kept in a “safe place,” but may not always be protected in this way. Increased use of electronic medical records heightens these anxieties, and the growing loss of health privacy frightens many.
Maybe one day we’ll have a national number, and all of our information will be on a disk. Given things in healthcare already, taking away patient autonomy, who’s gonna be actually calling the shots? That worries me. BC16 (Asymptomatic/Not Tested)
Others see laws to protect privacy and confidentiality as inherently limited in practical scope and effectiveness since at doctors’ offices, patients must often nevertheless sign away their confidentiality. In the end, rights and choices may be illusory.
Nowadays, you keep signing all these release forms. On the one hand, you are told that you are entitled to these privacy laws. But instantly everyone makes you sign these release forms, so it’s totally meaningless. I think individuals rights to privacy should be absolutely guaranteed. If you refuse to sign, and want a job at a corporation, you are free not to apply. That’s your only choice. BC24 (Symptomatic/Tested/Negative)
Though she is symptomatic, she has concerns (i.e., that despite legislation, discrimination can still occur) that asymptomatic individuals share as well.
Many simply distrust insurance companies, given high costs of medical treatments, and selfishness and greed that are deeply embedded in human nature. Symptomatic patients who needed treatment and thus health care coverage were acutely aware of the potential limitations of current legislation. These individuals highlighted concerns prevalent in patient communities, in which asymptomatic patients, too, are often involved and make testing decisions.
There is tremendous pressure to reduce medical costs. They would not hesitate to damage people. I don’t trust the industry, the economists, the legislature, or the doctors—based on my very low view of mankind. Mankind has proven to be weak for whatever reasons—economic, social, whatever—and will discriminate, and misuse their knowledge of someone else’s condition. A11 (Symptomatic/Tested/Positive)
This wariness and concern about cost-cutting echoes that of many asymptomatic individuals as well. Indeed, even GINA does not prohibit health insurers from increasing premiums for symptomatic individuals. In confronting these inevitabilities of potential information leaks and discrimination, many simply felt helpless and resigned. Some felt that economic “realities” made complete privacy and confidentiality virtually impossible. Tensions emerge since absolute protection of privacy can be costly, and lower levels of protection may be more realistic economically, but be more likely to lead to leaks and subsequent discrimination.
No matter how hard you try, if someone wants to remain anonymous, I don’t think anyone can guarantee that—that the information you give them will remain private. [Doctors] do the best they can. But people have ways of obtaining that information if they want. It’s all on computer files. I worked for a surgeon who said, “Give me 24 h, and I can find out everything there is to know about you. Your medical history, financial history, anything.” Unfortunately, I guess you have to accept it. What can you do? Kids have hacked into Pentagon computers. That’s the way the world is. A5 (Symptomatic/Tested/Positive)
The Uncertain Future of Coverage
Many also fear that coverage and/or laws could change, especially since insurance companies have economic and political clout. Individuals both with and without symptoms were wary of the precariousness of laws. Those without symptoms were concerned about discrimination once they got sick. For those who were at risk, but untested and asymptomatic, discrimination could at times be more abstract, but nonetheless be a source of fear. One’s own personal and/or financial circumstances or those of one’s family could also change, jeopardizing coverage. Insurance companies were seen as generally unaccommodating and rigid.
I don’t know if my husband’s going to change jobs, or we get new insurance, or something happens and he’s not working, or I have to go to work. It just might not be full coverage, or be different. Who knows? Everything could change. BC26 (Asymptomatic/Tested/Negative)
The interpretation and implementation of current law by courts and others, and possible changes in the law generated concerns as well.
The insurance companies are really powerful lobbies. So I don’t trust: that just because my result is not supposed to lead to discrimination now, that it always will. When we have more information, insurance companies are going to say it’s actually legitimate for them to insure differently. BC7 (Symptomatic/Not Tested)
The law may not be able to prevent differential treatment by insurance companies (e.g., higher rates for symptomatic employees); but uncertainty and apprehension persist as to the extent of these differences.
On-going economic vagaries exacerbate these anxieties. Many worry that employers or insurance companies could eventually go bankrupt, and that insurance plans could thus alter regardless of symptom status. Individuals expressed concerns about insurance benefits ending.
