Abstract
Objective
To evaluate the feasibility of robotic single-port transumbilical total hysterectomy using a home-made surgical glove port system.
Methods
We retrospectively reviewed the medical records of patients who underwent robotic single-port transumbilical total hysterectomy between January 2010 and July 2010. All surgical procedures were performed through a single 3-4-cm umbilical incision, with a multi-channel system consisting of a wound retractor, a surgical glove, and two 10/12-mm and two 8 mm trocars.
Results
Seven patients were treated with robotic single-port transumbilical total hysterectomy. Procedures included total hysterectomy due to benign gynecological disease (n=5), extra-fascial hysterectomy due to carcinoma in situ of the cervix (n=1), and radical hysterectomy due to cervical cancer IB1 (n=1). The median total operative time was 109 minutes (range, 105 to 311 minutes), the median blood loss was 100 mL (range, 10 to 750 mL), and the median weight of the resected uteri was 200 g (range, 40 to 310 g). One benign case was converted to 3-port robotic surgery due to severe pelvic adhesions, and no post-operative complications occurred.
Conclusion
Robotic single-port transumbilical total hysterectomy is technically feasible in selected patients with gynecological disease. Robotics may enhance surgical skills during single-port transumbilical hysterectomy, especially in patients with gynecologic cancers.
Keywords: Robotic surgery, Single-port, Laparoscopic, Hysterectomy, Gynecology
INTRODUCTION
Laparoscopic single-port transumbilical surgery (L-SPS) is an emerging technique. Recently, several investigators demonstrated the feasibility of the single-port transumbilical approach for many gynecological procedures, including hysterectomy, adnexal surgery, and myomectomy [1-6]. These articles showed that outcomes of L-SPS are comparable or superior to conventional laparoscopic surgery in terms of blood loss, hospital stay, and post-operative pain. Nevertheless, the limitations of L-SPS are also apparent, and L-SPS remains a challenging procedure due to its technical difficulties. Therefore, developing a better surgical instrument for L-SPS is essential.
Currently, the da Vinci robotic system (Intuitive Surgical Corporation, Sunnyvale, CA, USA) is the robot most frequently used for assisting laparoscopic surgery in the world. Robotic surgery has allowed surgeons to overcome some of the technical limitations of conventional laparoscopic surgery [7-9]. Optimized ergonomics and the endo-wristed instruments of the robotic platform may improve surgical proficiency during L-SPS.
The application of robotic surgery to laparoendoscopic single-site surgery (LESS) has already been introduced for a few urologic, colorectal, and gynecologic surgical procedures [3, 10-12]. However, Escobar and colleagues provide the only reported cases of robot-assisted LESS gynecologic surgery, including two hysterectomies, one bilateral salpingo-oophorectomy, and one retroperitoneal lymph node biopsy [3,13]. In the present study, we aim to evaluate the feasibility of robotic single-port transumbilical total hysterectomy (R-SPH) using a novel home-made surgical glove port system.
MATERIALS AND METHODS
1. Patients
Approval for this study was obtained from the Institutional Review Board of the Yonsei University College of Medicine. An Academic Fund of Severance Hospital for Innovative Robotic Surgery supported this study, and the fund covered the cost difference between robotic and conventional laparoscopic surgery. Patients underwent R-SPH between January 2010 and July 2010. Demographic data, medical conditions, surgical history, and post-operative follow-up visits were retrospectively reviewed from medical records, and the operative course, complications, pathology of the surgical specimens, and the operative outcomes were prospectively recorded into a computerized database. Inclusion criteria were patients who did not have any contraindication for surgery and have a planned hysterectomy for a gynecologic condition. Exclusion criteria were uterine size greater than 16 gestational weeks by pelvic examination, previous history of radiation, and confirmed ovarian malignancy. Total operating time for R-SPH was defined as the time from the beginning of skin incision to the completion of skin closure. Docking time and console time were recorded, as defined by Magrina and colleagues [14]. Postoperative pain intensity was rated immediately after surgery and at 6, 24, and 48 hours after surgery using a visual analog scale from 0-10.
