Abstract
BACKGROUND
The quality of medication use in older adults is suboptimal with a large percentage of individuals not receiving recommended care. Most efforts to evaluate the quality of medication use target high-risk drugs, appropriate treatment of prevalent chronic disease states, or a set of predefined quality indicators of medication use, rather than the patient. It is also suggested that racial differences in the quality of medication use may exist in older adults.
OBJECTIVE
To determine the prevalence, number, and types of medication-related problems in older adults, examining the impact of race on quality medication use.
METHODS
A prospective cohort study involving in-home interviews and medical record reviews of 200 community-residing older adults stratified by race (100 blacks, 100 whites) conducted three times over 1 year. No intervention to address medication-related problems was performed. The quality of medication use was reported as medication-related problems by clinical pharmacists.
KEY RESULTS
Mean age was 78.3 (whites) and 75.5 (blacks), with the majority being female. Although whites used more medications than blacks (11.6 versus 9.7; p < 0.01), blacks had more medication-related problems per person than whites (6.2 versus 4.9; p < 0.01). All patients had at least one medication-related problem; common problems at baseline, 6 months, and 12 months for both whites and blacks were undertreatment, suboptimal drug use, suboptimal dosing, nonadherence, and less costly alternative available. Blacks had significantly higher rates of nonadherence than whites (68% versus 42%; p < 0.01). Over the 12-month study, the number of medication-related problems not only persisted but increased (adjusted p=0.0168).
CONCLUSIONS
Medication-related problems are prevalent in both black and white older adults and persist over one-year. Blacks had more medication-related problems than whites, including higher rates of nonadherence. These findings require further study to better understand racial disparities in the quality of medication use in older adults and the impact of race on specific medication-related problems.
Keywords: Quality, Medication use, Medication-related problems, Older adults
INTRODUCTION
The quality of medication use in older adults falls below established standards; one study suggests that only 62% of individuals receive recommended care.1
Quality problems of medication use are of particular concern in older adults who are more likely to have multiple chronic diseases, visit multiple providers, and use multiple medications, placing them at an increased risk of developing medication-related problems.2,3 This, in turn, may compromise their health status, functional status, and quality of life.4,5 Not only do medication-related problems take their toll on the health and well being of older adults, drug-related morbidity and mortality is costly, estimated to be $177 billion annually.6,7 Table 1 outlines the main categories of quality problems of medication use and associated medication-related problems.
Table 1.
| Medication-Related Problem | Definition |
|---|---|
| Suboptimal Drug | The individual is receiving a drug that has no indication, is not effective, or is potentially not safe (i.e., potential for harm exceeds potential for benefit). |
| Suboptimal Dose, Duration, Frequency, or Administration | The individual is taking an appropriate medication, but the dose, duration, frequency or administration is not optimal to achieve desired response, or has the potential for harm. |
| Adverse Drug Events | The individual is experiencing an actual adverse consequence at the time of the interview that is attributed to a drug or the inappropriate use of a drug. |
| Nonadherence* | The individual has not filled a prescription, is not taking a drug, or is not using a drug as prescribed, whether intentional or unintentional. |
| Less Costly Drug Available | The individual is prescribed a medication for which a less costly, equally effective and safe drug is available, and preferred by the patient, but the patient is receiving a more expensive product; or the patient could benefit from prescription savings, but is not receiving eligible benefits and desires to. |
| Undertreatment | The individual has a medical condition or risk factors for a disease that would benefit from drug therapy (clear indication) and the patient has no contraindications to the drug, but the drug was not prescribed. |
| Suboptimal Medication Monitoring | The individual is receiving a drug and monitoring is recommended (according to established practice guidelines) to assess response to therapy or prevent harm, but the monitoring has not been done. |
We used 2 methods to assess nonadherence: the primary assessment (leading to identification of a medication-related problem of nonadherence) was the clinical pharmacist implicit assessment of adherence for each medication a person was taking (i.e., adherent, nonadherent)following the comprehensive medication review 14 and a validated patient self-report measure.37 Because no gold standard exists for measuring nonadherence, we relied on multiple methods of assessment.