Before, they couldn’t boot me out of coverage, because I was in the group. But now, I will be facing this question because the company has declared Chapter 11 bankruptcy, and it’s virtually certain that retirees will be losing their healthcare coverage. I may have eligibility for 18 month COBRA extension. I don’t know whether I can be turned down in this state or not, but I’d just as soon not even find out. A4 (Symptomatic/Tested/Positive)
Clearly, many are also unsure about the specific laws in their state, because these are often unclear, difficult to understand, or in flux.
Individuals worried about discrimination in future coverage for not just themselves, but their children, too. Indeed, some were concerned about privacy and discrimination more for their children than for themselves. Employers and others could inquire about an individual’s own genetic test results, or those of his or her parents.
I’m concerned about my kids—their future choices, and career-decisions, jobs and insurance—more than how all this affects me. How does anything on the record pertain to their life’s journey? Alpha arrived in my life late. So I went along with other decisions, without considering it. They might not get insurance, or it may be limited. Perhaps an employer may at some point have access to every known thing about us. A2 (Symptomatic/Tested/Positive)
Thus, the offspring of an individual with a mutation—whether this parent is symptomatic or not—may potentially confront discrimination. Parents fear such prejudice, and as a result can alter their testing and disclosure decisions. GINA covers discrimination based on family history—not just genetic tests alone—and indeed, these individuals are clearly concerned about such discrimination.
Implications
These fears about discrimination have several critical sets of implications, affecting decisions about testing, disclosure, and other areas, creating difficult stresses for individuals.
Testing and Treatment Decisions
At times, these discrimination concerns could hamper decisions to pursue testing. A woman at risk for HD said,
My sisters are so afraid that if their company finds out, they might get fired… They don’t want to be tested because of that. HD8 (Asymptomatic/Not Tested)
Fears of discrimination can hamper testing for Alpha, too.
People are afraid of it getting on the record, so they don’t get tested. The people I know who tested were already very sick. The son of a guy in our group is beginning to be symptomatic. The father tells him to get tested, but he just refuses. “I don’t want to know, and don’t want it on my record.” And you have to reach a certain level before doctors consider Prolastin. A6 (Symptomatic/Tested/Positive)
These fears or violations of confidentiality can thus preclude testing—until symptoms develop and become more serious, which can take time.
Such discrimination concerns led, too, to desires to test certain family members instead of others. One woman decided to test for BRCA in order to help her offspring. Her daughter said,
When my mom had ovarian cancer, she decided to get genetic testing for the benefit of me and my sister: to inform us, so we could decide what to do for ourselves. BC13 (Asymptomatic/Tested/Positive)
If this mother did not have the mutation, her daughters would therefore not have it either, and would not have to undergo testing, and risk receiving a mutation-positive result that, these individuals feared, could potentially prompt discrimination.
Due to fears of discrimination, others eschewed testing themselves, and instead actively tried to persuade family members—not always successfully—to undergo it. These test-avoiders sought to have family members’ genetic status checked—to gauge these other parties’ risks. Some of these test-avoiders tried to convince a parent to test, so that neither they nor their children would have to do so themselves. One woman reported, “I said to my mom, ‘I want you to be tested for us.’” HD8 (Asymptomatic/Not Tested) This woman’s offspring would then not be at risk if her mother (their grandmother) were mutation-negative.
I don’t want my kids to go through the stress of being tested. If I come out negative, they don’t have to be tested, and go through that stress. HD8 (Asymptomatic/Not Tested)
Conversely, some tested without thinking about the potential risks to privacy—and often later regretted not having considered these threats beforehand.
Fears of discrimination led many to struggle with difficult dilemmas of not only whether to test or not, but if so, whether to use one’s insurance to cover the cost, if that were an option. One computer programmer did not use her insurance for the test, and paid in cash.
I wasn’t sure I wanted a record of having the test in the government data bank. So I paid out of pocket. I didn’t really want a record of having this test, not yet knowing what the results were. BC26 (Asymptomatic/Tested/Negative)
She and others were cautious because they were uncertain about what their insurance covered.
Yet depending on the particular genetic test, others felt that the high financial costs of testing left them little choice. Many at risk of HD were able to undergo testing through research protocols, but those confronting other diseases often did not know of, or use, such an option. Instead, they had to weigh costs against the odds of possible discrimination. Many felt they had no choice but to have their insurance company pay.