2. Surgical techniques
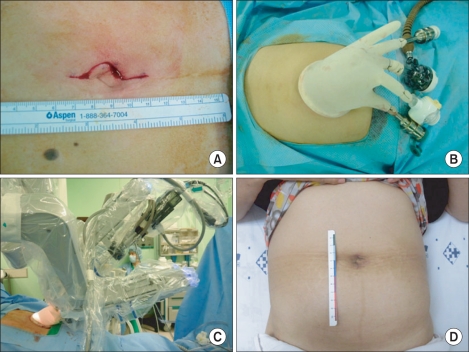
All surgical procedures were performed through a single 3-4 cm umbilical incision with a multi-channel system that consisted of a wound retractor, surgical gloves, and two 10/12-mm and two 8-mm trocars (Fig. 1). For a robotic single-port transumbilical access system, we made a 3-4 cm vertical umbilical skin incision via an open Hasson approach. Then, the Alexis Wound Retractor (Applied Medical, Rancho Santa Margarita, CA, USA) was inserted into the peritoneal cavity. The wrist portion of a size 7.5 surgical glove was fixed to the outer ring of the wound retractor. After making a small hole in the fingertips of the glove, two 10/12-mm and two 8-mm trocars were inserted, and the abdomen was insufflated with CO2 gas.
Fig. 1.
Photograph demonstrating a robotic single-port transumbilical access system. (A) A 3-4 cm vertical transumbilical skin incision was made for entry into the peritoneal cavity. (B) The Alexis Wound Retractor was inserted through the incision and the wrist portion of a size 7.5 glove was fixed to the outer ring of the wound retractor. (C) External view of the port placement during robotic single-port transumbilical hysterectomy. (D) Post-operative wound on the umbilicus at 4 weeks after surgery.
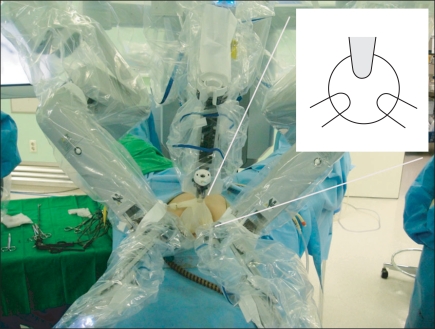
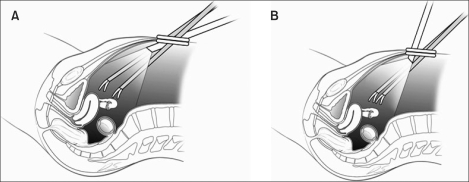
Patients were then placed in the steep Trendelenberg, low-lithotomy position, and the Da Vinci S robot was docked between their legs. The 12 mm trocar for the robotic 30-degree scope and two 8 mm trocars for the robotic instruments were placed in a triangular fashion (Fig. 2). The fourth arm was positioned to the back of the robot and not used. To reduce collisions between the robotic instruments and camera, we used a 30-degree robotic camera down or up depending on the conditions (Fig. 3). We used an EndoWrist Maryland bipolar, EndoWrist permanent Cautery Spatula, and EndoWrist needle holder. Through a 10 mm ancillary port, the surgical assistant performed endoscopic suction and counter-traction with a laparoscopic grasper.
Fig. 2.
Robotic single-port transumbilical access system, as seen from the patient's head. The 12-mm port for the robotic 30 degree scope and two 8 mm ports for the robotic instruments were placed in a triangular fashion.
Fig. 3.
Position of the robotic camera for robotic single-port transumbilical total hysterectomy to reduce collisions between the instruments and camera. (A) As in the conventional multi-port robotic surgery, if the camera and the instruments are inserted at shallow angles in a 30-degree downward position, collisions between the instruments and camera increase. (B) The 30-degree robotic camera is rotated upward to view the pelvic cavity, which results in fewer collisions between the instruments and camera and provides increased space for instruments to move more freely.