Research on the quality of medication use often targets select medication-related problems or pre-defined quality indicators of medication use.3,4,8,9 We recently proposed a framework that offers a more comprehensive and patient-centered definition of the quality of medication use.3 A comprehensive approach to evaluating medication use that takes into account the whole person and all the medications a person may be taking may provide more meaningful information upon which to intervene to improve the quality of medication use. The extent of racial disparities on the quality of medication use in older adults remains largely unknown. Older black adults have been found to have lower drug spending, use fewer prescription medications, have higher rates of medication non-adherence, and higher rates of underuse of necessary medications than whites.10–13 However, no study to our knowledge has examined racial differences in the quality of medication use when quality is reported as a composite of medication-related problems and takes into account all medications a patient may or may not be taking3
The purpose of this study was to assess the prevalence, number, and type of medication-related problems in black and white older adults at three points in time over a 12-month period through in-home interviews and medical record reviews, examining the impact of race on quality medication use. The study was specifically designed with no intervention to evaluate the quality of medication use over one year in older adults receiving usual care.
METHODS
Overview
The detailed methods for this longitudinal study are described elsewhere.14 Briefly, this study was a 12-month prospective cohort study in which 200 older adults stratified by race (100 white, 100 black; determined via self report and medical record verification) who resided independently in the community were recruited from the Department on Aging Eldercare Program and 2 senior housing complexes located in Orange County, North Carolina. Subjects met the following inclusion criteria: (1) white or black, (2) age ≥ 60 years; (3) residing independently in the community setting; (4) taking ≥3 regularly-scheduled prescription and/or non-prescription medications; (5) able to read and speak English; and (6) willing to participate, as indicated by providing informed consent and HIPAA-compliant authorization for release of medical information. Patients were excluded if they had ≥3 errors on a cognitive screening instrument or received clinical pharmacy services within the past 6 months.15 Using the Eldercare Program contact list, the pharmacists conducted a screening call with each older adult enrolled in the Eldercare program to describe the study and invite them to participate in a baseline visit for verification of eligibility and enrollment. Recruitment from the senior housing complexes relied on individual response by telephone to posted flyers. Of 435 older adults screened via telephone; 235 individuals were excluded because they were not eligible (105), could not be reached by phone (72), refused to participate (44), or had died (14).14 Thus 200 patients were enrolled into the study and interviewed by a pharmacist. The study was conducted from April 2005 through August 2007. The Biomedical Institutional Review Board of the University of North Carolina at Chapel Hill approved this study.
The study employed two pharmacists part-time with Doctor of Pharmacy degrees. One completed residency training in geriatrics, is a board-certified pharmacotherapy specialist, and has practiced as a clinical pharmacist in an outpatient, interdisciplinary geriatric practice setting for 6 years; the other is an independent consultant pharmacist providing medication management services to older adults in the community.
Data Collection and Measures
Data were collected at baseline, 6 months and 12 months. All measures used in this study have been described in detail elsewhere.14 The measures include demographics; the short test of functional health literacy in adults (S-TOFHLA), which categorizes patient’s ability to read and understand health-related material as inadequate (0–16), marginal (17–22), or adequate (23–36) health literacy; and an 8-item self-reported instrumental activities of daily living (IADL) scale, where the score on each item 0 (completely dependent on others), 1 (some assistance required), or 2 (independence) was summed to give a total score that ranged from 0 (poorest functional status) to 16 (best functional status).16,17
The quality of medication use was measured and reported as medication-related problems.3,14 The study investigators developed a list of seven medication-related problems following an extensive literature review; the measure was adapted from a previously published model to incorporate current professional knowledge and clinical experience and refined by study investigators over time.18–20,21 The underlying premise of this framework was that the number of medication-related problems a person has may be a reflection of their overall quality of medication use; the more problems, the poorer the quality of medication use. The pharmacists used a 3-step implicit process to guide their assessment of medication-related problems.14 The 3-step implicit process included 1) a comprehensive medication review with the older adult, 2) a medical record review, and 3) clinical pharmacist formulation of medication-related problems. During the comprehensive in-home medication review, the pharmacist recorded detailed information on medical conditions, medications, and medication-taking behaviors. Following the home visit, the pharmacist reviewed the patient’s medical record to abstract information on medications, medical conditions, laboratory values, physician assessment of the individual’s medical conditions, hospitalizations, and any information pertinent to assessing the quality of medication use. For the final step, the pharmacist formulated an assessment of the quality medication use, taking into account best research evidence (e.g., published literature, established indicators of quality care, clinical practice guidelines), clinical expertise and patient values. This assessment of quality took the form of a listing of potential medication-related problems for each individual (Table 1).