My health insurance would cover it. I thought: I pay for this health insurance. I don’t want this to be a financial burden now. I didn’t want to pay for it myself. But I was concerned because I didn’t know what it would mean for getting other coverage in the future…If they found out I got the test, and I then started having surgeries afterwards, they could put two and two together. It wasn’t clear that I wouldn’t get health insurance in the future. But it was a concern. BC25 (Asymptomatic/Tested/Negative)
Disclosure Decisions
Fears of discrimination, and lack of legal protection against it also shaped decisions about whether, and to whom to disclose one’s genetic risk. Wariness of possible discrimination can impede disclosures even to at-risk family members. Some did not even want to know a family member’s test result, so that they could claim ignorance if asked about it.
I didn’t want my mom to tell me for a long time, so she didn’t. I didn’t want to officially know, because if anyone asked me, I wanted to be honest and say I didn’t know. I assumed that if she didn’t tell me she was negative, she was probably positive. I don’t know how paranoid to be about getting health care and being discriminated against. BC13 (Asymptomatic/Tested/Positive)
In the face of uncertainty about having health insurance in the future, some were highly risk averse, and preferred to exercise caution—even though it would mean keeping secrets in the family, which could in turn cause strains.
Fears of discrimination can also impede wider disclosures (e.g., to friends)—even of simply the fact that someone else in a family, but not oneself, was affected. Such lack of disclosure can cause stress, too, since it could entail foregoing certain sources of support. Questions arose of whether one should disclose family members’ test results or history, or at times perhaps feign ignorance about it.
A few considered going public, in order to advance wider understanding of their disease, and reduce stigma. But concerns arose about the potential impacts on other family members who were asymptomatic and currently untested. These others may have a mutation.
One man wanted to publicize Alpha-1. His local TV station said, “We’ll come interview you.” If his son still lived there, he wouldn’t do it. But his son had moved away. His son could be a carrier or have the disease. That would lead to discrimination in employment and insurance. A1 (Symptomatic/Tested/Positive)
Being Stuck: Other Psychosocial Decisions
Possible discrimination could affect a wide range of other psychosocial decisions. Given uncertainties and distrust, many were simply afraid to risk altering their current coverage, even if they otherwise desired to change jobs or locations. One asymptomatic woman and her boyfriend in fact chose to get married, partially for insurance purposes.
Part of the reason why I decided to get married was that I would be more protected in terms of health insurance. Health insurance was just one added advantage. If you try and buy your own health insurance, they can discriminate against you, which scares me. BC13 (Asymptomatic/Tested/Positive)
Fears of possible discrimination could prevent individuals from moving to a different geographic location, or changing jobs. For instance, one woman wanted to relocate to another state for health reasons, but felt that she could not do so because of perceived threats to her insurance.
I can’t move out of state, because my insurance is a New York company. It doesn’t go with you. They can’t cut me off, but I can never move out of the city. I want to move to the South, because the winters are warm. I like it there. But I’m stuck. Legally, if you keep an address here, you need to have an apartment here. But I’m on disability. A3 (Symptomatic/Tested/Positive)
She could not afford two apartments: one in each location. Laws may in fact help protect her, but she simply does not trust these enough.
Worries about keeping insurance generally outweighed those about jobs. One woman said about fellow at-risk women,
I haven’t heard anyone say, “I’m worried I’m going to get fired.” But I have heard concern about being able to maintain insurance, switching jobs. BC9 (Symptomatic/Tested/Positive)
Factors Involved in Discrimination
Several factors can shape whether, and to what degree, discrimination occurs.
Type of Disease and Possible Symptoms
Certain symptoms, such as psychiatric ones, generate stigma and potential discrimination in and of themselves, whether or not they are recognized to be related to genetic or other disorders (e.g., HD). Hence, difficulties arise because HD—even if testing has not occurred—can cause non-specific, non-diagnostic psychiatric symptoms that can prompt interpersonal difficulties. Patients with HD may encounter antagonism not due to the fact of having a genetic illness, but because of these behavioral problems in and of themselves. More stigma may be attached to psychiatric problems than to other aspects of genetic disorders. Individuals eventually found to have HD often had earlier inter-personal problems that were not seen at the time as symptoms of any major diagnosis, and viewed only in retrospect as possibly related to a disease. Yet such early, non-diagnostic problems may generate discrimination.