After placing the robotic single-port access system, the overall procedure was similar to that of single-port transumbilical laparoscopic surgery as previously described [1,2]. The vaginal cuff was repaired with an intracorporeal continuous suture using 1-0 vicryl (Ethicon, Piscatsway, NJ, USA) in all patients. After hemostasis, the incision was repaired with a 2-0 Polysorb 5/8 circle needle (SynetureTM, Covidien, Mansfield, MA, USA).
RESULTS
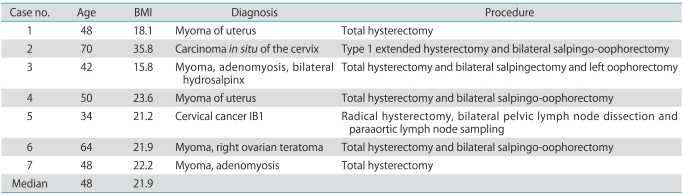
Seven patients underwent R-SPH between January 2010 and July 2010. Table 1 shows the patient characteristics, diagnosis, and surgical procedures. The median age was 48 years (range, 34 to 70 years), and the median BMI was 21.9 (range, 15.8 to 35.8). Procedures included total hysterectomy due to benign gynecological disease (n=5), extra-fascial hysterectomy due to carcinoma in situ of the cervix (n=1), and radical hysterectomy due to cervical cancer IB1 (n=1). Case number 2 received type 1 extended hysterectomy due to positive margin of carcinoma in situ of the uterine cervix on the conization specimen, and Case number 6 received hysterectomy by patient's own choice due to cancer phobia. Three cases of bilateral salpingo-oophorectomy were performed along with hysterectomy, and one case of bilateral salpingectomy and left oophorectomy was performed. In the radical hysterectomy case, bilateral pelvic lymph node dissection and paraaortic lymph node sampling were performed. Previous abdominal or pelvic surgery was noted in two cases (case number 1 and 4).
Table 1.
Patient characteristics and surgical procedures
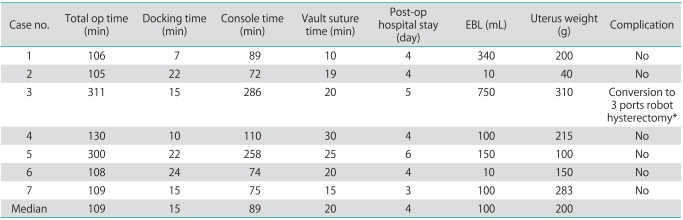
The median operative time was 109 minutes (range, 105 to 311 minutes). In detail, the median docking time was 15 minutes (range, 7 to 24 minutes), the median console time was 89 minutes (range, 72 to 286 minutes), and the median time for vault suture was 20 minutes (range, 10 to 30 minutes). The median blood loss was 100 mL (range, 10 to 750 mL), and the median weight of resected uteri was 200 g (range, 40 to 310 g) (Table 2). None of the patients were converted to laparotomy; however, the third case was converted to 3-port robotic surgery due to severe pelvic adhesions that resulted in significant intra-operative bleeding (750 mL). She was transfused with 3 units of whole blood. The additional ports were inserted about 10 cm apart from the umbilicus at the right and the left lower quadrant to complete the procedure. The fifth patient had stage IB1 cervical cancer. The histologic diagnosis was invasive squamous cell carcinoma, keratinizing type, and the estimated tumor size upon pelvic examination was less than 2 cm. Para-aortic lymph nodes dissection was performed up to the level of the inferior mesenteric artery (supplementary video). Seventeen pelvic lymph nodes and eight paraaortic lymph nodes were retrieved. Pathology revealed no metastasis to the lymph nodes.
Table 2.
Surgical outcomes of robotic single-port transumbilical hysterectomy
Op, operative; EBL, estimated blood loss.
*Case number 3 was converted to 3-port robotic hysterectomy due to severe pelvic adhesions.