Statistical Analysis
The sample size estimation for our study was based on confidence interval (CI) widths and detecting meaningful differences between whites and blacks in the proportion of individuals with ≥1 medication-related problem at baseline. A sample size of 100 per group met the conservative “sufficiently large” criterion formula21: n · p ≥10 or n (1−p) ≥10
where n is the sample size and p is the prevalence of ≥1 medication-related problem allowing the use of the normal distribution for calculation of CIs. This sample size resulted in 95% CI half-widths of 6% to 10% for prevalences ranging from 10% to 90% and provided an 80% power to detect absolute differences of ≥14% to 21% between whites and blacks depending on the prevalences in the 2 groups (α = 0.05).
Descriptive statistics are presented and comparisons were made by race (oversampled blacks to specifically address racial differences.) using two sample t-tests (continuous data) or chi-square tests of association (categorical data). The two primary outcomes identified a priori were: (1) overall prevalence of medication-related problems in the population for blacks and whites (proportion of subjects with any of the medication-related problems); and (2) average number of medication-related problems per person for blacks and whites. Secondary outcomes were the prevalence and average number of problems broken down by the seven individual medication-related problems for blacks and whites.
We used generalized linear mixed models to analyze the two primary endpoints of prevalence and number of medication related problems. The primary exposure of interest was race. Models were adjusted for a fixed pharmacist effect, to adjust for pharmacist variability, and for the following covariates identified a priori based on published literature: number of baseline medications; health literacy, defined as S-TOFHLA < 17; age; and gender. For the primary outcomes of interest, statistical significance was achieved at p≤0.05. No formal corrections for multiple testing were conducted for the secondary outcomes of interest. However, we were conservative in interpreting the findings of these secondary outcomes; statistical significance was reached at a level of 0.01, while tests with 0.01 <p-value ≤ 0.05 were only considered suggestive of a relationship. All analyses were conducted using SAS version 9.1 (SAS, Cary, NC).
RESULTS
Baseline demographic characteristics for the 200 subjects are presented in Table 2. The majority of participants in both groups were female (77%). Whites were significantly older, had more education, and were more likely to live alone. Whites used more medications (11.6 versus 9.7, p<0.01), had a greater number of chronic conditions (8.4 versus 7.4, p=0.01), and used more physicians (3.6 versus 2.8, <0.01), compared to blacks (Table 3). In addition, more whites maintained a written list of their medications than blacks (30% versus 16%, p=0.02), while a higher percentage of blacks could not purchase their medications due to cost (28% versus 12%, p<0.01). Whites were more likely than blacks to have adequate health literacy (58% vs. 29% p<0.01).
Table 2.
Demographic and baseline characteristics of community-residing older adults (n = 200)
| White (n = 100) | Black (n = 100) | P-value | |
|---|---|---|---|
| Age, mean (SD), y | 78.3 (8.2) | 75.5 (8.5) | 0.02 |
| Female, % | 72 | 81 | 0.13 |
| Education, highest level completed, % | <0.001 | ||
| Elementary | 8 | 24 | |
| Some high school | 6 | 19 | |
| High school graduate | 21 | 35 | |
| Some college or technical school | 24 | 12 | |
| College graduate | 18 | 6 | |
| Postgraduate | 23 | 4 | |
| Living alone, % | 64 | 49 | 0.03 |
Table 3.