One of my sisters was always difficult to get along with. I always knew she had a lot of problems—she just wasn’t sociable. She lived alone. If you got on her nerves, she’d tear your head off. A tough cookie. By the time her illness had progressed in her, she had very few friends. HD2 (Symptomatic/Tested/Positive)
Family History
As suggested above, whether others in a family are affected, and if so, to what degree, can also precipitate discrimination. Individuals who are caregivers of ill family members may themselves confront discrimination.
Types of Employer and Insurance
The type and size of employer can affect concerns and experiences related to discrimination. Trust of employers and coworkers proved important, and resulted from an amalgam of factors. Often, trust appeared to shape concerns about discrimination more than any one isolated, cross-cutting objective factor, such as the size of companies. Both large and small companies were seen as having potential advantages and disadvantages. For instance, on the one hand, small companies can be friendly, promoting trust.
Everybody at work knows. I work for a small design studio, and had an accident, and needed a lot of coverage. They covered me. It was fine. I’ve been there 8 years, and they’re like my family. When my mother does things that really upset me, I go to work and cry. I never thought ‘I shouldn’t tell them because maybe they’ll fire me.’ HD16 (Asymptomatic/Not Tested)
Yet, large companies can have more formalized institutional safeguards and procedures to ensure protection, and may be less threatened by the potential impact of increased medical expenses for any one employee. Employees may thus feel protected by a company’s large size.
This company is such a huge bureaucracy that the information wouldn’t go anywhere. BC13 (Asymptomatic/Tested/Positive)
Discussion
These data reveal critical aspects of the ‘lived experiences’ of discrimination among individuals confronting genetic diseases, illustrating how discrimination can take a wide range of forms. Importantly, discrimination can be indirect, implicit and subtle, making it hard to prove, which in turn can have several critical implications. It may impede not only genetic testing and research, as has been suggested in some prior research (Otlowski et al. 2003; Billings et al. 1992), but also disclosure, treatment, and major career and life decisions, causing stress that could potentially exacerbate illness.
The data suggest that wide and profound confusion about health insurance exists—e.g., what insurance companies are required to offer. Misunderstandings and confusion regarding the law (e.g., the transferability of insurance), exacerbated by mistrust of insurance companies’ motives, can lead to fears of possible discrimination that may or may not be entirely realistic, but nonetheless prevail, and potentially impede individuals in deciding whether to pursue testing and/or treatment. Such uncertainty, fears and wariness about insurance can lead individuals to take unnecessary precautions that may cause additional stress. A critic could potentially simply dismiss entirely these individuals’ fears and concerns about discrimination as not objective, but the data here suggest that these anxieties can nonetheless profoundly affect individuals’ health decisions and behaviors.
These data highlight, too, critical needs for the development of legislation to cover long term care insurance, and life and disability insurance, given these interviewees’ concerns about these areas as well. These individuals also express concern that genetic discrimination could be based on family history—not the results of a genetic test. Yet compared with genetic test results, family members’ diseases may be mentioned and discussed among coworkers as part of on-going daily interactions (i.e., that are not protected by privacy laws) rather than revealed solely through medical history forms. Consequently, an individual’s family medical history, more than his or her genetic test results, could be known by others, and prompt subtle discrimination.
Policy makers may distinguish between discrimination faced by asymptomatic vs. symptomatic individuals, and define genetic discrimination as referring only to that faced by asymptomatic individuals at risk, but the data here suggest several critical complications. Importantly, patients and family members here tend not to see this differentiation as distinctly or sharply, and rather, often perceive these realms as blurring. In part, these disorders themselves may have intermediate “grey areas”—e.g., possible (but not definitive) and/or non-specific symptoms. For instance, individuals who are at risk for HD but untested may be “difficult to get along with”, which may, only in retrospect, be seen as representing early, non-specific, non-diagnostic symptoms of the disease. Yet these inter-personal difficulties may nonetheless prompt discrimination. Similarly, exposures to environmental irritants may precipitate symptoms in otherwise asymptomatic individuals at-risk for Alpha. Thus, the distinction between symptomatic vs. asymptomatic may not be wholly clear, and individuals may face discrimination due to symptoms that are not yet recognized as caused by a genetic disorder. Other genetic diseases can no doubt pose such complications as well. Moreover, symptomatic and asymptomatic individuals are frequently members of the same families and disease communities. Fears of discrimination against symptomatic individuals may heighten anxieties among their asymptomatic family members, affecting the latter’s decisions. Hence, asymptomatic individuals may make decisions about testing and careers based on fears of whether and how they might be later covered or not covered by the ADA.