In all seven cases, there were no serious post-operative complications such as urinary infection, wound infection, ileus, or wound site hernia. The median hospital stay was 4 days (range, 3 to 6 days). Intravenous patient-controlled analgesia (IV-PCA) was started 30 minutes prior to the end of surgery and maintained for 48 hours for post-operative pain management, and the median pain score measured immediately after surgery was 5 (range, 3 to 6). The majority of patients required one additional intravenous pain medication, and oral nonsteroidal anti-inflammatory drugs provided adequate pain control after the IV-PCA was discontinued.
DISCUSSION
Our preliminary experiences with surgical outcomes after R-SPH demonstrated the technical feasibility of this surgical modality. The median operative time (109 minutes) and the median blood loss (100 mL) were comparable with those of laparoscopic single-port transumbilical total hysterectomy (L-SPH) and robotic multi-port surgery.
In fact, the history of single-port laparoscopic surgery in gynecology dates back to the 1960s. A single-port approach was used in the 1970s for tubal sterilization [15], and Pelosi and Pelosi [16] performed total hysterectomies and bilateral salpingo-oophorectomies using the single puncture technique in 1991. With advances in laparoscopic instruments and techniques in recent years, multi-channel L-SPS has shown promise, as compared with conventional laparoscopic surgery [1,2]. However, L-SPS remains a challenging procedure. Significant collisions between instruments, a limited degree of movement, inferior ergonomics, and a longer learning curve are the main obstacles keeping this procedure from full integration into usual practice.
In this regard, the da Vinci robotic system has already been introduced into single-port laparoscopic surgery by some innovative surgeons. Initial laboratory experience with robotic Natural Orifice Trans-luminal Endoscopic Surgery (NOTES) was reported in 2008 [17]. The first robotic single-port surgeries in humans were reported in urology patients who received radical prostatectomy, dismembered pyeloplasty, and radical nephrectomy [10]. Robotic-assisted single incision partial cecectomy and right colectomy has been reported in colorectal surgery [11,12]. Escobar et al. [3], Fader and Escobar [13] reported four cases of robot-assisted LESS gynecologic surgery, including two hysterectomy cases.
A distinctive feature of the R-SPH performed by our group is the use of a novel multi-channel single-port access system, which consisted of an Alexis Wound Retractor and a surgical glove with four trocars. At our institution, we also use this system for L-SPH [1,2]. This port system allows for the use of a maximum of five trocars, given the number of fingers on the glove, and provides a flexible platform for trocar allocation and trocar changes. Furthermore, due to the elasticity of the surgical glove, this port system allows for increased range of motion and repositioning of the instruments. In addition, there are no issues with gas leak, and the cost is much lower, because we do not use a commercially available single-port system.
For a successful R-SPH, positioning of the camera and instruments is important. Instrument collision can be reduced when the robotic camera and two instruments are placed in a triangular fashion to avoid a coaxial configuration (Fig. 2). The use of a 30-degree robotic camera rotated to look upward allows additional space for robotic arms to move more freely as previously described (Fig. 3) [18]. However, it requires additional time to dock the robotic platform in R-SPH (median, 15 minutes), when compared with conventional robotic surgery.
When considering technical challenges, introducing the robotic system into single-port surgery has several advantages over L-SPH or conventional robotic surgery. The robotic system affords important three-dimensional visualization, magnification of the view, a stable camera platform, fine movement, and tremor control [7,19,20]. The endo-wristed robotic arms provide articulation and more degrees of freedom, which allows for performance of complex surgical procedures, especially intracorporeal suturing and un-roofing the ureters. R-SPH also reduces instrument collisions. Most importantly, R-SPH has superior ergonomics, due to the console system, when compared with L-SPH. Given these advantages, we speculate that the learning curve might be decreased.
In addition, operative complications related to trocar insertion, such as epigastric vessel injury, operative wound infection, and hematoma formation might be avoided by reducing the number of ancillary ports penetrating the abdominal wall. In fact, evisceration of the small bowel and obstruction through the 8 mm robotic port site has been reported [21]. Robotic port site recurrences after radical hysterectomy for cervical cancer have also been reported [22].