Medication and health-related characteristics of community-residing older adults (n = 200)
| White (n = 100) | Black (n = 100) | P-value | |
|---|---|---|---|
| Medications, * mean (SD); range | 11.6 (5.0); 3–26 | 9.7 (4); 4–21 | 0.003 |
| Chronic conditions, † mean (SD); range | 8.4 (3.1); 2–19 | 7.4 (2.8); 2–18 | 0.01 |
| Physicians, mean (SD); range | 3.6 (1.8); 1–9 | 2.8 (1.5); 0–8 | <0.001 |
| Pharmacies, mean (SD); range | 1.3 (0.6); 1–3 | 1.3 (0.5); 1–3 | 0.42 |
| Has help with medications, % | 16 | 16 | 1.00 |
| Uses medication aid ‡, % | 70 | 57 | 0.06 |
| Pill box, % | 47 | 50 | 0.67 |
| Written list of medications, % | 30 | 16 | 0.02 |
| Shows written list to physician, % | 18 | 11 | 0.16 |
| Has some form of prescription drug coverage, % | 91 | 94 | 0.42 |
| Could not purchase meds due to cost, % | 12 | 28 | 0.005 |
| Short-test of functional health literacy in adults (S-TOFHLA) §; mean (SD); range | 24.2 (10.6); 0–36 | 14.8 (11.9); 0–35 | <0.001 |
| Adequate (%) | 58 | 29 | |
| Marginal (%) | 12 | 13 | |
| Inadequate (%) | 30 | 58 | |
| Lawton Instrumental Activities of Daily Living Scale (IADLs) ||; mean (SD); range | 13.7 (3.0); 1–16 | 13.5 (3.0); 4–16 | 0.69 |
Includes all medications (i.e., prescription, over-the-counter, and complementary and alternative medications).
Defined as any chronic condition documented in the medical record.
Does not add up to 100%, since patients may have been using more than one medication aid.
Scores range from 0 to 36 and are categorized as inadequate (0–16), marginal (17–22), or adequate (23–36) health literacy.
Scores range from 0 (low function, dependent) to 16 (high function, independent).
Prevalence of Medication-Related Problems
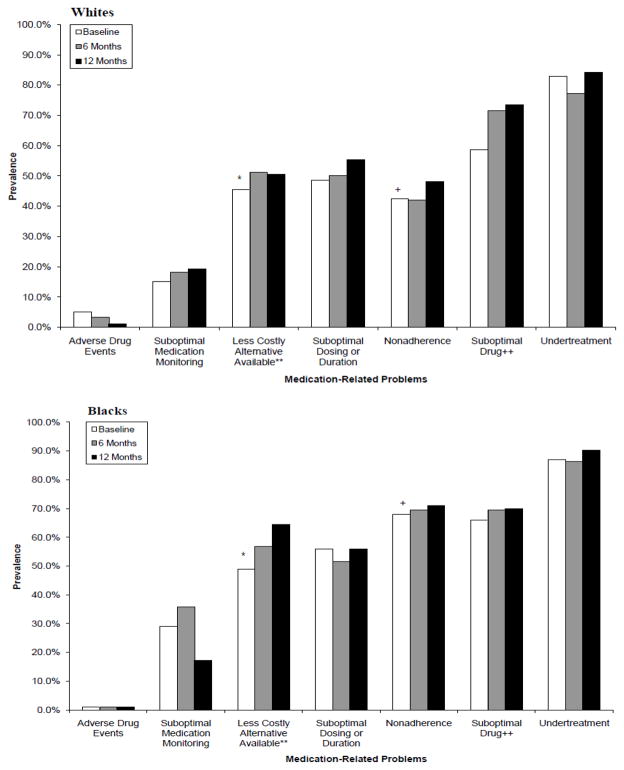
All patients had at least one medication problem at baseline, 6 months, and 12 months. Common problems at baseline, 6 months, and 12 months for both whites and blacks were undertreatment, suboptimal drug use, suboptimal dosing, nonadherence, and less costly alternative available (Figure 1).
Figure 1.
Prevalence of Medication-Related Problems over the 12-month Study
Significant differences between race at baseline: *p≤ 0.001 for race +p≤ 0.05 for race
Significant increase in a medication-related problem over time: **p≤0.001 for time ++p≤0.05 for time
All data adjusted for fixed pharmacist effect and baseline number of medications, health literacy, age, gender.