The current data suggest that patients may confront subtle discrimination, and that fears and concerns arise among individuals who have not been to genetic counselors (in part because of fears of genetic discrimination that may result from testing). Hence, genetic counselors may have little awareness of these individuals’ experiences and fears.
Though Greely (2005) presented three strong arguments for enacting GINA, the data suggest an additional benefit of anti-discrimination laws: reduction of ‘subtle discrimination’, against which legislation may have important value, both symbolic and “real”. We found only one mention of subtle discrimination with regard to race (Charles 1999), (which was on-line, and none in any academic journals) but none regarding genetics, where it may have important similarities as well as differences. Though “unconscious” discrimination has been mentioned with regard to other areas (e.g., race) (Legal Times, May 21, 2007), subtle discrimination, as it appears here, is in fact conscious.
Questions emerge of whether differences arise between asymptomatic individuals who have vs. have not been tested. Yet such a comparison may have certain limitations. An outside observer may seek to apply a hard and fast distinction between the experiences of these two groups, but in fact this line may be blurry. As we have described elsewhere (Klitzman et al. 2007b), symptomatic individuals may or may not undergo testing, based on complicated psychosocial reasons. An individual at risk of HD may suspect possible symptoms in him or herself, which may or may not in fact be present, and of which he or she, but not others, may be aware. This individual may not have been tested, but his or her fears of having the mutation can nevertheless prompt wariness of testing and disclosure of this genetic risk (e.g., to co-workers who are friends). An untested asymptomatic individual with subtle, non-specific symptoms may also experience subtle discrimination, regardless of whether or not he or she undergoes testing.
These results mirror efforts historically to eliminate other kinds of discrimination—e.g., attempts to address civil rights in the 1960s, and discrimination based on gender and sexual orientation. These prior endeavors illustrate how discrimination has not disappeared after any single piece of legislation, but rather has required lengthy periods (even decades) of attempts at implementation, court cases, and subsequent additional laws to rectify problems and alter public attitudes. In each of these historical examples, given the complex and nuanced social situations in which discrimination occurs, bias has nonetheless continued, despite the adoption of initial legislation.
Practice Implications
Currently, providers and patient advocacy organizations are often not entirely sure how to advise patients and family members concerning whether, when, and to whom to disclose genetic risks. Though GINA represents an important advance, these data suggest that subtle forms of discrimination could exist that may make it too early for patients to risk discrimination by disclosing fully and widely. It is premature to assess GINA’s full eventual effects, benefits and limitations, but it is crucial that this legislation does not inadvertently promote a false sense of protection and security. Caution and discretion remain key. Over upcoming years, the amount of discrimination may increase because of GINA, as some patients may now feel it is safer to begin to disclose more. Employers may feel it is permissible to engage in more discrimination, since it is not necessarily detected or detectable, and hence is not necessarily punishable. Indeed, the fine for violation of GINA is only $300,000, which may cost some employers less than a patient’s ongoing treatment over many years. Hence, companies may feel that it is cheaper financially to discriminate and merely pay the fine if caught.
These data highlight, as well, needs for genetic counselors and other providers to have up-to-date detailed information about current relevant federal and state laws, including potential limitations and extents of these policies. These areas will no doubt continue to evolve. Indeed, as mentioned above, recent Supreme Court rulings have narrowed the scope of protection provided by the ADA (Sutton v. United Airlines, Inc. 1999; Toyota Motor Manufacturing, Kentucky, Inc. v. Ella Williams 2002), leading Congress to redefine aspects of the legislation to broaden its coverage (2008, ADA Amendment). These interviewees underscore the importance of providers being cognizant and up-to-date about these shifting areas, in order to be able to offer clear information to patients and families. Enhanced education of providers, policy makers, patients, family members and others about the complex legal issues involved here (e.g., what the ADA defines as “disabled”) is vital. Just as the ADA has been found over the years to generate a range of ambiguities, GINA, too, will no doubt pose uncertainties that will need to be closely studied, monitored, and addressed. The need to maintain and offer up-to-date information may require additional effort from providers, that national professional organizations can potentially help in compiling and disseminating
The data here suggest, too, that genetic counselors might potentially address with clients whether other family members may need assistance in confronting fears or experiences of discrimination. Importantly, genetic counselors should also be as sensitive as possible to the possible effects of GINA over time and consider gauging these, since over upcoming years, this knowledge may help in refining and improving the legislation and/or its implementation.