It is important to acknowledge the technical limitations of R-SPH. As can be expected, collision and crowding problems do exist, although instrumental collision can be reduced by modification of the positioning of the instruments and the robotic camera. Most of these collisions occur externally between the robotic arms, due to the bulky robotic system. The lack of haptic feedback and the need for a well-trained surgical assistant are other limitations of robotic surgery. The most difficult problem of R-SPH is the larger wound size (3-4 cm) than that of L-SPH (1.5-2 cm), and it is the biggest hurdle in adopting R-SPH in usual clinical gynecologic practice. Use of 5 mm robotic instruments may reduce the incision size; however, there are certain limitations with the current robot system.
In our initial experience, the most exciting case was the fifth case, which was a radical hysterectomy, bilateral pelvic lymphadenectomy, and paraaortic lymphadenectomy in a patient with cervical cancer. Through the use of the robotic system, this is the first case in which a radical hysterectomy was performed successfully using a single-port approach, which is technically a nearly impossible procedure to perform with L-SPS. We feel that this case shows the future direction of robotic single-port transumbilical surgery in gynecology.
There are some limitations of the present study. This study included only a small number of cases, and we selected patients who were deemed to be good candidates for laparoscopic surgery, which may have introduced selection bias. The severe adhesions in the third case were unpredicted. However, given that R-SPH is a new technique, and it is important to establish its feasibility before proceeding with the procedure in more cases. In spite of these weaknesses, to the best of our knowledge, this is the first case series of R-SPH with a novel, home-made port system.
Integrating the existing robotic system into L-SPS enhanced surgical proficiency without increased complications or conversion to laparotomy. While this approach is unique and innovative, the current robotic system is bulky and not specifically designed for single-port surgery. An updated robotic system optimized for single-port surgery with a flexible camera and flexible instruments may solve this problem.
In conclusion, R-SPH is technically feasible in selected patients with gynecological disease. Robotics may enhance surgical skills during single-port transumbilical hysterectomy, particularly in patients with gynecological cancer. However, additional studies with gynecologic oncologic cases should be performed to explore the possible benefits of R-SPH.
ACKNOWLEDGMENTS
The authors are grateful to Dong-Su Jang (Medical Illustrator, Medical Research Support Section, Yonsei University College of Medicine, Seoul, Korea) for his help with the figures. This study was supported by grants from the Yonsei University Research Fund of 2010 (6-2010-0006), a Faculty Research Grant of Yonsei University College of Medicine 2009 (6-2009-0127), and National Research Foundation of Korea Grant funded by the Korean Government (7-2010-0264).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Jung YW, Kim YT, Lee DW, Hwang YI, Nam EJ, Kim JH, et al. The feasibility of scarless single-port transumbilical total laparoscopic hysterectomy: initial clinical experience. Surg Endosc. 2010;24:1686–1692. doi: 10.1007/s00464-009-0830-7. [DOI] [PubMed] [Google Scholar]
- 2.Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010;203:26, e1–e6. doi: 10.1016/j.ajog.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Escobar PF, Fader AN, Paraiso MF, Kaouk JH, Falcone T. Robotic-assisted laparoendoscopic single-site surgery in gynecology: initial report and technique. J Minim Invasive Gynecol. 2009;16:589–591. doi: 10.1016/j.jmig.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010;24:2248–2252. doi: 10.1007/s00464-010-0944-y. [DOI] [PubMed] [Google Scholar]
