Abstract
A 28-year-old male with hemophagocytic lymphohistiocytosis presented with left ventricular dysfunction and cardiac arrest. Percutaneous cardiopulmonary support (PCPS) was initiated, but left heart distension developed with associated aggravation of pulmonary edema. Percutaneous transseptal left atrial sheath (28-Fr) drainage was incorporated into the PCPS venous circuit under fluoroscopic guidance to enable left heart decompression 1 days after PCPS initiation. The patient's pulmonary edema improved markedly, and distention of his left heart diminished. He was successfully weaned from PCPS 5 days later. Percutaneous transseptal left atrial drainage with large venous cannulae is feasible and effective in decompressing the left heart in adult patients during PCPS.
Keywords: Heart arrest, Assisted circulation, Heart catheterization
Introduction
Percutaneous cardiopulmonary support (PCPS) is a mode of circulatory support provided to bridge patients with severe cardiac failure to recovery or heart transplantation.1),2) If venoarterial PCPS is applied, left heart distension and pressure overload may develop and lead to pulmonary edema, subendocardial ischemia, and further deterioration of left ventricular function. Therefore, left heart decompression is often necessary following PCPS.3-5) Although the percutaneous transseptal approach is considered to be more practical and leads to less complications than other techniques, it fails to effectively achieve left heart decompression in adult patients.6),7)
We report a case of successful left heart decompression in an adult during PCPS by using percutaneous transseptal left atrium (LA) drainage with a large venous cannula.
Case
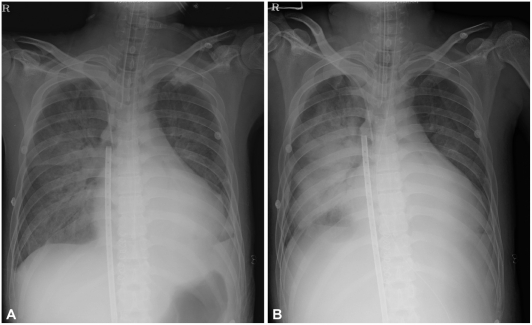
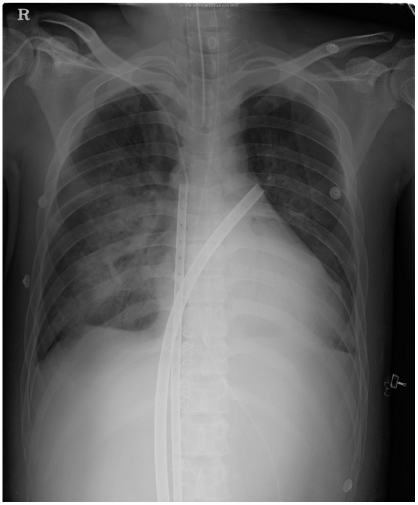
A 28-year-old male was referred to our unit with a 4-week history of high fever. He was 167 centimeters tall and weighed 55 kilograms. He was initially admitted to the general ward for diagnostic work-up. Laboratory results confirmed anemia, thrombocytopenia, decreased fibrinogen level. Bone marrow biopsy confirmed hemophagocytosis in the bone marrow and reduced natural killer-T cell activity. The diagnosis was secondary hemophagocytic lymphohistiocytosis (HLH) due to viral infection. Steroid and intravenous immunoglobulin were administered, but on the fifth hospital day the patient developed hemodynamic failure despite increased medical support. He was transferred to the intensive care unit, where echocardiography revealed severe left ventricular systolic dysfunction with an ejection fraction of 20%. On the next day, the patient experienced a seizure followed by pulseless cardiac arrest. PCPS was rapidly applied using a 21-Fr venous cannula in the right femoral vein and a 17-Fr arterial cannula in the right femoral artery (Fig. 1A). With a flow rate of 4.0 L/min, stable blood pressure was maintained but pulmonary edema and left heart distention rapidly deteriorated (Fig. 1B). Thirty-four hours later, it was decided to perform percutaneous transseptal LA decompression under fluoroscopic guidance. Transseptal puncture was performed via the left femoral vein using a Brockenbrough transseptal needle with a 8-Fr Mullin sheath. A 28-Fr cannula was positioned in the LA after dilating the puncture site of the atrial septum with a percutaneous mitral valvuloplasty dilator. The LA drain was then incorporated into the venous limb of the PCPS circuit. There were no complications related to this procedure. Within hours, the patient's pulmonary edema improved considerably, and his distended left heart diminished (Fig. 2). Decompression continued for 5 days, and the patient was weaned from PCPS after a total of 6 days following restoration of stable hemodynamics without neurologic sequelae. After immunosuppressive therapy, the patient was discharged. Echocardiography performed 4 months after discharge revealed normal left ventricular function without left to right shunting through the transseptal puncture site.
Fig. 1.
Chest radiographs showing interval change over time since percutaneous cardiopulmonary support initiation. A: anteroposterior chest radiograph illustrating percutaneous cardiopulmonary support initiation. B: chest radiograph showing severe pulmonary edema and left heart distension developed shortly after percutaneous cardiopulmonary support initiation.
Fig. 2.
Anteroposterior chest radiograph following percutaneous transseptal left atrial drainage while on percutaneous cardiopulmonary support, with left heart decompression and subsequent improvement of pulmonary edema.