Implications for Research
These data suggest several specific avenues for future research. Clearly, more studies are needed to understand the landscapes and contexts into which GINA has been introduced, and the effects it will have over time. GINA was passed based on fears, more than actual evidence of discrimination, and numerous aspects of patients’ views, fears and experiences of discrimination in the US and many other countries remain unknown. If discrimination is subtle, patients may be less likely to be aware of it, or to report it. Hence, further study should begin now, proactively, as the effects of GINA begin, to monitor and assess its effects over time. The law may not be able to prevent differential treatment based on genetic risk, but to understand the extent of such treatment is still crucial, in order to comprehend how best to address it—e.g., through enhanced education of patients, families, providers, employers, co-workers and others.
Specifically, research needs to assess more fully not only overt discrimination, but these more subtle fears and experiences; and to measure, if possible, frequencies of the various types of such occurrences both now (immediately post-GINA), and over time. Studies should assess, too, how often, to what degree, and when (e.g., among what subgroups of patients) fears of discrimination may impede individuals’ decisions to disclose their risks to family members and others, undergo testing and/or treatment, and change jobs or move; and what other factors, if any, may be involved (e.g., type of employer, insurer, or disease). Studies should also examine how the availability of treatment, and the existence of stigma associated with a particular disease for reasons other than genetic etiology (e.g., because of psychiatric symptoms) may affect these issues. As suggested above, future research can also analyze relationships between testing status and views and experiences of possible discrimination.
Yet, the current data suggest as well that critical methodological challenges and vagaries persist. The forms, degrees, and frequencies of discrimination remain difficult to assess, in large part because of key questions concerning how best to define “discrimination”, “failure to accommodate”, and “appropriate degrees of accommodation” in particular situations. Questions remain as to whether over-solicitude and “being treated differently” ever constitute discrimination, and if so, how and when, and what subcategories of genetic discrimination exist—raising a next generation of genetic discrimination issues. The notion of finding wholly objective and overt evidence, as opposed to subjective and implicit accounts of discrimination may also not be entirely realistic.
These data also have critical policy implications. The fact that these individuals are concerned about life, long-term care and disabilities insurance suggests that policy initiatives in these areas need to be urgently considered as well. Given the sensitivities, ambiguities, and nuances suggested by these data, how GINA is actually implemented, monitored and enforced will be crucial.
These data have several potential limitations. The sample size may be small compared to some other quantitative research, but is sufficient for a qualitative study of this kind, to illuminate the rage of themes that emerge (Klitzman et al. 2007c). We did not analyze statistical differences between those who reported vs. did not report discrimination, or those who reported genetic discrimination vs. disability discrimination, since the statistical power would be too low, given the sample size, to draw meaningful conclusions. However, these analyses can be pursued in future research.
These interviews were conducted before GINA was passed, while it was still being debated and widely discussed. Nonetheless, future research can examine these issues at later dates as well, when GINA is implemented, and periodically thereafter, given other changes in ever-evolving medical practice. We only interviewed the patient, not employers or others about patients’ reports, but these perceptions are important in and of themselves. Future research can investigate dyads of patients and others.
As mentioned above, a critic could potentially completely disregard patients’ fears of discrimination as subjective, yet these concerns nonetheless appear profoundly to affect coping and decisions about whether to pursue testing, and whether to disclose risk and test status to others. Similarly, an external observer could potentially assert that these concerns are about merely “possible discrimination”, yet as the Oxford English Dictionary indicates, discrimination depends on the presence of “unjust” or “prejudicial” treatment. Definitions of justice, and of being “pre-judged” vary widely (Rawls 1971), and are inherently open to differing interpretations and individual perceptions. Moreover, discrimination, as suggested here, can be subtle, combined with other motivations, and hard to disentangle and prove. Hence, it is often not definite and explicit, but only suspected.
As more genetic data is amassed on more individuals, needs increase to educate providers, patients, family members, employers, insurers, policy makers and others about these critical, nuanced, and ever-evolving issues—to understand what forms discrimination can and does take, when and how often, and with what implications, what the scope and limitations of legislation are, and where and how further education and policy may be beneficial. In these ways, the medical, legal and psychological interests of patients and their families can best be upheld.