Some differences in the prevalence of medication-related problems between blacks and whites are worth noting (Figure 1). First, not only was the prevalence of “a less costly alternative available” significantly different between blacks (49%) and whites (46%) at baseline after adjusting for fixed pharmacist effect, baseline number of medications, age, gender, and health literacy (p<0.0001), there was also a significant increase in the prevalence over the 12-month study. Second, a significant difference in the prevalence of nonadherence between blacks (68%) and whites (42%) at baseline was observed after adjusting for the same covariates (p=0.003); the rates of nonadherence slightly increased over the 12-month study to 71% for blacks and 48% for whites; however, this was not found to be statistically significant (p=0.32). Finally, although there was no significant difference in the prevalence of suboptimal drug use between blacks and whites at baseline, after adjusting for covariates, the data suggests that the prevalence of suboptimal drug use increased over time (p=0.03), with the most notable increases among white older adults.
Number of Medication-Related Problems
Overall, whites had on average fewer number of medication-related problems at baseline than blacks (mean (SD): 4.9 (2.7) whites vs. 6.3 (3.2) blacks; adjusted p=0.0004) (Table 4). Over the 12-month study, the number of medication-related problems persisted and actually increased over time (adjusted p=0.0168) in whites and blacks. Most of the increase in number of problems reflects use of suboptimal drugs and use of expensive drugs where less costly alternatives exist.
Table 4.
Number of Medication-Related Problems in Black and White Older Adults
| Problems | Black
|
White
|
p-values1 |
p-values2 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline n=100 |
6 Mos n=95 |
12Mos n=93 |
Baseline n=99 |
6 Mos n=88 |
12Mos n=83 |
Race3 | Time | Race3 | Time | |
| Overall | 6.34 (3.17) | 6.62 (3.42) | 6.61 (4.17) | 4.86 (2.70) | 5.09 (2.65) | 5.80 (3.25) | 0.0028 | 0.0182 | 0.0004 | 0.0168 |
| Adverse Drug Events 4 | 0.01 (0.10) | 0.01 (0.10) | 0.01 (0.10) | 0.05 (0.22) | 0.03 (0.18) | 0.01 (0.11) | -- | -- | -- | -- |
| Less Costly Alternative Available | 0.69 (0.83) | 0.81 (0.84) | 0.98 (1.05) | 0.59 (0.76) | 0.69 (0.79) | 0.72 (0.87) | 0.2856 | 0.0220 | 0.0706 | 0.0185 |
| Suboptimal Medication Monitoring | 0.38 (0.66) | 0.45 (0.66) | 0.18 (0.42) | 0.19 (0.49) | 0.20 (0.46) | 0.20 (0.44) | 0.0253 | 0.0763 | 0.0586 | 0.0745 |
| Nonadherence | 1.89 (2.25) | 1.79 (2.09) | 1.92 (2.74) | 0.91 (1.51) | 0.95 (1.58) | 1.05 (1.51) | 0.0002 | 0.3514 | 0.0054 | 0.3443 |
| Suboptimal Dosing or Duration | 0.75 (0.81) | 0.73 (0.80) | 0.75 (0.79) | 0.73 (0.91) | 0.66 (0.76) | 0.80 (0.85) | 0.9940 | 0.7624 | 0.2208 | 0.7751 |
| Suboptimal Drug | 1.26 (1.54) | 1.51 (1.58) | 1.52 (1.46) | 1.15 (1.48) | 1.47 (1.39) | 1.69 (1.80) | 0.7146 | 0.0016 | 0.5069 | 0.0014 |
| Undertreatment | 1.36 (0.92) | 1.33 (0.83) | 1.25 (0.65) | 1.24 (0.87) | 1.08 (0.79) | 1.33 (0.94) | 0.3425 | 0.8385 | 0.9342 | 0.8704 |
Data provided as mean (standard deviation)
Calculated from Poisson mixed model, adjusting for fixed pharmacist effect
Calculated from Poisson mixed model, adjusting for fixed pharmacist effect and baseline number of medications, health literacy, age, gender
The p-values listed for race are for comparisons of baseline data between blacks and whites.
An adverse drug event was defined as “The individual is experiencing an actual adverse consequence at the time of the interview that is attributed to a drug or the inappropriate use of a drug.”