Discussion
HLH is often a fatal disease caused by specific gene mutations, various infections, hematologic malignancies, autoimmune disorders or drugs. HLH may manifest with multiple organ dysfunction, including cardiac involvement.8),9)
According to the Extracorporeal Life Support Organization registry, there was an increase in the proportion of pediatric patients undergoing LA decompression over the study period, from 4% between 1995 and 1998, to 30% between 2003 and 2006.2) However, the data regarding adult patients are limited, and the frequency of left heart decompression and success rates have not been reported. As ischemic heart disease a very common underlying conditions in adult patients with PCPS, there may be greater need for left heart decompression in adult patients than in pediatric patients. Therefore, it is important to develop a useful left heart decompression method in adult patients during PCPS.
Aiyagari et al.6) showed that adequate decompression of the left heart could be achieved by transseptal left atrial sheath placement incorporated into an extracorporeal membrane oxygenation venous circuit in a study of 7 cases. However, there were no adult survivors. In that study, the size of the left atrial drain catheters used was 8- to 15-Fr. Larger LA cannulae diameters and higher maximum LA cannula flow rates indexed to body surface area were associated with more satisfactory left heart decompression.6) Poor outcomes in adult patients may be attributable to small cannula size. Therefore, we inserted a large cannula (28-Fr) into the LA under fluoroscopic guidance for our patient. Transsepal left heart catheterization using a large cannula has been widely applied to manage patients with various indications, such as ablation of atrial fibrillation and percutaneous mitral valvuloplasty, in which its safety and feasibility have been demonstrated.10-12) In addition, gradual dilation of the puncture site in the atrial septum may lower the risk of complications. To our knowledge, this is the first report describing effective left heart decompression and successful weaning of PCPS via percutaneous transseptal LA drainage in an adult patient.
In summary, percutaneous transseptal left atrial drainage with a large venous cannula appears to be feasible and effective for the decompression of the left heart in adult patients during PCPS.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Rhee I, Gwon HC, Choi JH, et al. Percutaneous cardiopulmonary support for emergency in-hospital cardiac arrest or cardiogenic shock. Korean Circ J. 2006;36:11–16. [Google Scholar]
- 2.Rajagopal SK, Almond CS, Laussen PC, Rycus PT, Wypij D, Thiagarajan RR. Extracorporeal membrane oxygenation for the support of infants, children, and young adults with acute myocarditis: a review of the Extracorporeal Life Support Organization registry. Crit Care Med. 2010;38:382–387. doi: 10.1097/CCM.0b013e3181bc8293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward KE, Tuggle DW, Gessouroun MR, Overholt ED, Mantor PC. Transseptal decompression of the left heart during ECMO for severe myocarditis. Ann Thorac Surg. 1995;59:749–751. doi: 10.1016/0003-4975(94)00579-6. [DOI] [PubMed] [Google Scholar]
- 4.Seib PM, Faulkner SC, Erickson CC, et al. Blade and balloon atrial septostomy for left heart decompression in patients with severe ventricular dysfunction on extracorporeal membrane oxygenation. Catheter Cardiovasc Interv. 1999;46:179–186. doi: 10.1002/(SICI)1522-726X(199902)46:2<179::AID-CCD13>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 5.Cheung MM, Goldman AP, Shekerdemian LS, Brown KL, Cohen GA, Redington AN. Percutaneous left ventricular "vent" insertion for left heart decompression during extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2003;4:447–449. doi: 10.1097/01.PCC.0000075325.53339.CA. [DOI] [PubMed] [Google Scholar]
- 6.Aiyagari RM, Rocchini AP, Remenapp RT, Graziano JN. Decompression of the left atrium during extracorporeal membrane oxygenation using a transseptal cannula incorporated into the circuit. Crit Care Med. 2006;34:2603–2606. doi: 10.1097/01.CCM.0000239113.02836.F1. [DOI] [PubMed] [Google Scholar]
- 7.Guirgis M, Kumar K, Menkis AH, Freed DH. Minimally invasive left-heart decompression during venoarterial extracorporeal membrane oxygenation: an alternative to a percutaneous approach. Interact Cardiovasc Thorac Surg. 2010;10:672–674. doi: 10.1510/icvts.2009.228346. [DOI] [PubMed] [Google Scholar]
- 8.Creput C, Galicier L, Buyse S, Azoulay E. Understanding organ dysfunction in hemophagocytic lymphohistiocytosis. Intensive Care Med. 2008;34:1177–1187. doi: 10.1007/s00134-008-1111-y. [DOI] [PubMed] [Google Scholar]
- 9.Karapinar B, Yilmaz D, Balkan C, Akin M, Ay Y, Kvakli K. An unusual cause of multiple organ dysfunction syndrome in the pediatric intensive care unit: hemophagocytic lymphohistiocytosis. Pediatr Crit Care Med. 2009;10:285–290. doi: 10.1097/PCC.0b013e318198868b. [DOI] [PubMed] [Google Scholar]
- 10.Hammerstingl C, Lickfett L. Safety of single transseptal puncture for ablation of atrial fibrillation: retrospective study from a large cohort of patients. J Cardiovasc Electrophysiol. 2008;19:E36. doi: 10.1111/j.1540-8167.2008.01115.x. author reply E37. [DOI] [PubMed] [Google Scholar]
- 11.Babaliaros VC, Green JT, Lerakis S, Lloyd M, Block PC. Emerging applications for transseptal left heart catheterization old techniques for new procedures. J Am Coll Cardiol. 2008;51:2116–2122. doi: 10.1016/j.jacc.2008.01.061. [DOI] [PubMed] [Google Scholar]
- 12.Liu TJ, Lai HC, Lee WL, et al. Immediate and late outcomes of patients undergoing transseptal left-sided heart catheterization for symptomatic valvular and arrhythmic diseases. Am Heart J. 2006;151:235–241. doi: 10.1016/j.ahj.2005.02.034. [DOI] [PubMed] [Google Scholar]