Acknowledgments
I would like to thank Wendy Chung, Karen Marder, Deborah Thorne, Carol Moskowitz, Jennifer Williamson, Edward Eden, Lori Tartell, Rubie Senie, Victor Grann, Carolyn Kumah, Lisa Chin and Melissa Conley. This project was funded through grant #5-R01-HG002431-01 from the ELSI program of the National Human Genome Research Institute.
Appendix: Sample Questions from Semi-Structured Interview
What do you feel comfortable or uncomfortable having others know about your genetic or other medical information? What assumptions do you make concerning protections of patient privacy and confidentiality?
Have you discussed testing and/or treatment issues with any other people? How, who, when and why? What did they say? How did you feel about the interactions you had with them about these issues?
Have you ever felt stigma or discrimination because of an illness? Because of other reasons?
Have other people ever found out about your health information without your wanting them to? When and how?
Does your employer have access to your health information? Do you think he/she would under new laws? Do you think your employer has ever used health information in work decisions (such as hiring or promotions_ with employees?
Do you know of others (such as family members) who have faced discrimination or stigma as a result of genetic or other health information? What experiences did these others have?
References
- Americans with Disabilities Act Amendments Act. 2008 Public Law 110–325 September 25 2008
- Billings PR, Kohn MA, de Cuevas M, Beckwith J, Alper JS, et al. Genetic discrimination as a consequence of genetic screening. American Journal of Human Genetics. 1992;50:476–482. [PMC free article] [PubMed] [Google Scholar]
- Brown L, editor. The new shorter Oxford English dictionary on historical principles. Vol. 1. Oxford: Clarendon; 1993. [Google Scholar]
- Charles KK. [Accessed August 26, 2008];A simple model of subtle discrimination. 1999 from http://www.fordschool.umich.edu/research/papers/PDFfiles/00-014.pdf.
- Geer KP, Ropka ME, Cohn WF, Jones SM, Miesfeldt S. Factors influencing patients’ decisions to decline cancer genetic counseling services. Journal of Genetic Counseling. 2001;10(1):25–40. doi: 10.1023/a:1009451213035. [DOI] [PubMed] [Google Scholar]
- Geertz C. Interpretation of cultures: Selected essays. New York: Basic Books; 1973. [Google Scholar]
- Genetic Information Nondiscrimination Act. 110th Congress, 2nd Session. H.R; 2008. p. 493. [Google Scholar]
- Greely HT. Banning genetic discrimination. New England Journal of Medicine. 2005;353(9):865–867. doi: 10.1056/NEJMp058116. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006. 2006;18(1):59–82. [Google Scholar]
- Hall MA, Rich SS. Laws restricting health insurers’ use of genetic information: impact on genetic discrimination. American Journal of Human Genetics. 2000;66:293–307. doi: 10.1086/302714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MA, McEwan JE, Barton JC, Walker AP, et al. Concerns in primary care population about genetic discrimination by insurers. Genetics in Medicine. 2005;7(5):311–316. doi: 10.1097/01.gim.0000162874.58370.c0. [DOI] [PubMed] [Google Scholar]
- Jones NL, Smith AM. Report for congress. [Accessed June 2, 2008];Genetic information: Legal issues relating to discrimination and privacy. 2003 from http://ncseonline.org/NLE/CRSreports/03Jun/RL30006.pdf.