Among the individual problems, a significant difference between blacks and whites in non-adherence remained after adjusting for pharmacist, number of medications, health literacy, age and gender (p=0.005). There was also a significant increase in the use of suboptimal drugs over time (p=0.001). In addition, some borderline results are worth noting: the increase over time in the problem of “less costly alternative available” (p=0.02), the differences between blacks and whites with respect to this problem at baseline (p=0.07), and the trend towards blacks having significantly more problems at baseline related to the need for medication monitoring (adjusted p=0.06) (Table 4).
Since nonadherence was such a large component of the overall number of medication-related problems and was the only problem that was significantly different between blacks and whites after covariate adjustment, we conducted a sensitivity analysis. We removed nonadherence from the list of medication-related problems, and reran the model. While the differences was not as large, the mean number of medication-related problems remained significantly greater for blacks than whites (4.34 versus 3.97; adjusted p=0.037).
DISCUSSION
This study demonstrates that medication-related problems are prevalent in community-dwelling older adults; medication-related problems affect both blacks and whites, with racial disparities observed in both the prevalence and number of medication-related problems; and, with usual medical care, medication-related problems persist over one year.
Overall, the average number of medication-related problems identified in our study was 6.3 for blacks and 4.9 for whites. The higher number of medication-related problems documented in our study compared to previous studies may be due to a several factors.21, 23,24 First, previous assessments of medication use often target patients with specific chronic conditions or pre-defined quality indicators. We examined medication-related problems across all chronic and acute diseases, taking into account the whole person. Such an approach is more likely to help clinicians better assess chronic conditions and implement strategies to improve older adults’ health. Second, most studies have focused on the community pharmacy setting, where pharmacists rely on patient interviews and prescription records in formulating an assessment of medication-related problems. In our study, pharmacists relied not only on information gathered from the patient during a comprehensive medication review, but gathered information from inspection of pill bottles, and, most notably, from the patient’s medical record. Thus, we had more information and a more complete picture of the patient when formulating assessments of medication use.
We observed racial differences in the quality of medication use. Several studies have documented lower rates of prescription drug spending in blacks compared to whites, use of fewer medications in blacks compared to whites, higher rates of medication nonadherence in blacks compared to whites, and higher rates of medication underuse in blacks compared to whites.10–13 Our findings are unique in that racial differences were found in the overall quality of medication use. Blacks had significantly more medication-related problems at baseline than whites (6.3 compared to 4.9, p=0.0003); a difference that persisted over the 12-month study, even after adjusting for health literacy, baseline number of medications, age, and gender. In addition, racial disparities were noted in the prevalence of several medication-related problems, including nonadherence and use of an expensive drug when a less costly alternative was available, with a trend toward some difference in the need for medication monitoring. Furthermore, when nonadherence was removed from the overall model the mean number of medication-related problems remained significantly greater for blacks than whites (4.34 versus 3.97; adjusted p = 0.037) at baseline, suggesting that other disparities in the quality of medication use do exist. Future studies will need to more closely examine disparities in the quality of medication use between blacks and whites and the impact of such disparities on health outcomes as well as elucidate factors that may be contributing to these disparities and the implications this may have on the design of interventions to improve outcomes.
The main findings from the study are important for several reasons. First, all of our patients were followed in primary care practices receiving what we would consider “standard of care”, yet medication-related problems were identified in both blacks and whites and persisted. This suggests that strategies to identify and resolve medication-related problems in the outpatient setting are needed.25 Second, racial differences in blacks and whites were noted, with blacks having significantly more medication-related problems overall than whites. This is not entirely surprising considering that racial disparities have been previously documented with respect to underuse of needed medications as well as medication nonadherence. Although further studies are needed to examine differences between blacks and whites with respect to specific medication-related problems, the study findings raise some important clinical considerations. Are there medication-related problems of particular concern in blacks that warrant further investigation? Should interventions to evaluate and manage medications in older adults differ based on race?