- 5.Kim YW, Park BJ, Ro DY, Kim TE. Single-port laparoscopic myomectomy using a new single-port transumbilical morcellation system: initial clinical study. J Minim Invasive Gynecol. 2010;17:587–592. doi: 10.1016/j.jmig.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Kim TJ, Lee YY, Kim MJ, Kim CJ, Kang H, Choi CH, et al. Single-port access laparoscopic adnexal surgery. J Minim Invasive Gynecol. 2009;16:612–615. doi: 10.1016/j.jmig.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Magrina JF, Zanagnolo VL. Robotic surgery for cervical cancer. Yonsei Med J. 2008;49:879–885. doi: 10.3349/ymj.2008.49.6.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramirez PT, Soliman PT, Schmeler KM, dos Reis R, Frumovitz M. Laparoscopic and robotic techniques for radical hysterectomy in patients with early-stage cervical cancer. Gynecol Oncol. 2008;110(3 Suppl 2):S21–S24. doi: 10.1016/j.ygyno.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Shafer A, Boggess JF. Robotic-assisted endometrial cancer staging and radical hysterectomy with the da Vinci surgical system. Gynecol Oncol. 2008;111(2 Suppl):S18–S23. doi: 10.1016/j.ygyno.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Kaouk JH, Goel RK, Haber GP, Crouzet S, Stein RJ. Robotic single-port transumbilical surgery in humans: initial report. BJU Int. 2009;103:366–369. doi: 10.1111/j.1464-410X.2008.07949.x. [DOI] [PubMed] [Google Scholar]
- 11.Ragupathi M, Ramos-Valadez DI, Pedraza R, Haas EM. Robotic-assisted single-incision laparoscopic partial cecectomy. Int J Med Robot. 2010;6:362–367. doi: 10.1002/rcs.346. [DOI] [PubMed] [Google Scholar]
- 12.Ostrowitz MB, Eschete D, Zemon H, DeNoto G. Robotic-assisted single-incision right colectomy: early experience. Int J Med Robot. 2009;5:465–470. doi: 10.1002/rcs.281. [DOI] [PubMed] [Google Scholar]
- 13.Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol. 2009;114:157–161. doi: 10.1016/j.ygyno.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 14.Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008;109:86–91. doi: 10.1016/j.ygyno.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Quinones GR, Alvarado DA, Ley Ch E. Tubal ligation using Yoon's ring. Ginecol Obstet Mex. 1976;40:127–136. [PubMed] [Google Scholar]
- 16.Pelosi MA, Pelosi MA., 3rd Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med. 1991;88:721–726. [PubMed] [Google Scholar]
- 17.Haber GP, Crouzet S, Kamoi K, Berger A, Aron M, Goel R, et al. Robotic NOTES (Natural Orifice Translumenal Endoscopic Surgery) in reconstructive urology: initial laboratory experience. Urology. 2008;71:996–1000. doi: 10.1016/j.urology.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 18.White MA, Haber GP, Autorino R, Khanna R, Forest S, Yang B, et al. Robotic laparoendoscopic single-site radical prostatectomy: technique and early outcomes. Eur Urol. 2010;58:544–550. doi: 10.1016/j.eururo.2010.06.040. [DOI] [PubMed] [Google Scholar]
- 19.Mendivil A, Holloway RW, Boggess JF. Emergence of robotic assisted surgery in gynecologic oncology: American perspective. Gynecol Oncol. 2009;114(2 Suppl):S24–S31. doi: 10.1016/j.ygyno.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Visco AG, Advincula AP. Robotic gynecologic surgery. Obstet Gynecol. 2008;112:1369–1384. doi: 10.1097/AOG.0b013e31818f3c17. [DOI] [PubMed] [Google Scholar]
- 21.Seamon LG, Backes F, Resnick K, Cohn DE. Robotic trocar site small bowel evisceration after gynecologic cancer surgery. Obstet Gynecol. 2008;112(2 Pt 2):462–464. doi: 10.1097/AOG.0b013e3181719ba8. [DOI] [PubMed] [Google Scholar]
- 22.Sert B. Robotic port-site and pelvic recurrences after robot-assisted laparoscopic radical hysterectomy for a stage IB1 adenocarcinoma of the cervix with negative lymph nodes. Int J Med Robot. 2010;6:132–135. doi: 10.1002/rcs.295. [DOI] [PubMed] [Google Scholar]