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Decision-making about reproductive choices among individuals at-risk for Huntington’s Disease. Journal of Genetic Counseling. 2007a;16(3):347–362. doi: 10.1007/s10897-006-9080-1. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Marder K. The roles of family members, health care workers and others in decision-making processes about genetic testing among individuals at risk for Huntington’s Disease. Genetics in Medicine. 2007b;9(6):358–371. doi: 10.1097/GIM.0b013e3180653c5a. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Disclosures of Huntington’s Disease risk within families: patterns of decision-making and implications. American Journal of Medical Genetics. 2007c;143:1835–1849. doi: 10.1002/ajmg.a.31864. [DOI] [PubMed] [Google Scholar]
- Klitzman R. Improving education on doctor-patient relationships and communication: the views of doctors who become patients. Academic Medicine. 2006;81(5):447–453. doi: 10.1097/01.ACM.0000222271.52588.01. [DOI] [PubMed] [Google Scholar]
- Lapham EV, Kozma C, Weiss JO. Genetic discrimination: perspectives of consumers. Science. 1996;274:621–624. doi: 10.1126/science.274.5287.621. [DOI] [PubMed] [Google Scholar]
- Legal Times. No intent, no foul? Unconscious bias in employment decisions is actionable under current law. 2007 May 21;XXX(21) [Google Scholar]
- Low L. Genetic discrimination in life insurance: empirical evidence from a cross-sectional survey of genetic support groups in the United Kingdom. BMJ. 1998;317(7173):1632–1635. doi: 10.1136/bmj.317.7173.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PS. Is there a pink slip in my gene? Genetic discrimination in the work place. Journal of Health Care Law & Policy. 2000;3(2):225–265. [PubMed] [Google Scholar]
- National Human Genome Research Institute. National institute of health. [Accessed January 28, 2009];Genetic Information Nondiscrimination Act of 2008. 2008 from www.genome.gov/pfv.cfm?pageID=10002328.
- NCSL. National Conference of State Legislatures. [Accessed March 24, 2006];Genetics and health insurance state anti-discrimination laws. 2006 from www.ncsl.org/programs/health/genetics/ndishlth.htm.
- New York Times. Congress passes bill to bar bias based on genes. 2008 May;2:2008. [Google Scholar]
- Nowlan WJ. A rational view of insurance and genetic discrimination. Science. 2002;297:195–196. doi: 10.1126/science.1070987. [DOI] [PubMed] [Google Scholar]
- Nowlan WJ. A scarlet letter or a red herring? Nature. 2003;421:313. doi: 10.1038/421313a. [DOI] [PubMed] [Google Scholar]
- Otlowski MF. Exploring the concept of genetic discrimination. Journal of Bioethical Inquiry. 2005;2(3):165–176. doi: 10.1007/BF02448597. [DOI] [PubMed] [Google Scholar]
- Otlowski MF, Taylor SD, Barlow-Stewart KK. Genetic discrimination: too few data. European Journal of Human Genetics. 2003;11:1–2. doi: 10.1038/sj.ejhg.5200910. [DOI] [PubMed] [Google Scholar]
- Oveson L, Yarborough M. 2. Vol. 2. The Ramazzini Institute for Occupational and Environmental Health Research; 2001. [Accessed May 21 2008]. Aspen report: “Ethical issues in occupational genetics”. www.ramazziniusa.org/apr01/geneticp. [Google Scholar]
- Pollack A. Congress near deal on genetic test bias bill. New York Times; 2008. Apr 23, [Google Scholar]
- Rawls J. A theory of justice. Harvard University Press; 1971. [Google Scholar]
- Rothenberg KH, Terry SF. Human genetics: before it’s too late—addressing fear of genetic information. Science. 2002;292(5579):196–197. doi: 10.1126/science.1075221. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research—techniques and procedures for developing grounded theory. Newbury Park: Sage; 1990. [Google Scholar]
- Sutton v. United AirLines, Inc. 527 U.S. 471 (1999).
- Taylor S, Treloar S, Barlow-Stewart K, Stranger M, Otlowski M. Investigating genetic discrimination in Australia: a large-scale survey of clinical genetics clients. Clinical Genetics. 2008;74:20–30. doi: 10.1111/j.1399-0004.2008.01016.x. [DOI] [PubMed] [Google Scholar]
- Taylor S, Treloar S, Barlow-Stewart K, Otlowski M, Stranger M. Investigating genetic discrimination in Australia: perceptions and experiences of clinical genetics service clients regarding coercion to test, insurance and employment. Australian Journal of Emerging Technologies and Society. 2007;5(2):63–83. [Google Scholar]
- Toyota Motor Manufacturing, Kentucky, Inc. v. Ella Williams, 534 U.S. 184 (2002).
- Treloar S, Taylor S, Otlowski M, Barlow-Steward K, Stranger M, Chenoweth K. Methodological considerations in the study of genetic discrimination. Community Genetics. 2004;7:161–168. doi: 10.1159/000082254. [DOI] [PubMed] [Google Scholar]
- Wertz DC. Genetic discrimination—an overblown fear? Nature. 2002;3:496. doi: 10.1038/nrg854. [DOI] [PubMed] [Google Scholar]