There are several limitations of our study. First, although we report trends toward significant differences between blacks and whites with respect to specific medication-related problems (e.g., less costly alternative available, medication monitoring needed), it is important to note that the sample size within each of these categories is quite small both in overall number and in terms of change. With such small samples we are limited in our ability to detect meaningful differences between blacks and whites as it relates to specific medication-related problems and to adjust for important covariates that might explain any racial differences. Second, we reported that over the 12-month study the number of medication-related problems persisted and actually increased over time (adjusted p=0.0168) in whites and blacks. Although beyond the scope of this paper, clearly, additional studies would be needed to further evaluate the increase in problems noted as well as any impact of race on a rise in problems. Third, we excluded older adults with cognitive impairment, a group at high risk of medication-related problems. Fourth, it was impossible to blind pharmacists to patient race. Fifth, despite our attempts to standardize their assessment, one pharmacist documented a mean of 1.6 more medication-related problems per patient than the other. Although we adjusted for a fixed pharmacist effect in our analyses, the potential variability in pharmacist’s assessments of medication-related problems will need to be considered in designing future studies. We recently completed reliability testing of the framework of medication-related problems among clinical pharmacists, using three paper-based clinical cases; there was substantial to almost perfect agreement in pharmacist identification of MRP categories (k=0.68–0.74) compared to a gold standard key. Additional inter-rater reliability testing is being conducted as part of an ongoing longitudinal intervention study. We continue to believe that an implicit framework for assessing medication-related problems in older adults remains the most appropriate method for assessing the overall quality of medication use for both clinical and research purposes.3 Finally, it will be important in future studies to determine physician agreement with the clinical pharmacist’s assessment of medication-related problems and their acceptance of recommendations to optimize medication therapy. These next steps will serve to strengthen the implicit measurement of the quality of medication use as we work toward a framework for assessing medication-related problems that is not only well defined and reliable, but valid.
CONCLUSION
Medication-related problems are prevalent in both black and white older adults and persist over one-year. Blacks had more medication-related problems than whites, including higher rates of nonadherence. Moreover, with no targeted intervention to address the quality of medication use, medication-related problems persist and appear to rise over time in both black and white older adults. These findings require further study to better understand racial disparities in the quality of medication use in older adults and the impact of race on specific medication-related problems.
Acknowledgments
Dr. Roth had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors wish to thank Robin H. Zook, PharmD, CGP, MTM Pharmacy Associates, for her assistance in subject recruitment, enrollment and data collection.
The authors wish to thank Ryan Owenby, PharmD for his assistance in project management and data entry (Ryan was a Doctor of Pharmacy student and a student research assistant, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill when this study was ongoing).
The authors wish to thank John Paul Timmins, MBA, Planning Systems Productivity & Co. for designing, developing, and maintaining the study database.
Funding Sources
Drs. Roth and Ivey receive funding from the National Institutes of Health, National Institute on Aging (Principal Investigator (MTR): 5K23AG024229-04 Research and Career Development Award). The funding agency has no role in the design and conduct of the study; data collection; management; analysis; interpretation of the data; or preparation, review, or approval of this manuscript.
Drs. Esserman and Weinberger receive funding from the National Institutes of Health (CTSA UL1RR025747). The funding agency has no role in the design and conduct of the study; data collection; management; analysis; interpretation of the data; or preparation, review, or approval of this manuscript.
Dr. Weinberger is supported by a VA Career Development Award. The funding agency has no role in the design and conduct of the study; data collection; management; analysis; interpretation of the data; or preparation, review, or approval of this manuscript.
The study was also supported by an American College of Clinical Pharmacy (ACCP) Frontiers Fund Research and Career Development Award.
Footnotes
CONFLICT OF INTEREST
There are no conflicts of interest or financial interests to declare for any of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Denise A. Esserman, Email: Denise_Esserman@med.unc.edu.
Jena L. Ivey, Email: ivey@unc.edu.
Morris Weinberger, Email: mweinber@email.unc.edu.
References
- 1.Shrank WH, Asch SM, Adams J, et al. The quality of pharmacologic care for adults in the United States. Med Care. 2006;44:936–45. doi: 10.1097/01.mlr.0000223460.60033.79. [DOI] [PubMed] [Google Scholar]
- 2.Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007 Dec;22(Suppl 3):391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth MT, Weinberger M, Campbell WH. Measuring the quality of medication use in older adults. J Am Geriatr Soc. 2009 Jun;57(6):1096–102. doi: 10.1111/j.1532-5415.2009.02243.x. Epub 2009 Apr 16. [DOI] [PubMed] [Google Scholar]
- 4.Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38:666–71. doi: 10.1067/mem.2001.119456. [DOI] [PubMed] [Google Scholar]
- 5.Higashi T, Shekelle PG, Adams JL, et al. Quality of care is associated with survival in vulnerable older patients. Ann Intern Med. 2005;143:274–81. doi: 10.7326/0003-4819-143-4-200508160-00008. [DOI] [PubMed] [Google Scholar]
- 6.Fu AZ, Jiang JZ, Reeves JH, Fincham JE, Lin GG, Perri M. Potentially inappropriate medication use and healthcare expenditures in the US community-dwelling elderly. Med Care. 2007;45:472–6. doi: 10.1097/01.mlr.0000254571.05722.34. [DOI] [PubMed] [Google Scholar]
- 7.Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: Updating the cost-of-illness model. J Am Pharm Assoc. 2001;41:192–9. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- 8.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 9.Knight EL, Avorn J. Quality indicators for appropriate medication use in vulnerable elders. Ann Intern Med. 2001;135:703–10. doi: 10.7326/0003-4819-135-8_part_2-200110161-00009. [DOI] [PubMed] [Google Scholar]
- 10.Smedley BD, Stith AY, Nelson AR, editors. for the Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, the Board on Health Sciences Policy, and the Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 11.Gaskin DJ, Briesacher BA, Limcangco R, Brigantti BL. Exploring racial and ethnic disparities in prescription drug spending and use among Medicare beneficiaries. Am J Geriatr Pharmacother. 2006;4:96–111. doi: 10.1016/j.amjopharm.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23:654–71. doi: 10.1007/s11606-008-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qato DM, Lindau ST, Conti RM, Schumm LP, Alexander GC. Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiol Drug Saf. 2010 Aug;19(8):834–42. doi: 10.1002/pds.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roth MT, Moore CG, Ivey JL, Esserman DA, Campbell WH, Weinberger M. The quality of medication use in older adults: methods of a longitudinal study. Am J Geriatr Pharmacother. 2008;6:220–33. doi: 10.1016/j.amjopharm.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–81. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 17.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 18.Strand LM, Morley PC, Cipolle RJ, Ramsey R, Lamsam GD. Drug-related problems: their structure and function. DICP. 1990;24:1093–7. doi: 10.1177/106002809002401114. [DOI] [PubMed] [Google Scholar]
- 19.Shrank WH, Polinski JM, Avorn J. Quality indicators for medication use in vulnerable elders. J Am Geriatr Soc. 2007;55 (Suppl 2):S373–82. doi: 10.1111/j.1532-5415.2007.01345.x. [DOI] [PubMed] [Google Scholar]
- 20.Kerr EA, Smith DM, Hogan MM, et al. Building a better quality measure: are some patients with poor quality actually getting good care? Med Care. 2003;41(10):1173–82. doi: 10.1097/01.MLR.0000088453.57269.29. [DOI] [PubMed] [Google Scholar]
- 21.Cipolle RJ, Strand LM, Morley PC, editors. Pharmaceutical Care Practice. New York, NY: McGraw-Hill; 2004. [Google Scholar]
- 22.Pagona M, Gauvreau K, editors. Principles of Biostatistics. 2. Pacific Grove, Calif: Duxbury; 2000. [Google Scholar]
- 23.Kassam R, Farris KB, Burback L, Volume CI, Cox CE, Cave A. Pharmaceutical care research and education project: pharmacists’ interventions. J Am Pharm Assoc. 2001;41(3):401–10. doi: 10.1016/s1086-5802(16)31254-2. [DOI] [PubMed] [Google Scholar]
- 24.Alkema GE, Wilber KH, Simmons WJ, Enguidanos SM, Frey D. Prevalence of potential medication problems among dually eligible older adults in Medicaid waiver services. Ann Pharmacother. 2007 Dec;41(12):1971–8. doi: 10.1345/aph.1K270. [DOI] [PubMed] [Google Scholar]
- 25.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 26.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]